Abstract
To assess the association between energy cost of walking and self-report of function, independent of comorbidity and gait speed, in older adults with mobility limitations. This cross-sectional observational study was conducted within an ambulatory clinical research training center. Forty-two older adults, age 65 and older, with slow and variable gait participated. Function was assessed using the Late Life Function and Disability Index- Basic Lower Extremity subscale, while energy cost of walking was derived by standardizing the mean oxygen consumption recorded during physiological steady state by gait speed. Comorbidity and gait speed were collected as co-variates. Pearson’s r correlation coefficient and regression analyses were used to assess the relationship between energy cost and function. Energy cost of walking was significantly correlated with self-reported function (Pearson’s r= −.50, p <.001); furthermore, energy cost of walking explained an additional 17% (p=.002) of the variance in self-reported function above and beyond the variance explained by comorbidity and gait speed combined.
Energy cost of walking is emerging as another significant factor related to functional performance among older adults, even after controlling for comorbidity and gait speed- robust variables known for their strong contributions to function. Knowledge of and attention to the efficiency of how one moves (high energy cost of walking) may enhance rehabilitation efforts to further reduce “functional burden” in older adults.
Keywords: Elderly, Gait, Physical function
1.0 Introduction
Remaining functionally independent within the community and maintaining a high quality of life are two common goals among older adults, often coinciding with aging. However, certain physiological changes that occur with aging, such as decreasing aerobic capacity and increasing energy cost of walking, may significantly challenge an older adult’s ability to maintain such goals. Progressive decline in aerobic capacity, the maximum amount of oxygen (and thus energy) available for use by the body at any one time, is thought to negatively impact independence and quality of life by reducing the total energy available to the body for performing basic and advanced daily activities(Fleg et al., 2005). With reduced maximum levels of “energy” available for routine function, activities such as walking may comprise a greater proportion of the available energy – therefore reducing the reserve available to complete additional activities (Figure 1A) (Ferrucci et al., 2000; Schrack, Simonsick, & Ferrucci, 2010b).
Figure 1.
Impact of aging on aerobic capacity. At age 80, the total available energy for use is lower than that at age 70. Therefore, tasks such as walking comprise a greater proportion of the total aerobic capacity in older adults (67% versus 50%); the reserve (energy) available for completing additional activities is reduced.
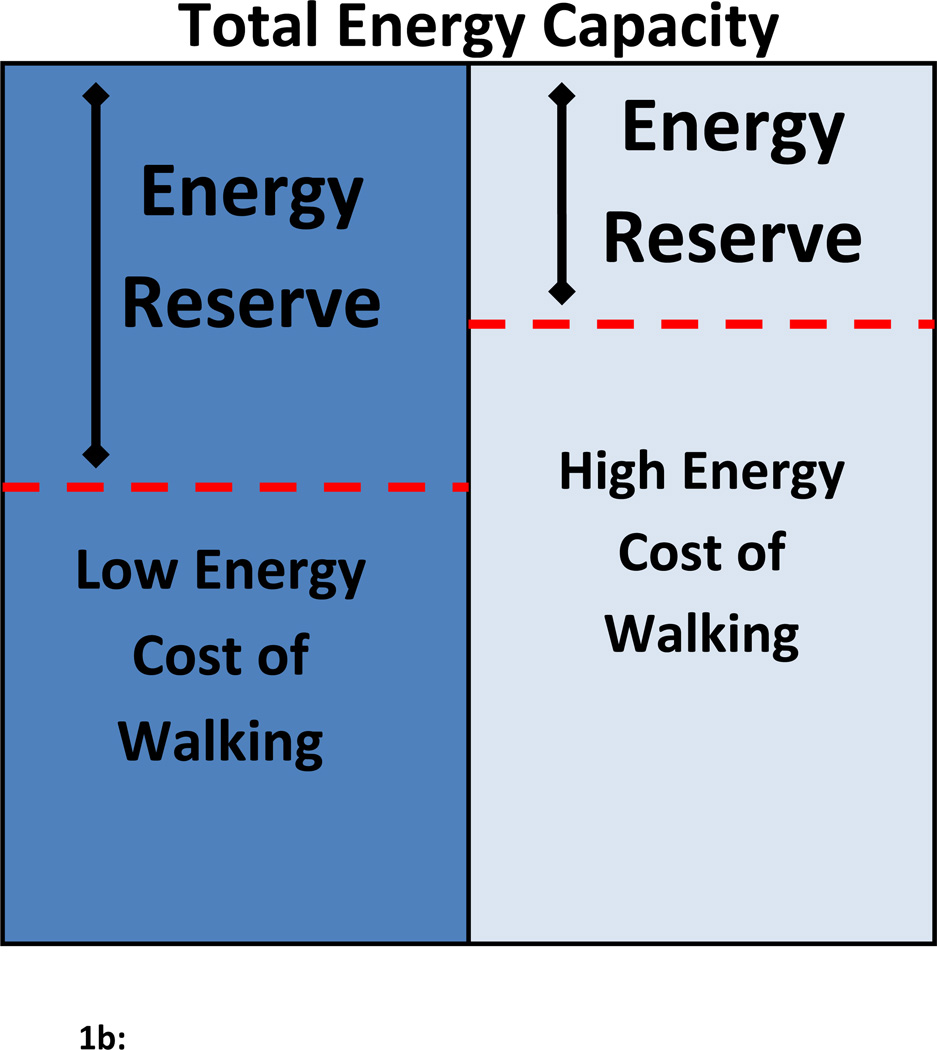
Potential impact of high energy cost of walking on energy reserves. Higher energy cost of walking utilizes a greater proportion of the total energy capacity. The higher energy cost of walking reduces the reserve energy available to perform additional activities.
