Abstract
Patellofemoral pain syndrome (PFPS) is a very common disorder of the knee. Due to multiple forces influencing the patellofemoral joint, clinical management of this ailment is particularly intricate. Patellofemoral pain syndrome has a multifactorial nature and multiple parameters have been proposed as potential risk factors, classified as intrinsic or extrinsic. Some of the intrinsic risk factors are modifiable and may be approached in treatment. A number of modifiable risk factors have been suggested, including quadriceps weakness, tightness of hamstring, iliopsoas and gastrosoleus muscles, hip muscles dysfunction, foot overpronation, tightness of iliotibial band, generalised joint laxity, limb length discrepancy, patellar malalignment and hypermobility. In general, the routine approach of physicians to this problem does not include assessment and modification of these risk factors and therefore, it may negatively affect the management outcomes. Changing this approach necessitates an easy and practical protocol for assessment of modifiable risk factors and effective and feasible measures to address them. In this review, we aimed to introduce assessment and intervention packages appropriate for this purpose.
Keywords: Anterior Knee Pain, Predisposing Factor, Assessment, Exercise, Management
INTRODUCTION
Patellofemoral pain syndrome (PFPS) is one of the most common ailments of the knee and accounts for 25% of all knee injuries encountered in sports medicine clinics [1–2].
Patellofemoral pain syndrome (PFPS) is an overuse injury characterized by aching pain in the peripatellar area that is exacerbated by physical activities such as climbing stairs, squatting, jumping, running and/or by sitting with the knees flexed for prolonged periods of time [3–5].
Clinical assessment and treatment of this condition are extremely difficult due to the multiple forces affecting the patellofemoral joint. A combination of factors, such as abnormal lower limb biomechanics, soft-tissue tightness, muscle weakness, and excessive exercise may result in increased cartilage and subchondral bone stress and subsequent PFPS [6].
There is clear consensus that the etiology of patellofemoral pain syndrome (PFPS) is multifactorial in nature. Good, scientific evidence exists for an association between PFPS and patellar alignment and mechanics, foot mechanics, and hip strength and mechanics [7].
Several risk factors have been proposed as possible parameters involved in pathogenesis of PFPS. These risk factors are classified as intrinsic or extrinsic risk factors [8].
Extrinsic risk factors are related to factors outside human body, such as the type of sports activity, environmental conditions, and the surface and equipment used. Intrinsic risk factors relate more to individual characteristics [8]. Some of these intrinsic risk factors are modifiable and may be addressed in the management of this disorder in clinical setting.
The review of existing literature has shown that some modifiable risk factors have been theorized to play a role in the development and persistence of PFPS, including quadriceps weakness, specifically in vastus medialis obliqus (VMO) [8–12], tightness of hamstring [8, 11, 13–15], tightness of iliopsoas [11, 16], tightness of iliotibial band [17–19], tightness of gastrosoleus [20–21], hip muscles dysfunction, especially abductors and external rotators [7, 22–23], foot overpronation [20, 24–25], generalized joint laxity [8, 26], limb length discrepancy [27], patellar malalignment [28–29] and patellar hypermobility [8, 28].
Diagnosis of PFPS is mainly clinical and will be made using the five clinical tests, including Patellar apprehension test, Vastus medialis coordination test, Eccentric step test, Patellofemoral grinding test (Clarke's test), and Waldrone's test [30]. A positive outcome on either the vastus medialis coordination test, the patellar apprehension test, or the eccentric step test increases the probability of PFPS to a significant degree [30]. The standard method and interpretation of these tests have been described [31–34].
HOW TO ASSESS THE ACCOMPANYING RISK FACTORS?
In this section, we will discuss the tests applied for assessment of above-mentioned risk factors. Of course, the accurate and objective assessment of each risk factor may mandate complex and expensive methods, such as isokinetic dynamometry, digital goniometry and electromyography, which are not available and practical in the clinical setting. So, we aim to explain simple clinical tests applicable to our routine approach.
Weakness of Quadriceps Muscle
One of the most significant anatomic factors suggested for influencing dynamic patellar stabilization is the strength of quadriceps muscle, especially the vastus medialis obliquus (VMO). It has been considered that this muscle is the main active medial stabilizer of the patella and frequently overpowered by the lateral forces acting on the patella, which include the vastus lateralis (VL), the lateral retinaculum and the iliotibial tract [20]. In some cases the VMO is weak; however, many cases with adequate VMO strength still display delayed onset of the VMO when compared with the vastus lateralis [5, 20, 35]. In these instances, imbalance exists in the activation patterns of the VMO and the VL [10].
It has been shown that the decreased explosive quadriceps strength is a predisposing factor in the development of PFPS [36]. Consequently, a muscle-strength evaluation seems important in PFPS. The isokinetic method is the procedure of choice for muscle-strength measurements. However, since an isokinetic dynamometer is not usually accessible, a functional muscle-strength evaluation by means of a functional test might be considered in the clinical setting. The one-legged hop test is the most common one and has a good reliability[37]. It has been demonstrated that the one-legged hop test correlates well with the isokinetic knee extensor torque [38–39]. As the hop test can be simply performed and a loss of explosive strength has been recognized as an important factor in the development of PFPS[36], it is an important test to evaluate functional muscle performance in patients with PFPS. This test is performed by jumping and landing on the same foot with the hands behind the back. The test is executed three times with each leg, alternately the right and left leg, and the hop distance was measured from toe [37]. A quotient (%) between the injured and non-injured leg is registered and defined as abnormal if the quotient is less than 85% [40].
In patients with PFPS, a selective hypotrophy of the vastus medialis obliquus (VMO) may be a common clinical finding. If this hypotrophy is significant, it can easily be examined clinically and measured by thigh circumference measures 2–3 cm proximal to the patella. In some PFPS patients, the VMO hypotrophy is less visually detectable, and can only be observed during quadriceps contraction. Clinical examination will show that these patients are not capable of generating a strong contraction of the VMO while contracting their quadriceps muscle. Finally, there are PFPS patients who have a VMO hypotrophy, which is hardly detectable by visual inspection or by clinical measurements. In the literature, this deficient activity of the VMO is assessed by EMG findings, since evaluation of isolated VMO activity is not possible only by clinical examination. Several studies have reported that the EMG of VMO/VL ratio in PFPS patients is less than in healthy subjects, with a decreased VMO activity [41–44]. However, it does not seem sensible to use EMG as a routine diagnostic measure.
Tightness of Hamstring
This risk factor is assessed by measurement of popliteal angle with goniometer, using the passive knee extension test [15]. Several studies have used this angle as a measure of hamstring length [45–47].
Hamstring muscle tightness is tested with the subject in a supine position. The examiner lifts one of the straightened limbs and measures the angle of hip flexion [8, 48] (Fig. 1).
Fig. 1.
Passive knee extension test
This test has an excellent inter-rater reliability (ICC= 0.96). Test–retest reliability was also shown to be good for this test [49].
Tightness of Iliopsoas
Decreased iliopsoas flexibility is evaluated using the modified Thomas test [10, 16, 50–52].
To do this test, the participants perch on the end of the bench and roll back into a supine position, while holding both knees firmly to their chest. They hold their contralateral hip in maximal flexion with both arms, while their testing leg is lowered towards the floor. An assistant supports this position by pushing gently on the contralateral knee. The participants are asked to relax the hip and thigh muscles of their testing leg so that a passive end point position is obtained due to gravity alone [53] (Fig. 2). If the iliopsoas is tight, the opposite leg will show initiation of hip flexion through a flexion contracture[16, 50–52]. The observer then assesses the hip angle relative to the horizontal, or 0°-axis, to the nearest degree. A negative angle represents flexion above the horizontal and a positive one represents extension below the horizontal [53].
Fig. 2.
Modified Thomas test to assess tightness of iliopsoas
This test has demonstrated a very good to excellent inter-rater reliability (ICC= 0.90). Test–retest reliability was also shown to be good for this test [49].
Tightness of Iliotibial Band (ITB)
To clinically assess the ITB length, physicians traditionally use the Ober test to evaluate hip adduction as an indirect measure of its length [18, 54–56].
