Abstract
Hematopoietic stem cell transplant survivors who are 1-3 years post-transplant are challenged by the need to resume valued social roles and activities—a task that may be complicated by enduring transplant-related psychological distress common in this patient population. The present study investigated whether transplant survivors who receive adequate social support from their spouse or intimate partner experience lower distress. Effects of receiving a greater quantity of partner support (a common approach to studying enacted support) were compared with effects of receiving more effective partner support (i.e., support that more closely matches their needs in terms of its quantity and quality). Men and women (N = 230) who were 1-3 years post-transplant completed measures of partner support quantity (Manne & Scholl, 2001), partner social support effectiveness (Rini & Dunkel Schetter, 2010), and psychological distress (Brief Symptom Inventory; Derogatis & Spencer, 1982). Potential medical and sociodemographic confounds were controlled in analyses. As hypothesized, survivors reported less distress when they received more effective partner support (p < .001). Quantity of partner support was not associated with distress (p = .23). An interaction revealed that when partner support was effective, the quantity of support survivors received was not associated with their distress (p=.90); however, when partner support was ineffective, receiving a greater quantity of partner support was associated with substantially elevated distress (p = .002). Findings suggest that clinical approaches to addressing or preventing enduring distress after HSCT should target features of partner support related to its appraised effectiveness.
Keywords: Hematopoietic stem cell transplantation, social support, psychological adjustment
Hematopoietic stem cell transplantation (HSCT) is an aggressive treatment for hematological and lymphatic cancers along with a growing number of other diseases (Copelan, 2006). It usually involves a lengthy hospitalization that begins with a potentially lethal regimen of high dose chemotherapy (sometimes with total body irradiation), followed by a life-saving infusion of blood-producing stem cells. Patients and their caregivers must cope with numerous medical and psychosocial challenges, including distressing medical procedures (e.g., protective isolation due to immunosuppression), risk for life-threatening complications (e.g., graft versus host disease [GvHD], infections, organ toxicities, relapse, secondary cancers), acute and chronic side effects (e.g., immunosuppression, sexual dysfunction, occupational disability, negative body image, fatigue, cognitive impairment), and practical problems (e.g., ongoing medical care, disrupted family and work roles, difficulties with social reintegration, financial difficulties; Andrykowski & McQuellon, 1999; Bevans, Mitchell, & Marden, 2008; Copelan, 2006; Syrjala, Kurland, Abrams, Sanders, & Heiman, 2008; Wingard, Vogelsang, & Deeg, 2002).
Transplant recipients are also at risk for clinical and subclinical distress, including symptoms of depression and anxiety as well as more general forms of distress such as those related to existential concerns and loneliness (e.g., Rusiewicz et al., 2008; see Mosher, Redd, Rini, Burkhalter, & DuHamel, 2009 for a review). On average, distress peaks around the time of HSCT and then declines in the year thereafter (Broers, Kaptein, Le Cessie, Fibbee, & Hengeveld, 2000; Keogh et al., 1998; Syrjala et al., 2004). However, this trajectory does not describe all transplant recipients equally well; although estimates vary, on average their distress is higher than healthy controls and up to 40% of survivors report distress even years after transplant (Andrykowski et al., 2005; Bishop, 2008; Broers et al., 2000; McQuellon et al., 1998; Syrjala, Chapko, Vitaliano, Cummings, & Sullivan, 1993; Syrjala et al., 2004; see Hoodin, Harper, & Posluszny, 2010 and Mosher et al., 2009 for reviews).
Research has identified various sociodemographic and medical predictors of elevated distress among transplant recipients, including worse pre-transplant psychological adjustment (e.g., Broers et al., 2000; Syrjala et al., 1993), poor post-transplant physical functioning (Broers et al., 2000), being female (Syrjala et al., 2004), and having chronic GvHD (Syrjala et al., 1993, 2004; see Hoodin et al., 2010, for a more complete listing). In addition, although some studies report modest or minimal effects of social support (Molassiotis, van den Akker, & Boughton, 1997), most evidence shows that it is associated with psychological adjustment to transplant (e.g., Frick et al., 2006; Hochhausen et al., 2007; Jacobsen et al., 2002; Jenks Kettmann & Altmaier, 2008; Syrjala et al., 2004; Wells, Booth-Jones, & Jacobsen, 2009). For instance, transplant recipients with more negative perceptions of pre-transplant support have more depressive symptoms post-transplant (Jenks Kettman & Altmaier, 2008; Syrjala et al., 2004) and they report worse post-transplant quality of life (Hochhausen et al., 2007). Fewer studies have measured social support post-transplant, but one study linked lower post-transplant support with greater post-traumatic stress symptomatology (Widows, Jacobsen, & Fields, 2000).
There is also evidence that HSCT can have long lasting detrimental effects on transplant recipients’ relationship with their spouse or intimate partner (Andrykowski et al., 2005). This evidence is notable because most transplant recipients name their partner as their primary caregiver (e.g., Eldredge et al., 2006; Fife, Monahan, Abonour, Wood, & Stump, 2009; Frick, Rieg-Appleson, Tyroller, & Bumeder, 2005; Siston et al., 2001; Stetz, McDonald, & Compton, 1996). Thus, like psychosocial stress more generally (Rini & Dunkel Schetter, 2010), this challenging treatment has the potential to undermine a critical source of social support for transplant recipients, with implications for their post-transplant psychological recovery. Taken together, this evidence highlights a pressing need for a more in-depth understanding of social support within the intimate relationships of transplant survivors. Such research should focus specifically on partner support rather than measuring support aggregated across multiple support providers (e.g., family members or unspecified close others), as past research has done.
Guided by the foregoing, the present study investigated partner support as a predictor of distress among transplant survivors. We focused on post-transplant partner support among survivors who were 1- to 3-years post-transplant, which allowed us to investigate a timeframe during which enduring elevated distress is likely to hinder a critical turning point in recovery from HSCT. Specifically, 1-year post-transplant is a psychological milestone at which many survivors turn their attention to resuming valued roles and activities—a key task in long-term recovery, and one that can be stressful for both survivors and their loved ones (Lee, 2008; McQuellon et al., 1998). We also sought to address two shortcomings of existing research that limit its usefulness for guiding development of interventions. First, as noted above, existing studies have investigated support aggregated across multiple support providers (e.g., Frick et al., 2006; Heinonen et al., 2001; Hochhausen et al., 2007; Jacobsen et al., 2002; Jenks Kettmann & Altmaier, 2008; Molassiotis et al., 1997; Wells et al., 2009). In our view, research focused on partner support would provide a strong foundation for the development of effective social support interventions because it would enable them to target support from the most likely main support provider.
Second, most existing studies have investigated perceived social support (i.e., the extent to which it is perceived to be available if needed; e.g., Heinonen et al., 2001; Hochhausen et al., 2007; Jacobsen et al., 2002; Jenks Kettmann & Altmaier, 2008; Wells et al., 2009). Findings from these studies are relatively unhelpful for guiding interventions because they provide little information about support behaviors that should be promoted or addressed. Even past studies that investigated a more behavioral aspect of support (i.e., enacted support) are not optimally useful because they have applied a traditional measurement approach in which a greater quantity of social support is conceptualized as representing better support—that is, more plentiful resources for the recipient. Yet, because of individual differences in skill, motivation, and ability to overcome their own burdens, some partners are less likely than others to provide support that truly helps transplant recipients cope effectively with their treatment. Partners do not always understand the best way to help or, if they do, they may not implement it effectively.