While the age-related decline in aerobic capacity reduces the total energy available for older adults to complete daily tasks, age-related change in the way activities of daily living are performed - increases the energy demand from the body during task performance. Age-related gait abnormalities are known to increase walking energy expenditure - the energy cost of walking(R. Waters, 1992; R. L. Waters, Barnes, Husserl, Silver, & Liss, 1988; R. L. Waters & Lunsford, 1985; Wert, Brach, Perera, & VanSwearingen, 2010). Increased energy cost of walking has the potential to yield adverse functional consequences for older adults, as the amount of energy used during walking comprises a greater portion of the total energy available. As such, older adults may experience usual walking as both a more intense physical activity and a fatigue-producing daily activity. The greater intensity and fatigueability of walking emerges as the reserve between energy that is available and that which is being used by the body – narrows (Figure 1B). This is of great concern as daily walking-related activities perceived to cause greater fatigue and exhaustion are more apt to be reduced or discontinued (Hortobagyi, Mizelle, Beam, & DeVita, 2003; Vestergaard et al., 2009). Age-related higher energy cost of walking has the potential to lead to a decline in overall activity and greater risk of future mobility disability.
Although researchers have alluded to the contribution of energy cost of walking to functional decline in older adults (Hortobagyi, Finch, Solnik, Rider, & DeVita, 2011; Hortobagyi, et al., 2003; Malatesta et al., 2003; J. VanSwearingen, Perera S, Brach JS, Cham R, Rosano C, Studenski S, 2009), few if any studies have directly assessed such a relationship, especially among vulnerable older adults who have begun to show signs of mobility limitation. Therefore, the purpose of this study is to assess the cross-sectional relationship between energy cost of walking and function in a sample of community-dwelling older adults with mobility limitation (slowed and variable gait). We hypothesize that energy cost of walking will explain a unique portion of the variance in function of older adults, beyond that explained by robust variables known to be associated with function (gait speed and comorbidity). Specifically, we expect older adults with high energy cost of walking compared to low cost, to report poorer physical function.
2.0 METHODS
Data used for this cross-sectional study were collected as part of a baseline assessment (prior to randomization) for a 12-week randomized, controlled clinical trial comparing two forms of therapeutic activity to improve energy cost of walking and mobility in older adults with evidence of walking difficulty (J. VanSwearingen, Perera S, Brach JS, Cham R, Rosano C, Studenski S, 2009). This study was approved by the University of Pittsburgh Institutional Review Board, and all participants provided informed consent prior to participation.
2.1 Participants
Participants were recruited from the Pittsburgh Pepper Registry, a registry of older adults who have expressed an interest in participating in mobility research. Eligible subjects were community-dwelling older adults (≥ 65 years) with slow (0.6 ≤ speed ≤ 1.0 m/s) and variable gait (step length variability > 4.5% coefficient of variation or step width variability of <7% or > 30%), as determined during baseline testing using a computerized walkway (GaitMat IIa). Gait speed and variability of this type and magnitude have been shown to place older adults at greater risk for falls and future mobility disability (Brach JS, 2005; Maki, 1997). Eligibility was also dependent on the ability to ambulate independently with or without a cane; physician approval to participate in a low to moderate intensity exercise program; and a Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975) of 24 or greater. Only individuals with complete baseline data for all variables of interest (age, gait speed, comorbidity, function, and energy cost of walking) were included in the analyses.
2.2 Measures
2.2.1 Physical Function
The Late Life Function and Disability Instrument- Basic Lower Extremity Subscale (LLFDI-BLE)(Haley et al., 2002; Sayers et al., 2004), a self-report questionnaire, was used to assess physical function in older adults. The BLE subscale reports the difficulty in completing 14 activities which represent common daily activities performed by older adults, and primarily involves standing and essential walking (eg. walk around one floor of home, get into and out of car, step up and down from a curb, go up and down a flight of stairs, stand up from a low, soft couch). Scores on the BLE subscale range from 0–100, where higher scores indicate better function. The LLFDI has been shown to be a reliable (ICC= .91–.98) and valid measure of function in older adults (Haley, et al., 2002; Sayers, et al., 2004).
