Abstract
Purpose
Platelet-rich plasma (PRP) is derived from centrifuging whole blood to obtain a high platelet concentration containing numerous growth factors. Despite its widespread use, there is still a lack of high-level evidence regarding randomized clinical trials assessing the efficacy of PRP in treating ligament injuries. Although there is research showing an improvement in the early stages of healing in the animal model of acute medial collateral ligament (MCL) injury of the knee, there is no strong evidence to support the efficacy of PRP injections for treating MCL lesions in humans.
Case Report
In this report, we present a case of an elite football player, treated with multiple PRP local injections followed by rehabilitation, for a high grade MCL lesion of the knee. He was able to resume training at day 18, painfree, with full range of motion and the ability to complete a functional test based on all sport specific movements. He played matches at 25 days with no residual symptoms or functional deficit. There were no further complaints or recurrences at the 16 months follow up.
Conclusions
On the basis of this report, we can assume that the treatment of high grade acute MCL lesions of the knee with PRP is a promising therapeutic option to be further explored with good quality Randomized Controlled Trials (RCTs).
Keywords: Medial Collateral Ligament (MCL), Platelet Rich Plasma (PRP), Football
INTRODUCTION
The medial collateral ligament (MCL) of the knee is one of the most commonly injured ligaments during sports, particularly those involving valgus knee loading such as soccer, ice hockey and skiing [1–3]. While multiple ligament injuries, including symptomatic chronic MCL laxity, may require surgical treatment, the majority of patients who sustain MCL injuries can achieve pre-injury activity level with conservative treatment alone [4]. High grade lesions will often require only a few weeks of partial immobilization and rehabilitation [5, 6].
Platelet Rich Plasma (PRP) has been proposed as a treatment method to assist regenerative healing processes in acute ligament injuries. In animal studies, there is some evidence that PRP improves healing and mechanical strength in the early stages of acute medial collateral ligament (MCL) injury [7–11]. Hildebrand et al. showed that the application of Platelet Derived Growth Factors BB (PDGF-BB) in the medial collateral ligament of rats increased the ultimate load, energy absorbed to failure, and elongation values compared with a control group [7].
Similarly, Batten at al showed that platelet-derived growth factor has a positive effect on strength characteristics of healing animal ligament when administered in appropriate doses soon after injury. Of note, however, a marked drop in the effectiveness of platelet-derived growth factor was observed when it was administered more than 24 hours after injury [8]. In addition to this initial evidence, more recent researches confirmed that the local administration of different growth factors promotes early steps in ligament healing and the repair of structural properties in a rabbit model [9–11].
If experimental studies on animal ligaments are limited, a recent review identified no prospective studies on PRP application in MCL lesions in humans [12]. Despite its apparent widespread use, to date there has been no case report published on this topic.
We will present an illustrative case which shows clinical and radiological outcomes following multiple PRP injections in an elite football player who sustained a high grade MCL injury.
CASE PRESENTATION
Forty-five minutes into training, a 27 year old National Team football striker (CE) sustained a knee valgus stress trauma, while performing a foot to foot collision with an opponent. Reconstruction of the trauma mechanism revealed an abduction and external rotation of the lower leg. Unable to weightbear, initial physical examination revealed swelling and bone tenderness at the medial femoral condyle. There was minimally painful medial knee joint opening at 25 degrees flexion with valgus stress test but there was no laxity at full knee extension. The rest of the clinical examination of the knee was unremarkable. Initial treatment consisted of rest, ice, compression and elevation. Weight bearing was not allowed and he was placed in a lateral knee hinged brace restricted at 25 degrees of flexion.
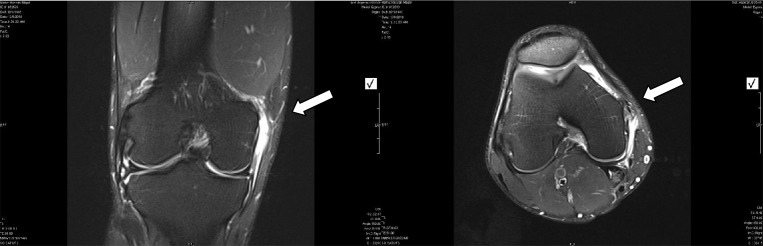
Anteroposterior and lateral X radiographs did not reveal any abnormalities. Magnetic Resonance Imaging (MRI), performed at 24 hours, showed a complete tear of the MCL from its proximal attachment (Fig. 1), a grade III sprain in according with Stoller classification [13].