Indeed, many transplant recipients report instances of ineffective or problematic support from their partner and others. For instance, Andrykowski and colleagues (1999) found that many survivors report concerns related to others not understanding their needs (56% of survivors), others not knowing what to say to them or how to treat them (51%), others being overprotective (49%), and problems communicating with their spouse or partner (49%). General concerns about the effect of transplant on their relationship with their partner are also prevalent (46%). At the same time, transplant recipients rely on their partner for various types of support, and partner support has the potential to be a valuable resource for helping them cope with survivorship issues such as long-term and late effects of transplant, continuing medical follow up, and complex self-care routines such as those related to screening (Rizzo et al., 2006).
In sum, social support attempts are not always successful at providing their intended benefit from the perspective of the recipient. In the present study we applied a theoretical framework that explicitly considers features of social support attempts associated with recipients’ appraisals of their effectiveness. Specifically, the social support effectiveness framework (Rini & Dunkel Schetter, 2010) enables investigation of the effectiveness of social support attempts made by a specific provider, with effective support defined as emotional, informational, and instrumental support appraised by recipients as providing a good match for their needs in terms of their amount and type, not being difficult to obtain, being skillfully delivered, and not negatively influencing their self-concept. In our research investigating social support effectiveness in pregnancy we found that women who received more effective partner support in early pregnancy reported lower concurrent prenatal anxiety as well as lower prenatal anxiety in later pregnancy (Rini et al., 2006).
In sum, in the present study we investigated associations between partner support and transplant survivors’ distress, evaluating the value of differentiating between the quantity of partner support (partner support quantity) and its effectiveness (partner social support effectiveness or partner SSE) in order to provide useful information to guide development of interventions. Participants were 230 men and women who were 1- to 3-years post-transplant. We hypothesized that more effective partner support (i.e., greater partner SSE) would predict lower survivor distress. We also hypothesized that the association between partner support quantity and survivors’ distress would be moderated by partner SSE. Specifically, we hypothesized that receiving a greater quantity of partner support would be associated with lower survivor distress only for survivors whose partner provided effective support. In contrast, we hypothesized that receiving a greater quantity of partner support from a partner who provided ineffective support would be associated with greater survivor distress.
Method
Participants and Procedure
The sample was composed of 230 HSCT survivors who participated in screening for a randomized controlled trial testing a cognitive behavioral intervention for distressed HSCT survivors (DuHamel et al., 2010). They had not begun the intervention at the time of data collection nor were they required to meet the trial’s distress-related criteria to be included in these analyses. Potential participants were identified through oncologists and patient databases at three hospitals in the northeastern United States, mailed a recruitment letter and study materials (including an informed consent form), and telephoned to verify their eligibility and interest. Seven hundred and fifty one survivors were prescreened to evaluate whether they met criteria for entry into screening: They had to be at least 18 years old, English speaking, and 1- to 3-years post-transplant. They were excluded from screening if they were awaiting another transplant (n = 15), because such patients face different psychosocial challenges than do patients who have successfully completed transplant. They were also excluded if language barriers prevented them from completing consent procedures and study measures (n = 43). Eligible survivors who agreed completed a mailed questionnaire and a telephone interview conducted by a trained research assistant. Consent was obtained at the beginning of the interview. The questionnaire and interview each took about 60 minutes to complete and included measures for the present study as well as other psychosocial measures not reported here. Of the 498 survivors who met criteria for parent study screening, 452 (91%) consented to screening and 328 (73%) of these participants subsequently completed the screening interview and questionnaire. The other 118 were lost to contact (n = 48), withdrew from the study (n = 28), became ineligible (e.g., due to relapse; n = 10), or did not complete the measures before the study ended (n = 26). Most of the 328 participants (n = 303, 92%) provided necessary medical data through medical record review. Of these 303 participants, 230 (76%) were married, cohabiting, or had a main intimate partner and were therefore included in the present study. The institutional review boards at all three institutions approved the study.
Measures
Partner support quantity
Partner support quantity was assessed with the 8-item Partner Responses to Cancer Inventory (Manne & Schnoll, 2001) which measures the frequency with which partners provide specific types of informational, instrumental, and emotional support (e.g., “comforted me by showing me some physical affection”) in the prior month. Responses are made on a scale from 1 = never responds this way to 4 = often responds this way (with behaviors that have not occurred coded as “not applicable”). Items are averaged, and higher scores indicate a greater quantity of support received in the prior month (Cronbach’s alpha = .82).
Partner social support effectiveness
Partner social support effectiveness was assessed with the 25-item Social Support Effectiveness–Questionnaire (Rini & Dunkel Schetter, 2010). For each of three types of partner support (emotional, informational, instrumental), participants read a brief description of the type of support then respond to questions assessing: 1) how well the quantity of the support matched the amount needed (0 = very poor to 4 = excellent); 2) the extent to which the respondent wished it had been different somehow (0 = not at all to 4 = extremely); 3) the extent to which it was perceived to have been provided skillfully (0 = not at all to 4 = extremely); 4) how difficult it was to get (0 = never to 4 = always); and 5) whether the partner ever offered the support without being asked (0 = never to 4 = always). An additional 10 items assess unintended negative byproducts of receiving support (e.g., feelings of guilt or indebtedness; 0 = yes and 2 = no). Responses focus on support provided in the prior 3 months. Total scores can range from 0-80, with higher scores indicating more effective support during that time period (Cronbach’s alpha = .95).
Distress
Distress was assessed with the 53-item Brief Symptom Inventory (BSI; Derogatis & Spencer, 1982), which includes symptoms related to depression, anxiety, somatization, hostility, paranoid ideation, interpersonal sensitivity, obsession-compulsion, psychoticism, and phobic anxiety. Participants rated the extent to which each symptom caused them discomfort in the prior month on a scale from 0 = not at all to 5 = extremely. Distress was indexed by the BSI global severity index, which uses responses to all 53 items and is the scale’s most sensitive indicator of distress (Derogatis & Spencer, 1982; Cronbach’s α = .94).
Sociodemographic characteristics
Sociodemographic data were self-reported and included age, sex, relationship status (coded 1 = married, 0 = not married), annual household income, education (1 = college degree, 0 = no college degree), work status (1 = working part or full time, 0 = other status), and race/ethnicity (1 = Non-Hispanic White, 0 = Other). History of mental health problems prior to diagnosis was assessed by asking whether participants had seen “anyone for emotional or psychiatric problems” and, if they answered “yes,” how long ago. This variable was coded “yes” if the visit(s) occurred prior to their cancer diagnosis.
