Abstract
Acupuncture has been used for millennia in traditional Chinese medicine as a technique believed to restore the balance of energy in the body caused by disease through the use of needles inserted into specific points or energy channels. This energy is called the De qi. The use of acupuncture for the treatment of pain in musculoskeletal disorders is increasing. Some patients seek alternative therapies because of lack of improvement with conventional treatments. The potential physiological effects of acupuncture on pain relief have been attributed to biochemical processes such as the release of endorphins into the limbic structures, subcortical areas and brain stem, mechanisms that are also present in placebo-induced analgesia. In addition, pain relief with acupuncture is also associated with patient expectations, beliefs and interactions with their acupuncturists. In this review, we summarize the latest evidence on the treatment of musculoskeletal conditions including rheumatoid arthritis, fibromyalgia, neck pain, shoulder pain, low back pain and knee pain with traditional Chinese acupuncture (TCA), electroacupuncture (EA), and the use of moxibustion. Acupuncture is relatively safe but there are still reports of serious and fatal side effects that must be taken into account when recommending this therapy. Many of the latest trials assessing the benefits of acupuncture in rheumatic diseases found that acupuncture was not better than sham acupuncture implying that the analgesic effects observed are related to a strong placebo response. While the literature on this topic is extensive, many of the studies lack methodological rigor, and additional large, well-controlled, high quality trials are still needed to determine if acupuncture might be useful in the treatment of chronic rheumatic diseases.
Keywords: Acupuncture, Rheumatic diseases, Treatment, Rheumatoid arthritis, Fibromyalgia, Osteoarthritis, Neck pain, Shoulder pain, Knee pain, Low back pain
Introduction
Acupuncture was developed in ancient China, with pictographs dating from the Shang Dynasty (1600–1100 BC) which suggest that it was already practiced at that time [1]. Its first written description appears in the Yellow's Emperor's Classic of Medicine 200 BC. In traditional Chinese medicine (TCM), health is seen as the result of the balance of energy, called qi in the body. When this energy is imbalanced, health is compromised and disease occurs. It is believed that qi flows through channels or meridians and that the insertion of needles along these meridians (acupuncture) restores the energy balance, hence the health, to the individual [2]. When performing traditional Chinese acupuncture (TCA), the acupuncturist inserts hair thin needles into specific acupuncture points along meridians specific for each condition. Manual stimulation is then performed in an attempt to have the patient feel de qi, a sensation of tingling, numbness, heaviness and/or mild soreness. In TCM, eliciting a positive de qi response indicates that location of the appropriate energy channel has been successful. Once de qi is found the needles are left in place between 20-40 minutes. De qi might be elicited more than once in each point during an acupuncture session [3]. The use of electroacupuncture (EA), a technique increasingly being adopted by traditional acupuncturists, aims to increase the de qi sensation. Moxibustion is another technique that has been used in conjunction with acupuncture in TCM, using moxa or mugwort herb (Artemisa vulgaris). In moxibustion, sticks of moxa can be applied directly on the skin or with acupuncture needles along meridian points, and are burnt to warm the area and stimulate blood flow and qi.
Acupuncture is increasingly being used as a complementary therapy in the Western world. In 2002, the National Health Interview Survey found that 4.1% of the respondents reported using acupuncture in their lifetime, suggesting by extrapolation, that 8 million of Americans had used this therapy (2 million in the previous year). Back pain was the most common reason for its use (34%), followed by joint pain (16%) and neck pain (13.6%); conditions such as arthritis, gout, lupus and fibromyalgia were grouped together and represented 6.5% of acupuncture use. Participants were asked if they felt that acupuncture helped with their condition: 46.3% stated that acupuncture “helped a great deal”, 25.8% had “some help”, 14.6% had “only a little help” and 13.4% felt that acupuncture did “not help at all”[4], which demonstrates that most people receiving acupuncture believe it has been effective for them. In 2007, [5] the National Health Interview Survey estimated that 4 out of 10 adults in the United States used complementary and alternative medicine. Compared to 2002 [4], the use of acupuncture increased by 31%.
While acupuncture in TCM it has been used for the treatment of many disorders, in this review, we examine its use for pain relief in musculoskeletal diseases, which are mostly chronic. We conducted a literature search in Medline, EMBASE and Cochrane Library of articles in English, French, German and Spanish, published between January 2007 and July 2012, on the most recent evidence on the use of acupuncture in rheumatic conditions including rheumatoid arthritis (RA), fibromyalgia, neck pain, shoulder pain, low back pain and knee pain. We review below some of the methodological issues related to the robustness of the acupuncture literature, potential safety concerns, mechanistic pathways of acupuncture-induced analgesia and current data on the specific conditions listed above.
The clinical effects of acupuncture: methodological considerations
Many randomized controlled trials (RCT) evaluating acupuncture have insufficient methodological quality [6-11]. A major challenge in these studies is the choice of an adequate placebo control [12, 13]. A common control procedure has been the use of sham acupuncture where needles are inserted on either meridians not specific for the condition under study, or in areas outside meridians; often this is coupled with a more superficial needle insertion than what is performed in the true acupuncture group. However, there is concern that this technique may not be physiologically inert, and that even the most superficial needling on non-meridian points could cause a chemical and physiological reaction in subjects similar or identical to that of true acupuncture [14]. A different acupuncture placebo modality includes the use Streitberger needles [15], which are retractable, and although they attach to the skin they do not penetrate it. It has been suggested that even only touching the skin might provide a stimulus and therefore not be an inert action [16]. Another common critique to the Streitberger needle is that patients might be able to discern that they are in a placebo group because of lack of sensation. This is particularly true for those patients who had acupuncture in the past and can recognize a De qi sensation which is not likely to happen with retractable needles. This is one reason patients with previous acupuncture therapy are excluded from most acupuncture trials. Some acupuncture trials include 3 arms: real acupuncture, sham/placebo acupuncture and standard medical care or control group with waiting list [16]. In many trials a benefit of acupuncture over the standard care control group is observed, but no differences are observed when compared to the sham acupuncture group raising doubts as to whether the effect of acupuncture is no more than placebo, or if the sham procedure has a physiological effect that is indistinguishable from true acupuncture, and therefore therapeutically active [17].
