Dear Editor,
Although epidemic, vitamin D deficiency is still under-diagnosed.[1] In 30% of patients it can present as proximal muscle weakness before the biochemical signs of vitamin D deficiency appear leading to unnecessary investigative work up. So in at-risk individuals it should be kept as one of the differential diagnosis for muscle weakness, as the condition is reversible and easily treated with vitamin D and calcium supplementation.
A 33-year-old black female, was referred to our hospital because of elevated Creatinine kinase. She has been having difficulty in getting up from chair over last couple of months. She also complained of having generalized aches and pains while doing her routine work. She is a mother of four children and has been on orlistat and following a diet for losing weight. On physical examination, muscle bulk and muscle tone was normal; the muscle power was 3/5 in the flexors and extensors of the hip and shoulder. There was no other neurological deficit.
Laboratory parameters [Table 1] revealed hypochromic microcytic anemia due to severe iron deficiency. vitamin B12, thyroid function tests, erythrocyte sedimentation rate, serum magnesium, potassium and phosphate levels were normal. A search for inflammation or other causes of myopathy was negative which included an auto-antibody screen such as ANA, Rheumatoid factor and anti JO-1 antibodies. Serum ionized calcium was low with normal alkaline phosphatase but borderline high Parathyroid hormone (PTH) levels. Her serum 25-hydroxy vitamin D was extremely low (4 ng/ml, reference range > 30-100). Levels of Creatinine Kinase, Aldolase, myoglobin and Lactate Dehydrogenase (LDH) were elevated. Electromyography was also normal. To rule out myositis, muscle biopsy of the left deltoid was done which showed non-specific minimal muscle fiber atrophy [Figure 1a–c]. Keeping in consideration her risk factors which included Orlistat intake, less sun exposure, high melanin pigment, and poor dietary intake diagnosis of proximal myopathy due to severe vitamin D Deficiency associated with rhabydomyolsis was made based on the clinical and biochemical findings. Medical treatment was initiated, and orlistat was withdrawn. Her serum biochemistry values along with proximal myopathy and muscle tenderness improved on follow-up in 2 months.
Table 1.
Laboratory parameters
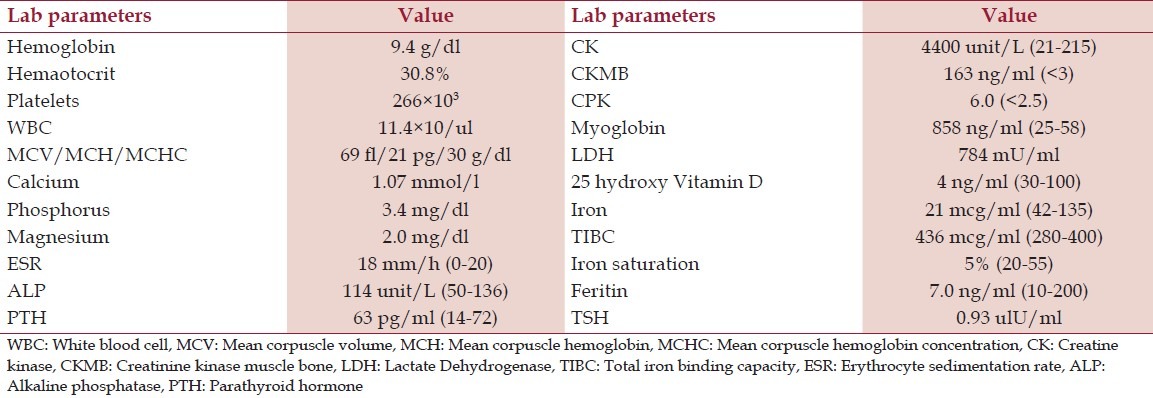
Figure 1.
