Abstract
Objective
The authors report the outcomes of a community-based, barber health adviser pilot intervention that aims to develop customized educational materials to promote knowledge and awareness of prostate cancer (CaP) and informed decision making about prostate cancer screening (PCS) among a predominantly African American clientele.
Method
First, the authors implemented a series of learner verification processes with barbershop clients (n = 15) to adapt existing CaP health promotion materials. Following intervention implementation in the barbershop, they conducted structured surveys with barbershop clients (n = 40) to evaluate the intervention.
Results
Findings from the posttest showed both a significant increase in barbershop clients' self-reported knowledge of CaP and in the likelihood of discussing PCS with a health care provider (p < .001). The client's cultural model of CaP risk factors revealed cultural consensus (eigenratio = 3.3) and mirrored the biomedical model. All clients surveyed reported positively on the contents of the educational materials, and more than half (53%) had discussed CaP at least twice with their barber in the last month.
Conclusion
Based on the pilot results, the barber-administered intervention was an appropriate and viable communication channel for promoting CaP knowledge and awareness in a priority population, African American men.
Keywords: PSA testing, general health and wellness, health education, men of color, special populations
Introduction
Prostate cancer (CaP) remains the second most prevalent cancer in men in the United States, with an estimated 192,280 new cases and 27,360 deaths occurring in 2009 (American Cancer Society, 2009). Although the incidence and mortality rates for CaP continue to decline for all U.S. men, African American men experience a disproportionate burden of disease. From 2000 and 2004, the incidence rate was 58% higher for African Americans, and the mortality rate was 2.4 times higher compared with Whites. A primary contributing factor to this racial disparity is late-stage diagnosis, often the outcome of low levels of awareness, knowledge, and access to prostate cancer screening (PCS) among African American men (Jones, Underwood, & Rivers, 2007; Jones & Wenzel, 2005; Richardson, Webster, & Fields, 2004). Current recommendations encourage men to discuss with their health care providers the risks, benefits, side effects, and questions surrounding PCS and the potential consequences of the decision, commonly referred to as the informed decision-making process (Briss et al., 2004; Lim & Sherin, 2008; Smith, Cokkinides, & Brawley, 2008; U.S. Preventive Services Task Force, 2002, 2008). New research findings highlighted in the popular media have the potential to confuse the public about the benefits of PCS. Examples include the ongoing discoveries of novel biomarkers for risk assessment and detection of CaP (Couzin, 2009) and the recent interim results of two large randomized clinical trials on prostate-specific antigen (PSA) testing, wherein the U.S. trial showed no benefits and the European trial indicated small incremental benefits for the reduction of CaP deaths when compared with the greater risk of overdiagnosis (Andriole et al., 2009; Schroder et al., 2009). To ensure all men, particularly those at increased risk, have the pertinent information needed to engage in the informed decision-making process, there is a critical need to explore efficacious and novel communication channels to disseminate reliable and credible information.
The barbershop represents an accessible setting for many African Americans, whereby customized information can be disseminated in a trusted environment. Therefore, some researchers recommend concentrating health promotion efforts on CaP for African American men in valued community venues, such as the barbershop. Pilot studies have concluded the barbershop is a culturally relevant, feasible, and appropriate venue for community-based CaP education programs and barbers are ready participants (Allen, Kennedy, Wilson-Glover, & Gilligan, 2007; Forrester-Anderson, 2005; Fraser et al., 2009; Hart & Bowen, 2004; Hart et al., 2008). Drawing from prior research studies and public health outreach initiatives in this area, we conceived of the Barbers Against Prostate Cancer pilot study.
The overall goals of this study were to develop customized educational and training materials for African Americans for use in a barbershop-based intervention purposed to promote CaP knowledge and informed decision making for PCS and to test the feasibility of using barbers trained as barber health advisers to deliver the intervention. Lay health adviser programs have been frequently implemented with minority and underserved women and Hispanic migrant farmworker populations, but have been less commonly used with target populations of men, in this case in the context of the barbershop (Coughlin & Wilson, 2002; Fernandez, Gonzales, Tortolero-Luna, Partida, & Bartholomew, 2005; Larkey, 2006; Luque et al., 2007; Rhodes, Foley, Zometa, & Bloom, 2007). The original study aims of the pilot project were (1) to assess the feasibility of training barbers to disseminate relevant CaP messages and (2) to provide systematic training to barbers to prepare them to deliver CaP education in the community setting. This article evaluates the receipt of the CaP messages from survey results with barbershop clients to address Aim 1. The results from Aim 2 have been discussed elsewhere (Luque et al., in press). Moreover, this article details the process of developing the educational materials used by the barbers to educate clients rather than the prior materials developed to educate the barbers in the barber training program.
This article outlines (a) the process of developing and adapting culturally and linguistically appropriate educational materials customized to the barbershop setting and (b) the postintervention survey results conducted with barbershop clients to assess potential changes in knowledge, attitudes, beliefs, and intentions related to CaP and PCS as a result of exposure to the barbershop-based education program intervention. The project was implemented based on the underlying tenets of community-based participatory research (CBPR), in partnership with a local community health agency, which worked with the inner-city African American population, and were engaged in multiple phases of the research project (Israel, Schulz, Parker, & Becker, 1998).
Method
Recruitment Strategy
Barbershops and barbers
Collaboratively with the community health agency, two initial barbershops servicing an older African American clientele were identified based on the inclusion criteria for the study. Through a snowball sampling strategy, two additional barbershops were recruited into the study. The final sample for this study consisted of four barbershops, with two barbers from each barbershop participating in the entire study (n = 8 barbers).