Healthcare encounters are complex and rely on multiple components including the therapeutic ritual, patients' and providers' beliefs, attitudes, preferences and expectations which can result in positive effects, even when patients are given an inert intervention (placebo) [18]. Linde et al. conducted a meta-analysis of 37 RCTs evaluating acupuncture and compared sham acupuncture to no acupuncture (nonspecific effect) and sham acupuncture to real acupuncture (specific effect). Sham acupuncture was more effective than no acupuncture, and real acupuncture was more effective than sham acupuncture. Interestingly, the effect size was larger for the non-specific effects than the specific ones, suggesting that a large component of the response to acupuncture is due these non-specific effects, possibly placebo. Overall the meta-analysis only found a small to moderate specific effect of acupuncture over sham, and trials with large sample sizes and low risk of bias yielded less positive results.
A few experimental studies have evaluated the role of the communication between recipients of acupuncture and their acupuncturists, and the resulting expectations, on the response to therapy. In one RCT [19], traditional acupuncture with electrostimulatiton was compared to sham acupuncture in patients with knee osteoarthritis (OA) while experimentally manipulating the communication styles of the acupuncturists. While no differences were observed between the true acupuncture and sham control groups, patients who interacted with acupuncturists who delivered high expectations statements (e.g. “I think this will work for you”) had less pain and increased satisfaction at the end of the study than those who interacted with acupuncturists delivering neutral expectations (e.g. “It may or may not work for you”). Traditional acupuncture was not more effective than the use of superficial sham acupuncture in non-meridian points but the acupuncturists' communication style had a significant effect on pain reduction and satisfaction, suggesting that these effects mediate placebo responses [19].
A meta-analysis [20] of four acupuncture trials for different conditions that measured expectations showed a significant association between higher outcome expectations and subsequent improvement. Unfortunately, most RCTs of acupuncture have not controlled or adjusted for the effect of communication style of acupuncturists, which can create expectations of benefit that can clearly result in improved outcomes in patients receiving more positive communication about potential therapeutic effects.
Safety of acupuncture
While there is a perception that acupuncture is generally safe, in a recent review by Ernst [21] of acupuncture trials published from 2000 until 2009 including a total of 57 systematic reviews without language restriction, serious adverse events were reported: 95 cases were found in the categories of trauma, infection and other causes. Thirty eight cases of infection were found; bacterial infections were the most common and responded well to antibiotics. Forty two cases of organ trauma were found. The most common traumatic complication was pneumothorax. Most patients recovered but 4 patients died due to pneumothorax. A total of 5 patients from different ages groups were reported as dead, although they had consulted their acupuncturist for minor complains. In another review, Ernst and Zhang [22] also found that 26 cases of cardiac tamponade secondary to acupuncture have been reported in the literature up to January 2010 and that in 14 cases this complication was fatal. So although acupuncture is often considered without risk to patient safety, it is important to recognize that serious adverse events, including death can occur, and moreover, that these events might be underreported [22].
Analgesic effects of acupuncture
Different hypotheses have been proposed to explain the analgesic effects of acupuncture on the basis of animal and human studies. These effects are complex and likely the result of the interplay between neurochemical, physiologic and psychologic factors related to patients' expectations of benefit [19, 23-35]. Moreover, many of the findings observed in mechanistic studies of acupuncture, have also been reported as effects of the placebo response.
There is evidence supporting the role of endogenous opioids (encephalin, dynorphin, β-endorphin and endomorphin) and serotonin (5-HT) in acupuncture-mediated analgesia. Mayer et al. [23] and Pomeranz et al. [24] showed that acupuncture-induced analgesia is blocked by naloxone in mice and in humans, supporting the role of endogenous opioids.
Functional brain studies demonstrate activation of structures in the brain and brain stem involved in pain pathways with acupuncture needling and many also show similar patterns, sometimes with lower intensity with sham procedures, such as superficial needle penetration, non-meridian needling, or use of retractable needles (which attach to the skin but do not penetrate it). Studies with positron emission tomography (PET) have shown increments in the binding of μ opioids to receptors in the brain after several days of acupuncture [25]. With acupuncture treatment, functional magnetic resonance imaging (fMRI) demonstrates activation of the basal anterior brain, limbic system and other areas of the brain related to affective and somatosensory functions [26].
Expectations and patient's beliefs play a significant role in the modulations of pain perception [27, 35]. Pariente et al. [27] studied the response of the brain to needling with real acupuncture, placebo sham acupuncture (retractable needle) and skin prick (overt placebo group with patients being told this was an inert intervention) in a single blind randomized crossover design including 14 patients with osteoarthritis which also examined the effects of patients' expectations. Patients experienced only mild relief of their pain during real acupuncture and placebo acupuncture but no relief with the overt placebo. PET scans showed a higher degree of activation in the insula ipsilateral to the stimulated side during real acupuncture than with sham acupuncture. Interestingly, they also noticed than when patients expected they would receive real acupuncture the dorsolateral prefrontal cortex, the rostral anterior cingulated cortex and the midbrain were activated; these areas are involved in pain modulation and reward expectation. When assessing the retractable needle group in comparison to the overt placebo group (no expectations of improvement) there was also activation of the dorsolateral prefrontal cortex, the rostral anterior cingulated cortex and midbrain implying that placebo responses participate in acupuncture-induced analgesia, painful stimuli and the anticipation of pain can activate the dorsolateral prefrontal cortex resulting in pain relief possibly by activating the opioid system in the midbrain as a “top-down effect” [28,29]. The activation of the rostral anterior cingulate cortex which is linked to pain perception could also modulate the experience of pain through dopaminergic pathways involved in expectation and reward effects [30]. These effects have also been shown to play a role in placebo-induced and opioid-induced analgesia [29, 31].
In an experimentally-induced pain study, Kong et al. [35] compared the analgesic effects of verum and sham acupuncture in subjects conditioned to either positive or neutral expectations of analgesia. They found that for subjects with high expectations, the magnitude of the analgesic response was similar in verum and sham groups. However, the expected fMRI signal decreased in the brain seen with analgesia was more extensive in those subjects receiving verum compared to those who received sham.
As can be seen, the potential effects of acupuncture on pain are complex and often difficult to separate from placebo responses. Better quality RCTs including various control groups, and incorporating neurochemical and neurofunctional studies are needed to further elucidate and quantify the specific analgesic effects of acupuncture.