In side lying, the lower leg is flexed to 45 degrees to maintain a neutral lumbar lordosis. The tester stabilises the pelvis with the hand as necessary. The knee is flexed to 90 degrees and the upper leg is passively brought into abduction and extension. The tester lowers the leg into adduction, attempting to control for any visually observed unwanted hip rotation. The end point (angle of adduction) is deemed when no further adduction occurs. If the limb is horizontal, it is considered to be at 0 degrees, if below horizontal (adducted), the angle is recorded as a positive number, and if above horizontal (abducted), the angle is recorded as a negative number [19, 28] (Fig. 3).
Fig. 3.

Ober test to assess tightness of ilitibial band
This clinical test has been shown to have excellent intra and inter-tester reliability [57–58].
Tightness of Gastrosoleus Complex
To assess this type of tightness, weight bearing lunge test is used. This test measures the range of dorsiflexion at the ankle joint. A tape measure is fixed along the floor with the 0 centimeter point at the junction of the floor and wall. The participants position their foot beside the tape so that their heel line and big toe are aligned beside the tape measure. The observer holds the participant's heel to prevent it from lifting off the floor and manually locks the subtalar joint so it remains in a neutral position throughout the test. The participants lunge forward until their knee touches the wall. Then the foot is progressively moved away from the wall until the maximum range of ankle dorsiflexion is reached without the heel lifting (Fig. 4). The most frequent measurements taken at this point are the distance from the foot to the wall or the angle of the tibial shaft from the vertical line using a gravity goniometer [53]. This test is demonstrated to have an excellent intra-rater and inter-rater reliability [59].
Fig. 4.
Forward lunge test to assess tightness of gastrocnemius
Hip Muscles Dysfunction
Hip muscles (particularly the abductors and external rotators) have key role in maintaining the optimal lower limb alignment during weight bearing activities. Diminished strength or coordination of these muscles may be related with an increase in hip internal rotation and adduction, with deleterious effects on the knee. Strong evidence demonstrates this disorder in individuals with PFPS [7, 22, 60].
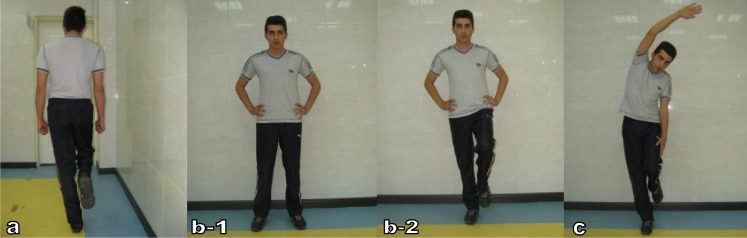
Tests of hip abductor strength (especially gluteus medius) in functional tasks are required and probably useful in identifying athletic individuals who require strengthening [61]. The Trendelenburg test is probably the most commonly known of these tests and is used to assess the ability of hip abductors to hold the pelvis level while the subject performs a single-leg stance. With pelvis fixated, subject lifts one leg to stand in single leg stance with the hip and knee flexed at 90 degrees. Subject should not laterally shift the pelvis as the leg is lifted not balance by side bending the trunk or lift the pelvis at the same time as taking the leg off the floor (Fig. 5-a). Lateral pelvic shift or lowering of one side of the pelvis indicates weakness in the gluteus medius (GM) [61–64]. Modified versions of the Trendelenburg test have been described, such as double- to single-leg stance test (with and without arm elevation). In this test, subject begins standing with two feet on the floor then lifts one leg (Fig. 5-b). Tester watches for notable pelvic tilt on one side, and lateral pelvic shift that may indicate some weakness or lack of control of the GM [61, 65]. The Single-leg balance and anterior or frontal overhead reach squat is a progression of the Trendelenburg test and is commonly used to assess the ability of GM to hold the pelvis level during a more dynamic functional task (Fig. 5-c). Standing in single leg stance, the subject reaches one arm overhead to the same side as the lifted leg. Examiner notes for signs of pelvic tilt towards this side [61, 66].
Fig. 5.
Tests to assess hip abductor dysfunction (a- Trendelenburg sign, b- Double to single leg stance test and c- Single-leg balance and anterior or frontal overhead reach test)
To test external rotator muscles, the patient should be examined standing, and then asked to lift the contralateral foot off the ground while flexing the affected knee. If the hip goes into internal rotation as the patient does a single-legged squat, there may be hip external rotator muscle weakness such that strengthening of the hip rotator muscles may be indicated as part of the patellofemoral rehabilitation program [23].
Excessive Foot Pronation
To investigate this hypothesized intrinsic risk factor [20, 25, 67], Foot Posture Index Version 6 (FPI-6) has been used. This easy to implement clinical assessment tool has good face validity and evaluates the multisegmental nature of foot posture in all three planes and does not require the use of specialized equipment (Fig. 6). The FPI is a 6-item assessment tool performed during relaxed stance, with each item scoring between –2 and +2 to give a sum between –12 (highly supinated) and +12 (highly pronated) [68]. Items include talar head palpation, curves above and below the lateral malleoli, calcaneal angle, talonavicular bulge, medial longitudinal arch, and forefoot-to-rearfoot alignment [69].
Fig. 6.

Assessment of foot pronation using FPI-6 (a- front view, b- side view)
It has been shown that the FPI is able to detect differences between those with and without PFPS and also has high intra- and inter-rater reliability among individuals with PFPS [68, 70].
Generalized Joint Laxity (GJL)
Studies have shown a significant correlation with generalized ligamentous laxity tests and symptomatic PFPS [8, 26, 28, 71, 72].
The instrument to assess this risk factor is the Beighton and Horan Joint Mobility Index (BHJMI), in which the range of scoring is between 0 and 9, with high scores denoting greater joint laxity. The maneuvers used in this scoring system are listed below:
Passive dorsiflexion of the little fingers beyond 90° (one point for each hand) – two points
Passive apposition of the thumbs to the flexor aspects of the forearm (one point for each thumb) –two points
Hyperextension of the elbows beyond 10° (one point for each elbow) – two points
Hyperextension of the knee beyond 10° (one point for each knee) – two points
Forward flexion of the trunk with knees fully extended so that the palms of the hands rest flat on the floor – one point
The Index produces an overall score between 0 and 9; 1 point is given if the criterion is met, 0 if it is not. The overall index scores are often categorized into 1 of 3 groups: 0 to 2, 3 to 4, or 5 to 9. This allows the physician to interpret the scores that are at the high end of the spectrum (i.e. 5 to 9) as indicative of GJL [73–74]. This index has been shown to have a good to excellent reliability in screening for generalized joint laxity [73–75].
Limb Length Discrepancy
It has been proposed as a probable risk factor for patellofemoral pain [8, 27, 76, 77].
The leg-length difference will be evaluated by gauging the distance between the anterior superior iliac spine and the medial malleolus of both legs with the subject in the supine position [27] (Fig. 7). This method has a high intra-rater and inter-rater reliability [78–79].
Fig. 7.
Assessment of true leg length
Patellar Malalignment
Abnormal patellar alignment is believed to be one of the primary causes, but not necessarily the only cause, of PFPS [80]. Patellar alignment is a static measure and can be obtained in various knee flexion angles with or without quadriceps contraction. Patellar alignment can be measured in two aspects, mediolateral displacement and medioateral tilt. Some authors have reported that lateral tilt and displacement were significantly more pathological in patients with PFPS than in controls at 0 degree knee flexion [81–84]. However, although lateral malalignment or maltracking is considered an important characteristic feature of PFPS, the link has not been well clarified [80].
Usually, patellar tilt test and mediolateral glide are applied to assess the patellar alignment. To carry out patellar tilt test, patient lies in the supine position with the knee extended and the quadriceps relaxed. The degree of medial and lateral patellar tilting is determined by comparing the height of medial patella border with that of lateral patellar border. The examiner places his or her thumb and index finger on the medial and lateral border of the patella. Both digits should be of equal height. If the digit palpating the medial border is more anterior than the lateral border, then the patella is tilted laterally. If the digit palpating the lateral border is more anterior than the medial border, then the patella is tilted medially [28].