Barbershop clients
Clients recruited for the formative research (learner verification) and postintervention surveys were drawn from a convenience sample. Eligibility criteria for clientele participation included the following: (a) men aged 40 years and older, (b) African American, (c) no history of CaP, and (d) previous customer of the barbershop. Fifteen African American male barbershop clients from two of the four barbershops participated in part of the formative research processes, by answering a learner verification survey on draft versions of our educational brochure, and the results were used to develop our core set of educational materials (brochure and poster). On completion and implementation of the education intervention by the 8 barbers, 40 African American male barbershop clients (10 from each barbershop) were recruited to complete a postintervention survey in this posttest-only study design to assess receipt and impact of the educational messages from the clients' perspective.
Setting
The four barbershops in this study were located in east Tampa, Florida. There are more than 30 barbershops in east Tampa, servicing primarily an African American clientele. Fifty-seven percent of the residents in east Tampa identify as African American with a median household income of $27,118, and the district is characterized by an unemployment rate above the national average; however, the area has recently been the focus of major redevelopment activities to revitalize businesses and infrastructure (Briscoe & McClain, 2000; U.S. Census Bureau, 2000).
Adaptation of Prostate Cancer Materials
Members of the research team had previously developed a set of CaP education materials (brochure, video, and flip-chart) as part of toolboxes tailored for African American men for dissemination in a variety of community venues. These “tools” formed the basis for our current intervention (Meade, Calvo, Rivera, & Baer, 2003). Whereas these prior materials focused primarily on early detection and screening, the materials were adapted and customized for the barbershop setting to include informed decision-making verbiage reflective of current guidelines for PCS. As part of this process, learner verification techniques were used to verify that specific content or format features of the message were consistent with the characteristics of the intended audience (Doak, Doak, & Meade, 1996). The questions aimed to assess elements such as acceptability, attraction, and comprehension. For example, participants were asked to think about the images, colors, format, and overall feel and persuasiveness of the brochure and to answer questions specific to the anatomical diagrams, quotations and text, understanding of terminology, and appropriateness of photographs. After interviewing eight clients, we reached saturation (no new information obtained) and then revised our materials for a second iterative stage, following procedures described in Doak et al. (1996; see also Morse, 1995). As part of the first iteration, participants were also asked to list words that they associated with cancer, to list risk factors they believed caused prostate cancer, and to describe the location and function of the prostate gland. Content validity of the educational brochure was also evaluated by a group of four medical experts—a general practitioner, an urologist, a genitourinary surgeon, and a behavioral scientist specializing in prostate and colorectal cancer—to verify the scientific accuracy. On the advice of one of the medical experts, we added the sentence, “Your chance of getting prostate cancer increases if you have a family history of the disease, such as a brother or father.” The final set of educational materials used by the barbers in the lay health adviser (LHA) intervention included a brochure, poster (modified from the brochure, refer to Figure 1), DVD (produced by another cancer center targeted to African Americans), plastic prostate model (exemplifying the normal and abnormal gland), barber talking points card (to assist in their conversations with clients, refer to Table 1), and list of community resources for follow-up.
Figure 1. Barbers Against Prostate Cancer Education Poster.
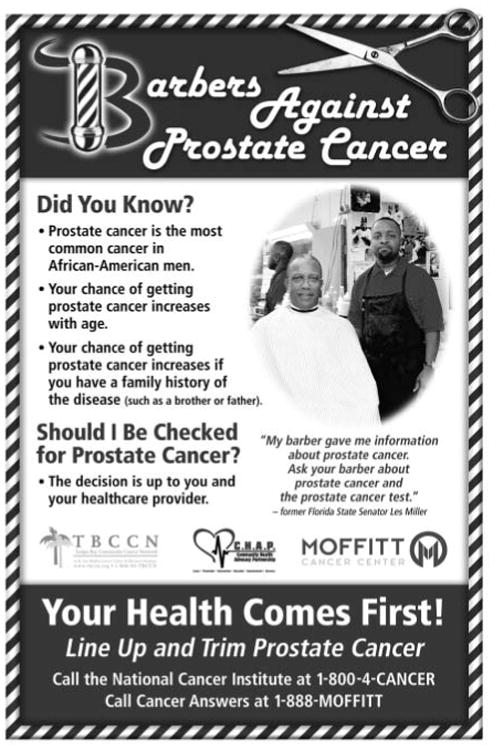
Table 1. Barbers Against Prostate Cancer Talking Points.