2.2.2 Energy Cost of Walking
Energy Cost of Walking
The energy cost of walking is a measure that reflects, via a measure of oxygen consumption, the energy used for all bodily actions during walking(Boyd et al., 1999), and is defined as the mean rate of oxygen consumption standardized by gait speed (R. Waters, 1992). Prior to baseline testing, all participants completed required practice walking sessions on a treadmill in order to become familiar and comfortable with treadmill walking. Once familiarization was complete, participants completed the baseline oxygen consumption assessment. Participants walked on a treadmill at their self-selected, usual walking speed for up to 6 minutes, while oxygen consumption was recorded with open-circuit spirometry (Medgraphics VO2000™ b). Energy cost of walking (ml/kg m) was calculated using the mean rate of oxygen consumption during physiological steady state (Boyd, et al., 1999; McArdle, Katch, & Katch, 1986). Steady state was identified by the plateau of oxygen consumption (ml/kg min) during walking; this is the physiologic point where the oxygen demand by the body is met by the oxygen being consumed – which in turn is equivalent to the energy expended for the task. Steady state typically occurs after 2–3 minutes of constant walking at a consistent gait speed; the plateau (or period of steady state) was identified when differences in oxygen consumption varied less than 3 ml/kg min. Concurrent assessment of the respiratory exchange ratio (RER) was also completed to identify steady state; RER values below 1.1 represent activity performed within the aerobic state where oxygen used represents the amount of energy expended for a given task. RER values above 1.1 indicate a transition into an anaerobic state, where oxygen consumed no longer accurately reflects the energy expended. Each participant record was individually inspected to determine if a period of steady state could be defined based on the parameter discussed above. Once a 1–3 minute period of steady state was identified, energy cost was calculated by dividing the mean oxygen consumption (ml/kg min) during steady state by the gait speed (held consistent) during treadmill walking. Individual records not within the stated parameters for steady state were not included in the analyses. Sub-maximal treadmill walking has frequently been used to assess energy cost of walking in older adults (Christiansen, Schenkman, McFann, Wolfe, & Kohrt, 2009; Fiser et al., 2010; Macko et al., 2001; Malatesta, et al., 2003; Martin, Rothstein, & Larish, 1992; McArdle, et al., 1986; Parvataneni K., 2008; Ralston, 1960; Schenkman, Hall, Kumar, & Kohrt, 2008; Schrack, Simonsick, & Ferrucci, 2010a; J. VanSwearingen, Perera S, Brach JS, Cham R, Rosano C, Studenski S, 2009; R. Waters, 1992; R. L. Waters, et al., 1988; Wert, et al., 2010).
2.2.3 Gait Speed
Gait Speed
Overground gait speed was recorded as participants walked over a 4m computerized walkway (GaitMat II)(Brach, 2008) at their self-selected, usual walking pace. Participants were encouraged to walk at a pace that represented their usual walking intensity as they completed various tasks throughout their daily routines. After practice trials, participants completed two consecutive 8-meter passes for data collection. Gait speed was recorded over the central 4 meters of the computerized walkway, the two 2 meters of inactive panels at the beginning and end of the GaitMat II walkway allowed for acceleration and deceleration. Gait speed was averaged over the two walks. Since gait speed is known to be associated with function (Cress et al., 1995; Potter, Evans, & Duncan, 1995; Studenski, 2009; Studenski et al., 2011) and energy cost of walking (Malatesta, et al., 2003; Martin, et al., 1992; Ralston, 1960), gait speed was treated as a covariate in our analyses.
2.2.4 Comorbidity
Comorbidity
The Comorbidity Index, a self-report assessment of 18 common health conditions, consolidated to 8 domains (cardiovascular, respiratory, musculoskeletal, neurological, general, cancer, diabetes, and visual) was used to assess medical history(Rigler, Studenski, Wallace, Reker, & Duncan, 2002). The total number of domains (of the 8) involved was recorded, and served as a second covariate in our analyses – as comorbidity has also been associated with function in older adults.
2.3 Data Analysis
We used appropriate descriptive statistics (mean, standard deviation, percentage) to summarize characteristics of our sample of older adults. We used Pearson product-moment correlation coefficients (r) to assess bivariate relationships among energy cost of walking, function, and covariates known to influence function. We fit linear regression models with function as the outcome; energy cost of walking as the primary independent variable of substantive interest; and relevant co-variables (gait speed and comorbidity) deemed important a priori as additional independent variables. Regression coefficient estimate and its statistical significance for energy cost of walking, and increase in the model coefficient of determination (R2) following the addition of energy cost of walking as an independent variable were interpreted as evidence of an association between energy cost of walking and function, independent of gait speed and comorbidity. All statistical analyses were performed with PASW Statistics 18 software.