Medical characteristics
We abstracted from medical charts data regarding diagnosis, history of disease relapse (yes/no) and prior transplant (yes/no), weeks since transplant, type of transplant (1 = allogeneic, 0 = autologous), HLA match (1 = matched, 0 = unmatched), presence of acute and chronic GvHD (yes/no), number of serious transplant-related complications (not counting GvHD; e.g., infections, mucositis), number of post-transplant hospitalizations, and current disease status (1 = alive with disease, 0 = free of disease). Physical functioning was assessed with a self-report version of the Karnofsky Performance Scale (Karnofsky et al., 1948), which uses a 7-point response scale ranging from 40 (disabled, requiring special care and help) to 100 (normal) in 10-point increments. Scores have been associated with quality of life and clinically significant illness in HSCT patients (Wingard, Curbow, Baker, & Piantadosi, 1991).
Data Analysis
First, descriptive statistics were computed. No variable had more than 8 missing values, so missing values were mean or mode replaced (for continuous and categorical variables, respectively). Univariate analyses were used to examine the distributional properties of study measures. Variables for number of serious transplant complications and post-transplant hospitalizations were moderately positively skewed and were therefore trichotomized (0, 1, ≥ 2). Next we investigated the need to control sociodemographic (age, patient sex, marital status, education, income, work status, race/ethnicity) and medical variables (diagnosis, history of relapse and prior transplant, type of transplant, HLA match, weeks since transplant, presence of acute and chronic GvHD, number of serious transplant-related complications, number of post-transplant hospitalizations, current disease status, current self-reported physical functioning) by examining bivariate associations between these variables and distress. Any that were significantly associated with distress were evaluated as potential control variables in the main analysis, which was a hierarchical multiple regression analysis in which distress was regressed on partner support quantity, partner SSE, and their interaction. Continuous variables were mean centered and interactions terms involving continuous variables were calculated using mean centered variables to reduce multicollinearity and enhance interpretability of findings.
Results
Description of Sample
Descriptive statistics for the sample are shown in Table 1. Participants were primarily non-Hispanic White and married. There were approximately equal numbers of men and women. The median annual household income was over $80,000, with a broad range that represented the entire scale. Participants’ ages ranged from 23 to 80, with an average age of 55 years. Most had completed at least some college, although a modest percentage had a high school education or less. Fewer than half were working full or part time. The most common diagnoses were multiple myeloma, lymphoma, or leukemia. Two-thirds of participants had undergone autologous transplant. Most participants (66%) reported that they were able to perform normal activities with either no or minor physical complaints. BSI-gsi scores indicated that 24% of survivors met criteria for probable clinically diagnosable distress. On average, partner support quantity was relatively high, with mean scores falling between “sometimes responds this way” and “often responds this way” (M = 3.44, SD = .56), although observed scores spanned the full range of the scale. Average partner SSE was also relatively high (M = 61.52, SD = 14.70); observed scores nearly spanned the full scale (9-80).
Table 1.
Descriptive Statistics (N = 230)
| Variable | n (%) | M (SD) | Range |
|---|---|---|---|
| Sex--Male | 123 (54%) | ||
| Marital status—Married | 215 (94%) | ||
| Race/ethnicity | |||
| Non-Hispanic White | 205 (89%) | ||
| Hispanic/Latino | 7 (3%) | ||
| African American/Black | 6 (3%) | ||
| Other | 11 (5%) | ||
| Missing | 1 (0%) | ||
| Age (years) | 54 (10) | 23 to 80 | |
| Annual household income (median) | > $80,000 | < $10,000 to > $80,000 | |
| Education | |||
| High school or less | 32 (14%) | ||
| Partial college | 45 (20%) | ||
| Four-year college degree | 95 (41%) | ||
| Graduate degree | 58 (25%) | ||
| Working full or part time | 98 (43%) | ||
| Diagnosis | |||
| Multiple myeloma | 77 (33%) | ||
| Lymphoma | 72 (31%) | ||
| Leukemia | 42 (18%) | ||
| Other | 39 (17%) | ||
| History of pre-transplant disease relapse | 23 (10%) | ||
| Type of transplant | |||
| Autologous | 154 (67%) | ||
| Allogeneic (matched) | 38 (17%) | ||
| Allogeneic (unmatched) | 38 (17%) | ||
| Weeks since transplant | 93 (27) | 27 to 173 | |
| History of prior transplant(s) | 15 (7%) | ||
| Number of serious transplant complications | |||
| None | 158 (69%) | ||
| One | 39 (17%) | ||
| Two or more | 34 (15%) | ||
| Graft versus Host Disease | |||
| Acute | 11 (5%) | ||
| Chronic | 20 (9%) | ||
| Number of post-transplant hospitalizations | |||
| None | 141 (61%) | ||
| One | 46 (20%) | ||
| Two or more | 43 (19%) | ||
| Current disease status | |||
| Free of disease | 164 (71%) | ||
| Alive with disease | 66 (29%) | ||
| Self-reported physical functioninga | 86.80 (11.22) | ||
| No physical complaints | 50 (22%) | ||
| Minor physical complaints | 97 (42%) | ||
| Normal activity with effort | 45 (20%) | ||
| Other | 30 (13%) | ||
| Missing | 8 (3%) |
Measured with the Karnofsky Performance Scale (Karnofsky et al., 1948) adapted for self-report (Wingard et al., 1991).
Predictors of Survivors’ Post-Transplant Distress
Correlations among primary study variables are shown in Table 2. Potential confounds that were significantly associated with distress in bivariate analyses included sex (women reported more distress than men, F[1,228] = 8.70, p = .004); age (r = −.24, p < .001); education (survivors with post-high school education reported less distress than those with a high school education or less, F[1,228] = 7.47, p = .01); income (r = −.14, p = .03); history of mental health problems (survivors with a history of problems prior to diagnosis reported higher distress than those who did not F[1,228] = 6.66, p = .01); number of post-transplant hospitalizations (r = .20, p = .002); HLA match (unmatched allogeneic transplant was associated with greater distress than autologous or matched allogeneic transplant, F[1,228] = 4.67, p = .03); number of serious transplant-related complications (r = .13, p = .048); and physical functioning (r = −.45, p < .001). The most important of these variables were selected for entry into the final model by entering them in a simultaneous multiple regression predicting distress and retaining those that uniquely predicted distress at a conservative level of p < .25 (sex, income, age, and physical functioning).
Table 2.