Mediolateral glide is another measurement of static patellofemoral orientation. McConnell [85, 86] describes the technique as follows: The glide component is examined by use of a tape measure to record the distance from the midpatella to the lateral femoral epicondyle and the distance from the midpatella to the medial femoral epicondyle. The midpatellar point is determined by visual assessment. The patella should be sitting equidistant from each epicondyle when the knee is flexed to 20 degrees.
Measurement of these components is usually done through a combination of visual estimation and palpation, often with the additional use of a tape measure. However, the normative data for these measurements have never been established, unfortunately [87].
Patellar Hypermobility
An increase in medial patellar mobility is significantly associated with the occurrence of the patellofemoral pain syndrome [8].
The patellar mobility test measures passive patellar mediolateral range of motion from the patellar resting position and indicates the integrity and tightness of the medial and lateral restraints. The test is performed with the knee flexed 20 to 30 degrees and the quadriceps relaxed. The patella is divided into four longitudinal quadrants and then an attempt is made to displace the patella in a medial and then lateral direction under the guidance of the examiner's index finger and thumb (Fig. 8). Lateral patellar mobility of three quadrants is suggestive of an incompetent medial restraint. Medial mobility of three or more quadrants suggests a hypermobile patella [28].
Fig. 8.
Patellar mobility test
As with other techniques of patellar position, the assessment of mediolateral mobility is difficult to quantify by manual assessment. Otherwise, the reliability of these measurements is quite low [28, 88].
HOW TO ADDRESS THE RISK FACTORS?
After identification of modifiable intrinsic risk factors, they should be addressed with measures aimed to correct or modify them in a safe, available and effective manner. Of course, there is no consensus on a standard, generally accepted, protocol for each risk factor. In this section, we will try to explain the interventions which have been demonstrated to be efficient based on the existing literature.
Weakness of Quadriceps Muscle
Restoring quadriceps strength and function has been shown to be an important factor in the rehabilitation process [20].
Both weight-bearing and non-weight-bearing exercises may notably improve subjective and clinical outcomes in patients with PFPS [89]. However, selecting the proper exercises requires an understanding of patellofemoral joint biomechanics. During open chain exercises, the amount of quadriceps muscle force required to extend the knee progressively increases as the knee moves from 90° to full knee extension [5]. As well, the patellofemoral joint contact area diminishes as the knee extends, thereby increasing patellofemoral joint stress. By contrast, during closed chain exercises the quadriceps muscle force is minimal at full knee extension and therefore, patellofemoral joint stresses are reduced [5]. Examples of closed chain exercises include lunges, wall slides, squats and leg press machines. Both open and closed chain exercises should be performed so that strengthening can be performed throughout a large arc of motion. Isometrics and open kinetic chain exercises, such as knee extensions, are recommended if there is significant quadriceps weakness or pain with weight bearing [20]. As soon as possible, however, patients should be progressed to the closed kinetic chain exercises, which are more useful than open chain exercises in improving function [20]. To increase eccentric control of the quadriceps, the rehabilitation program also should include exercises performed while standing on one leg. It has been shown that isotonic eccentric training of quadriceps muscles may be effective in pain reduction and functional improvement of patients and can be suggested as part of the treatment [90]. Activation of the lower abdominal and oblique muscles, for example in step-down exercises, helps to decrease the anterior rotation of the pelvis and the consequent internal rotation of the femur [20].
The following is a sample exercise program designed to strengthen the quadriceps muscle:
Stage 1 (first 6 weeks):
- CKC exercises:
- Semi squat with 40 degrees knee flexion, 3 sets, 10 repetitions
- Progressive step-up (10 centimeters high), 3 sets, 10 repetitions
- OKC exercises:
- Straight leg rise in leg external rotation (supine), 3 sets, 10 repetitions
- Sitting leg extension (10° flexion to full extension), 3 sets, 10 repetitions (Fig. 9)
Fig. 9.
Quadriceps strengthening exercises (a- Semi squat with 40 degrees knee flexion, b- Progressive step-up, c- Straight leg rise in external rotation and d- Sitting leg extension)
Stage 2 (second 6 weeks):
- CKC exercises:
- Squat with 90 degrees knee flexion, 3 sets, 10 repetitions
- Progressive step-up (20 centimeters high), 3 sets, 10 repetitions
- OKC exercises:
- Straight leg rise in leg external rotation (supine), 3 sets, 10 repetitions
- Sitting leg extension (90° flexion to full extension), 3 sets, 10 repetitions
Patients are directed to practice these exercises daily [91–92].
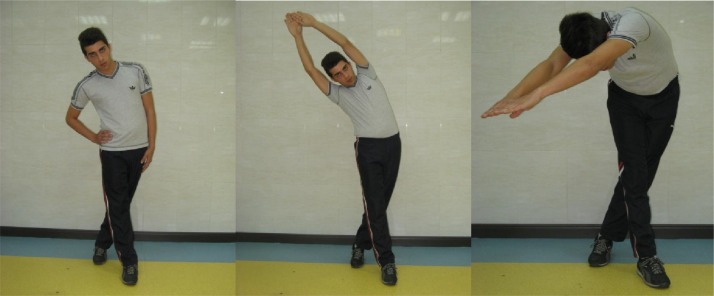
Hamstring Tightness
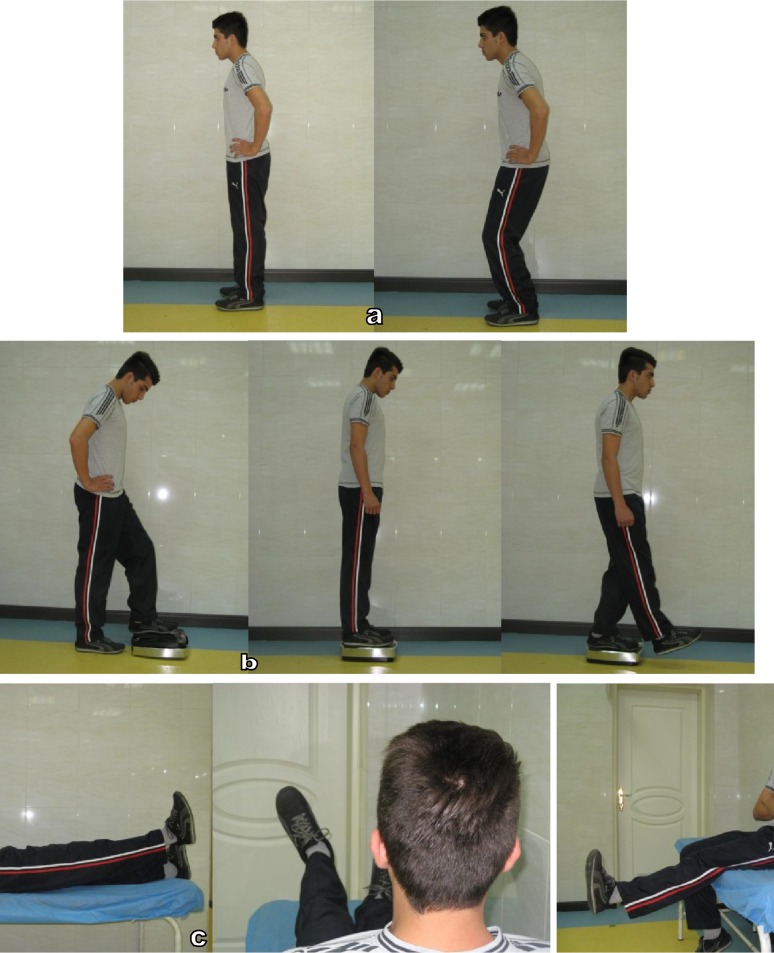
In the case of hamstring tightness, patients are taught to perform 3 alternating repetitions of four passive stretching exercises (Fig. 10), and all stretching repetitions will be held for 15 seconds (12 × 15 s). This program will continue until the end of the 12-week program [93].
Fig. 10.