| What is cancer? |
| Cancer cells are abnormal cells that can grow to form tumors |
| What is the prostate? |
| Prostate is the size of a walnut and makes sperm |
| What is prostate cancer? |
| Growth of abnormal cancer cells in the prostate |
| What are the main risk factors for prostate cancer? |
| Age, having a first-degree relative with prostate cancer (such as a brother or father), African American |
| What are the tests for prostate cancer? (these two tests are used together) |
| PSA—Prostate-specific antigen, blood test |
| DRE—or the “finger test” |
| What are some of the informed decisions relating to prostate cancer? |
| Understanding the nature and risks of prostate cancer |
| Understanding the benefits, harms and alternatives to Screening |
| Participating in decision making with your doctor or health care provider |
| Making a decision consistent with preferences and values |
| Possibly deciding to make the decision about it later |
| What are the patient benefits of shared decisions relating to prostate cancer? |
| Takes an active role in his health care |
| Becomes better informed |
| Chooses the option most consistent with his personal preferences |
| Where are the local resources to find out more about prostate cancer? |
| Community Health Advocacy Partnership |
| Call Cancer Answers |
Training Program and CBPR Approach
A total of eight barbers completed more than 10 contact hours of training to administer the educational intervention with the adapted and customized educational materials. The training was a combination of didactic instruction, interactive group exercises, and team building, congruent with Empowerment Education learning approaches (Freire, 1970; Wallerstein & Bernstein, 1988). The community health agency partners, together with members of the research team and a local urologist, provided onsite training in the agency's facilities and in each of the four barbershops to allow the barbers to work through the CaP curriculum, as well as practice and gain familiarity with the intervention. In addition, congruent with the tenets of CBPR, the community health agency partners met with the researchers during grant preparation and study design conception, secured letters of support from the barbershops, monitored the barbers throughout the pilot project with shop visits, attended project meetings, worked with local television stations and African American newspapers for local coverage, contributed to public forums and professional conference presentations, received National Institutes of Health human subjects protection training, and facilitated a focus group with the barbers as part of the postintervention evaluation. The development of the barber training program, curriculum, and evaluation is described elsewhere (Luque et al., in press; Meade, Menard, Luque, Martinez-Tyson, & Gwede, 2009).
Postintervention Survey
To assess the receipt and impact of the intervention, a postintervention survey was developed, pilot-tested with available barbers and volunteer clients in the shops, and then administered to 10 clients in each barbershop, for a total of 40 completed surveys. The 51-item postintervention survey was developed based on the current literature, questions we developed to receive feedback on the educational materials, a ranking exercise of CaP risk factors with items generated from free-listing in the learner verification survey and the scientific literature, and items from the National Cancer Institute Health Information National Trends Survey (HINTS) on the domain of PSA testing history (Hart & Bowen, 2004; Hess et al., 2007; Nelson et al., 2004). Four main areas in the questionnaire collected data on (a) barbershop patronage, (b) receipt of various types of educational materials from the barber and behavioral intentions with PCS related to the information received, (c) PSA testing history and discussions with providers about the PSA, and (d) demographic information. The response rate for the completion of the postintervention surveys was 75% (40 surveys completed out of 53 clients approached).
The primary outcome variables measured in the postintervention survey were the likelihood of discussing CaP with a health care provider after receiving educational materials from their barber and participants' self-reported knowledge scores of CaP. Responses to likelihood of discussing CaP with a health care provider were rated on a 4-point Likert-type scale ranging from very unlikely to very likely. Knowledge scores were rated on a 5-point Likert-type scale ranging from low to high. Other outcome variables of interest were the effect of the intervention on feelings of worry related to CaP, rated on a 4-point Likert-type scale ranging from not worried to very worried, and projected PCS modality intention (PSA, digital rectal examination [DRE], or both).
Analysis
Frequency distributions of sociodemographic variables and question item responses were analyzed. Standard statistical techniques were used, including the Fisher's exact test for categorical data and the nonparametric Wilcoxon signed ranks test for continuous data performed at a two-sided α = .05 level using SPSS, Version 17.0. The analysis of the rank order question of 15 items employed cultural consensus analysis, a measurement model that calculates the level of shared knowledge within groups and solves for individual elements of cultural competency as well as the average level of competency for the group (Romney, Weller, & Batchelder 1986; Weller & Romney, 1988). Conducting a principal components analysis of the correlation matrix among participants produces the solution for individual estimates of competency. The convention for indicating a high level of sharing of the cultural model is predicated by calculating a ratio of the first to second eigenvalue that is greater than 3.0. Positive results from this analysis would indicate that the clients agreed on the rank order of CaP risk factors after receiving the barber education, suggesting a shared knowledge domain. Three open-ended items generated minimal qualitative data for thematic analysis, and these were analyzed by coding responses and searching for patterns in the responses as well as confirmatory thematic analysis among members of the research team.
Results
Adaptation of Prostate Cancer Materials
Before beginning the learner verification questions on the educational brochure, the clients were asked to think about cancer and to name three things which came to mind. Many responses included words with negative connotations, such as debilitating, detrimental, bad, death, dying, neglect, sickness, worry, and long suffering. During the learner verification survey, when asked to explain the definition of the prostate gland, 33% of the men did not know the function and/or location of the gland. Therefore, in the final brochure, there was a clear anatomical diagram describing the prostate. When asked to explain what the word prostate gland meant to them, some responses included too low a sperm count could kill you, swelling, and trouble. Only 13% of the respondents correctly identified the prostate as being a vital part of the reproductive system.
The clients' responses to the learner verification items ensured the terms and recommendations were understood and the tone, key messages (“the decision is up to you and your healthcare provider”), photos, anatomical diagrams, layout, and color scheme were culturally appropriate. In addition to adopting or adapting verbiage on informed decision making from the CDC's “Prostate Cancer Screening Decision Guide for African Americans,” major changes from the previous toolbox brochure included pictures, colors, fonts, and style format. In addition to photos of participating barbers, the brochure cover featured a well-known and highly regarded civic leader. Other specific changes to the revamped brochure included changing a photo of an anonymous man to a photo of the barbers, moving the header, “Your Health Comes First! Line Up and Trim Prostate Cancer” from the top to the bottom of the brochure cover for better emphasis, and changing the words prostate cancer to prostate test in the phrase to enhance reading ease, “Ask yourself these questions about the prostate test.” The primary educational message conveyed in the brochure was that men should discuss PCS with their health care provider and make an informed decision. The resulting educational brochure and accompanying poster was a culmination of comments and recommendations from the target audience—African American men aged more than 40 years—and verified by medical experts for scientific accuracy.