Correlations between study variables (N = 230)
| Variables | 1 | 2 | 3 | Mean | SD | Range |
|---|---|---|---|---|---|---|
| 1.Distress | -- | −.09 | −.49*** | .47 | .41 | 0.00 – 2.27 |
| 2.Partner support quantity | -- | .50*** | 3.44 | .56 | 1.10 – 4.00 | |
| 3.Partner social support effectiveness | -- | 61.52 | 14.79 | 9.00 – 80.00 |
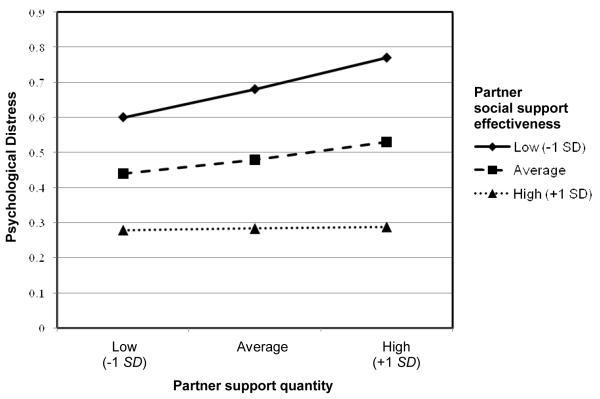
In the final model these control variables were entered in Step 1, partner support quantity was entered in Step 2, partner SSE was entered in Step 3, and the interaction between partner support quantity and partner SSE was entered in Step 4. As shown in Table 3, partner support quantity did not explain a significant proportion of variance in distress in Step 2, β = −.07, t = −1.20, p = .23. However, Step 3 results revealed that survivors reported significantly less distress when their partner provided more effective support, β = −.44, t = −6.74, p < .001. With partner SSE in the model, the parameter estimate for partner support quantity changed substantially, becoming a significant positive predictor of distress, β = .15, t = 2.46, p = .02. This finding suggests that the unique variance associated with receiving more partner support after partialling out variance associated with the effectiveness of that support was associated with greater distress. In addition, there was a significant interaction between partner support quantity and partner SSE, β = −.16, t = −2.64, p = .01. As illustrated in Figure 2, the amount of partner support received was not associated with distress when the support was highly effective (simple slope B = .01, SE = .06, t = .13, p = .90), whereas receiving more partner support was related to greater distress when the support was highly ineffective (simple slope B = .15, SE = .05, t = 3.20, p = .002). The positive association between partner support quantity and distress was marginally significant at average levels of partner SSE (simple slope B = .08, SE = .05, t = 1.71, p = .09). As is also clear in Figure 1, survivors who received more effective partner support reported significantly less distress than those who received less effective partner support, and this association was significant at all levels of partner support (all simple slopes ps < .001). Splitting the sample into high versus low partner support quantity and partner SSE using the midpoints of the two scales enabled us to compare distress scores for the 8% of the sample that reported receiving a high quantity of partner support that was appraised as being ineffective. Mean BSI-gsi in this subgroup was substantially higher (M = .90, SD = .55) than the mean BSI-gsi for the rest of the sample (M = .41, SD = .35). The effect size for this difference (Cohen’s d = 1.07) demonstrates the clinical significance of the elevated distress in this subgroup.
Table 3.
Multiple regression analysis predicting patients’ post-transplant distress (N = 230)
| Step 1 |
Step 2 |
Step 3 |
Step 4 |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | B | SE | B | SE | B | SE |
| Intercept | .39 | .03*** | .39 | .03*** | .44 | .03*** | .46 | .03*** |
| Femalea | .17 | .05*** | .17 | .05*** | .06 | .05 | .06 | .05 |
| Age | −.01 | .002** | −.01 | .002** | −.01 | .002** | −.01 | .002** |
| Income | −.02 | .01† | −.02 | .01 | −.02 | .01† | −.03 | .01* |
| Physical functioning | −.02 | .002*** | −.02 | .002*** | −.01 | .002*** | −.01 | .002*** |
| Partner support quantity | -- | -- | −.05 | .04 | .11 | .05* | .08 | .05 |
| Partner social support effectiveness (SSE) | -- | -- | -- | -- | −.01 | .002*** | −.01 | .002*** |
| Partner support quantity * Partner SSE | -- | -- | -- | -- | -- | -- | −.005 | .01** |
|
| ||||||||
| ΔF for step | 23.60*** | 1.43 | 45.37*** | 6.98* | ||||
| R2 for step | .30 | .00 | .12 | .02 | ||||
| F or full model | 24.53*** | |||||||
| R2 for full model | .44 | |||||||
p < .10.
p < .05.
p < .01.
p < .001
Coded 1 = female, 0 = male to indicate the survivor’s sex.
Figure 1.
Interaction between post-transplant partner social support effectiveness and partner support quantity predicting patient distress.
In addition, survivors reported more distress if they were younger, β = −.16, t = −3.06, p = .003, had a lower income, β = −.11, t = −2.22, p = .03, and reported worse physical functioning, β = −.33, t = −5.95, p < .001. An interesting finding was that in Steps 1 and 2 survivor sex was a significant predictor, such that women reported more distress than men. However, the effect of survivor sex became non-significant once partner SSE was added to the model, suggesting that women reported greater distress because, on average, they received less effective support from their partner compared to their male counterparts.
Discussion
We investigated partner support as a key resource that may help explain why some survivors suffer from enduring distress during a key psychological transition that takes place 1- to 3-years post-transplant, evaluating the usefulness of differentiating between the quantity of partner support and its effectiveness. Consistent with the SSE framework (Rini & Dunkel Schetter, 2010) and our past work (Rini et al., 2006), we defined partner SSE as emotional, informational, and instrumental support appraised by recipients as providing a good match for their needs in terms of their amount and type, not being difficult to obtain, being skillfully delivered, and not negatively influencing their self-concept. We found that receiving more effective partner support (versus receiving more support without reference to its effectiveness) predicted lower distress after controlling for potential sociodemographic and medical confounds. Furthermore, survivors who received a greater quantity of support from a partner who provided ineffective support reported higher distress than survivors who received partner support that represented other combinations of quantity and effectiveness. Receiving a greater quantity of ineffective support appears to have had adverse effects, perhaps because of greater exposure to ineffective support. This finding is notable in light of the fact that people with cancer often cope by seeking or accepting social support and are particularly likely to do so if they are experiencing greater stress as a result of their cancer (e.g., Deimling et al., 2006; Dunkel-Schetter, Feinstein, Taylor, & Falke, 1992).
The results of the present study are consistent with findings from Frick and colleagues (2006), who showed that negative support, although not as common as positive support, was more strongly associated with poor quality of life among people preparing for HSCT. It is also consistent with a broader literature showing that, compared to positive support, negative support is more strongly associated with recipient well-being (Franks et al., 1992; Pagel, Erdly, & Becker, 1987; Rook, 1984).
We should note that the measure of partner support quantity we used is well-validated and has provided valuable insights into support processes in the context of cancer (e.g., Manne et al., 2008; Manne & Schnoll, 2001; Rini et al., 2008). Yet, although the behaviors it assesses may often be provided effectively, that will not always be the case. For instance, household chores or errands completed by a partner may ease the recipient’s burden, but they may also fail to meet the survivor’s standards or they may be enacted in a way that communicates resentment. When support is provided ineffectively in these and other ways, receiving a greater quantity of support is unlikely to reduce distress and it may actually increase it, as suggested by our findings.
Implications for Interventions
It has been noted that cancer patients who do not have adequate social support would benefit from intervention to improve their support (Spiegel & Diamond, 2001). The SSE framework provides a theoretical basis to guide intervention development, and our findings suggest the potential value of using it to improve partner support for distressed HSCT survivors.