Fig. 1.
MRI T2 coronal and transversal images, showing a high grade lesion of the proximal insertion of the MCL (arrows)
Thigh setting exercises in isometric modality and straight leg lifts were immediately initiated, together with local anti-inflammatory modalities (electrotherapy, cryotherapy).
Given the severity of the injury, the important return to play time constraints and the availability of PRP technique in our facility, the athlete elected to undergo a treatment of weekly PRP injections. The subject had 27 ml of blood withdrawn from an antecubital vein and the plasma separated into PRP and platelet poor (PPP) fractions, with a commercially available centrifuge based separation system (Biomet Recover™, USA). Using sterile technique, 3 ml of inactivated PRP in a single depot was infiltrated using a 23 gauge at the highest tender point. This caused moderate discomfort for the athlete. The region was then iced for 15 minutes and the patient was discharged and advised to ice for 20 minutes every 1-2 hours on the same day. Post-injection program consisted of keeping a lateral knee hinged brace locked at 25 degrees.
The day after the first injection, the patient reported a mild increase of the pain in the site of the lesion (from 5/10 to 7/10 on a VAS score); however, the pain level returned at pre-injection level by 48 hours. Injections were performed at day 1, 8, 15 post injury and after each infiltration the same adverse pain reactions were reported. In fact, an increase in the pain from 0/10 to 2/10 on a VAS score after both the second and the third injection, resolving in 48 hours, was reported by the patient.
The patient was able to walk pain free at day 3 post injury, so crutches were discontinued. At day 5, CE started range of motion exercises in the swimming pool and, when he reached 90 degree of range of motion (ROM), started progressive resistance training. This part of rehabilitation was performed in an unlocked hinged knee brace. ROM was complete at day 10 and the knee brace was removed. Eccentric strengthening for the popliteus muscle and functional activities were introduced starting with jogging, cutting and other football specific activities. Progression of physiotherapy was based on pain and only symptoms free exercises were allowed.
By day 18, CE was pain free, with full ROM. Quadriceps and hamstrings strength were within 85% of the unaffected leg, as assessed by Isokinetic test. He was able to complete the Illinois and 505 agility tests and to perform all football specific movements with and without the ball (sprinting, accelerations and decelerations, cutting, crosses, passes, shooting, dribbling, heading and one vs one scenario) with no adverse reactions. CE resumed group training at day 18. There was still minimal tenderness and swelling on the medial femoral condyle, together with minimal residual pain free opening of the medial joint with stress in valgus, were still present. However, importantly, CE reported no functional instability. After the completion of a full week of group training without symptoms (in particular absence of pain and subjective feeling of instability), CE played a friendly match at 25 days post injury, without residual symptoms or functional deficit.
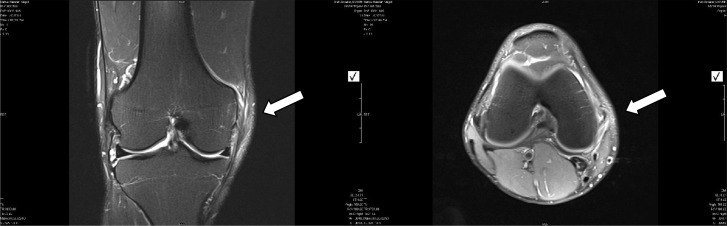
Follow up at 4 weeks showed minimal medial femoral condyle tenderness on palpation and persistent 2-3 mm pain free opening of the medial joint with stress in valgus. Follow up MRI at 5 weeks (Figure 2) showed incomplete healing process of the MCL, with persisting edema over the medial femoral condyle region.
Fig. 2.
MRI T2 coronal and transversal sequences, showing an ongoing process of reparation of the lesion of the proximal insertion of the MCL (arrows)
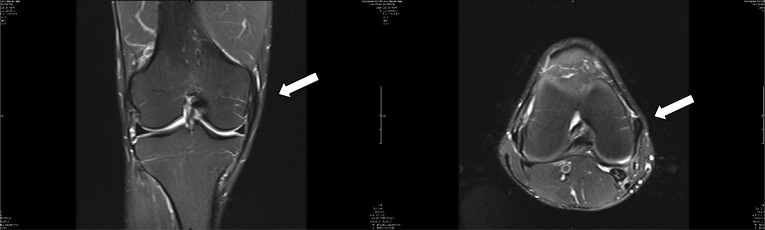
There were no further complaints, complications or recurrences at 16 months follow up and MRI showed reparative changes with no signs of complications (Fig. 3).