Sociodemographic Characteristics
Table 2 describes the sociodemographic characteristics of clients participating in the postintervention surveys. The clients represented 15 different zip codes in Hillsborough County, with the highest proportion residing in east Tampa (20%, lower-income area) and north Tampa (18%, higher-income area). The mean age of participants was 53 years (ranging from 40 to 73 years). The mean for education level, measured by the number of years of schooling, was 14 years (ranging from 10 to 18 years). Fifty percent of the participants reported an annual household income of less than $70,000. Moreover, participants reported a high rate of private insurance coverage (78%), with a smaller percentage reporting Medicare or Medicaid coverage (15%). Seven percent reported having no health insurance coverage.
Table 2. Demographic Characteristics of African American Barbershop Clients (N = 40).
| Characteristic | Percentage (n) |
|---|---|
| Age (years) | |
| 40-49 | 45 (18) |
| 50-59 | 38 (15) |
| 60-73 | 17 (7) |
| Education, n (%) | |
| Some high school | 5 (2) |
| High school graduate | 25 (10) |
| Some college | 25 (10) |
| Bachelors degree or above | 45 (18) |
| Marital status, n (%) | |
| Single | 27 (11) |
| Married | 63 (25) |
| Divorced | 10 (4) |
| Household income, n (%) | |
| Salary level $0-$29,000 | 10 (4) |
| Salary level $30,000-$49,000 | 20 (8) |
| Salary level $50,000-$69,000 | 20 (8) |
| Salary level $70,000 and above | 50 (20) |
| Health insurance, n (%) | |
| Private health insurance | 78 (31) |
| Public health insurance (e.g., Medicare, Medicaid) | 15 (6) |
| Zip codes, n (%) | |
| Residence in main east Tampa zip code | 20 (8) |
| Residence in same zip code as study barbershops | 27 (11) |
Postintervention Survey Data
The majority of the clients surveyed (55%) visited the barbershop every 2 weeks and spent approximately 45 minutes per visit. Barbershop loyalty was very high, with the majority (90%) attending the same barbershop throughout the year. In one of the open-ended questions, we asked clients to think about what they knew about CaP before the barber introduced them to the topic. Less than half of the participants (43%) provided any detail about their knowledge of PCS, or “the test,” in their nomenclature. One participant responded,
my doctor explained it to me, the ups and downs, the treatment, what it does to you, yes it was a concern, it could kill you, my first one was at 40 years old, I get it every 5 years.
Another client characterized preventive screening tests as similar to “maintenance on an automobile.” There was some variation about the length of the testing interval and the age to begin testing among the clients. One common theme was the knowledge of the association between African American men and mortality from CaP. For example, one participant responded, “prostate cancer is one of the leading cancers in Black men, it is worth looking more into it.”
Participants reported that the materials were easy to understand, had an attractive color scheme, and featured familiar faces printed on the materials. Most participants (78%) reported that the educational materials increased their knowledge of CaP. All barbershop clients surveyed reported positively on the contents of the brochure and poster, and more than half (53%) had discussed CaP at least two times with their barber in the last month or had received some other form of health-related advice from their barber (56%). The results of the cultural consensus analysis from the ranking of 15 CaP risk factors demonstrated consensus (eigenratio = 3.3), suggesting overall agreement for a cultural model of CaP risk, with an average level of competency (mean = 0.52, SD = 0.27; Table 3). The top five risk factors ranked overall were (a) family history, (b) age, (c) not getting the exam, (d) African American heritage, and (e) diet. When asked to rate their CaP knowledge on a 5-point scale before receiving the education and afterwards, results suggested there was a significant increase in self-rated knowledge (z = ‒3.98, p < .01). Using the Spearman rank correlation, there was a moderate positive correlation between self-rated CaP knowledge and having had a PSA test, ρ(40) = .33, p < .05, meaning that clients who ranked themselves high on the knowledge score index generally were more likely to have had the PSA test. Regarding dissemination, most participants (90%) indicated that they either had already or would be taking the brochures home with them. Most agreed that they would pass on the brochures to family or friends (88%) and discuss the topic of CaP (90%).
Table 3. Clients' Ranking of Prostate Cancer Risk Factors.
| Item | Rank |
|---|---|
| Family history | 1 |
| Age | 2 |
| Not getting PCSa | 3 |
| African American | 4 |
| Dieta | 5 |
| Fooda | 6 |
| Lifestylea | 7 |
| Smokinga | 8 |
| Chemicals in environmenta | 9 |
| No exercisea | 10 |
| Stressa | 11 |
| Alcohola | 12 |
| Povertya | 13 |
| Contaminated watera | 14 |
| Not having sexa | 15 |
Categories were generated from free-listing questions in pilot survey phase. Other items were added from the scientific literature and risk factors identified by the American Cancer Society.