A central feature of the SSE framework is its recognition that the type of support most likely to match support recipients’ needs at any given time is not always apparent to support providers, much less to researchers or clinicians. Because open communication is the best way for providers to find out recipients’ support needs, interventions for couples coping with HSCT should include methods for enhancing communication. Our findings suggest that interventions may be particularly useful if they reduce the occurrence of ineffective partner support, although improving the effectiveness of support is also a worthy goal. It may be possible to adapt existing interventions that use cognitive-behavioral techniques to enhance communication and related skills in couples coping with cancer (e.g., Manne et al., 2007; Porter et al., 2009), refocusing them to address factors related to the appraised effectiveness of partner support (e.g., matching by quality or amount, or appraised difficulty of obtaining it; see Rini & Dunkel Schetter, 2010). For instance, partners could be trained to determine the support most likely to meet the survivor’s needs at a given time, and survivors could be trained to communicate their needs in a non-threatening manner.
Although good communication is likely to improve the extent to which the quality and quantity of support matches survivors’ needs, our research suggests that good communication may also enhance partner SSE through other pathways. Specifically, in our research with pregnant women we found that women appraised their partner’s support as more effective when they were more satisfied with their relationship and perceived it to be more intimate and equitable (Rini et al., 2006). To the extent that good communication enhances intimacy and other aspects of relationship quality (Porter, Keefe, Hurwitz, & Faber, 2005), improving couples’ communication may enhance survivors’ appraisals of the effectiveness of partner support both directly (by allowing couples to clarify each others’ support needs) and indirectly (by improving the perceived quality of the relationship).
There are other skills that should enable partners to provide more effective support, as shown by our research with a small sample of partners of pregnant women (Rini & Dunkel Schetter, 2010). For instance, we found that partners’ caregiving skills (e.g., their ability to recognize and interpret their partner’s needs, show appropriate physical affection, balance cooperation versus control when providing support, and avoid over-involvement; Kunce & Shaver, 1994) predicted women’s appraisals of the effectiveness of their support. Improving these types of skills may help partners enact difficult types of support more effectively.
Techniques to address cognitive processes should also be explored for enhancing the effectiveness of partner support. For instance, it may be useful to train survivors to reappraise problematic partner support in more favorable terms, recognizing the positive intent that motivates it (Bradbury & Fincham, 1992; McNulty & Karney, 2001). Acceptance-based approaches to couples therapy (e.g., Christensen et al., 2004; Jacobson et al., 2000) could be adapted for this purpose. Applying the SSE framework would require a focus on features of support most likely to contribute to survivors’ appraisals of the effectiveness of support provided to them (e.g., reasons why support may seem difficult to get).
It is important to note that different subgroups of couples may require different intervention approaches. For instance, there may be different dynamics in short-term versus long-term relationships that would affect how support needs are communicated and appraised as well as how they are fulfilled (e.g., Ray, 2006). Relationship duration is also likely to be confounded with the age of the survivor and partner, implicating issues surrounding the normative or non-normative nature of serious illness and the need for caregiving (which is likely to be more expected in older than younger couples).
In addition to addressing problems that reduce the effectiveness of partner support once these problems become apparent, it may also be possible to take a more preventive approach in couples at risk for the occurrence of ineffective partner support. This approach would involve screening for longstanding patterns of ineffective support or risk-related individual factors (e.g., dispositional characteristics that hinder provision or receipt of effective support, poor social skills) and/or relationship characteristics (e.g., poor relationship quality, intimacy, and equity; Rini et al., 2006). Intervening to address stable dispositional characteristics and longstanding relationship issues would most likely be unrealistic in this population. A more feasible approach would be to target problems caused by the novel and emotionally difficult challenges of transplant. This is not to say that pre-existing dispositional and relationship issues should be ignored. Interventions are likely to be more effective for individual couples if they address specific patterns of deficits that exist in the couple (e.g., skill-related versus situational).
Interventions for couples facing HSCT will need to minimize burden on these already-stressed couples. We have found that delivering interventions via telephone can be effective and is well-accepted (DuHamel et al., 2010). Any intervention targeting partners will also need to account for the emotional and practical challenges they face as caregivers. Research has shown a high degree of distress among partners (Bishop et al., 2007; Fife et al., 2009; Frick et al., 2005; Siston et al., 2001), and they may also be faced with providing care while coping with their own health issues. Training in coping skills that help partners manage these types of issues and mobilize support for themselves would be a promising addition to intervention approaches discussed above (Given, Given, & Kozachik, 2001).
Finally, there may be couples for whom it is not possible to improve the effectiveness of partner support, for instance, those with longstanding relationship difficulties. In such cases it might be possible to supplement partner support with support from others in the survivor’s intimate social network, such as friends or family members (Rini et al., 2008). Because it is not always the case that support from others can compensate for ineffective or negative partner support (Pistrang & Barker, 1995), research is needed to understand ways to circumvent negative effects of ineffective partner support that cannot be addressed.
Directions for Future Research
In addition to intervention development, there are other promising directions for future research. Studies that apply qualitative and/or observational methods would be useful for investigating the nature and qualities of support attempts that survivors find to be effective (or ineffective). Furthermore, research is needed to investigate whether findings from this research generalize to other populations. One population of interest would be patients undergoing solid organ transplant, who share some characteristics with HSCT patients (e.g., immunosuppression and associated risks) but not others (e.g., high dose chemotherapy used in HSCT). Social support processes similar to those described in the present study may occur among individuals receiving solid organ transplants, particularly if they face an extended recovery.
An additional avenue for research is investigation of behavioral outcomes (e.g., compliance with treatment and self-care regimens, healthcare utilization) and physical health outcomes (e.g., re-hospitalizations, relapse and other morbidities, mortality). Past research has revealed an association between social support and these types of outcomes, and some of it suggests a role for social support effectiveness. For instance, Rodrigue and colleagues (Rodrigue, Pearman, & Moreb, 1999) found that people with more “stable” pre-HSCT social support (defined in terms of the strength of the relationship between the patient and the caregiver and caregiver characteristics that would impede provision of effective support) were more likely to be alive post-transplant. Similarly, Frick and colleagues (Frick, Motzke, Fischer, Busch, & Bumeder, 2005) found that HSCT recipients who had reported more problematic pre-transplant support had a higher likelihood of dying after transplant. Research is needed to replicate these findings, investigate the role of partner SSE, and examine potential mediators.
Limitations and Strengths
We would like to note several limitations of this study. The first is its cross-sectional design, which makes it impossible to draw causal conclusions about the association between partner SSE and survivor distress. Further research is needed to replicate these findings with a prospective, longitudinal study design. A second limitation is the fact that the sample excludes individuals who are divorced or single. Therefore, findings may not apply to social support provided within highly distressed relationships or by caregivers other than partners. Third, many of our participants were non-Hispanic White, and many had moderate to high income and a post-high school education. Thus, findings may not apply to patients who are non-White or of lower socioeconomic status. However, evidence suggests that our sample approximates the population of HSCT recipients in terms of race/ethnicity (e.g., Joshua et al., 2010; Kollman et al., 2004), and economically disadvantaged patients may be generally underrepresented in HSCT populations because some will lack financial and supportive resources evaluated during pre-transplant screening (Hamadani, Craig, Awan, & Devine, 2010). Nonetheless, researchers should consider adjusting sampling methods to ensure more diverse samples. Finally, we assessed only the patient’s perspective. Future research on these processes would be most informative if the perspectives of both members of these couples are assessed. It should also account for the health of caregivers, many of whom may be coping with their own health problems.