3.0 RESULTS
Of the 50 participants eligible for the original RCT, 43 older adults had complete baseline data (age, comorbidity, gait speed, BLE function, and energy cost of walking) and were included in this cross-sectional study. Of the 7 participants excluded from the analyses, 2 had incomplete energy cost of walking data, 4 were missing comorbidity data, and 1 had incomplete measures of function. Older adults in our sample had a mean age of 77.0 (SD = 5.5) years, and a mean gait speed of 0.90 (.15) m/s (Table 1). The mean energy cost of walking in our sample of older adults with mobility limitations, .30 ml/kg m (SD = .10), was greater than the mean cost of walking reported for healthy older adults (.16 ml/kg m)(R. Waters, 1992; R. L. Waters, et al., 1988). The mean basic lower extremity function score, 63.3 (SD= 9.6), of our sample was similar to functional scores of older adults with moderate functional limitations (65.6) (Haley, et al., 2002).
Table 1.
Characteristics of Participants (N=43)
| Variable | Mean (SD) | Range |
|---|---|---|
| Age (y) | 77.0 (5.5) | 66–88 |
| Gender (n[% female]) | 29 (67) | NA |
| Comorbidity (0–8) | 4.2 (2.0) | 0–8 |
| Usual gait speed (m/s) | .90 (.15) | .58–1.04 |
| Energy Cost of walking (ml/kg m) | .30 (.10) | .12–.54 |
| LLFDI-BLE function (0–100) | 63.3 (9.6) | 43–88 |
Abbreviations: LLFDI-BLE = Late Life Function and Disability Instrument – Basic Lower Extremity subscale; NA = not applicable
A Pearson correlation matrix was generated to assess the relationship between energy cost of walking, comorbidity, gait speed, and basic lower extremity function. Energy cost of walking was associated with BLE function (Pearson’s r= −.50, p <.001); the negative relationship suggests a higher cost of walking is associated with a lower report of BLE function. Additionally, BLE function was related to gait speed (Pearson’s r=.48, p=.001), but was poorly associated with comorbidity (Pearson’s r= −.23, p=.07) in our sample (Table 2).
Table 2.
Baseline Correlations between Energy Cost and Function (r and p-values)
| Variables | Energy Cost | BLE Function | Comorbidity |
|---|---|---|---|
| BLE Function | −.50 (.001) | ||
| Comorbidity | −.10 (.27) | −.23 (.07) | |
| Gait Speed | −.25 (.05) | .48 (.001) | −.23 (.07) |
Abbreviations: BLE = Basic Lower Extremity subscale of Late Life Function and Disability Index
The relationship between energy cost of walking, comorbidity, gait speed, and basic lower extremity function was further assessed using linear regression (Table 3). When energy cost of walking was the only variable in the model, it significantly accounted for approximately 20% of the variance in basic lower extremity function, p=.002 (Model 1, Step 1). Independently, comorbidity failed to show a significant explanation in the variance of function in our sample (p=.136 [Model 2, Step 1]), while gait speed independently accounted for 19% of the variance in function, p=.003 (Model 3, Step 1).
Table 3.
Variance in Function Related to Energy Cost of Walking
| Model | Step | Variable | β (P) | R2 (P) | R2 change |
|---|---|---|---|---|---|
| 1 | 1 | Energy Cost | −.446 (.002) | .199 (.002) | - |
| 1 | Comorbidity | −.234 (.136) | .055 (.136) | - | |
| 2 | Comorbidity | −.286 (.037) | .328 (.0001) | .273 | |
| Energy Cost | −.525 (.0001) | ||||
| 1 | Gait Speed | .435 (.003) | .190(.003) | - | |
| 2 | Gait Speed | .336 (.016) | .303 (.001) | .113 | |
| Energy Cost | −.351 (.012) | ||||
| 1 | Comorbidity | −.131 (.365) | .249 (.004) | - | |
| Gait Speed | .425 (.003) | ||||
| 2 | Comorbidity | −.203 (.124) | .420 (.0001) | .172 | |
| Gait Speed | .326 (.019) | ||||
| Energy Cost | −.434 (.002) | ||||
β = Standardized coefficient
In models where comorbidity, gait speed, or both, were already in the model - energy cost of walking significantly provided additional explanation in the variance of function. Energy cost of walking explained an additional 27% (p=.0001) of the variance in function beyond that of comorbidity alone (Model 2, Step 2), 11% (p=.012) above that of gait speed alone (Model 3, Step 2), and 17% (p=.002) beyond that explained by comorbidity and gait speed combined (Model 4, Step 2).