There were a number of questions related to health care provider discussions that could take place as a result of the barbershop education. When asked to answer retrospectively before receiving educational materials and information from their barber, 75% of participants reported being either “somewhat likely” or “very likely” to discuss CaP with their health care provider, but after the educational encounter, the proportion increased to 85% (p = .0001). Before being educated by their barbers, 35% of participants were either “somewhat worried” or “very worried” about their prostate health, but after receiving the education, the proportion increased to 45% (p = .0002; Table 4). When asked what they would do if a doctor recommended PCS, 88% of participants reported that they would be “very likely,” whereas only 10% were “somewhat likely” to follow the advice. When asked how likely they would be to recommend that a friend or family member discuss PCS with their health care provider, 65% of participants were “very likely” and 25% were “somewhat likely” to make a recommendation. Regarding preferences for PCS, 83% of participants responded that they would request the PSA and DRE together.
Table 4. Self-Reported Changes in Behavior Resulting From Barbershop Education Program.
| Percentage of Responses | |||
|---|---|---|---|
|
|
|||
| Dependent Variables | Retrospective | Postintervention | p Valuea |
| Likelihood of discussing CaP with a health care provider | |||
| Somewhat not likely to not likely | 25 | 15 | |
| Somewhat likely to very likely | 75 | 85 | <.001 |
| Level of worry about prostate health | |||
| Somewhat not worried to not worried | 65 | 55 | |
| Somewhat worried to very worried | 35 | 45 | <.001 |
Note: CaP = prostate cancer.
p Value based on Fisher's exact test of difference between self-reported before and after measures.
Barbershop client participants answered a series of questions selected from the HINTS (2007) survey to assess their PSA testing history. Table 5 compares the barbershop survey data with the HINTS 2005 national survey data, using only data from the subsample of African American men 40 years and older. Despite the small sample of barbershop clients, there were some similarities in the proportions of answers in response categories when compared with the national 2005 HINTS subsample survey data for African American men 40 years and older (n = 65). The limitation of using the 2005 HINTS data for comparative purposes is noted, due to the small sample of African Americans in the data set. The same proportion of participants (85%) in both surveys had heard of the PSA; however, in the barbershop survey, a greater proportion (80%) had received the test and had discussed the PSA test with their health care provider (88%). In response to whether their health care provider encouraged them to ask questions about the PSA test, more than half (57%) of the participants in the barbershop survey answered “yes, definitely,” similar to the HINTS survey results (54%).
Table 5. HINTS Survey Frequency Results.
| Percentage of Responses | ||
|---|---|---|
|
|
||
| Question | BAPC Study | HINTS 2005 |
| Have you ever heard of the PSA test? | (n = 40) | (n = 65) |
| Yes | 85 | 85 |
| No | 15 | 15 |
| Have you ever had the PSA test? | (n = 40) | (n = 65) |
| Yes | 80 | 69 |
| No | 20 | 31 |
| When did you have your most recent PSA test? | (n = 32) | (n = 38) |
| A year ago or less | 84 | 82 |
| 1-2 years ago | 0 | 10 |
| 2-5 years ago | 6 | 5 |
| More than 5 years ago | 10 | 3 |
| Has a health care provider ever talked to you about the PSA test? | (n = 40) | (n = 55) |
| Yes | 88 | 67 |
| No | 12 | 33 |
| Which of the following statements best describes your health care provider's recommendation about PSA tests? | (n = 35) | (n = 37) |
| Should have | 71 | 84 |
| Should not have | 6 | 5 |
| No recommendation | 23 | 11 |
| Did your health care provider encourage you to ask questions or express any concerns you had about PSA testing? | (n = 35) | (n = 37) |
| Yes, definitely | 57 | 54 |
| Yes, somewhat | 20 | 32 |
| No | 14 | 11 |
| No questions or concerns | 9 | 3 |
Note: BAPC = Barbers Against Prostate Cancer study; HINTS = National Cancer Institute Health Information National Trends Survey; PSA = prostate-specific cancer.
Discussion
Developing culturally appropriate cancer educational materials and programs have been found to dispel myths, eliminate misconceptions, and change fatalistic attitudes about cancer and cancer screening and treatments, all examples of cultural and experiential factors that have been shown to serve as barriers to PCS (Clarke-Tasker & Dutta, 2005; Guidry, Fagan, & Walker, 1998; Weinrich, Weinrich, Priest, & Fodi, 2003). However, many materials are neither culturally and literacy appropriate nor easily accessible to all population groups (Guidry et al., 1998; Kilbridge et al., 2009). Barbers Against Prostate Cancer is distinguished for its attention to customizing educational materials to increase knowledge of CaP in a priority population, African American men. Other barbershop-based education projects have used CaP education materials aimed at a general audience (Cowart, Brown, & Biro, 2004). We started with brochures, which had already been designed for the African American community (Meade et al., 2003), but we further adapted the brochures and posters to the barbershop venue and disseminated the educational messages through trained barber health advisers, trusted members of the community. Although the content, photos, and color scheme changed significantly, some of the verbiage and anatomical diagrams in the adapted brochure remained the same, verifying that the prior materials used appropriate language, written at the sixth-grade reading level. Based on the formative research, having photos of the barbers and a prominent civic leader on the adapted brochure and poster strengthened the appeal and persuasiveness of the message. Moreover, the barbers and clients told us the content was very easy to comprehend. In addition, prominent positioning of the plastic CaP model facilitated dialogue in the shops. After a photograph of a pair of barbers was featured in a JET magazine article focused on health disparities and CaP, the barbers told us that both this article and another article in the local African American newspaper and television coverage offered further credibility of the project in the community's perspective (Parham, 2008).