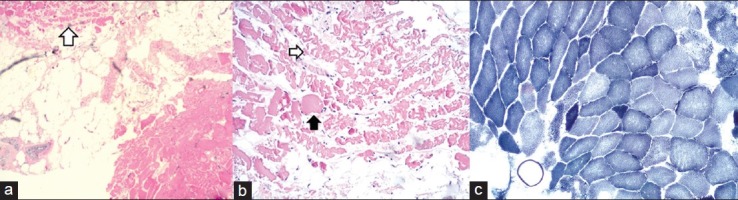
(a) A small cluster of atrophic cells (small arrow) with some more normal myocytes in the bottom right. They are separated by fat (×4). (b) Centered on the atrophic fibers which are ragged and irregular (small white arrow). One myocyte (small black arrow) is more normal with a geometric outline and solid cytoplasm (×10). (c) The NADH (Nicotinamide Adenine Dinucleotide) stain shows a couple of cells with significantly darker staining than their neighbors and are also small in comparison. These are the atrophic cells. There are no nflammatory cells
Vitamin D deficiency is defined as a 25-hydroxy vitamin D level of less than 20 ng/ml and a level between 21 ng and 29 ng/ml is considered as relative insufficiency.[2] Lack of sunlight exposure, higher skin melanin content, dietary insufficiency of vitamin D and Orlistat led to vitamin D deficiency in our patient. Orlistat affects body fat as well as interfere with absorption of vitamin D. McDuddie demonstrated that mean vitamin D levels were significantly reduced compared with baseline after 1 month of Orlistat, despite multivitamin supplementation including vitamin D.[3]
In 30% it can present mainly as proximal myopathy. A serum 25-hydroxy vitamin D level below 20 ng/ml causes increased body sway and a level below 10 ng/ml leads to difficulties in rising from a chair, inability to ascend stairs and pain and discomfort due to muscular effort as in our patient.[4] Clement et al. highlighted the importance of vitamin D in patients with multiple myeloma, and showed that it is common and can cause generalized musculoskeletal pain and increase the risk of falls in such patients yet it often goes unrecognized.[5] Furthermore, Glucecek et al demonstrated that hypercholesterolemic patients with vitamin D deficiency are intolerant to statins due to myositis-myalgia more tahn general population without deficiency. And after supplementation with vitamin D, statin could be successfully reintroduced in 90% of patients without having recurrent myositis-myalgia, reflecting a reversible interaction between vitamin D and statins on skeletal muscles.[6] Basis of this hypothesis is skeletal muscle contains vitamin D receptors that modulate various transcription factors in muscle cells,[7] mediating muscle cell proliferation and differentiation into mature type II muscle fibers. Furthermore, vitamin D is responsible for the active transportation of calcium into sarcoplasmic reticulum necessary for sarcomeric muscular contraction which has been shown to play a role in maintenance of postural equilibrium.[8]
The assessment of serum 25 OHD (25 hydroxy vitamin D) is the only reliable test as clinical myopathy may be present before the development of biochemical signs (low calcium and increased Alkaline phosphatase) of bone disease.[2] Elevation of muscle enzyme creatinine kinase level has been reported in a minority of patients with vitamin D related muscle weakness,[9] but was significantly elevated in our patient pointing towards the significant muscle damage. Muscle biopsy is not indicated and if done, shows non-specific muscle fiber atrophy and no signs of inflammatory reaction. The ultimate evidence of the diagnosis rests on the response to therapy. Proximal muscle strength strikingly improves when 25-hydroxy vitamin D levels increases from 4 ng to 16 ng/ml and continues to improve as the levels increase to more than 40 ng/ml.[10]
We conclude that in patients with proximal muscle weakness, finding a typical constellation of biochemical alterations should limit additional costly and invasive neuromuscular workup for other causes of muscle dysfunction. In such a patient, an early therapeutic trial of vitamin D is warranted. A lack of objective improvement in proximal muscle strength after about a month on an adequate dosage of vitamin D indicates a need for reevaluation of the diagnosis.
References
- 1.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–73. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 2.Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxy vitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84:18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 3.McDuffie JR, Calis KA, Booth SL, Uwaifo GI, Yanovski JA. Effects of orlistat on fat-soluble vitamins in obese adolescents. Pharmacotherapy. 2002;22:814–22. doi: 10.1592/phco.22.11.814.33627. [DOI] [PubMed] [Google Scholar]
- 4.Al-Said YA, Al-Rached HS, Al-Qahtani HA, Jan MM. Severe proximal myopathy with remarkable recovery after vitamin D treatment. Can J Neurol Sci. 2009;36:336–9. doi: 10.1017/s0317167100007083. [DOI] [PubMed] [Google Scholar]
- 5.Clement Z, Ashford M, Sivakumaran S. Vitamin D deficiency in a man with multiple myeloma. N Am J Med Sci. 2011;3:469–71. doi: 10.4297/najms.2011.3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glueck CJ, Abuchaibe C, Wang P. Symptomatic myositis-myalgia in hypercholesterolemic statin-treated patients with concurrent vitamin D deficiency leading to statin intolerance may reflect a reversible interaction between vitamin D deficiency and statins on skeletal muscle. Med Hypotheses. 2011;77:658–61. doi: 10.1016/j.mehy.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Simpson RU, Thomas GA, Arnold AJ. Identification of 1,25-dihydroxy vitamin D3 receptors and activities in muscle. J Biol Chem. 1985;260:8882–91. [PubMed] [Google Scholar]
- 8.Pfeifer M, Begerow B, Minne HW. vitamin D and muscle function. Osteoporos Int. 2002;13:187–94. doi: 10.1007/s001980200012. [DOI] [PubMed] [Google Scholar]
- 9.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of vitamin D on falls: A meta-analysis. JAMA. 2004;291:1999–2006. doi: 10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]
- 10.Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, et al. Higher 25-hydroxy vitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged ≥ 60 y. Am J Clin Nutr. 2004;80:752–8. doi: 10.1093/ajcn/80.3.752. [DOI] [PubMed] [Google Scholar]