The efficacy of acupuncture for specific rheumatic conditions
In the following sections we review the latest evidence for efficacy of acupuncture in selected rheumatic disorders. We describe the results of the available systematic reviews and, in addition, any other recent RCTs.
Rheumatoid Arthritis
The evidence for the efficacy of acupuncture in the treatment of RA is sparse and inconclusive. A few systematic reviews have been published evaluating RCTs of acupuncture in RA patients. A 2005 [10] Cochrane review included 2 RCTs [36, 37] examining the effects of TCA and EA on disease activity in 84 patients with RA. There was no statistically significant benefit of acupuncture compared to the control intervention on pain, patient global assessment, number of swollen or tender joints, and erythrocyte sedimentation rate (ESR) or C - reactive protein (CRP) levels. The conclusions were limited because of the poor methodological quality of the studies and small sample size.
In a more recent review, Lee et al. [38] included 8 RCTs of patients with RA treated with acupuncture with or without electrical stimulation or moxibustion. Five trials were from China and one each from Canada, Brazil and the United Kingdom [36, 37, 39, 40-44]. Two trials used penetrating sham acupuncture in non-acupuncture points [36, 39], one trial used sham acupuncture in acupuncture points [38], one used non penetrating acupuncture on acupuncture points [37], and conventional drug comparators were used in 4 trials [41-44]. The trials were heterogeneous and not all of them were double blinded [36, 39, 40]. Drop-outs according to group allocation were only provided in 3 RCT [36, 39, 40]. None of the RCT reported whether they had succeeded in blinding the patients. Overall, no statistically significant differences were observed between TCA, EA or moxibustion, and the control interventions. Most of the positive trials were conducted in China, and it has been shown that many of the Chinese trials evaluating acupuncture have poor methodological quality [45]. Another systematic review which included the same studies also failed to show a benefit of acupuncture in any modality when compared to control groups [46].
At this time, the use of acupuncture in RA is not supported by the evidence available. The published RCTs were underpowered, and their methodological quality was not optimal.
Fibromyalgia
After osteoarthritis, fibromyalgia is the second most common rheumatological condition in the United States (US) affecting between 2-4% of the population [47]. A 12 week double blinded RCT in 100 patients with fibromyalgia [48] compared TCA with 3 control interventions: TCA for an unrelated condition; sham acupuncture in non-specific acupuncture points and non-penetrating needling. The primary outcome was pain using a visual analogue scale (VAS) at 1, 4, 8, 12 weeks, 3 and 6 months after treatment. No statistically significant differences were found among groups.
A 2007 systematic review [49] pooled data from 5 RCTs which evaluated acupuncture as a co-intervention along with conventional therapy in 316 patients with fibromyalgia. Three RCTs were found to have positive results [50-52] including 2 of the better quality studies [50, 51]. EA was used in 2 trials [50, 52] while TCA was used in 3 trials [51, 53, 54]. Although pain scores improved, this effect lasted less than 6 weeks in one trial [50] but up to 7 months in the other [51]. The other 2 RCTs showed not benefit of acupuncture over sham acupuncture [53] or over the control group [54].
A more recent review in 2010 [55] included 7 RCTs [25, 50, 51, 53, 54, 56, 57] with 385 patients and the median number of treatment courses was 9 (range 6-25). The outcomes analyzed were pain, fatigue, sleep disturbances, physical function and adverse events. A small analgesic effect was found with acupuncture treatment but it was not maintained at follow up (on average at week 26). A subgroup analysis found that the significant decrease in pain occurred more frequently in RCTs where individualized TCA and EA were used. There was no difference in the results when stratified according to the use of penetrating versus non-penetrating sham acupuncture.
Most RCTs finding beneficial results had small sizes and unclear or high risk of bias (inappropriate randomization or concealment of allocation or blinding). The studies with less bias reported no difference in pain between active and control groups. There was no evidence to support efficacy for other outcomes including fatigue, sleep disturbances, or physical function. Given these results, there is insufficient evidence to recommend acupuncture for the treatment of fibromyalgia.
Neck Pain
A recent National Health Interview Survey estimated that 38% of individuals with chronic neck pain in the United States used complementary and alternative medicine including acupuncture [4, 5]. Even though the use of acupuncture for neck pain has increased over the years, its efficacy remains to be proved [4, 5].
A 2010 Cochrane review examined the efficacy of acupuncture for chronic neck pain [8]. The review included 10 trials [58-68] with a total of 661 patients. There was a moderate statistically significant improvement of pain in patients receiving acupuncture compared to those in the sham interventions and waiting list group (pooled standardized mean difference (SMD) -0.37, 95% confidence interval (CI) 0.61 to -0.12). Moderate evidence of benefit was also found for acupuncture in the treatment of patients with chronic neck disorders with radicular symptoms when comparing to waiting list control at short-term follow-up (less than 3 months). Based on this review there was some evidence of efficacy with acupuncture for chronic neck pain in the short-term.
A recently published systematic review [93] included 29 high quality RTCs with a total of 17922 patients with neck or back pain, shoulder pain, osteoarthritis and chronic headache from the United States, United Kingdom, Germany, Spain and Sweden. This review however, excluded many of the trials included in the meta-analysis described above. For nonspecific musculoskeletal pain (neck or back) the effect size when comparing acupuncture versus sham acupuncture was 0.37 (95% CI, 0.27-0.46). Suggesting modest efficacy of acupuncture for the treatment of neck and back pain.
Shoulder pain
Shoulder pain is a common complaint in primary care settings. Prevalence studies indicate that 16 to 34% of the general population has suffered from shoulder pain [68]. A 2008 Cochrane review [9] included 9 trials evaluating acupuncture for shoulder pain [69-77]. The description of the interventions was poor in most of the studies. For rotator cuff disease there was no significant difference between active groups or placebo. For shoulder function, a statistically significant improvement of 17.3 (95% CI 7.79-26.81) was observed in the 100-point Constant Murley scale after 4 weeks of treatment in patients treated with acupuncture compared to controls. Results were no longer significant - by month 4. Based on this review, the authors concluded that there was not enough evidence to either recommend or refute acupuncture for chronic (more than 3 weeks duration) shoulder pain, and that better quality RCTs were needed.