Many barriers to engaging in informed decision making with PCS have been identified, including patient comorbidity, limited health literacy, prior refusal of care, forgetfulness, acute care visits, and limited physician time (Guerra, Jacobs, Holmes, & Shea, 2006). In health promotion campaigns, men may receive CaP information in the form of pamphlets; however, some studies have shown that communicating the complex message of informed decision making in this format has not been shown to be effective. For example, in a randomized controlled trial, researchers found that brochures that discussed informed decision making placed in waiting rooms rarely led to actual observed informed decision making in the clinical setting (Kripalani et al., 2007). Multimedia approaches have also been used to facilitate informed decision making, yet one study demonstrated that patients with low literacy skills may experience difficulty with this educational format (Kim, Knight, & Tomori, 2001). Future studies in community venues are needed to determine whether materials placed in such locales and disseminated by trained LHAs may lead to greater informed decision making in the clinical encounter. Our study findings are congruent with another recent study by Kilbridge et al. (2009), which show that limited understanding of prostate anatomy and low literacy might serve as barriers for informed decision making, thus calling for an LHA role to prepare the patient for such physician-led discussions. In our study, the clients reported that they appreciated the ease of understanding the messages contained in our educational materials and the explanation provided by the barbers. The ranking results, listing family history, not getting PCS, age, and African American heritage in the top ranked responses for CaP risk factors, accords well with the biomedical model. The clients' cultural model of CaP risk factors from the ranking exercise included African American heritage, age, and family history, but these categories were not identified in the preliminary free-listing exercise. It was through the education program and the barber's talking points that the African American men learned that they were in a higher risk category for CaP and that age and family history were important risk factors. However, the belief that just getting the test can prevent CaP is a misconception that needs to be addressed, and interventions targeting positive lifestyle changes in diet and physical activity will have the most immediate impact in a climate of uncertain benefits around PCS. To address these uncertainties, the barbershop intervention aimed to overcome knowledge deficits and fears around CaP and PCS by providing men with accessible and relevant information to their life situation.
Despite the emphasis on informed decision making in the barber training, there was difficulty in translating this concept to the LHA intervention. Our consistent message to the barbers in the training and throughout the intervention was to convince their clients to speak to their health care provider about PCS, but at times this message was simplified to “need to get the test.” Nevertheless, the barber-administered intervention made the topic of CaP a comfortable one to discuss in the context of a trusted community setting and helped address some of the fears and negative emotional responses to cancer and PCS, specifically the DRE, that may have negative connotations (Allen et al., 2007). Further systematic, observational research should be conducted to analyze how often cancer-related health topics, specifically related to CaP, are discussed in typical barber– client interactions, as has been done in the beauty salon context for women's cancers (Solomon et al., 2004).
When comparing the responses of the HINTS questions between the client survey and the national survey data, a larger proportion of men in our study had not received the PSA in more than 5 years, had not received a PSA test recommendation, and had not been encouraged to ask questions about the test from their health care provider. Nevertheless, the data suggest that as a result of the intervention, the barbershop clients reported that they would be more likely to discuss PCS with their health care provider as well as encourage a friend or family member to have this discussion. The intervention led to a moderately higher degree of feelings of worry about prostate health, indicating that psychological dimensions, inclusive of worry, anxiety, and stress, should be further assessed in future interventions. Moreover, the survey results add further evidence that physician recommendation and increased knowledge about CaP remain strong motivators for deciding to elect PCS (Ross & Uhler, 2006).
There are several limitations to the pilot study. The barbershop clients surveyed reported that they believed their CaP knowledge increased as a result of the intervention; however, the study design did not employ a pretest/posttest design and asked clients to think retrospectively on a series of questions. Moreover, the generalization of survey findings is limited by the small sample size and the nonrandom selection of barbershops and clients to participate in the study, which turned out to not be representative of the population residing near the barbershops, which were in low-income neighborhoods. Many clients reported living in the east Tampa district when they were younger but moved out to the suburbs eventually. Despite the fact that many of these men lived dispersed around the county, the barber shop, similar to some area churches, served as a nexus for the Black community. Although the pilot project results have limited generalizability, the project was well received by both the barbers and the community, and there is community interest in expanding the program to other barbershops in the greater Tampa Bay area.
The outcomes of this study indicate the increasing need to decentralize our cancer prevention and control educational efforts, historically from the clinical setting, and begin to consider familiar, community-based, nonthreatening, and respected venues for cancer communications. The high response rate, receptivity of the barbers, and the engagement of the community health agency indicate that when African Americans are approached in a culturally and linguistically appropriate manner, they are adherent and receptive to participation in research. In this study, a novel communication channel was assessed to determine the feasibility of disseminating pertinent education and information related to CaP and PCS to African American men, a high risk and priority population. The results of this multiphased barber health adviser education intervention suggest an overall positive effect. The postintervention survey results with barbershop clients suggest positive knowledge, attitude, belief, and intention changes related to CaP and PCS as a result of exposure to the barbershop-based education program. The novel application of cultural consensus analysis to create a culturally correct answer key for the ranking exercise produced a positive knowledge outcome in lieu of using objective knowledge measures, which may have not been appropriate for the study given the nuanced messages from the barbers. Barber interest continues postintervention, and a barbershop advisory council has been formed to assist with wider dissemination efforts. The cancer center remains engaged with the barbers in cancer education and outreach efforts. Future studies should include testing the efficacy of this intervention strategy with a more representative sample for further refinement and dissemination.