Hamstring stretch (a- unilateral standing, b- bilateral standing, c- unilateral sitting and d- bilateral sitting)
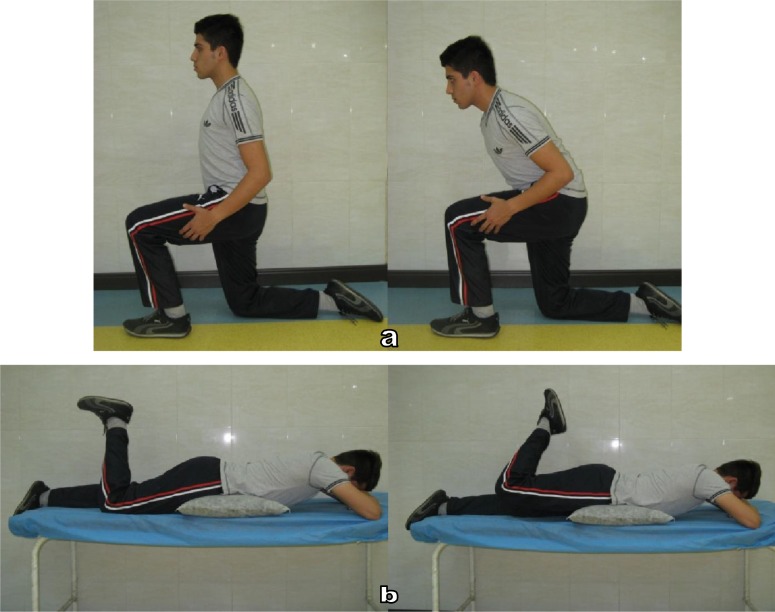
Hip Flexor Tightness
In patients with hip flexor tightness, the stretching program includes passive modified lunge stretch and the active prone leg lifts with the knee bent.
For the modified lunge, each subject was instructed to assume a half-kneeling position with the ipsilateral knee on the ground. A pillow or towel was placed under the knee as needed for comfort. The subject was told to keep the trunk erect and the pelvis in a posterior tilt and to lean forward by flexing the contralateral hip and knee in order to maximize the stretching sensation in the groin of the ipsilateral limb (Fig. 11-a).
Fig. 11.
Hip flexor stretch (a- kneeling on one foot, b- prone lying)
For the prone leg lifts with the knee bent, subjects were instructed to assume a prone position with the ipsilateral knee flexed to 90 degrees, relax their hamstring muscles, and squeeze their gluteal muscles as much as possible to lift the thigh. Pillows were placed under the abdomen as needed for comfort (Fig. 11-b). Both stretches are done for 10 repetitions each in a single daily session and each stretch held for 30 seconds, with up to a 30-second rest period between repetitions [94].
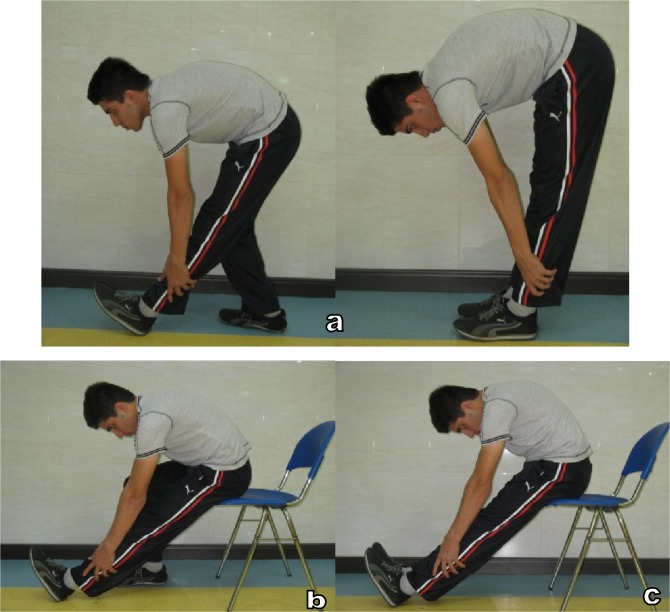
Iliotibial Band Tightness
The exercises to address iliotibial band tightness include common standing stretches in 3 positions of upright standing, overhead clasped hands and diagonally lowered arms [93].
Stretch 1 begins with the subject standing upright. The leg being stretched is extended and adducted across the other leg. The subject exhales while slowly flexing the trunk in a direction lateral to the opposite side. This motion continues until a stretch is felt on the side of the hip around the greater trochanter. Stretch 2 is the same as stretch 1 except the hands are clasped overhead, and the arm on the same side of the leg being stretched is stretched in the same direction. Stretch 3 is the same as stretch 2 except the subject no longer extends arms overhead but diagonally downward (Fig. 12).
Fig. 12.
ITB stretch (a- upright standing, b- overhead clasped hands and c- diagonally lowered arms)
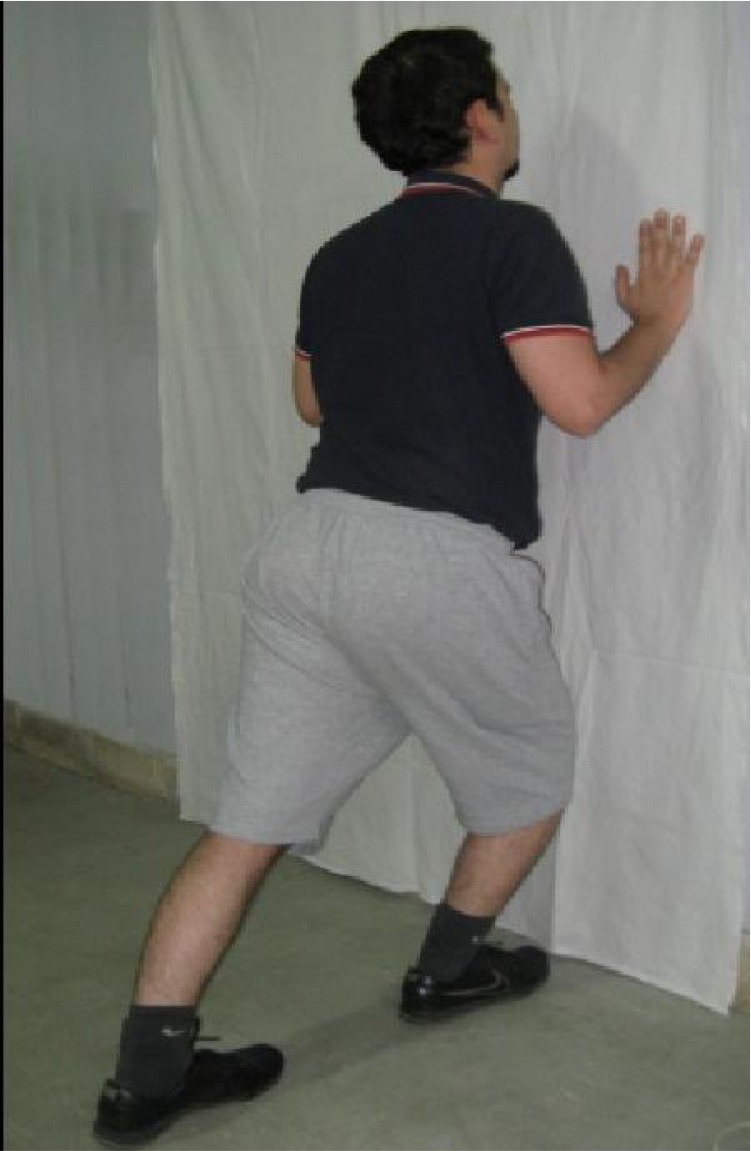
Gastrosoleus Tightness
In the case of gastrosoleus tightness, static stretching in forward lunge position is recommended. To do this stretch, patients stand with arms supported on the wall anterior to the body. Both legs are straight, the hip in neutral rotation, with only the forefoot resting on the platform. The ankle joint is dorsiflexed progressively by leaning towards the wall until they feel the largest stretch that they are willing to tolerate (Fig. 13). Patients are taught to hold the static stretch for 60 seconds and complete two repetitions, for a total of 120 seconds of stretch during each session. Each session is performed on a daily basis over a 12-week period [96–97].
Fig. 13.