The present study also had a number of important strengths, including its focus on social support from the most likely primary caregiver—the partner. In addition, it is one of the few studies to investigate social support actually received by transplant survivors (i.e., enacted support) rather than perceived available support, an approach that yields information highly relevant to the development of psychosocial interventions for transplant survivors. Overall, our findings highlight the value of studying partner support in a way that explicitly accounts for the extent to which it is a good match for survivors’ needs in terms of its quality and quantity, as defined by the social support effectiveness framework, with one notable finding being the identification of a group at risk for elevated post-transplant distress: survivors who receive a relatively large quantity of support from partners who are perceived to provide ineffective support. The importance of the quality of caregiving in transplant outcomes is increasingly recognized, as is the potential for stresses of transplant to adversely affect survivors, caregivers, and their relationship (Fife et al., 2009; Zabora, Smith, Baker, Wingard, & Curbow, 1992). Unfortunately, there is little research to guide development of psychosocial interventions that consider caregivers’ role in supporting the survivor during and after transplant. The present study provides a rich and valuable starting point for development of such interventions.
Acknowledgments
This study was supported by grant CA093609 from the National Cancer Institute. The authors would like to thank Julian Silva, Paul B. Greene, Catalina R. Lawsin, Anna Rusiewicz, Maria Nenova, and Jacob Stebel for their assistance with data collection.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/CCP
Contributor Information
Jane Austin, William Paterson University.
Catherine E. Mosher, Memorial Sloan-Kettering Cancer Center
Jack E. Burkhalter, Memorial Sloan-Kettering Cancer Center
Christine Dunkel Schetter, University of California at Los Angeles.
Katherine N. DuHamel, Memorial Sloan-Kettering Cancer Center
References
- Andrykowski MA, McQuellon RP. Bone marrow transplantation. In: Holland JC, editor. Psycho-oncology. Oxford University Press; New York, NY: 1999. pp. 289–299. [Google Scholar]
- Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Baumont JL, Brady MJ, Wingard JR. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. Journal of Clinical Oncology. 2005;23:599–608. doi: 10.1200/JCO.2005.03.189. doi:10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- Andrykowski MA, Cordova MJ, Hann DM, Jacobsen PB, Fields KK, Phillips G. Patients’ psychosocial concerns following stem cell transplantation. Bone Marrow Transplantation. 1999;24:1121–1129. doi: 10.1038/sj.bmt.1702022. doi: 10.1038/sj.bmt.1702022. [DOI] [PubMed] [Google Scholar]
- Bevans MF, Mitchell SA, Marden S. The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT) Supportive Care in Cancer. 2008;16:1243–1254. doi: 10.1007/s00520-008-0420-6. doi: 10.1007/s00520-008-0420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop MM. Psychosocial sequelae of hematopoietic cell transplantation in survivors and caregivers. Biology of Blood and Marrow Transplantation. 2008;15:29–32. doi: 10.1016/j.bbmt.2008.10.001. doi:10.1016/j.bbmt.2008.10.001. [DOI] [PubMed] [Google Scholar]
- Bishop MM, Beaumont JL, Hahn EA, Cella D, Andrykowski MA, Brady MJ, Wingard JR. Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. Journal of Clinical Oncology. 2007;25:1403–1411. doi: 10.1200/JCO.2006.07.5705. doi:10.1200/JCO.2006.07.5705. [DOI] [PubMed] [Google Scholar]
- Bradbury TN, Fincham FD. Attributions and behavior in marital interaction. Journal of Personality and Social Psychology. 1992;63:613–628. doi: 10.1037//0022-3514.63.4.613. doi:10.1037/0022-3514.63.4.613. [DOI] [PubMed] [Google Scholar]
- Broers S, Kaptein AA, Le Cessie S, Fibbee W, Hengeveld MW. Psychological functioning and quality of life following bone marrow transplantation: A 3-year follow-up study. Journal of Psychosomatic Research. 2000;48:11–21. doi: 10.1016/s0022-3999(99)00059-8. doi:10.1016/S0022-3999(99)00059-8. [DOI] [PubMed] [Google Scholar]
- Christensen A, Atkins DC, Berns S, Wheeler J, Baucom DH, Simpson LE. Traditional versus integrative behavioral couple therapy for significantly and chronically distressed married couples. Journal of Consulting and Clinical Psychology. 2004;72:176–191. doi: 10.1037/0022-006X.72.2.176. doi:10.1037/0022-006X.72.2.176. [DOI] [PubMed] [Google Scholar]
- Copelan EA. Hematopoietic stem-cell transplantation. New England Journal of Medicine. 2006;354:1813–1826. doi: 10.1056/NEJMra052638. doi:10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- Deimling GT, Wagner LJ, Bowman KF, Sterns S, Kercher K, Kahana B. Coping among older-adult, long-term cancer survivors. Psycho-Oncology. 2006;15:143–159. doi: 10.1002/pon.931. doi:10.1002/pon.931. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Spencer PM. The Brief Symptom Inventory (BSI): Administration, and Procedures Manual-I. Clinical Psychometric Research; Baltimore, MD: 1982. [Google Scholar]
- DuHamel KN, Mosher C, Winkel G, Labay L, Rini C, Meschian YM, Redd WH. Randomized clinical trial of telephone-administered cognitive behavioral therapy to reduce PTSD and distress symptoms after hematopoietic stem cell transplantation. Journal of Clinical Oncology. 2010 doi: 10.1200/JCO.2009.26.8722. Advance online publication. doi: 10.1200/JCO.2009.26.8722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel-Schetter C, Feinstein LG, Taylor SE, Falke R. Patterns of coping with cancer. Health Psychology. 1992;11:79–87. doi: 10.1037//0278-6133.11.2.79. doi:10.1037/0278-6133.11.2.79. [DOI] [PubMed] [Google Scholar]
- Eldredge DH, Nail LM, Maziarz RT, Hansen LK, Ewing D, Archbold PG. Explaining family caregiver role strain following autologous blood and marrow transplantation. Journal of Psychosocial Oncology. 2006;24:53–74. doi: 10.1300/J077v24n03_03. doi:10.1300/J077v24n03_03. [DOI] [PubMed] [Google Scholar]
- Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplantation. 2009;43:959–966. doi: 10.1038/bmt.2008.405. doi:10.1038/bmt.2008.405. [DOI] [PubMed] [Google Scholar]
- Franks P, Shields C, Campbell T, McDaniel S, Harp J, Botelho RJ. Association of social relationships with depressive symptoms: Testing an alternative to social support. Journal of Family Psychology. 1992;6:49–59. doi:10.1037/0893-3200.6.1.49. [Google Scholar]