Published after the Cochrane review [78], the German Randomized Acupuncture Trial for chronic shoulder pain (GRASP) trial, evaluated 424 patients with chronic shoulder pain (more than 6 weeks) with a VAS pain score of more than 50 mm. Participants were randomly assigned to TCA, sham acupuncture (superficial needling in non-acupuncture points) or conservative treatment (physiotherapy, physical exercise, heat and cold therapy and TENS). Patients in the acupuncture and sham groups were blinded to treatment; they received 15 treatments over 6 weeks. The primary outcome was 50% improvement in VAS pain score after the completion of treatment and 3 months later. A statistically significant difference was found in all outcomes. At completion of treatment, the percentages of responders were: for TCA 68% (95% CI 58–77%), for sham 40% (95% CI 27–53%), and for the conservative treatment 28% (95% CI 14–42%). After 3 months, these percentages respectively were 65%, 24%, and 37%. TCA was statistically significantly superior to sham and conservative treatment (p < 0.01). This Study had some limitations; the success of blinding in the acupuncture groups was not reported. In addition, by 3 months 27% of the patients were lost to follow up.
While the results of this last trial may be promising, the prior Cochrane systematic review including 9 trials did not show clear efficacy.
The more recent meta-analysis mentioned in the neck pain section [93] pooled data from only 3 RCTs (versus 10 in the Cochrane review) including this last German trial [78] and found a statistically significant difference between acupuncture for the treatment of chronic shoulder pain (more than 4 weeks duration): 0.62 (95% CI, 0.46-0.77).
Low back pain
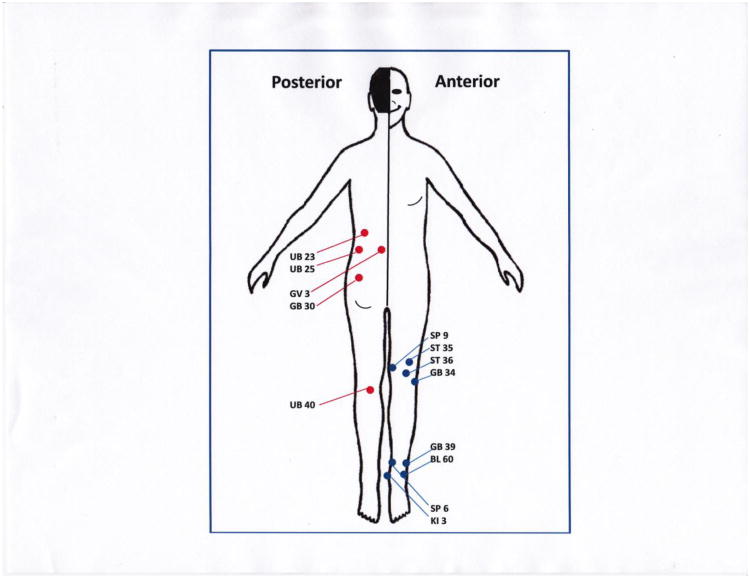
Back pain is the most common reason in the United States to visit an acupuncturist [79]. Figure 1 shows the most common acupuncture points used for treatment of low back pain (in red; for knee pain in blue). Most episodes of back pain resolve on their own but up to 7% of patients develop pain that lasts more than 6 weeks [80]. Acupuncture for the treatment of low back pain has been reviewed more extensively than for any other musculoskeletal disorders. A 2005 meta-analysis [81] of 22 RCTs in patients with chronic low back pain (more than 3 months) showed a small but statistically significant difference in pain scores in short and longer-term follow-up (6 weeks on average) when comparing TCA with sham acupuncture, sham TENS or placebo controls. However, acupuncture was not better than active controls receiving standard therapy or other physical therapies such as manipulation or massage.
Figure 1.
Schematic representation of acupuncture of the more common low back pain points used and some of the more common knee pain points used. Knee points in blue. ST: Stomach meridian, GB: Gall bladder meridian, BL: bladder meridian, KI: kidney meridian and SP: spleen meridian, UB: urinary bladder. These points were obtained as an approximated reference of the most common acupuncture points from the Chinese Acupuncture and Moxibustion [90] and from Acupuncture: A Comprehensive Text [91]. Low back pain points in red. These points were adapted as an approximated reference of the most common acupuncture points used for low back pain from Cheng [92] in Chinese acupuncture and moxibustion.
The 2007 German Acupuncture Trials for Chronic Low Back pain (GERAC) [82] included 1162 patients randomly assigned to TCA (10 sessions with up to 5 more sessions if a partial response was attained were offered), sham acupuncture (superficial needling at non-acupuncture points) and guideline-based conventional therapy. After 6 months there was a statistically significant response in both the TCA and sham groups compared to guideline-based conventional therapy (response rate with TCA 47.6% sham 44.2% and with conventional therapy 27.4%).
A 2008 meta-analysis [83] found similar results with no differences between TCA and sham groups in pain scores, but both improving more that controls. A subsequent 2011 Cochrane review [11] including 35 RCTs found some evidence of efficacy of acupuncture in decreasing pain and improving function in the short-term at the end of treatment when comparing it to sham or to conventional therapy. There was also limited evidence supporting that acupuncture in conjunction with conventional therapy was better than conventional therapy alone. However, acupuncture was not better than sham interventions or conventional therapy in the longer term.
Knee osteoarthritis
In the latest decade the incidence of knee pain has increased, affecting more than 25% of patients 55 years or older [84]. Knee osteoarthritis is also a common reason for patients to seek care from acupuncturists [4]. Most research on acupuncture for knee osteoarthritis has been performed in Germany [85, 86, 87]. The available evidence has been summarized in various meta-analyses.
A 2007 meta-analysis of 9 RCTs [88] reported that patients receiving acupuncture had similar pain and function outcomes to those receiving sham acupuncture, but improved significantly more than those in the waiting list control group. Another 2007 meta-analysis by different authors [84] included 13 RCTs with 1334 patients and compared patients receiving acupuncture with those receiving sham acupuncture, with control groups receiving usual care, or with other groups receiving an active intervention. The authors reported that “adequate TCA” was significantly better in improving outcomes, including WOMAC scores for both pain and function, than “true sham” or other control interventions. “Adequate TCA” was defined an acupuncture technique consisting of at least 6 treatments, at least one per week, with needle placement in at least 4 points for each painful knee during 20 minutes, and either achieving De qi or using EA with sufficient intensity to produce sensation. “True sham” was defined as any sham procedure that did not stimulate nerves in the same neurological segments in the knee joint even if it included superficial needle penetration which was felt to be an active treatment.