4.0 DISCUSSION
In our study of older adults with mobility disability, energy cost walking was significantly related to physical function; older adults with higher energy costs of walking reported poorer physical functioning. Furthermore, while it is well known that comorbidity and gait speed make robust contributions to differences in performance roles and activity of daily living function in older adults (Cress, et al., 1995; Kishimoto et al., 1998; Potter, et al., 1995; Roos & Havens, 1991; Studenski, 2009; Studenski, et al., 2011; Verbrugge & Patrick, 1995), energy cost of walking appears to also be strongly related to function, explaining an additional 17% of the variance in BLE function - above and beyond the variance explained by comorbidity and gait speed combined. Such findings build support for the view that energy cost of walking may have a unique association with function in older adults, above and beyond more robust variables such as gait speed and comorbidity. Although the mechanisms underlying the relationship between energy cost of walking and physical function have not been clearly elucidated, researchers have suggested that older adults with higher costs of walking experience greater intensity of effort and fatigue during functional activities (Ferrucci, et al., 2000; Hortobagyi, et al., 2003; Schrack, et al., 2010b), potentially giving rise to poorer reports of function. It appears that “how” one moves (or walks), possibly the efficiency or skill of movement as related to the cost of movement, may help explain differences in function among older adults, beyond that explained by merely how fast or slow one walks.
As related to the efficiency of walking, or how one walks, versus merely the speed with which they walk – our findings may have important clinical implications. Previously demonstrated relations of gait speed to both present and future mobility and physical disability underscores the importance of gait interventions targeted to increase gait speed. Based on our current and prior findings (J. VanSwearingen, Perera S, Brach JS, Cham R, Rosano C, Studenski S, 2009; Wert, et al., 2010), increasing speed at any energy cost of walking may not be the best or recommended approach. An intervention aimed to reduce the energy cost of walking by improving the timing of postures to the stepping pattern and phases of gait resulted in both gait energy cost savings, increased gait speed and improved physical function, whereas a gait intervention targeted for impairments of strength, endurance and balance resulted in no change in the energy cost of walking, increased speed and no improvement in function (J. VanSwearingen, Perera, Brach, Wert, & Studenski, 2011). In the presence of abnormal gait patterns, older adults may benefit most from an initial focus on more energetic cost effective strategies of gait re-education to restore timing and coordination of the locomotor pattern. While the functional benefit of improved gait speed remains significant with regards to older adults, it may be that improving speed within a more efficient pattern of gait may be both the most effective and sustainable program of walking rehabilitation for older adults with mobility impairments.
Schrack and colleagues (2010) have presented a model of an “energetic pathway to mobility loss”, which suggests that as the energy required by the body to perform various physical tasks approaches the maximum level of energy available to the body, older adults may begin to experience greater levels of fatigue (Schrack, et al., 2010b). Once a certain “threshold” of fatigue has been breached, changes in physical function are likely to occur in an effort to reduce the energy expenditure. In older adults, fatigue is a commonly reported symptom, and has been shown to be associated with restricted activity and disability(Liao & Ferrell, 2000; Vestergaard, et al., 2009). Specifically, Vestergaard et al. (2009) showed that older adults with complaints of fatigue had reduced hand-grip strength, slower walking speed, and higher mobility and ADL activity and disability compared to non-fatigued counterparts (Vestergaard, et al., 2009). In a similar study of exertion/fatigue and older adults, Julius and colleagues (2012) reported perceived effort of walking was significantly associated with physical activity and function (Julius, Brach, Wert, & VanSwearingen, 2012). Older adults with a higher perceived effort (RPE) during walking reported lower LLFDI scores for total, BLE, and ALE subscales. Vestergaard and colleagues (2009) have further suggested that subclinical impairments (ie. inflammatory markers, thyroid function) may be responsible for increasing the fatigueability of body systems (tissues), which in turn contributes to poorer reports of function (Vestergaard, et al., 2009). There is also a growing body of evidence demonstrating age-related changes to gait characteristics and posture can also influence the energy cost of walking(Saha, Gard, Fatone, & Ondra, 2007; Wert, et al., 2010) – which may further contribute to a change in the perception of exertion during walking related activities for older adults. While the mechanism underlying the relationship between energy cost of walking and function remains to be clearly determined, it is likely to be multifaceted and incorporates physiologic and age-related changes from a variety of bodily systems. Additional longitudinal studies are needed to strengthen the causal inferences.