Acknowledgments
The authors thank all those who participated in the research, the participating barbers, Community Health Advocacy Partnership (Ronald Brookins), Dr. James Brookins, LaShonda Coulbertson, Dr. Julio Pow-Sang, Dr. Jeffrey Starling, Dr. Brent Sullivan, and the Tampa Bay Community Cancer Network.
Funding: The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article:
This article was supported by NIH Grant No. U01 CA114627-03S2 from the National Cancer Institute.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
Authors' Note: The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute. This research was previously presented at the American Association for Cancer Research, the Science of Health Care Disparities, Carefree, Arizona, February 3, 2009.
References
- Allen JD, Kennedy M, Wilson-Glover A, Gilligan TD. African-American men's perceptions about prostate cancer: Implications for designing educational interventions. Social Science & Medicine. 2007;64:2189–2200. doi: 10.1016/j.socscimed.2007.01.007. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. ACS: Cancer facts & figures 2009. 2009 Retrieved January 23, 2010, from http://www.cancer.org/downloads/STT/500809web.pdf.
- Andriole GL, Crawford ED, Grubb RL, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. New England Journal of Medicine. 2009;360:1310–1319. doi: 10.1056/NEJMoa0810696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briscoe R, McClain G. African-American family support analysis: Strengths of African-American familes. Tampa: Louis de la Parte Florida Mental Health Institute, University of South Florida; 2000. [Google Scholar]
- Briss PA, River BK, Reilley B, Coates R, Lee NC, Mullen P, et al. Promoting informed decision making about cancer screening: What can communities and health care systems accomplish? Conceptual background and a systematic review. American Journal of Preventive Medicine. 2004;26:67–80. doi: 10.1016/j.amepre.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Clarke-Tasker VA, Dutta AP. African-American men and their reflections and thoughts on prostate cancer. Journal of the National Black Nurses Association. 2005;16:1–7. [PubMed] [Google Scholar]
- Coughlin SS, Wilson KM. Breast and cervical cancer screening among migrant and seasonal farmworkers: A review. Cancer Detection and Prevention. 2002;26:203–209. doi: 10.1016/s0361-090x(02)00058-2. [DOI] [PubMed] [Google Scholar]
- Couzin J. Biomarkers: Metabolite in urine may point to high-risk prostate cancer. Science. 2009;323:865. doi: 10.1126/science.323.5916.865a. [DOI] [PubMed] [Google Scholar]
- Cowart LW, Brown B, Biro DJ. Educating African American men about prostate cancer: The barbershop program. American Journal of Health Studies. 2004;19:205–213. [Google Scholar]
- Doak LG, Doak CC, Meade CD. Strategies to improve cancer education materials. Oncology Nursing Forum. 1996;23:1305–1312. [PubMed] [Google Scholar]
- Fernandez ME, Gonzales A, Tortolero-Luna G, Partida S, Bartholomew LK. Using intervention mapping to develop a breast and cervical cancer screening program for Hispanic farmworkers: Cultivando la salud. Health Promotion Practice. 2005;6:394–404. doi: 10.1177/1524839905278810. [DOI] [PubMed] [Google Scholar]
- Forrester-Anderson IT. Prostate cancer screening perceptions, knowledge and behaviors among African American men: Focus group findings. Journal of Health Care for the Poor and Underserved. 2005;16(Suppl. A):22–30. doi: 10.1353/hpu.2005.0122. [DOI] [PubMed] [Google Scholar]
- Fraser M, Brown H, Homel P, Macchia RJ, LaRosa J, Clare R, et al. Barbers as lay health advocates: Developing a prostate cancer curriculum. Journal of the National Medical Association. 2009;101:690–697. doi: 10.1016/s0027-9684(15)30978-0. [DOI] [PubMed] [Google Scholar]
- Freire P. Pedagogy of the oppressed. New York: Herder & Herder; 1970. [Google Scholar]
- Guerra CE, Jacobs SE, Holmes JH, Shea JA. Are physicians discussing prostate cancer screening with their patients and why or why not? A pilot study. Journal of General Internal Medicine. 2006;22:901–907. doi: 10.1007/s11606-007-0142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidry JJ, Fagan P, Walker V. Cultural sensitivity and readability of breast and prostate printed cancer education materials targeting African Americans. Journal of the National Medical Association. 1998;90:165–169. [PMC free article] [PubMed] [Google Scholar]
- Hart A, Bowen DJ. The feasibility of partnering with African-American barbershops to provide prostate cancer education. Ethnicity & Disease. 2004;14:269–273. [PubMed] [Google Scholar]
- Hart A, Underwood S, Smith W, Bowen D, Rivers B, Jones R, et al. Recruiting African-American barbershops for prostate cancer education. Journal of the National Medical Association. 2008;100:1012–1020. doi: 10.1016/s0027-9684(15)31437-1. [DOI] [PubMed] [Google Scholar]
- Hess P, Reingold J, Jones J, Fellman M, Knowles P, Ravenell J, et al. Barbershops as hypertension detection, referral, and follow-up centers for Black men. Hypertension. 2007;49:1040–1046. doi: 10.1161/HYPERTENSIONAHA.106.080432. [DOI] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches in public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Jones R, Underwood S, Rivers B. Reducing prostate cancer morbidity and mortality in African American men: Issues and challenges. Clinical Journal of Oncology Nursing. 2007;11:865–872. doi: 10.1188/07.CJON.865-872. [DOI] [PubMed] [Google Scholar]
