Abstract
Posttraumatic stress disorder (PTSD) has previously been associated with increased risk for a variety of chronic medical conditions and it is often underdiagnosed in minority civilian populations. The current study examined the effects of resilience on the likelihood of having a diagnosis of PTSD in an inner-city sample of primary care patients (n = 767). We measured resilience with the Connor-Davidson Resilience Scale, trauma with the Childhood Trauma Questionnaire and Trauma Events Inventory, and assessed for PTSD with the modified PTSD symptom scale. Multiple logistic regression model with presence/absence of PTSD as the outcome yielded 3 significant factors: childhood abuse, nonchild abuse trauma, and resilience. One type of childhood abuse in moderate to severe range (OR, 2.01; p = .0001), 2 or more types of childhood abuse in moderate to severe range (OR, 4.00; p ≤ .0001), and 2 or more types of nonchildhood abuse trauma exposure (OR, 3.33; p ≤ .0001), were significantly associated with an increased likelihood of PTSD, while resilience was robustly and significantly associated with a decreased likelihood of PTSD (OR, 0.93; p ≤ .0001). By understanding the role of resilience in recovery from adverse experiences, improved treatment and interventional methods may be developed. Furthermore, these results suggest a role for assessing resilience in highly traumatized primary care populations as a way to better characterize risk for PTSD and direct screening/psychiatric referral efforts.
Keywords: psychiatry, urban population
INTRODUCTION
Resilience is broadly defined as the tendency to successfully adapt to risk or adversity, and it is well known that African Americans as a group face disproportionate risk for a number of adverse health outcomes, including posttraumatic stress disorder (PTSD).1,2 Unfortunately, variation within this population in terms of positive outcomes such as resilience is rarely explored. PTSD affects 7.8% of the general population and traumatic exposure is the main risk factor for development of PTSD.3 Urban, impoverished populations experience high rates of traumatic exposure and have a higher burden of disease compared to other groups, yet the most common outcome following a potentially traumatic event (PTE) is, in fact, recovery.4 Prior research has focused on the identification of biopsychosocial risk and protective factors; however, increasing evidence suggests that peritraumatic psychological processes—not prior characteristics—are the strongest predictors of developing PTSD following a traumatic event.5
Since there is no evidence that being African American itself confers an increased risk for PTSD, it remains unclear to what degree health disparities related to African Americans’ and other ethnic minority groups’ higher risk of developing PTSD are related to their relative overexposure to PTEs or to peritraumatic and posttraumatic processes.3 This gap in knowledge has important clinical and research implications, as interventions to enhance resilience may be particularly relevant to vulnerable urban populations.6 Interventions designed to reduce the negative impact of traumatic events represent a significant secondary prevention strategy, and it is important to appropriately stratify high-risk subgroups in terms of their potential for recovery and need for treatment referral especially in urban, primary care settings with high rates of traumatic exposures.5–7
Within the framework of primary care settings, it is important to note that PTSD and trauma exposure are associated with higher rates of physical illness, as well as increased health care utilization.8–11 In addition, trauma exposure and PTSD are associated with a variety of metabolic abnormalities, including hyperlipidemia and diabetes, which may mediate these adverse health outcomes.12–19 Thus, a resilience framework is applicable to chronic medical conditions such as metabolic syndrome and diabetes, which also disproportionately affect minority groups.20 Historically, resilience frameworks were first developed in child and adolescent populations who did not develop symptoms despite high exposure to adversity.21–22 Measuring and characterizing resilience in families and adult populations represents a paradigm shift. In some studies, when both risk and resilience factors are measured, racial and ethnic disparities are reduced, or are no longer significant, suggesting that these differences are better explained by cultural differences in resilience.23,24
Therefore, the aim of this study was to investigate the effect of resilience on the presence of posttraumatic stress disorder following childhood and/or nonchildhood abuse trauma exposure in a group of impoverished, minority adults in an inner-city primary care setting. We hypothesized that in the presence of multiple risk factors, resilience would significantly decrease the odds of developing a diagnosis of PTSD.
METHODS
Participants
This study was part of a larger study investigating genetic and trauma-related risk factors for PTSD and depression in a population of urban, low-income, highly traumatized, predominantly African American men and women.25,26 Inclusion criteria included age of 18 to 75 years, understanding English, and ability to give informed consent. The study was approved by the institutional review boards of Emory University School of Medicine and Grady Memorial Hospital.