While it appears that higher energy costs of walking may have a detrimental relationship with physical function in older adults, unlike some factors related to function (comorbidity: cardiovascular disease, stroke, arthritis) that are limited in their ability to be “changed”, energy cost of walking appears to be amenable to intervention (Christiansen, et al., 2009; J. VanSwearingen, Perera S, Brach JS, Cham R, Rosano C, Studenski S, 2009). VanSwearingen et al. (2009) investigated the impact of two different exercise interventions on energy cost of walking in older adults with mobility disability. Older adults who completed an exercise program based on principles of motor learning which enhanced skill and smooth, automatic movement control reduced their energy cost of walking more than older adults who completed a general strengthening and overground walking program (J. VanSwearingen, Perera S, Brach JS, Cham R, Rosano C, Studenski S, 2009). While the ability to reduce energy cost of walking appears feasible in older adults, larger studies with long-term follow-up are needed to assess sustainability of change in energy cost of walking and subsequent influences on function.
This study has substantial strengths. Our participants are a clinically relevant population of older adults, at greater risk for additional decline in mobility. Within our small sample, energy cost of walking adds significantly to the explanation of the variance in function beyond that of robust variables, comorbidity and gait speed.
4.1 Study Limitations
Our sample of older adults was selected based on slow and variable gait, which made for a homogenous population, limiting the generalizability of our results to like populations. However, despite the small homogenous sample, we were able to find a substantial cross-sectional relationship between energy cost of walking and function. Finally, because our study was cross-sectional, no causal relationships could be established.
4.2 Conclusion
Energy cost of walking has a strong association with function in our sample of older adults with mobility disability; older adults with high energy cost of walking compared to low, demonstrated a poorer self-report of function. In light of our findings, along with recent literature demonstrating the amenability of energy cost to change with exercise intervention, we suggest attention be given to the assessment of energy cost of walking when addressing functional concerns in older adults. Knowledge of higher energy cost of walking and initiation of subsequent treatment strategies may enhance existing healthcare interventions aimed at reducing “functional burden” in older adults who are at risk for additional functional decline.
Acknowledgments
Funding Source
This project was funded in part by the Pittsburgh Claude D. Pepper Older Americans Independence Center (Grant #: P30 AG024827); and JS Brach is supported by the National Institutes on Aging and American Federation of Aging Research Paul Beeson Career Development Award (K23 AG026766).
Glossary
List of Abbreviations
- LLFDI-BLE
Late Life Function and Disability Instrument –Basic Lower Extremity Subscale
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement:
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript. (Author(s): David Wert, Jennifer Brach, Subashan Perera, Jessie VanSwearingen).
SUPPLIERS:
a. EQ, Inc, PO Box 16, Chalfont, PA 18914-0016
b. Medical Graphics Corp., 350 Oak Grove Parkway, St. Paul, MN 55127
Contributor Information
David M. Wert, Email: dmw29@pitt.edu.
Jennifer S. Brach, Email: jbrach@pitt.edu.
Subashan Perera, Email: ksp9@pitt.edu.
Jessie VanSwearingen, Email: jessievs@pitt.edu.
References
- Boyd R, Fatone S, Rodda J, Olesch C, Starr R, Cullis E, Graham K. High- or low-technology measurements of energy expenditure in clinical gait analysis? [Research Support, Non-U.S. Gov't] Developmental Medicine & Child Neurology. 1999;41(10):676–682. doi: 10.1017/s0012162299001395. [DOI] [PubMed] [Google Scholar]
- Brach JS BJ, VanSwearingen JM, Newman A, Studenski S. Too much or too little step width variability is associatted with a fall history in older persons who walk at or near normal gait speed. Journal of NeuroEngineering and Rehabilitation. 2005;2 doi: 10.1186/1743-0003-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brach JS, Perera S, Studenski S, Newman A. The Reliability and Validity of Measures of Gait Variability in Community-Dwelling Older Adults. Archives of Physical Medicine & Rehabilitation. 2008;89:2293–2296. doi: 10.1016/j.apmr.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen CL, Schenkman ML, McFann K, Wolfe P, Kohrt WM. Walking economy in people with Parkinson's disease. [Research Support, N.I.H., Extramural] Movement Disorders. 2009;24(10):1481–1487. doi: 10.1002/mds.22621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cress ME, Schechtman KB, Mulrow CD, Fiatarone MA, Gerety MB, Buchner DM. Relationship between physical performance and self-perceived physical function. [Comparative Study Multicenter Study Research Support, U.S. Gov't, P.H.S.] Journal of the American Geriatrics Society. 1995;43(2):93–101. doi: 10.1111/j.1532-5415.1995.tb06372.x. [DOI] [PubMed] [Google Scholar]