- Jones RA, Wenzel J. Prostate cancer among African-American males: Understanding the current issues. Journal of the National Black Nurses Association. 2005;16:55–62. [PubMed] [Google Scholar]
- Kilbridge KL, Fraser G, Krahn M, Nelson EM, Conaway M, Bashore R, et al. Lack of comprehension of common prostate cancer terms in an underserved population. Journal of Clinical Oncology. 2009;27:2015–2021. doi: 10.1200/JCO.2008.17.3468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S, Knight S, Tomori C. Health literacy and shared decision making for prostate cancer patients with low socioeconomic status. Cancer Investigation. 2001;19:684–691. doi: 10.1081/cnv-100106143. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Sharma J, Justice E, Justice J, Spiker C, Laufman L, et al. Low-literacy interventions to promote discussion of prostate cancer: A randomized controlled trial. American Journal of Preventive Medicine. 2007;33:83–90. doi: 10.1016/j.amepre.2007.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkey L. Las mujeres saludables: Reaching Latinas for breast, cervical and colorectal cancer prevention and screening. Journal of Community Health. 2006;31:69–77. doi: 10.1007/s10900-005-8190-2. [DOI] [PubMed] [Google Scholar]
- Lim LS, Sherin K. Screening for prostate cancer in U.S. men: ACPM position statement on preventive practice. American Jouranl of Preventive Medicine. 2008;34:164–170. doi: 10.1016/j.amepre.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Luque JS, Monaghan P, Contreras R, August E, Baldwin J, Bryant C, et al. Implementation evaluation of a culturally competent eye injury prevention program for citrus workers in a florida migrant community. Progress in Community Health Partnerships. 2007;1:359–369. doi: 10.1353/cpr.2007.0040. [DOI] [PubMed] [Google Scholar]
- Luque JS, Rivers B, Kambon M, Brookins R, Green BL, Meade CD. Barbers against prostate cancer: A feasibility study for training barbers to deliver prostate cancer education in an urban African American community. Journal of Cancer Education. doi: 10.1007/s13187-009-0021-1. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CD, Calvo A, Rivera MA, Baer RD. Focus groups in the design of prostate cancer screening information for Hispanic farmworkers and African American men. Oncology Nursing Forum. 2003;30:967–975. doi: 10.1188/03.ONF.967-975. [DOI] [PubMed] [Google Scholar]
- Meade CD, Menard JM, Luque JS, Martinez-Tyson D, Gwede CK. Creating community-academic partnerships for cancer disparities research and health promotion. Health Promotion Practice. 2009 Oct 12; doi: 10.1177/1524839909341035. Epud ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse J. The significance of saturation. Qualitative Health Research. 1995;5:147–149. [Google Scholar]
- Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, et al. The Health Information National Trends Survey (HINTS): Development, design, and dissemination. Journal of Health Communication. 2004;9:443–460. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- Parham M. Men and prostate cancer: Take action to save your life. JET Magazine. 2008 Jun 9; Retrieved February 23, 2010, from http://findarticles.com/p/articles/mi_m1355/is_22_113/ai_n27497002/
- Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Medicine. 2007;33:418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Richardson JT, Webster JD, Fields NJ. Uncovering myths and transforming realities among low-SES African-American men: Implications for reducing prostate cancer disparities. Journal of the National Medical Association. 2004;96:1295–1302. [PMC free article] [PubMed] [Google Scholar]
- Romney AK, Weller SC, Batchelder WH. Culture as consensus: A theory of culture and informant accuracy. American Anthropologist. 1986;88:313–338. [Google Scholar]
- Ross LE, Uhler RJ. Age, race, and repeated prostate-specific antigen (PSA) test use in the National Health Interview Survey. Ethnicity & Disease. 2006;16:244–247. [PubMed] [Google Scholar]
- Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. New England Journal of Medicine. 2009;360:1320–1328. doi: 10.1056/NEJMoa0810084. [DOI] [PubMed] [Google Scholar]
- Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2008. CA: A Cancer Journal for Clinicians. 2008;58:161–179. doi: 10.3322/CA.2007.0017. [DOI] [PubMed] [Google Scholar]
- Solomon F, Linnan L, Wasilewski Y, Lee A, Katz M, Yang J. Observational study in ten beauty salons: Results informing development of the North Carolina BEAUTY and Health Project. Health Education & Behavior. 2004;31:790–807. doi: 10.1177/1090198104264176. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. U S Census 2000. 2000 Retrieved November 30, 2008, from http://www.census.gov/main/www/cen2000.html.
- U.S. Preventive Services Task Force. Screening for prostate cancer: Recommendation and rationale. Annals of Internal Medicine. 2002;137:915–916. doi: 10.7326/0003-4819-137-11-200212030-00013. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2008;149:185–191. doi: 10.7326/0003-4819-149-3-200808050-00008. [DOI] [PubMed] [Google Scholar]
- Wallerstein N, Bernstein E. Empowerment education: Freire's ideas adapted to health education. Health Education Quarterly. 1988;15:379–394. doi: 10.1177/109019818801500402. [DOI] [PubMed] [Google Scholar]
- Weinrich SP, Weinrich MC, Priest J, Fodi C. Self-reported reasons men decide not to participate in free prostate cancer screening. Oncology Nursing Forum. 2003;30:E12–E16. doi: 10.1188/03.ONF.E12-E16. [DOI] [PubMed] [Google Scholar]
- Weller SC, Romney AK. Systematic data collection. London: SAGE; 1988. [Google Scholar]