- Frick E, Motzke C, Fischer N, Busch R, Bumeder I. Is perceived social support a predictor of survival for patients undergoing autologous peripheral blood stem cell transplantation? Psycho-oncology. 2005;14:759–770. doi: 10.1002/pon.908. doi: 10.1002/pon.908. [DOI] [PubMed] [Google Scholar]
- Frick E, Ramm G, Bumeder I, Schulz-Kindermann F, Tyroller M, Fischer N, Hasenbring M. Social support and quality of life of patients prior to stem cell or bone marrow transplantation. British Journal of Health Psychology. 2006;11:451–462. doi: 10.1348/135910705X53849. doi:10.1348/135910705X53849. [DOI] [PubMed] [Google Scholar]
- Frick E, Rieg-Appleson C, Tyroller M, Bumeder I. Social support, affectivity, and the quality of life of patients and their support-givers prior to stem cell transplantation. Journal of Psychosocial Oncology. 2005;23:15–34. doi: 10.1300/j077v23n04_02. doi:10.1300/J077v23n04_02. [DOI] [PubMed] [Google Scholar]
- Given BA, Given CW, Kozachik S. Family support in advanced cancer. CA: A Cancer Journal for Clinicians. 2001;51:213–231. doi: 10.3322/canjclin.51.4.213. doi:10.3322/canjclin.51.4.213. [DOI] [PubMed] [Google Scholar]
- Hamadani M, Craig M, Awan FT, Devine SM. How we approach patient evaluation for hematopoietic stem cell transplantation. Bone Marrow Transplantation. 2010 doi: 10.1038/bmt.2010.94. Advance online publication. doi:10.1038/bmt.2010.94. [DOI] [PubMed] [Google Scholar]
- Heinonen H, Volin L, Uutela A, Zevon M, Barrick C, Ruutu T. Quality of life and factors related to perceived satisfaction with quality of life after allogeneic bone marrow transplantation. Annals of Hematology. 2001;80:137–143. doi: 10.1007/s002770000249. doi:10.1007/s002770000249. [DOI] [PubMed] [Google Scholar]
- Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S, Henslee-Downey J. Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. Journal of Psychosocial Oncology. 2007;25:87–101. doi: 10.1300/J077v25n01_05. doi:10.1300/J077v25n01_05. [DOI] [PubMed] [Google Scholar]
- Hoodin F, Harper FW, K., Posluszny DM. Psychological care of adult allogeneic transplant patients. In: Lazarus HM, Laughlin MJ, editors. Allogeneic Stem Cell Transplantation. Springer; Totowa, NJ: 2010. pp. 619–656. doi: 10.1007/978-1-59745-478-0_35. [Google Scholar]
- Jacobsen PB, Sadler IJ, Booth-Jones M, Soety E, Weitzner MA, Fields KK. Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. Journal of Consulting and Clinical Psychology. 2002;70:235–240. doi: 10.1037//0022-006x.70.1.235. doi:10.1037/0022-006X.70.1.235. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: An acceptance-based, promising new treatment for couple discord. Journal of Consulting and Clinical Psychology. 2000;68:351–355. doi: 10.1037//0022-006x.68.2.351. doi:10.1037/0022-006X.68.2.351. [DOI] [PubMed] [Google Scholar]
- Jenks Kettmann JD, Altmaier EM. Social support and depression among bone marrow transplant patients. Journal of Health Psychology. 2008;13:39–46. doi: 10.1177/1359105307084310. doi:10.1177/1359105307084310. [DOI] [PubMed] [Google Scholar]
- Joshua TV, Rizzo JD, Zhang MJ, Hari PN, Kurian S, Pasquini M, Majhail NS, Horowitz MM. Access to hematopoietic stem cell transplantation: Effect of race and sex. Cancer. 2010;116:3469–3476. doi: 10.1002/cncr.25297. doi: 10.1002/cncr.25297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH. The use of the nitrogen mustards in the palliative treatment of carcinoma. Cancer. 1948;1:634–656. doi:10.1002/1097-0142(194811)1:4<634::AID-CNCR2820010410>3.0.CO;2-L. [Google Scholar]
- Keogh F, O’Riordan J, McNamara C, Duggan C, McCann SR. Psychosocial adaptation of patients and families following bone marrow transplantation: A prospective, longitudinal study. Bone Marrow Transplantation. 1998;22:905–911. doi: 10.1038/sj.bmt.1701443. doi:10.1038/sj.bmt.1701443. [DOI] [PubMed] [Google Scholar]
- Kollman C, Abella E, Baitty RL, Beatty PG, Chakraborty R, Christiansen CL, Nyman JA. Assessment of optimal size and composition of the U.S. National Registry of Hematopoietic Stem Cell Donors. Transplantation. 2004;78:89–95. doi: 10.1097/01.tp.0000132327.40702.97. doi: 10.1097/01.TP.0000132327.40702.97. [DOI] [PubMed] [Google Scholar]
- Kunce LJ, Shaver PR. An attachment-theoretical approach to caregiving in romantic relationships. In: Bartholomew K, Perlman D, editors. Advances in Personal Relationships. Vol. 5. Jessica Kingsley Publishers; London: 1994. pp. 205–237. [Google Scholar]
- Lee SJ. Quality of life issues post-transplantation. In: Soiffer RJ, editor. Hematopoietic Stem Cell Transplantation. Humana Press; Totowa, NJ: 2008. pp. 537–559. doi: 10.1007/978-1-59745-438-4. [Google Scholar]
- Manne S, Rini C, Rubin S, Rosenblum N, Bergman C, Edelson M, Rocereto T. Long-term trajectories of psychological adaptation among women diagnosed with gynecological cancers. Psychosomatic Medicine. 2008;70:677–787. doi: 10.1097/PSY.0b013e31817b935d. doi:10.1097/PSY.0b013e31817b935d. [DOI] [PubMed] [Google Scholar]
- Manne S, Rubin S, Edelson M, Rosenblum N, Bergman C, Hernandez E, Winkel G. Coping and communication-enhancing intervention versus supportive counseling for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2007;75:615–628. doi: 10.1037/0022-006X.75.4.615. doi:10.1037/0022-006X.75.4.615. [DOI] [PubMed] [Google Scholar]
- Manne S, Schnoll RA. Measuring supportive and unsupportive responses to cancer treatment: A factor analysis of the Partner Responses to Cancer Inventory. Journal of Behavioral Medicine. 2001;24:297–321. doi: 10.1023/a:1010667517519. doi: 10.1023/A:1010667517519. [DOI] [PubMed] [Google Scholar]
- McNulty JK, Karney BR. Attributions in marriage: Integrating specific and global evaluations of a relationship. Personality and Social Psychology Bulletin. 2001;27:943–955. doi:10.1177/0146167201278003. [Google Scholar]
- McQuellon RP, Russell GB, Rambo TD, Craven BL, Radford J, Perry JJ, Hurd DD. Quality of life and psychological distress of bone marrow transplant recipients: The ‘time trajectory’ to recover over the first year. Bone Marrow Transplantation. 1998;21:477–486. doi: 10.1038/sj.bmt.1701115. doi:10.1038/sj.bmt.1701115. [DOI] [PubMed] [Google Scholar]
- Molassiotis A, van den Akker OB, Boughton BJ. Perceived social support, family environment and psychosocial recovery in bone marrow transplant long-term survivors. Social Science and Medicine. 1997;44:317–325. doi: 10.1016/s0277-9536(96)00101-3. doi:10.1016/S0277-9536(96)00101-3. [DOI] [PubMed] [Google Scholar]