A 2010 Cochrane review assessed the efficacy of acupuncture in patients with osteoarthritis of the knee, hip or hand [7] including 3438 patients and found a statistically significant difference in pain decrease favoring acupuncture over the sham control. However, these pooled short-term results did not meet the predefined scores for clinical relevance and there was substantial statistical heterogeneity in the studies. The review concluded that there might be small benefits of acupuncture compared to sham interventions but that they do not to have a sufficient clinical relevance or impact. This small benefit might be secondary to placebo and inadequate blinding in some trials.
An additional trial on 560 patients with osteoarthritis of the knee that we described in the section on expectations found no differences between acupuncture and sham acupuncture, but both groups significantly improved compared to waiting list participants [19]. At least part of the benefit observed in both the active and sham groups was mediated through the acupuncturists' communication style providing positive versus neutral expectations of improvement.
The recent meta-analysis by Vickers et al. [93] included 5 RTCs of patients with osteoarthritis, mainly of the knee, but also excluded many other trials included in other systematic reviews. The authors found a statistically significant effect when comparing acupuncture versus sham acupuncture of 0.26 (95% CI, 0.17-0.34). This effect size was very small and may not be clinically significant given that a common threshold for clinical significance is an effect size of 0.3 or greater. Therefore, the potential beneficial action of acupuncture on osteoarthritis pain does not appear to be clinically relevant.
Conclusions
Acupuncture has become a widely accepted intervention for many conditions that involve pain, including multiple musculoskeletal disorders as shown in this review and in many others available in the literature [2, 3]. Many theories have been proposed to explain the biochemical and physiologic effect of acupuncture in pain pathways [4, 5, 27, 35].
Various methodological issues need to be considered when evaluating the evidence related to acupuncture treatment for pain including the design of the study, appropriate blinding, allocation and randomization, the non-specific effects of this modality of alternative therapy, patient's beliefs and expectations and provider's behavior[16-20, 27, 35, 89]. Acupuncture is relatively safe but there are still reports of serious and fatal side effects that must be taken into account when recommending this therapy to our patients [21, 22].
Many of the recent trials which report that acupuncture is not better than sham interventions suggest that the effects of acupuncture are related to a strong placebo response. However, many authors believe that even minimal stimulation, as elicited with sham procedures, could result in analgesia. With the evolving advances in neurosciences, well designed high quality RCTs including neurochemical and functional evaluations of the brain will be crucial in our understanding of whether the analgesic effects of acupuncture are specific to this treatment and not simply a placebo response enhanced by patients' expectations.
Acknowledgments
Dr. Suarez-Almazor is the recipient of a K24 award from the National Institute on Arthritis, Musculoskeletal and Skin Disorders (NIAMS K24AR053593). Manuscripts contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIAMS or NIH.
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported
Contributor Information
Matxalen Amezaga Urruela, Email: mamezaga@mdanderson.org, Baylor College of Medicine and The University of Texas M.D. Anderson Cancer Center, Department of General Internal Medicine and Ambulatory Treatment, The University of Texas M.D. Anderson Cancer Center, 1400 Pressler St, Unit 1465, Houston, TX, 77030. Phone: 713-745-4516, Fax: 713-563-4491.
Maria E. Suarez-Almazor, Email: msalmazor@mdanderson.org, Chief, Section of Rheumatology, Department of General Internal Medicine, Department of General Internal Medicine and Ambulatory Treatment, The University of Texas M.D., Anderson Cancer Center, 1400 Pressler St, Unit 1465, Houston, TX, 77030. Phone: 713-745-4516, Fax: 713-563-4491.
References
- 1.Robson T. An Introduction to Complementary Medicine. Allen & Unwin; 2004. p. 90. [Google Scholar]
- 2.Kaptchuk T. Acupuncture: theory, efficacy and practice. Ann Intern Med. 2002:374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 3.Mao JJ, Farrar JT, Armstrong K, et al. De qi: Chinese acupuncture patients's experiences and beliefs regarding acupuncture needling sensation-an exploratory survey. Acupunct Med. 2007;4:158–165. doi: 10.1136/aim.25.4.158. [DOI] [PubMed] [Google Scholar]
- 4.Burke A, Upchurch DM, Dye C, et al. Acupuncture use in the United States: findings from the National Health Interview Survey. J Altern Complement Med. 2006;12(7):639–648. doi: 10.1089/acm.2006.12.639. [DOI] [PubMed] [Google Scholar]
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults: United States. Natl Health Stat Report. 2009;12:1–23. [PubMed] [Google Scholar]
- 6.Shuai P, et al. Issues of design and statistical analysis in controlled clinical acupuncture trials: An analysis of English-language reports from Western journals. Statistics in Medicine. 2012;31(7):606–618. doi: 10.1002/sim.4034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7•.Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database of Systematic Reviews. 2010;1:CD001977. doi: 10.1002/14651858.CD001977.pub2. 10.1002/14651858.CD001977.pub2. This review concluded that acupuncture relieves pain in peripheral OA but the effect is not clinically relevant, in the review the authors attributed these differences to placebo, bias and other factors as patient's expectations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trinh K, Graham N, Gross A, et al. Acupuncture for neck disorders. Cochrane Database of Systematic Reviews. 2006;3:CD004870. doi: 10.1002/14651858.CD004870.pub3. 10.1002/14651858.CD004870.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Green S, Buchbinder R, Hetrick SE. Acupuncture for shoulder pain. Cochrane Database of Systematic Reviews. :CD005319. doi: 10.1002/14651858.CD005319. 10.1002/14651858.CD005319. [DOI] [PubMed] [Google Scholar]