- Ferrucci L, Bandinelli S, Benvenuti E, Di Iorio A, Macchi C, Harris TB, Guralnik JM. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. [Research Support, Non-U.S. Gov't. 2000 doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- Research Support, U.S. Gov't, P.H.S.] Journal of the American Geriatrics Society. 48(12):1618–1625. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- Fiser WM, Hays NP, Rogers SC, Kajkenova O, Williams AE, Evans CM, Evans WJ. Energetics of walking in elderly people: factors related to gait speed. [Comparative Study] Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2010;65(12):1332–1337. doi: 10.1093/gerona/glq137. [DOI] [PubMed] [Google Scholar]
- Fleg JL, Morrell CH, Bos AG, Brant LJ, Talbot LA, Wright JG, Lakatta EG. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112(5):674–682. doi: 10.1161/CIRCULATIONAHA.105.545459. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Haley SM, Jette AM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, Ashba J. Late Life Function and Disability Instrument: II. Development and evaluation of the function component. 2002 doi: 10.1093/gerona/57.4.m209. Evaluation Studies. [DOI] [PubMed] [Google Scholar]
- Research Support, U.S. Gov't, P.H.S.] Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 57(4):M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- Hortobagyi T, Finch A, Solnik S, Rider P, DeVita P. Association between muscle activation and metabolic cost of walking in young and old adults. 2011 doi: 10.1093/gerona/glr008. Comparative Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Support, N.I.H., Extramural] Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 66(5):541–547. doi: 10.1093/gerona/glr008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hortobagyi T, Mizelle C, Beam S, DeVita P. Old adults perform activities of daily living near their maximal capabilities. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(5):M453–M460. doi: 10.1093/gerona/58.5.m453. [DOI] [PubMed] [Google Scholar]
- Julius L, Brach J, Wert D, VanSwearingen J. Perceived effort of walking: relationship with gait, physical function and activity, fear of falling, and confidence in walking in older adults with mobility limitations. Physical Therapy. 2012;92(10):1268. doi: 10.2522/ptj.20110326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishimoto M, Ojima T, Nakamura Y, Yanagawa H, Fujita Y, Kasagi F, Kagamimori S. Relationship between the level of activities of daily living and chronic medical conditions among the elderly. [Research Support, Non-U.S. Gov't] Journal of Epidemiology. 1998;8(5):272–277. doi: 10.2188/jea.8.272. [DOI] [PubMed] [Google Scholar]
- Liao S, Ferrell BA. Fatigue in an older population. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.] Journal of the American Geriatrics Society. 2000;48(4):426–430. doi: 10.1111/j.1532-5415.2000.tb04702.x. [DOI] [PubMed] [Google Scholar]
- Macko RF, Smith GV, Dobrovolny CL, Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic stroke patients. [Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.] Archives of Physical Medicine & Rehabilitation. 2001;82(7):879–884. doi: 10.1053/apmr.2001.23853. [DOI] [PubMed] [Google Scholar]
- Maki BE. Gait changes in older adults: predictors of falls or indicators of fear.[see comment] Journal of the American Geriatrics Society. 1997;45(3):313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- Malatesta D, Simar D, Dauvilliers Y, Candau R, Borrani F, Prefaut C, Caillaud C. Energy cost of walking and gait instability in healthy 65- and 80-yr-olds. [Clinical Trial Comparative Study] Journal of Applied Physiology. 2003;95(6):2248–2256. doi: 10.1152/japplphysiol.01106.2002. [DOI] [PubMed] [Google Scholar]
- Martin PE, Rothstein DE, Larish DD. Effects of age and physical activity status on the speed-aerobic demand relationship of walking. Journal of Applied Physiology. 1992;73(1):200–206. doi: 10.1152/jappl.1992.73.1.200. [DOI] [PubMed] [Google Scholar]
- McArdle W, Katch F, Katch V. Exercise Physiology. Philadelphia: Lea and Febiger; 1986. [Google Scholar]
- Parvataneni KPL, Olney S, Brouwer B. Kinematic, kinetic and metabolic parameters of treadmill versus overground walking in healthy older adults. Clinical Biomechanics. 2008;24:95–100. doi: 10.1016/j.clinbiomech.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Potter JM, Evans AL, Duncan G. Gait speed and activities of daily living function in geriatric patients. [Comparative Study] Archives of Physical Medicine & Rehabilitation. 1995;76(11):997–999. doi: 10.1016/s0003-9993(95)81036-6. [DOI] [PubMed] [Google Scholar]
- Ralston H. Comparison of energy expenditure during treadmill walking and floor walking. J Appl Physiol. 1960;15 doi: 10.1152/jappl.1960.15.6.1156. [DOI] [PubMed] [Google Scholar]