Fig. 3.
MRI T2 coronal and transversal sequences, showing a complete process of reparation of the lesion of the proximal insertion of the MCL (arrows)
DISCUSSION
This is the first case reported in the literature on the use of PRP for the treatment of an isolated, non complicated acute MCL lesion. We are aware that many clinicians may already utilize PRP for the treatment of MCL injuries but no cases have been documented in the literature.
The presence of different classification systems in the literature may create confusion on the correct definition of this injury. The Hughston classification system defines this as a grade III lesion, resulting in instability and absolute medial separation at 30 degrees of flexion [11]. As discussed, without dynamic X rays, medial separation cannot be quantified, in order to) identify the opening as a 1+ (0-5 mm), 2+ (5-10 mm or 3+ (more than 10 mm) [14]. In according with Fetto and Marshall Classification System [1], this lesion is defined as a grade II MCL lesion, with laxity present at 30 but not at 0 degrees. Indelicato [15] defined such a lesion as a grade II, due to the limited amount of medial opening with valgus stress at 30 degrees of knee flexion and the presence of a firm end point.
Despite treatment (surgical versus conservative) for isolated complete MCL injury being confused by the conflicting and overlapping classification schemes, nowadays most isolated lesions are treated conservatively[6]. Lesions that may require surgical intervention include chronic MCL injuries (more than 3 months’ duration with high-grade valgus laxity and knee instability) that have failed non-operative treatment, multiple-ligament knee injuries, large bony avulsions, tibial plateau fracture, intra-articular entrapment of the end of a ligament, or anteromedial instability (positive anterior drawer test)[6, 16, 17].
Previous reports showed that an isolated complete tear of the MCL treated conservatively requires a period of rehabilitation of four to eight weeks [18, 19]. In our case, the athlete had an important international football competition starting in four weeks; therefore we decided to apply PRP treatment with the hope of accelerating the recovery. We decided to apply the treatment despite a paucity of clinical evidence for the use of PRP in the treatment of MCL lesions, on the basis of promising animal studies [7, 8].
The clinical evolution following PRP application and rehabilitation was favorable, with the player able to return to football activity without symptoms at day 18 and to play a complete football match at day 25. This seems to be at the lower level of the expected recovery, as discussed above [18, 19].
Functional outcome was excellent, with no pain during football activity. Significantly, residual laxity of the medial joint with valgus stressing was not giving subjective feeling of instability. Despite this, radiological investigations performed before return to play showed an incomplete healing of the ligament. Also clinical investigation, with persistent pain on palpation and swelling at the proximal MCL insertion, was suggesting an ongoing healing process. Thus, since a positive effect of PRP on pain has been reported in patellar human tendinopathy [20], it may have happened that PRP acted on the pain, allowing an earlier return to sport activity without accelerating the healing process. Since no tests were performed on the biological and strength characteristics of healing ligament, this possibility cannot be excluded.
At 16 months follow up there were no recurrences, complications or further complaints, with the player returning to the same level of competition. This may indicate that PRP may be considered a safe therapeutic technique on a short term evaluation.
A single case report, representing Level IV evidence, allows no clear indication as to the benefits of the PRP injection to be gleaned from the pure clinical outcome, other than that it was satisfactory.
Finally, we have to highlight how, since there is no substantial evidence for the volume, concentration of platelets and frequency of application of PRP, our treatment regime was speculative and further research is required in order to establish protocols.
CONCLUSION
The use of PRP technology in the management of ligament lesions has some support from in vitro and animal studies. While its clinical use in humans is still early, it might have the potential be a viable tool for the practitioner and the athlete as this case report shows.
Many questions remain regarding the use of PRP in acute MCL injury, including its mode of action, optimal dosing, optimal timing of application, long term efficacy, relevance of platelet and GF concentrations, the need for preapplication activation and safety profiles. Thus the technique requires further evaluation of its indications, efficacy and safety before any comprehensive conclusions can be drawn.
ACKNOWLEDGMENTS
Written informed consent was obtained from the patient for publication of this report.