- Mosher CE, Redd WH, Rini C, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: A review of the literature. Psycho-Oncology. 2009;18:113–127. doi: 10.1002/pon.1399. doi:10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagel MD, Erdly WW, Becker J. Social networks: We get by with (and in spite of) a little help from our friends. Journal of Personality and Social Psychology. 1987;53:793–804. doi: 10.1037//0022-3514.53.4.793. doi:10.1037/0022-3514.53.4.793. [DOI] [PubMed] [Google Scholar]
- Pistrang N, Barker C. The partner relationship in psychological response to breast cancer. Social Science and Medicine. 1995;40:789–797. doi: 10.1016/0277-9536(94)00136-h. doi:10.1016/0277-9536(94)00136-H. [DOI] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Hurwitz H, Faber M. Disclosure between patients with gastrointestinal cancer and their spouses. Psychooncology. 2005;14:1030–1042. doi: 10.1002/pon.915. doi:10.1002/pon.915. [DOI] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Baucom DH, Hurwitz H, Moser B, Patterson E, Kim HJ. Partner-assisted emotional disclosure for patients with gastrointestinal cancer: Results from a randomized controlled trial. Cancer. 2009;115(18 suppl):4326–4338. doi: 10.1002/cncr.24578. doi: 10.1002/cncr.24578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray M. Informal care in the context of long-term marriage: The challenge to practice. Practice. 2006;18:129–142. doi: 10.1080/09503150600760173. [Google Scholar]
- Rini C, Dunkel Schetter C. The effectiveness of social support transactions in intimate relationships. In: Davila J, Sullivan K, editors. Support Processes in Intimate Relationships. Oxford; New York, NY: 2010. pp. 26–67. [Google Scholar]
- Rini C, Dunkel Schetter C, Glynn LM, Hobel C, Sandman CA. Effective social support: Antecedents and consequences of partner support during pregnancy. Personal Relationships. 2006;13:207–229. doi:10.1111/j.1475-6811.2006.00114.x. [Google Scholar]
- Rini C, Manne S, DuHamel KN, Austin J, Ostroff J, Boulad F, Redd WH. Social support from family and friends as a buffer of low spousal support among mothers of critically ill children: A multilevel modeling approach. Health Psychology. 2008;27:593–603. doi: 10.1037/0278-6133.27.5.593. doi:10.1037/0278-6133.27.5.593. [DOI] [PubMed] [Google Scholar]
- Rizzo JD, Wingard JR, Tichelli A, Lee SJ, Van Lint MT, Burns L, J., Socié G. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Biology of Blood and Marrow Transplantation. 2006;12:138–151. doi: 10.1016/j.bbmt.2005.09.012. doi:10.1016/j.bbmt.2005.09.012. [DOI] [PubMed] [Google Scholar]
- Rodrigue JR, Pearman TP, Moreb J. Morbidity and mortality following bone marrow transplantation: Predictive utility of pre-BMT affective functioning, compliance, and social support stability. International Journal of Behavioral Medicine. 1999;6:241–254. doi: 10.1207/s15327558ijbm0603_3. doi: 10.1207/s15327558ijbm0603_3. [DOI] [PubMed] [Google Scholar]
- Rook KS. The negative side of social interaction: impact on psychological well-being. Journal of Personality and Social Psychology. 1984;46:1097–1108. doi: 10.1037//0022-3514.46.5.1097. doi:10.1037/0022-3514.46.5.1097. [DOI] [PubMed] [Google Scholar]
- Rusiewicz A, DuHamel KN, Burkhalter J, Ostroff J, Winkel G, Scigliano E, Papadopoulos E, Siston A. Psychological distress in long-term survivors of hematopoietic stem cell transplantation. Psychooncology. 2008;17:329–337. doi: 10.1002/pon.1221. doi: 10.1002/pon.1221. [DOI] [PubMed] [Google Scholar]
- Siston AK, List MA, Daugherty CK, Banik DM, Menke C, Cornetta K, Larson RA. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplantation. 2001;27:1181–1188. doi: 10.1038/sj.bmt.1703059. doi:10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Diamond S. Psychosocial interventions in cancer: Group therapy techniques. In: Baum A, Andersen BL, editors. Psychosocial interventions for cancer. American Psychological Association; Washington, DC: 2001. pp. 215–233. doi:10.1037/10402-012. [Google Scholar]
- Stetz KM, McDonald JC, Compton K. Needs and experiences of family caregivers during marrow transplantation. Oncology Nursing Forum. 1996;23:1422–1427. Retrieved from http://ons.metapress.com/content/0190-535X/ [PubMed] [Google Scholar]
- Syrjala KL, Chapko MK, Vitaliano PP, Cummings C, Sullivan KM. Recovery after allogeneic marrow transplantation: A prospective study of predictors of long-term physical and psychosocial functioning. Bone Marrow Transplantation. 1993;11:319–327. Retrieved from http://eresources.library.mssm.edu:2072/bmt/index.html. [PubMed] [Google Scholar]
- Syrjala KL, Kurland BF, Abrams JR, Sanders JE, Heiman JR. Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood. 2008;111:989–996. doi: 10.1182/blood-2007-06-096594. doi: 10.1182/blood-2007-06-096594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers ME, Martin PJ. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–2343. doi: 10.1001/jama.291.19.2335. doi:10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- Wells KJ, Booth-Jones M, Jacobsen PB. Do coping and social support predict depression and anxiety in patients undergoing hematopoietic stem cell transplantation. Journal of Psychosocial Oncology. 2009;27:297–315. doi: 10.1080/07347330902978947. doi:10.1080/07347330902978947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingard JR, Curbow B, Baker F, Piantadosi S. Health, functional status and employment of adult survivors of bone marrow transplant. Annals of Internal Medicine. 1991;114:113–118. doi: 10.7326/0003-4819-114-2-113. Retrieved from http://www.annals.org/ [DOI] [PubMed] [Google Scholar]
- Wingard JR, Vogelsang GB, Deeg HJ. Stem cell transplantation: supportive care and long-term complications. Hematology. 2002:422–444. doi: 10.1182/asheducation-2002.1.422. Retrieved from http://asheducationbook.hematologylibrary.org/ [DOI] [PubMed] [Google Scholar]
- Widows MR, Jacobsen PB, Fields KK. Relation of psychological vulnerability factors to posttraumatic stress disorder symptomatology in bone marrow transplant recipients. Psychosomatic Medicine. 2000;62:873–882. doi: 10.1097/00006842-200011000-00018. Retrieved from http://www.psychosomaticmedicine.org/ [DOI] [PubMed] [Google Scholar]
- Zabora JR, Smith ED, Baker F, Wingard JR, Curbow B. The family: The other side of bone marrow transplantation. Journal of Psychosocial Oncology. 1992;10:35–46. doi: 10.1300/J077v10n01_0. [Google Scholar]