- 10.Casimiro L, et al. Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis. Cochrane Database of Systematic Reviews. 2005 doi: 10.1002/14651858.CD003788.pub2. 0.1002/14651858.CD003788.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Furlan Andrea D, et al. Acupuncture and dry-needling for low back pain. Cochrane Database of Systematic Reviews. 2005 doi: 10.1002/14651858.CD001351.pub2. 10.1002/14651858.CD001351.pub2. [DOI] [PubMed] [Google Scholar]
- 12.White AR, Filshie, Cummings TM. Clinical trials of acupuncture: consensus for recommendations for optimal treatment, sham controls and binding. J Altern Complement Med. 2001;9:237–245. doi: 10.1054/ctim.2001.0489. [DOI] [PubMed] [Google Scholar]
- 13.Vickers AJ. Placebo controls in randomized trials of acupuncture. Eval Health Prof. 2002;25(4):421–435. doi: 10.1177/0163278702238055. [DOI] [PubMed] [Google Scholar]
- 14.Bing Z, Villanueva L, Le Bars D. Acupuncture and diffuse noxious inhibitory controls: naloxone-reversible depression of activities of trigeminal convergent neurons. Neuroscience. 1990;37(3):809–818. doi: 10.1016/0306-4522(90)90110-p. [DOI] [PubMed] [Google Scholar]
- 15.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352(9125):364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 16.Langevin HM, Hammerschlag R, Lao L, et al. Controversies in acupuncture research: selection of controls and outcome measures in acupuncture clinical trials. J Altern Complement Med. 2006;12(10):943–953. doi: 10.1089/acm.2006.12.943. [DOI] [PubMed] [Google Scholar]
- 17.Khadilkar A, Obebiyi DO, Brosseau L, et al. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Sys Rev. 2008;4:CD003008. doi: 10.1002/14651858.CD003008.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linde K, Niemann K, Schneider A, et al. How large are the nonspecific effects of acupuncture? A meta-analysis of randomized controlled trials. BMC Medicine. 2010;8:75. doi: 10.1186/1741-7015-8-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19••.Suarez-Almazor ME, Looney C, Liu Y, et al. A Randomized Controlled Trial of Acupuncture for Osteoarthritis of the Knee: Effects of Patient- Provider Communication. Arthritis Care & Res. 2010;62:9, 1229–1236. doi: 10.1002/acr.20225. In this study, concrete evidence of the non-specific effects of patient's expectations and communication styles are evaluated in patients with OA of the knee treated with acupuncture versus sham acupuncture and control groups, raising the question regarding the effectiveness of TCA over sham acupuncture and waiting list; the placebo effect of sham acupuncture being not different in outcomes than TCA and pain perception and patient satisfaction in groups with different communications styles in their providers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linde K, Witt C, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128:264–271. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 21••.Ernst E, Lee M, Choi TY. Does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011:755–764. doi: 10.1016/j.pain.2010.11.004. This review summarizes the latest evidence in the safety of acupuncture and its efficacy in numerous reviews. Also raises a concern regarding the under-reporting of side effects in clinical trials and regular practices all over the world. [DOI] [PubMed] [Google Scholar]
- 22.Ernst E, Zhang J. Cardiac tamponade caused by acupuncture: A review of the literature. Int Journal of Cardiology. 2011;149:287–289. doi: 10.1016/j.ijcard.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 23.Mayer D, Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Res. 1977;121:368–372. doi: 10.1016/0006-8993(77)90161-5. [DOI] [PubMed] [Google Scholar]
- 24.Pomeranz DC. Naloxone blocks acupuncture analgesia and causes hyperalgesia: endorphin is implicated. Life Sci. 1976;19:1757–1762. doi: 10.1016/0024-3205(76)90084-9. [DOI] [PubMed] [Google Scholar]
- 25.Harris RE, Zubieta JK, Scott DJ, et al. Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on mu-opioid receptors (MORs) Neuroimage. 2009;47:1077–1085. doi: 10.1016/j.neuroimage.2009.05.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhond RP, Kettner N, Napadow V. Neuroimaging acupuncture effects in the human brain. J Altern Complement Med. 2007;13:603–616. doi: 10.1089/acm.2007.7040. [DOI] [PubMed] [Google Scholar]
- 27.Pariente J, White P, Frackowiak RS, et al. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005;25:1161–1167. doi: 10.1016/j.neuroimage.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 28.Peyron R, Laurent B, Garcia-Larrea L. Functional imaging of brain responses to pain. A review and meta-analysis. Clin Neurophysiol. 2000;30:263–288. doi: 10.1016/s0987-7053(00)00227-6. [DOI] [PubMed] [Google Scholar]
- 29.Wager TD, Rilling JK, Smith EE, et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303:1162–1167. doi: 10.1126/science.1093065. [DOI] [PubMed] [Google Scholar]
- 30.Fuente-Fernandez R, Stoessl AJ. The placebo effect in Parkinson's disease. Trends Neurosci. 2002;25:302–306. doi: 10.1016/s0166-2236(02)02181-1. [DOI] [PubMed] [Google Scholar]
- 31.Petrovic P, Ingvar M. Imaging cognitive modulation of pain processing. Pain. 2002;95:1–5. doi: 10.1016/s0304-3959(01)00467-5. [DOI] [PubMed] [Google Scholar]
- 32.Wang SM, Kain ZN, White P. Acupuncture analgesia: I. The scientific basis. Anesth Analg. 2008;106:602–610. doi: 10.1213/01.ane.0000277493.42335.7b. [DOI] [PubMed] [Google Scholar]
- 33.Hang JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26:17–22. doi: 10.1016/s0166-2236(02)00006-1. [DOI] [PubMed] [Google Scholar]
- 34.Pomeranz B. Scientific research into acupuncture for the relief of pain. J Altern Complement Med. 1996;2:53–60. doi: 10.1089/acm.1996.2.53. [DOI] [PubMed] [Google Scholar]