REFERENCES
- 1.Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop. 1978;132:206–18. [PubMed] [Google Scholar]
- 2.Peterson L, Junge A, Chomiak J, et al. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28:S51–7. doi: 10.1177/28.suppl_5.s-51. [DOI] [PubMed] [Google Scholar]
- 3.Lorentzon R, Wedren H, Pietila T. Incidence, nature, and causes of ice hockey injuries. A three-year prospective study of a Swedish elite ice hockey team. Am J Sports Med. 1988;16:392–6. doi: 10.1177/036354658801600415. [DOI] [PubMed] [Google Scholar]
- 4.Reider B, Sathy MR, Talkington J, et al. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22:470–7. doi: 10.1177/036354659402200406. [DOI] [PubMed] [Google Scholar]
- 5.Jones RE, Henley MB, Francis P. Non operative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop. 1986;213:137–140. [PubMed] [Google Scholar]
- 6.Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77–90. [PMC free article] [PubMed] [Google Scholar]
- 7.Hildebrand KA, Woo SL-Y, Smith DW, et al. The effects of platelet derived growth factor-BB on healing of the rabbit medial collateral ligament: an in vivo study. Am J Sports Med. 1998;26:549–54. doi: 10.1177/03635465980260041401. [DOI] [PubMed] [Google Scholar]
- 8.Batten ML, Hansen JC, Dahners LE, et al. Influence of dosage and timing of application of platelet derived growth factor on early healing of the rat medial collateral ligament. J Orthop Res. 1996;14:736–41. doi: 10.1002/jor.1100140509. [DOI] [PubMed] [Google Scholar]
- 9.Yoshioka T, Kanamori A, Washio T, et al. The effects of plasma rich in growth factors (PRGF-Endoret) on healing of medial collateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. 2012 Apr 13; doi: 10.1007/s00167-012-2002-x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 10.Ueshima K, Kitaoka K, Nakase J, et al. Promotion of rabbit ligament healing by local delivery of hepatocyte growth factor. J Orthop Sci. 2011;16:451–7. doi: 10.1007/s00776-011-0101-z. [DOI] [PubMed] [Google Scholar]
- 11.Saiga K, Furumatsu T, Yoshida A, et al. Combined use of bFGF and GDF-5 enhances the healing of medial collateral ligament injury. Biochem Biophys Res Commun. 2010;402:329–34. doi: 10.1016/j.bbrc.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 12.Paoloni J, De Vos RJ, Hamilton B, et al. Platelet-rich plasma treatment for ligament and tendon injuries. Clin J Sport Med. 2011;21:37–45. doi: 10.1097/JSM.0b013e31820758c7. [DOI] [PubMed] [Google Scholar]
- 13.Stoller DW, Tirman PF, Bredella MA. Diagnostic Imaging Orthopaedics. Salt Lake City, Utah: Amirsys; 2004. Knee; pp. 54–7. [Google Scholar]
- 14.Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76:1328–44. doi: 10.2106/00004623-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Indelicato P. Isolated medial collateral ligament injuries of the knee. J Am Acad Ortho Surg. 1995;3:9–14. doi: 10.5435/00124635-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Azar FM. Evaluation and treatment of chronic medial collateral ligament injuries of the knee. Sports Med Arthrosc. 2006;14:84–90. doi: 10.1097/01.jsa.0000212311.77817.c8. [DOI] [PubMed] [Google Scholar]
- 17.Mook WR, Miller MD, Diduch DR, et al. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946–57. doi: 10.2106/JBJS.H.01328. [DOI] [PubMed] [Google Scholar]
- 18.Derscheid GL, Garrick JG. Medial collateral ligament injuries in football. Nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9:365–8. doi: 10.1177/036354658100900605. [DOI] [PubMed] [Google Scholar]
- 19.Holden DL, Eggert AW, Butler JE. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11:340–4. doi: 10.1177/036354658301100511. [DOI] [PubMed] [Google Scholar]
- 20.Gosens T, Den Oudsten BL, Fievez E, et al. Pain and activity levels before and after platelet-rich plasma injection treatment of patellar tendinopathy: a prospective cohort study and the influence of previous treatments. Int Orthop. 2012;36:1941–6. doi: 10.1007/s00264-012-1540-7. [DOI] [PMC free article] [PubMed] [Google Scholar]