Gastrosoleus stretch (forward lunge)
Hip Muscle Dysfunction
The hip strengthening program starts with isometric strengthening exercises for the gluteus medius. This exercise is performed in sidelying with the hips and knees slightly flexed to minimize contribution from the tensor fascia lata. When a stable spinal position could be maintained while performing concurrent hip and knee flexion with alternate legs, the patients are progressed to dynamic exercises. The subsequent program of dynamic hip-strengthening exercises for the lateral rotators and the abductors of the hip predominately target the gluteus medius and maximus. Gluteus medius exercises are done in side lying, with hips and knees flexed, performing hip abduction with external rotation, while maintaining a neutral spinal position by coactivating the transversus abdominus. The patients are instructed to keep both feet together and lift the uppermost knee as high as possible, while concurrently palpating their Anterior Superior Iliac Spine (ASIS) ipsilateral to the side of lower-extremity motion (Fig. 14-a). This is done to ascertain when pelvic rotation occurred. The patients are instructed to stop when movement is felt. In the next stage, performing this exercise with an extended knee will increase the resistance (Fig. 14-b). To isolate the gluteus medius and minimize tensor fascia lata activity, the hip is maintained in a slightly extended position and externally rotated to less than 25°. When patients are able to perform 2 sets of 15 repetitions of the above exercises, they are progressed to the quadruped position to perform hip external rotation/abduction, and hip extension (Fig. 14-c). The demand is further increased by applying an external load using either Theraband tied around the thighs, or a soft weight around the ankles. The amount of weight is increased gradually in 0.5-kg increments. In later stages, the patients are progressed to weight-bearing exercises (Usually after 6 weeks). These exercises include isometric hip abduction performed in weight bearing against a wall, upper-extremity activities performed in a single-leg stance and holding Theraband [65], standing hip abduction using resistance bands placed just proximal to the ankles; and single-leg standing exercise off the side of a 10-cm step (beginning with the free limb lower than the level of the step, patients contract the stance-limb hip abductor muscles and raise the free leg to step level while keeping the stance knee extended) [98], single and double-leg squats and rotating the body medially while maintaining a static lower extremity with relative external rotation at the hip [61, 65].
Fig. 14.
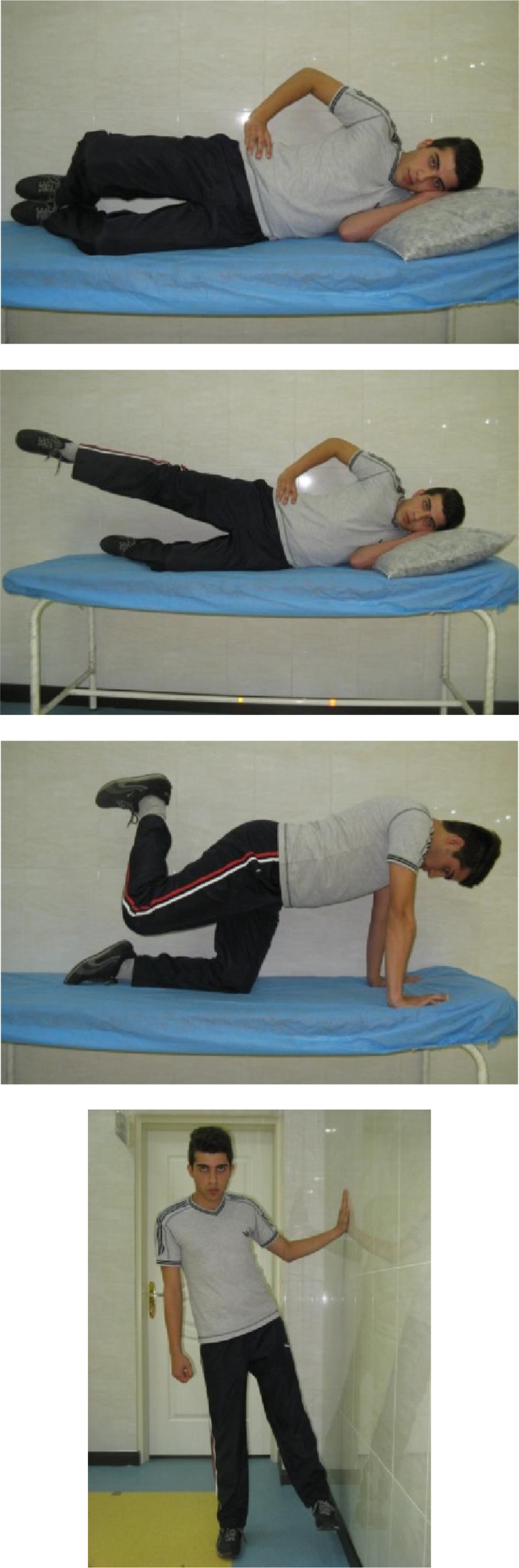
Hip strengthening exercises (a- flexed knee, b- extended knee, c- quadruped and d- weight bearing positions)
Performing at least 2 training sessions a week that involve 2 to 3 sets of between 6 to 15 repetitions per set will lead to considerable increases in muscular strength and endurance [99]. However, for rehabilitation purpose, it is recommended to prescribe strengthening exercises on a daily basis initially, with the number of repetitions and sets controlled by the patients’ level of pain, swelling, and response to exercise. As healing progresses, the muscle can be exercised every second day so the frequency becomes 3 to 4 times per week[61]. Usually, the program should persist for 6-12 weeks [65].
Foot Hyperpronation
Some studies have shown that custom-fitted foot orthoses may considerably improve pain, stiffness, and physical function for patients with patellofemoral pain who display excessive foot pronation [100].
In patients with excessive foot pronation, custom made foot orthoses are prescribed for the subjects after assessment of foot overpronation with FPI-6. These orthosis are fabricated by an expert orthotist with method described by Johnston and Gross [100].
Limb Length Inequality
Intervention for limb length inequality is usually determined by two factors: the amount of the inequality and whether or not the patient is symptomatic. As a general rule, clinicians should exercise caution when undertaking intervention strategies for limb length inequality less than 5 mm [76].
In the case of significant limb length inequality, correction is made with lifts no greater than one-half of difference between limb lengths. An interval of 2 weeks between lift therapy adjustments is considered and each lift increment should not be more than 3 to 6 millimetres, as described by Blustein and D'amico [101].
Generalized Joint Laxity
It has been shown that proprioception and balance exercises may cause decrease in pain and improvement of functional status in patients with benign joint hypermobility syndrome (BJHS) [102].
The recommended exercise program is as the following:
First week: walking backward (30 s), heel walking (30 s), walking on fingertips (30 s), walking with eyes closed (30 s), standing on one extremity (30 s), bending forward and backward on one extremity (eyes open) (30 s), bending forward and backward on one extremity (eyes closed) (30 s), slowly sitting on a high chair and standing up (20 times).
Second week: exercise with rocker bottom wood (2 to 3 min), slowly sitting on a low chair and standing up (10 times), plyometric exercises (passing through a 15 cm height by jumping) (10 times), 8 exercises (slow walk–broad circle, fast walk– broad circle, slow walk–narrow circle, fast walk–narrow circle) (5 times) are added to program.
Third week: exercises with Biomechanical Ankle Platform System (BAPS) board (2–3 min) and minitrampoline jumping exercises (30 times) are added [102].
Patellar Malalignment
In persons with patellar malalignment, patellar taping using the Grelsamer and McConnell technique [103] is included to assist with pain reduction. Nonrigid, hypoallergenic underwrap is used to provide skin protection, and rigid poly cotton zinc-oxide tape is employed for taping corrections. In the case of patellar malalignment, taping corrections are applied in a predetermined order of anterior tilt, medial tilt, glide, and fat pad unloading until the participant's pain is reduced by at least 50%. Participants were taught to apply independently and were instructed to reapply the tape daily and wear the tape during all waking hours for the duration of the trial [104].
Patellar Hypermobility
In the case of patellar hypermobility, the patella is usually tilted first because when the patella is moved in a medial direction, the medial border will move anteriorly indicating relatively tight deep lateral retinacular structures. A medial glide tape is then applied to the patella followed by an external rotation tape applied superiorly and inferiorly to improve the seating of the patella in the trochlea [105].