- 35.Kong J, Kaptchuk TJ, Polich G, et al. Expectancy and treatment interactions: a dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage. 2009;45:940–949. doi: 10.1016/j.neuroimage.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Man SC, Baragar FD. Preliminary clinical study of acupuncture in rheumatoid arthritis. J Rheumatol. 1974;1:126–129. [PubMed] [Google Scholar]
- 37.David J, Townsend S, Sathanathan R, et al. The effect of acupuncture on patients with rheumatoid arthritis: a randomized, placebo-controlled cross-over study. Rheumatology. 1999;38:864–869. doi: 10.1093/rheumatology/38.9.864. [DOI] [PubMed] [Google Scholar]
- 38.Lee MS, Shin BC, Ernst E. Acupuncture for rheumatoid arthritis: a systematic review. Rheumatology. 2008;47:1747–1753. doi: 10.1093/rheumatology/ken330. [DOI] [PubMed] [Google Scholar]
- 39.Tam LS, Leung PC, Li T, et al. Acupuncture in the treatment of rheumatoid arthritis: a double-blind controlled pilot study. BMC Complement Altern Med. 2007;7:35. doi: 10.1186/1472-6882-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zanette SD, Born IG, Brenol JC, Xavier RM. A pilot study of acupuncture as adjunctive treatment of rheumatoid arthritis. Clin Rheumatol. 2008;27:627–635. doi: 10.1007/s10067-007-0759-y. [DOI] [PubMed] [Google Scholar]
- 41.Wang YJ. Combined acupuncture and west medication treating 109 cases of rheumatoid arthritis. Hunan Guiding J TCM P. 2002;8:769–770. [Google Scholar]
- 42.Zhou JL, Zhu Q. Effects of acupuncture on rheumatoid arthrirtis. Chin J Rheumatol. 2000;4:169–171. [Google Scholar]
- 43.Xiang QX. Masters thesis. Heilongjiang Trad Chin Med College; Heilongjiang, China: 2005. Study of the early curative effect on rheumatoid arthritis by acupuncture combined with electronic moxibustion. [Google Scholar]
- 44.Liu W, Liu B, Wang Y, et al. Observation on the therapeutic effect of acupuncture and moxibustion in 120 cases of rheumatoid arthritis. Chin Acupunct Moxibustion. 2003;23:577–578. [Google Scholar]
- 45.Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998;19:159–166. doi: 10.1016/s0197-2456(97)00150-5. [DOI] [PubMed] [Google Scholar]
- 46.Wang C, Pablo P, Chen X, et al. Acupuncture for the pain relief in patients with rheumatoid arthritis: a systematic review. Arthritis Care Res. 2008;59(9):1249–1256. doi: 10.1002/art.24009. [DOI] [PubMed] [Google Scholar]
- 47.Wolfe F, Ross K, Anderson J, et al. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]
- 48.Nassim A, Sherman K, Jacobsen C, et al. A randomized controlled clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Int Med. 2005;143:11–24. doi: 10.7326/0003-4819-143-1-200507050-00005. [DOI] [PubMed] [Google Scholar]
- 49.Mayhew E, Ernst E. Acupuncture for fibromyalgia-a systematic review of randomized clinical trials. Rheumatology. 2007;26:801–804. doi: 10.1093/rheumatology/kel406. [DOI] [PubMed] [Google Scholar]
- 50.Deluze C, Bosia L, Zirbs A, et al. Electroacupuncture in fibromyalgia: results of a controlled trial. Br Med J. 1993:306–393. doi: 10.1136/bmj.305.6864.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martin D, Sletten C, Williams B, et al. Improvement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trial. Mayo Clin Proc. 2006;81:749–757. doi: 10.4065/81.6.749. [DOI] [PubMed] [Google Scholar]
- 52.Guo X, Jia J. Comparison of therapeutic effects on fibromyalgia syndrome between dermal-neurological electric stimulation and electric acupuncture. Chinese J Clin Rehab. 2005;9:171–173. [Google Scholar]
- 53.Assefi N, Sherman K, Jacobsen C, et al. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Int Med. 2005;143:10–21. doi: 10.7326/0003-4819-143-1-200507050-00005. [DOI] [PubMed] [Google Scholar]
- 54.Sprott H. Efficiency of acupuncture in patients with fibromyalgia. Clin Bull Myofascial Therapy. 1998;3(37):37–43. [Google Scholar]
- 55.Langhorst J, Klose P, Musial F, et al. Efficacy of acupuncture in fibromyalgia syndrome--a systematic review with a meta-analysis of controlled clinical trials. Rheumatology. 2010;49:778–788. doi: 10.1093/rheumatology/kep439. [DOI] [PubMed] [Google Scholar]
- 56.Harris RE, Tian XT, Williams, et al. Treatment of fibromyalgia with formula acupuncture: investigation of needle placement, needle stimulation and treatment frequency. J Altern Compl Med. 2005;11:663–671. doi: 10.1089/acm.2005.11.663. [DOI] [PubMed] [Google Scholar]
- 57.Lautenschlager J, Schnorrenberger CC, Muller W. Acupuncture in generalized tendomyopathia (fibromyalgia syndrome) [in German] Dtsch Ztschr Akup. 1989;32:122–128. [Google Scholar]
- 58.White P, Lewith G, Prescott P, et al. Acupuncture versus placebo for the treatment of chronic mechanical neck pain. Ann Intern Med. 2004;141:920–928. doi: 10.7326/0003-4819-141-12-200412210-00007. [DOI] [PubMed] [Google Scholar]
- 59.Irnich D, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. 200;322(7302):1574–1578. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vickers AJ. Statistical re-analysis of four recent randomized trials of acupuncture for pain using analysis of covariance. Clin J Pain. 2004;20(5):319–323. doi: 10.1097/00002508-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 61.Birch S, Jamison R. Controlled trial of Japanese acupuncture for chronic myofascial neck pain: Assessment of specific and nonspecific effects of treatment. Clin J Pain. 1998;14:248–255. doi: 10.1097/00002508-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 62.Coan RM, Wong G, Coan PL. The acupuncture treatment of neck pain: A randomized controlled study. Am J Chin Med. 1982;9(4):326–332. doi: 10.1142/s0192415x81000433. [DOI] [PubMed] [Google Scholar]
- 63.David J, Modi S, ALuko AA, et al. Chronic neck pain: A comparison of acupuncture treatment and physiotherapy. Br J Rheumatol. 1998;37:1118–1122. doi: 10.1093/rheumatology/37.10.1118. [DOI] [PubMed] [Google Scholar]