- Rigler SK, Studenski S, Wallace D, Reker DM, Duncan PW. Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clinical Rehabilitation. 2002;16(4):420–428. doi: 10.1191/0269215502cr515oa. [DOI] [PubMed] [Google Scholar]
- Roos NP, Havens B. Predictors of successful aging: a twelve-year study of Manitoba elderly. [Research Support, Non-U.S. Gov't] American Journal of Public Health. 1991;81(1):63–68. doi: 10.2105/ajph.81.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha D, Gard S, Fatone S, Ondra S. The effect of trunk-flexed postures on balance and metabolic energy expenditure during standing. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.] Spine. 2007;32(15):1605–1611. doi: 10.1097/BRS.0b013e318074d515. [DOI] [PubMed] [Google Scholar]
- Sayers SP, Jette AM, Haley SM, Heeren TC, Guralnik JM, Fielding RA. Validation of the Late-Life Function and Disability Instrument. [Research Support, U.S. Gov't, P.H.S. Validation Studies] Journal of the American Geriatrics Society. 2004;52(9):1554–1559. doi: 10.1111/j.1532-5415.2004.52422.x. [DOI] [PubMed] [Google Scholar]
- Schenkman M, Hall D, Kumar R, Kohrt WM. Endurance exercise training to improve economy of movement of people with Parkinson disease: three case reports. [Case Reports Research Support, N.I.H., Extramural] Physical Therapy. 2008;88(1):63–76. doi: 10.2522/ptj.20060351. [DOI] [PubMed] [Google Scholar]
- Schrack JA, Simonsick EM, Ferrucci L. Comparison of the Cosmed K4b(2) portable metabolic system in measuring steady-state walking energy expenditure. [Comparative Study Randomized Controlled Trial Research Support, N.I.H., Intramural] PLoS ONE [Electronic Resource] 2010a;5(2):e9292. doi: 10.1371/journal.pone.0009292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrack JA, Simonsick EM, Ferrucci L. The energetic pathway to mobility loss: an emerging new framework for longitudinal studies on aging. [Research Support, N.I.H., Intramural Research Support, Non-U.S. Gov't Review] Journal of the American Geriatrics Society. 2010b;58(Suppl 2):S329–S336. doi: 10.1111/j.1532-5415.2010.02913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studenski S. Bradypedia: is gait speed ready for clinical use? [Editorial] Journal of Nutrition, Health & Aging. 2009;13(10):878–880. doi: 10.1007/s12603-009-0245-0. [DOI] [PubMed] [Google Scholar]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Guralnik J. Gait speed and survival in older adults. [Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural Research Support, Non-U.S. Gov't] JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanSwearingen J, Perera S, Brach J, Wert D, Studenski S. Impact of Exercise to Improve Gait Efficiency on Activity and Participation in Older Adults with Mobility Limitations: A Randomized Controlled Trial. Physical Therapy. 2011;91:1740–1751. doi: 10.2522/ptj.20100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanSwearingen J, Perera S, Brach JS, Cham R, Rosano C, Studenski S. A Randomized Trial of Two Forms of Therapeutic Activity to Improve Walking: Effect on the Energy Cost of Walking. J Gerontol Med Sci. 2009 doi: 10.1093/gerona/glp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, Patrick DL. Seven chronic conditions: their impact on US adults' activity levels and use of medical services. [Comparative Study] American Journal of Public Health. 1995;85(2):173–182. doi: 10.2105/ajph.85.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vestergaard S, Nayfield SG, Patel KV, Eldadah B, Cesari M, Ferrucci L, Guralnik JM. Fatigue in a representative population of older persons and its association with functional impairment, functional limitation, and disability. [Comparative Study Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural Research Support, Non-U.S. Gov't] Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2009;64(1):76–82. doi: 10.1093/gerona/gln017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters R. Energetics. In: Perry J, editor. Gait Analysis: Normal and Pathological Function. Thorofare, NJ: SLACK Incorporatated; 1992. [Google Scholar]
- Waters RL, Barnes G, Husserl T, Silver L, Liss R. Comparable energy expenditure after arthrodesis of the hip and ankle. 1988 Comparative Study. [PubMed] [Google Scholar]
- Research Support, Non-U.S. Gov't] Journal of Bone & Joint Surgery - American Volume. 70(7):1032–1037. [PubMed] [Google Scholar]
- Waters RL, Lunsford BR. Energy cost of paraplegic locomotion. [Research Support, U.S. Gov't, Non-P.H.S.] Journal of Bone & Joint Surgery - American Volume. 1985;67(8):1245–1250. [PubMed] [Google Scholar]
- Wert DM, Brach J, Perera S, VanSwearingen JM. Gait biomechanics, spatial and temporal characteristics, and the energy cost of walking in older adults with impaired mobility. [Research Support, N.I.H., Extramural] Physical Therapy. 2010;90(7):977–985. doi: 10.2522/ptj.20090316. [DOI] [PMC free article] [PubMed] [Google Scholar]