CONCLUSION
Due to the multifactorial nature of PFPS, numerous risk factors may be implicated in development of PFPS or aggravation of its symptoms. Although many risk factors have been proposed in this context, but only some of them are intrinsic, and among them, just a few may be modifiable. So, it makes sense to investigate these risk factors in each patient with PFPS and correct or modify them with proper interventions, if applicable. Of course, multiple sophisticated methods exist to accurately diagnose or effectively treat the patients. But many of these methods are not available or cost effective in the clinical setting. In this review, we have tried to introduce simple and easy methods appropriate for use in our routine approach, which have been shown as reliable and effective measures in the existing literature. However, more high quality prospective studies are warranted to investigate the effectiveness of this risk factor- based clinical approach [106].
ACKNOWLEDGMENTS
The authors gratefully acknowledge Dr. Masih Shafiei and Mr. Kian Zahedi for their valuable contributions in illustration of assessment tests and exercise programs.
REFERENCES
- 1.Baquie P, Brukner P. Injuries presenting to an Australian sports medicine centre: a 12-month study. Clin J Sport Med. 1997;7:28–31. doi: 10.1097/00042752-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Devereaux MD, Lachmann SM. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br J Sports Med. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154–63. doi: 10.1177/0363546510379967. [DOI] [PubMed] [Google Scholar]
- 4.McConnell J. Management of patellofemoral problems. Man Ther. 1996;1:60–6. doi: 10.1054/math.1996.0251. [DOI] [PubMed] [Google Scholar]
- 5.Powers CM. Rehabilitation of patellofemoral joint disorders: a critical review. J Orthop Sports Phys Ther. 1998;28:345–54. doi: 10.2519/jospt.1998.28.5.345. [DOI] [PubMed] [Google Scholar]
- 6.Wilk KE, Davies GJ, Mangine RE, et al. Patellofemoral disorders: a classification system and clinical guidelines for nonoperative rehabilitation. J Orthop Sports Phys Ther. 1998;28:307–22. doi: 10.2519/jospt.1998.28.5.307. [DOI] [PubMed] [Google Scholar]
- 7.Davis IS, Powers CM. Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat. J Orthop Sports Phys Ther. 2010;40:A1–16. doi: 10.2519/jospt.2010.0302. [DOI] [PubMed] [Google Scholar]
- 8.Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28:480–9. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 9.Cowan SM, Hodges PW, Bennell KL, et al. Altered vastii recruitment when people with patellofemoral pain syndrome complete a postural task. Arch Phys Med Rehabil. 2002;83:989–95. doi: 10.1053/apmr.2002.33234. [DOI] [PubMed] [Google Scholar]
- 10.Cowan SM, Bennell KL, Hodges PW, et al. Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82:183–9. doi: 10.1053/apmr.2001.19022. [DOI] [PubMed] [Google Scholar]
- 11.Waryasz GR, McDermott AY. Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dyn Med. 2008;7:9. doi: 10.1186/1476-5918-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomee R, Grimby G, Svantesson U, et al. Quadriceps muscle performance in sitting and standing in young women with patellofemoral pain syndrome and young healthy women. Scand J Med Sci Sports. 1996;6:233–41. doi: 10.1111/j.1600-0838.1996.tb00097.x. [DOI] [PubMed] [Google Scholar]
- 13.Smith AD, Stroud L, McQueen C. Flexibility and anterior knee pain in adolescent elite figure skaters. J Pediatr Orthop. 1991;11:77–82. doi: 10.1097/01241398-199101000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35:793–801. doi: 10.2519/jospt.2005.35.12.793. [DOI] [PubMed] [Google Scholar]
- 15.White LC, Dolphin P, Dixon J. Hamstring length in patellofemoral pain syndrome. Physiotherapy. 2009;95:24–8. doi: 10.1016/j.physio.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Tyler TF, Nicholas SJ, Mullaney MJ, et al. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34:630–6. doi: 10.1177/0363546505281808. [DOI] [PubMed] [Google Scholar]
- 17.Winslow J, Yoder E. Patellofemoral pain in female ballet dancers: correlation with iliotibial band tightness and tibial external rotation. J Orthop Sports Phys Ther. 1995;22:18–21. doi: 10.2519/jospt.1995.22.1.18. [DOI] [PubMed] [Google Scholar]
- 18.Puniello MS. Iliotibial band tightness and medial patellar glide in patients with patellofemoral dysfunction. J Orthop Sports Phys Ther. 1993;17:144–8. doi: 10.2519/jospt.1993.17.3.144. [DOI] [PubMed] [Google Scholar]
- 19.Hudson Z, Darthuy E. Iliotibial band tightness and patellofemoral pain syndrome: a case-control study. Man Ther. 2009;14:147–51. doi: 10.1016/j.math.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Collado H, Fredericson M. Patellofemoral pain syndrome. Clin Sports Med. 2010;29:379–98. doi: 10.1016/j.csm.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Sanchis-Alfonso V, Rosello-Sastre E, Martinez-Sanjuan V. Pathogenesis of anterior knee pain syndrome and functional patellofemoral instability in the active young. Am J Knee Surg. 1999;12:29–40. [PubMed] [Google Scholar]
- 22.Prins MR, van der Wurff P. Females with patellofemoral pain syndrome have weak hip muscles: a systematic review. Aust J Physiother. 2009;55:9–15. doi: 10.1016/s0004-9514(09)70055-8. [DOI] [PubMed] [Google Scholar]
- 23.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–56. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 24.Barton CJ, Bonanno D, Levinger P, Menz HB. Foot and ankle characteristics in patellofemoral pain syndrome: a case control and reliability study. J Orthop Sports Phys Ther. 2010;40:286–96. doi: 10.2519/jospt.2010.3227. [DOI] [PubMed] [Google Scholar]
- 25.Powers CM, Maffucci R, Hampton S. Rearfoot posture in subjects with patellofemoral pain. J Orthop Sports Phys Ther. 1995;22:155–60. doi: 10.2519/jospt.1995.22.4.155. [DOI] [PubMed] [Google Scholar]
- 26.al-Rawi Z, Nessan AH. Joint hypermobility in patients with chondromalacia patellae. Br J Rheumatol. 1997;36:1324–7. doi: 10.1093/rheumatology/36.12.1324. [DOI] [PubMed] [Google Scholar]
- 27.Kannus P, Niittymaki S. Which factors predict outcome in the nonoperative treatment of patellofemoral pain syndrome? A prospective follow-up study. Med Sci Sports Exerc. 1994;26:289–96. [PubMed] [Google Scholar]
- 28.Dixit S, DiFiori JP, Burton M, et al. Management of patellofemoral pain syndrome. Am Fam Physician. 2007;75:194–202. [PubMed] [Google Scholar]
- 29.Fredericson M, Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85:234–43. doi: 10.1097/01.phm.0000200390.67408.f0. [DOI] [PubMed] [Google Scholar]
- 30.Nijs J, Van Geel C, Van der auwera C, et al. Diagnostic value of five clinical tests in patellofemoral pain syndrome. Man Ther. 2006;11:69–77. doi: 10.1016/j.math.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Souza T. The knee. In: Hyde TE GM, editor. Conservative management of sport injuries. Maryland: Williams & Wilkins; 1997. pp. 394–5. [Google Scholar]
- 32.Reider B. The knee. In: Reider B, editor. The orthopaedic physical examination. 2nd ed. Philadelphia: Elsevier Saunders; 2005. pp. 201–46. [Google Scholar]