- 64.Irnich D, Behrens N, Molzen H, et al. Randomized trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. 2001;322:1574–1578. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Loy T. Treatment of cervical spondylosis: Electroacupuncture versus physiotherapy. Med Jou Aust. 1983;2:32–34. [PubMed] [Google Scholar]
- 66.Petrie JP, Hazleman BL. A controlled study of acupuncture in neck pain. Br J Rheumatol. 1986;25:271–275. doi: 10.1093/rheumatology/25.3.271. [DOI] [PubMed] [Google Scholar]
- 67.White PF, Craig WF, Vakharia AS, et al. Percutaneous neuromodulation therapy: Does the location of electrical stimulation effect the acute analgesic response? Anesth Analg. 2000;91:949–954. doi: 10.1097/00000539-200010000-00034. [DOI] [PubMed] [Google Scholar]
- 68.Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57(11):649. doi: 10.1136/ard.57.11.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Berry H, Fernandes L, Bloom B, et al. Clinical study comparing acupuncture, physiotherapy, injection and oral anti–inflammatory therapy in the shoulder. Curr Med Res Opin. 1980;7:121–126. doi: 10.1185/03007998009112038. [DOI] [PubMed] [Google Scholar]
- 70.Ceccherelli F, Bordin M, Gagliardi G, et al. Comparison between superficial and deep acupuncture in the treatment of the shoulder's myofascial pain: A randomized and controlled study. Acupunct Electrother Res. 2001;26:229–238. doi: 10.3727/036012901816355938. [DOI] [PubMed] [Google Scholar]
- 71.Dyson-Hudson TA, Shiflett SC, Kirshblum CS, et al. Acupuncture and trager psychophysical integration in the treatment of wheelchair user's shoulder pain in invidividuals with spinal cord injury. Arch Phys Med Rehab. 2001;82:1038–1046. doi: 10.1053/apmr.2001.24888. [DOI] [PubMed] [Google Scholar]
- 72.Kleinhenz J, Streitberger K, Windeler J, et al. Randomised clinical trialcomparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83(2):235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- 73.Lin ML, Huang CT, Lin JG, Tsai SK. A comparison between the pain relief effect of electroacupuncture, regional nerve block and electroacupuncture plus regional nerve block in frozen shoulder. Acta Anaesthesiol Sin. 1994;32(4):237–242. [PubMed] [Google Scholar]
- 74.Moore ME, Berk SN. Acupuncture for chronic shoulder pain. An experimental study with attention to the role of placebo and hypnotic susceptibility. Ann Intern Med. 1976;84(4):381–384. doi: 10.7326/0003-4819-84-4-381. [DOI] [PubMed] [Google Scholar]
- 75.Romoli M, van der Windt D, Giovanzana P, et al. International research project to devise a protocol to test the effectiveness of acupuncture on painful shoulder. J Altern Compl Med. 2000;6(3):281–287. doi: 10.1089/acm.2000.6.281. [DOI] [PubMed] [Google Scholar]
- 76.Sun KO, Chan KC, Lo SL, et al. Acupuncture for frozen shoulder. Hong Kong Med J. 2001;7:381–391. [PubMed] [Google Scholar]
- 77.Yuan DW. Bioholographic acupuncture therapy for 44 cases of scapulohumeral periarthritis. Shanghai J Acupunct Moxibustion. 1995;14(2):68. [Google Scholar]
- 78.Molsberger A, Schneider T, Gotthardt, et al. German randomized Acupuncture Trial for chronic shoulder pain (GRASP)- A pragmatic, controlled, patient-blinded, multicentre trial in an outpatient care environment. Pain. 2010;151:146–154. doi: 10.1016/j.pain.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 79.Cherkin DC, Deyo RA, Sherman KJ, et al. Characteristics of visits to licensed acupuncturists, chiropractors, massage therapists, and naturopathic physicians. J Am Board Fam Pract. 2002;15:6463–6472. [PubMed] [Google Scholar]
- 80.Speed C. Low back pain. BMJ. 2004;328:1119–21. doi: 10.1136/bmj.328.7448.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Manheimer E, White A, Berman B, et al. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142(8):651–663. doi: 10.7326/0003-4819-142-8-200504190-00014. [DOI] [PubMed] [Google Scholar]
- 82.Haake M, Muller HH, Schade-Brittinger C, et al. German acupuncture trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel group trial with 3 groups. Arch Intern Med. 2007;167(17):1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 83.Yuan J, Purepong N, Kerr DP, Bradbury I, McDonough S, et al. Effectiveness of acupuncture for low back pain: a systematic review. Spine. 2008;33:887–900. doi: 10.1097/BRS.0b013e318186b276. [DOI] [PubMed] [Google Scholar]
- 84.White A, Foster NE, Cummings M, et al. Acupuncture treatment for chronic knee pain: a systematic review. Rheumatology (Oxford) 2007;46(3):384–390. doi: 10.1093/rheumatology/kel413. [DOI] [PubMed] [Google Scholar]
- 85.Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366(9480):136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 86.Witt CM, Jena S, Brinkhaus B, et al. Acupuncture in patients with osteoarthritis of the knee or hip: a randomized, controlled trial with an additional nonrandomized arm. Arthritis Rheum. 2006;54(11):3485–3493. doi: 10.1002/art.22154. [DOI] [PubMed] [Google Scholar]
- 87.Scharf HP, Mansmann U, Streitberger K, et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med. 2006;145(1):12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 88.Manheimer E, Linde K, Lao L, et al. Meta-analysis: acupuncture for osteoarthritis of the knee. Ann Intern Med. 2007;146(12):868–877. doi: 10.7326/0003-4819-146-12-200706190-00008. [DOI] [PubMed] [Google Scholar]
- 89.Walach H. The efficacy paradox in randomized controlled trials of CAM and elsewhere: beware of the placebo trap. J Altern Complement Med. 2001;7(3):213–218. doi: 10.1089/107555301300328070. [DOI] [PubMed] [Google Scholar]
- 90.Cheng X. Chinese Acupuncture and Moxibustion. Beijing, China: Foreign Languages Pr; 1999. Chinese Acupuncture and Moxibustion. [Google Scholar]
- 91.O'Connor J. Acupuncture: A Comprehensive Text. Chicago: Eastland Pr; 1981. [Google Scholar]
- 92.Cheng X. Chinese acupuncture and moxibustion. Beijing: Foreign Language Press; 1987. pp. 322–329. [Google Scholar]
- 93.Vickers AJ, DPhil A, Cronin MS, et al. Acupuncture for Chronic Pain. Arch Intern Med. 2012 Sep 10; doi: 10.1001/archinternmed.2012.3654. published online. 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]