- 33.Malanga GA, Andrus S, Nadler SF, et al. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003;84:592–603. doi: 10.1053/apmr.2003.50026. [DOI] [PubMed] [Google Scholar]
- 34.Selfe J, Harper L, Pedersen I, Breen-Turner J, et al. Four outcome measures for patellofemoral joint problems. Part 1: Development and validity. Physiotherapy. 2001;87:507–15. [Google Scholar]
- 35.Van Tiggelen D, Cowan S, Coorevits P, et al. Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37:1099–105. doi: 10.1177/0363546508331135. [DOI] [PubMed] [Google Scholar]
- 36.Witvrouw E, Lysens R, Bellemans J, et al. Open versus closed kinetic chain exercises for patellofemoral pain. A prospective, randomized study. Am J Sports Med. 2000;28:687–94. doi: 10.1177/03635465000280051201. [DOI] [PubMed] [Google Scholar]
- 37.Ageberg E, Zätterström R, Moritz U. Stabilometry and one-leg hop test have high test-retest reliability. Scand J Med Sci Sports. 1998;8:198–202. doi: 10.1111/j.1600-0838.1998.tb00192.x. [DOI] [PubMed] [Google Scholar]
- 38.Rice J, Bennett G, Ruhling R. Comparison of two exercises on VMO and VL EMG activity and force production. Isokinet Exerc Sci. 1995;5:61–7. [Google Scholar]
- 39.Insall J. Current Concepts Review: patellar pain. J Bone Joint Surg Am. 1982;64:147. [PubMed] [Google Scholar]
- 40.Steinkamp LA, Dillingham MF, Markel MD, et al. Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med. 1993;21:438–44. doi: 10.1177/036354659302100319. [DOI] [PubMed] [Google Scholar]
- 41.Morrish GM, Woledge RC. A comparison of the activation of muscles moving the patella in normal subjects and in patients with chronic patellofemoral problems. Scand J Rehabil Med. 1997;29:43–8. [PubMed] [Google Scholar]
- 42.Powers CM, Landel R, Perry J. Timing and intensity of vastus muscle activity during functional activities in subjects with and without patellofemoral pain. Phys Ther. 1996;76:946–55. doi: 10.1093/ptj/76.9.946. [DOI] [PubMed] [Google Scholar]
- 43.Souza DR, Gross MT. Comparison of vastus medialis obliquus: vastus lateralis muscle integrated electromyographic ratios between healthy subjects and patients with patellofemoral pain. Phys Ther. 1991;71:310–6. doi: 10.1093/ptj/71.4.310. [DOI] [PubMed] [Google Scholar]
- 44.Witvrouw E, Werner S, Mikkelsen C, et al. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005;13:122–30. doi: 10.1007/s00167-004-0577-6. [DOI] [PubMed] [Google Scholar]
- 45.Youdas JW, Krause DA, Hollman JH, et al. The influence of gender and age on hamstring muscle length in healthy adults. J Orthop Sports Phys Ther. 2005;35:246–52. doi: 10.2519/jospt.2005.35.4.246. [DOI] [PubMed] [Google Scholar]
- 46.Fredriksen H, Dagfinrud H, Jacobsen V, et al. Passive knee extension test to measure hamstring muscle tightness. Scand J Med Sci Sports. 1997;7(5):279–82. doi: 10.1111/j.1600-0838.1997.tb00153.x. [DOI] [PubMed] [Google Scholar]
- 47.Hopper DCM, Chromiak F, Canini E, et al. Evaluation of the effect of two massage techniques on hamstring muscle length in competitive female hockey players. Phys Ther Sport. 2005;6:137–45. [Google Scholar]
- 48.Greene WB, Heckman JD. The Clinical Measurement of Joint Motion. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1994. [Google Scholar]
- 49.Gabbe B, Bennell K, Wajswelnerc H, et al. Reliability of common lower extremity musculoskeletal screening tests. Phys Ther Sport. 2004;5:90–7. [Google Scholar]
- 50.Thurston A. Assessment of fixed flexion deformity of the hip. Clin Orthop Relat Res. 1982;169:186–9. [PubMed] [Google Scholar]
- 51.Harvey D. Assessment of the flexibility of elite athletes using the modified Thomas test. Br J Sports Med. 1998;32:68–70. doi: 10.1136/bjsm.32.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bartlett MD, Wolf LS, Shurtleff DB, et al. Hip flexion contractures: a comparison of measurement methods. Arch Phys Med Rehabil. 1985;66:620–5. [PubMed] [Google Scholar]
- 53.Dennis RJ, Finch CF, Elliottc BC, et al. The reliability of musculoskeletal screening tests used in cricket. Phys Ther Sport. 2008;9:25–33. doi: 10.1016/j.ptsp.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 54.Magee DJ. Orthopedic Physical Assessment. 5 ed. Philadelphia: W.B. Saunders; 2008. [Google Scholar]
- 55.Herrington L, Rivett N, Munroa S. The relationship between patella position and length of the iliotibial band as assessed using Ober's test. Man Ther. 2006;11:182–6. doi: 10.1016/j.math.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 56.Wang TG, Jan MH, Lin KH, Wang HK. Assessment of stretching of the iliotibial tract with Ober and modified Ober tests: an ultrasonographic study. Arch Phys Med Rehabil. 2006;87:1407–11. doi: 10.1016/j.apmr.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 57.Melchione WE, Sullivan MS. Reliability of measurements obtained by use of an instrument designed to indirectly measure iliotibial band length. J Orthop Sports Phys Ther. 1993;18:511–5. doi: 10.2519/jospt.1993.18.3.511. [DOI] [PubMed] [Google Scholar]
- 58.Reese N, Bandy W. Use of an inclinometer to measure flexibility of the iliotibial band using the Ober test and the modified Ober test: differences in magnitude and reliability of measurements. J Orthop Sports Phys Ther. 2003;33:326–30. doi: 10.2519/jospt.2003.33.6.326. [DOI] [PubMed] [Google Scholar]
- 59.Bennell KL, Talbot RC, Wajswelner H, et al. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44:175–80. doi: 10.1016/s0004-9514(14)60377-9. [DOI] [PubMed] [Google Scholar]
- 60.Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37:232–8. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- 61.Presswood L, Cronin J, Keogh JWL, et al. Gluteus medius: Applied anatomy, dysfunction, assessment, and progressive strengthening. Strength Cond J. 2008;30:41. [Google Scholar]
- 62.Janda V. Muscle Function Testing. London: Butterworths; 1983. [Google Scholar]
- 63.Peterson-Kendall F, Kendall-McCreary E, Geise-Provance P, et al. Muscles testing and function with posture and pain. Baltimore: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 64.Wilson E. Core stability: assessment and functional strengthening of the hip abductors. Strength Cond J. 2005;27:21–3. [Google Scholar]
- 65.Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33:647–60. doi: 10.2519/jospt.2003.33.11.647. [DOI] [PubMed] [Google Scholar]
- 66.Fredericson M, Wolf C. Iliotibial band syndrome in runners: innovations in treatment. Sports Med. 2005;35:451–9. doi: 10.2165/00007256-200535050-00006. [DOI] [PubMed] [Google Scholar]
- 67.Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: a theoretical model. J Orthop Sports Phys Ther. 1987;9:160–5. doi: 10.2519/jospt.1987.9.4.160. [DOI] [PubMed] [Google Scholar]
- 68.Redmond A, Crosbie J, Ouvrier R. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech. 2006;21:89–98. doi: 10.1016/j.clinbiomech.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 69.Redmond A. The foot posture index: reference sheet and data sheet. 1998. [cited 2011 November 20]; Available at: http://www.leeds.ac.uk/medicine/FASTER/z/pdf/FPI-Reference-sheets.pdf. Access date.
- 70.Barton CJ, Levinger P, Crossley KM, et al. Relationships between the Foot Posture Index and foot kinematics during gait in individuals with and without patellofemoral pain syndrome. J Foot Ankle Res. 2011;4:10. doi: 10.1186/1757-1146-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–8. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barber Foss KD, Ford KR, Myer GD, et al. Generalized Joint laxity associated with increased medial foot loading in female athletes. J Athl Train. 2009;44:356–62. doi: 10.4085/1062-6050-44.4.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Boyle KL, Witt P, Riegger-Krugh C. Intrarater and Interrater Reliability of the Beighton and Horan Joint Mobility Index. J Athl Train. 2003;38:281–5. [PMC free article] [PubMed] [Google Scholar]
- 74.Juul-Kristensen B, Rogind H, Jensen DV, et al. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford) 2007;46:1835–41. doi: 10.1093/rheumatology/kem290. [DOI] [PubMed] [Google Scholar]
- 75.Remvig L, Jensen DV, Ward RC. Are diagnostic criteria for general joint hypermobility and benign joint hypermobility syndrome based on reproducible and valid tests? A review of the literature. J Rheumatol. 2007;34:798–803. [PubMed] [Google Scholar]
- 76.Brady RJ, Dean JB, Skinner TM, et al. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003;33:221–34. doi: 10.2519/jospt.2003.33.5.221. [DOI] [PubMed] [Google Scholar]
- 77.Carlson M, Wilkerson J. Are differences in leg length predictive of lateral patello-femoral pain? Physiother Res Int. 2007;12:29–38. doi: 10.1002/pri.351. [DOI] [PubMed] [Google Scholar]
- 78.Gogia PP, Braatz JH. Validity and reliability of leg length measurements. J Orthop Sports Phys Ther. 1986;8:185–8. doi: 10.2519/jospt.1986.8.4.185. [DOI] [PubMed] [Google Scholar]
- 79.Hoyle D, Latour M, Bohannon R. Intraexaminer, interexaminer, and interdevice comparability of leg length measurements obtained with measuring tape and metrecom. J Orthop Sports Phys Ther. 1991;14:263–8. doi: 10.2519/jospt.1991.14.6.263. [DOI] [PubMed] [Google Scholar]
- 80.Song CY, Lin JJ, Jan M, et al. The role of patellar alignment and tracking in vivo: The potential mechanism of patellofemoral pain syndrome. Phys Ther Sport. 2011;12:140–7. doi: 10.1016/j.ptsp.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 81.Biedert RM, Gruhl C. Axial computed tomography of the patellofemoral joint with and without quadriceps contraction. Arch Orthop Trauma Surg. 1997;116:77–82. doi: 10.1007/BF00434106. [DOI] [PubMed] [Google Scholar]
- 82.Salsich GB, Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther. 2007;37:521–8. doi: 10.2519/jospt.2007.37.9.521. [DOI] [PubMed] [Google Scholar]
- 83.Taskiran E, Dinedurga Z, Yagiz A, et al. Effect of the vastus medialis obliquus on the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 1998;6:173–80. doi: 10.1007/s001670050095. [DOI] [PubMed] [Google Scholar]
- 84.Witonski D, Goraj B. Patellar motion analyzed by kinematic and dynamic axial magnetic resonance imaging in patients with anterior knee pain syndrome. Arch Orthop Trauma Surg. 1999;119:46–9. doi: 10.1007/s004020050353. [DOI] [PubMed] [Google Scholar]
- 85.Watson CJ, Propps M, Galt W, et al. Reliability of McConnell's classification of patellar orientation in symptomatic and asymptomatic subjects. J Orthop Sports Phys Ther. 1999;29:378–85. doi: 10.2519/jospt.1999.29.7.378. [DOI] [PubMed] [Google Scholar]
- 86.Powers CM, Mortenson S, Nishimoto D, et al. Criterion-related validity of a clinical measurement to determine the medial/lateral component of patellar orientation. J Orthop Sports Phys Ther. 1999;29:372–7. doi: 10.2519/jospt.1999.29.7.372. [DOI] [PubMed] [Google Scholar]
- 87.Wilson T. The Measurement of Patellar Alignment in Patellofemoral Pain Syndrome: Are We Confusing Assumptions With Evidence? J Orthop Sports Phys Ther. 2007;37:330–41. doi: 10.2519/jospt.2007.2281. [DOI] [PubMed] [Google Scholar]
- 88.Watson CJ, Leddy HM, Dynjan TD, et al. Reliability of the lateral pull test and tilt test to assess patellar alignment in subjects with symptomatic knees: Student raters. J Orthop Sports Phys Ther. 2001;31:368–74. doi: 10.2519/jospt.2001.31.7.368. [DOI] [PubMed] [Google Scholar]
- 89.Kaya D, Doral MN, Callaghan M. How can we strengthen the quadriceps femoris in patients with patellofemoral pain syndrome? Muscles, Ligament and Tendons Journal. 2012;2:25–32. [PMC free article] [PubMed] [Google Scholar]
- 90.Eapen C, Nayak CD, Pazhyaottyil Zulfeequer C. Effect of eccentric isotonic quadriceps muscle exercises on patellofemoral pain syndrome: An exploratory pilot study. Asian J Sports Med. 2011;2:227–34. doi: 10.5812/asjsm.34747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther. 2011;6:112–25. [PMC free article] [PubMed] [Google Scholar]
- 92.Harvie D, O'Leary T, Kumar S. A systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works? J Multidiscip Healthc. 2011;4:383–92. doi: 10.2147/JMDH.S24595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sainz de Baranda P, Ayala F. Chronic flexibility improvement after 12 week of stretching program utilizing the ACSM recommendations: hamstring flexibility. Int J Sports Med. 2010;31:389–96. doi: 10.1055/s-0030-1249082. [DOI] [PubMed] [Google Scholar]
- 94.Winters MV, Blake CG, Trost JS, et al. Passive versus active stretching of hip flexor muscles in subjects with limited hip extension: a randomized clinical trial. Phys Ther. 2004;84:800–7. [PubMed] [Google Scholar]
- 95.Fredericson M, White JJ, Macmahon JM, et al. Quantitative analysis of the relative effectiveness of 3 iliotibial band stretches. Arch Phys Med Rehabil. 2002;83:589–92. doi: 10.1053/apmr.2002.31606. [DOI] [PubMed] [Google Scholar]
- 96.Gajdosik RL, Allred JD, Gabbert HL, et al. A stretching program increases the dynamic passive length and passive resistive properties of the calf muscle-tendon unit of unconditioned younger women. Eur J Appl Physiol. 2007;99:449–54. doi: 10.1007/s00421-006-0366-7. [DOI] [PubMed] [Google Scholar]
- 97.Nakamura M, Ikezoe T, Takeno Y, et al. Effects of a 4-week static stretch training program on passive stiffness of human gastrocnemius muscle-tendon unit in vivo. Eur J Appl Physiol. 2012;112:2749–55. doi: 10.1007/s00421-011-2250-3. [DOI] [PubMed] [Google Scholar]
- 98.Sled EA, Khoja L, Deluzio KJ, et al. Effect of a home program of hip abductor exercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: a clinical trial. Phys Ther. 2010;90:895–904. doi: 10.2522/ptj.20090294. [DOI] [PubMed] [Google Scholar]
- 99.Kraemer WJ, Adams K, Cafarelli E, et al. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34:364–80. doi: 10.1097/00005768-200202000-00027. [DOI] [PubMed] [Google Scholar]
- 100.Johnston LB, Gross MT. Effects of foot orthoses on quality of life for individuals with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2004;34:440–8. doi: 10.2519/jospt.2004.34.8.440. [DOI] [PubMed] [Google Scholar]
- 101.Blustein SM, D'Amico JC. Limb length discrepancy. Identification, clinical significance, and management. J Am Podiatr Med Assoc. 1985;75:200–6. doi: 10.7547/87507315-75-4-200. [DOI] [PubMed] [Google Scholar]
- 102.Sahin N, Baskent A, Cakmak A, et al. Evaluation of knee proprioception and effects of proprioception exercise in patients with benign joint hypermobility syndrome. Rheumatol Int. 2008;28:995–1000. doi: 10.1007/s00296-008-0566-z. [DOI] [PubMed] [Google Scholar]
- 103.Grelsamer RP. The effects of patellar taping on patellofemoral incongruence. A computed tomography study. Am J Sports Med. 2001;29:829. [PubMed] [Google Scholar]
- 104.Cowan SM, Bennell KL, Hodges PW. Therapeutic patellar taping changes the timing of vasti muscle activation in people with patellofemoral pain syndrome. Clin J Sport Med. 2002;12:339–47. doi: 10.1097/00042752-200211000-00004. [DOI] [PubMed] [Google Scholar]
- 105.McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc. 2007;15:95–104. doi: 10.1097/JSA.0b013e318054e35c. [DOI] [PubMed] [Google Scholar]
- 106.Bagheri Sh, Bayat MR, Halabchi F. The effect of 8-week exercise program on patellofemoral pain syndrome. J Res Rehab Sci. 2011;7:357–67. In Persian. [Google Scholar]