Members of the research team approached adult patients waiting for their outpatient appointments at the primary medical care or obstetrical-gynecological clinics of Grady Memorial Hospital in Atlanta, Georgia, to solicit for study participation. During the recruitment phase of this study, 58% of those approached agreed to participate, and a cumulative percentage of 84% and 91% of the second and third subjects approached agreed if the initial subject approached did not participate. Participants gave informed consent and completed a battery of self-report measures. Due to variation between subjects with respect to literacy, all self-report measures were obtained by interview.
Measures
Sociodemographic information, including age, sex, race, education, employment status, income, and marital status, were collected. Dichotomous variables were created for employment status (employed or unemployed), marital status (married or others [single, divorced, separated, or widowed]), and race (African American or others). Education was coded as 3 levels (1 = high school or below, 2 = some college or technical school, 3 = college graduates or graduate school). Monthly income was characterized by 3 levels (1 = income <$1000, 2 = $1000–$2000, 3 = income >$2000).
Childhood abuse was assessed retrospectively with the self-report, psychometrically validated 28-item Childhood Trauma Questionnaire (CTQ).27,28 Scores were extracted for the categories of emotional, physical, and sexual abuse. Following Bernstein and Fink’s score ranges for none, mild, moderate, and severe levels of abuse, we classified participants into 2 groups: (a) none to mild range and (b) moderate and severe range for each of the aforementioned type of abuse.27 We then divided the participants into 3 categories based on the number of types of abuse (emotional, physical, or sexual) they had in the moderate and severe range: (a) those with no abuse in the moderate and severe range and (b) those with 1 type of abuse in the moderate and severe range, and (c) those with 2 or more types in this range. Therefore, childhood abuse was modeled in this manner.
Nonchildhood abuse trauma was assessed using the Traumatic Events Inventory.29,30 This instrument screens for lifetime exposure to different categories of trauma, including natural disaster, serious accident or injury, sudden life-threatening illness, military combat, being attacked with a weapon, witnessing a family member or friend being attacked with a weapon, being attacked without a weapon, witnessing a family member or friend being attacked without a weapon, witnessing the murder of a friend or family member, or being sexually assaulted under duress. For each category of the instrument, having had the exposure was scored as 1 and no exposure as 0. Score ranges from 0 to 15 for nonchildhood abuse trauma, with higher scores reflecting exposure to more types of trauma. The childhood trauma items in this inventory were excluded to avoid overlap with the information collected with the CTQ. We divided the participants into 3 categories based on the number of types of trauma they had experienced: (a) those with no traumatic exposures and (b) those with 1 type of traumatic exposure, and (c) those with 2 or more types of traumatic exposure. Nonchildhood abuse trauma was modeled in this manner.
Resilience was assessed with the 10-item, self-rated Connor-Davidson Resilience Scale (CD-RISC).31 The full CD-RISC was found to have an unstable structure across 2 demographically equivalent samples and was thus modified into a 10-item scale with good internal consistency, construct validity, and excellent psychometric properties for efficient measurement of resilience.31,32 Items were rated on a 5-point Likert scale, ranging from “not true at all” (scored 0) to “true nearly all the time” (scored 4). Score ranges from 0 to 40 with higher score reflecting greater resilience.
Posttraumatic stress disorder was assessed using the PTSD symptom scale (PSS). The PSS is a psychometrically valid 17-item self-report scale assessing PTSD symptomatology over the 2 weeks prior to rating.7,29,33,34 This measure provides a conservative estimate of PTSD diagnosis compared to the SCID (Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) (DSM-IV).35 A categorical variable that serves as a proxy for PTSD was created based on DSM-IV A-E criterion responses to the PSS questionnaire (A, presence of trauma; B, presence of at least 1 intrusive symptom; C, presence of at least 3 avoidance/numbing symptoms; and D, presence of at least 2 hyperarousal symptoms; and E, present for at least 1 month).
Statistical Analyses
Analyses were performed using STATA software (StataCorp 2007, Stata Statistical Software: release 10. College Station, Texas, StataCorpLP). Sociodemographic and clinical variables were characterized with descriptive statistics and significant differences by PTSD status were identified using the χ2 test (Wilcoxon rank-sum was used for resilience). Logistic regression was performed with PTSD as the categorical outcome variable and childhood abuse, nonchildhood abuse trauma exposure, and resilience as the independent variables, controlling for age, sex, race, education, employment, income, and marital status. Statistical significance required a 2-sided p value of < .05.
RESULTS
A total of 767 adults completed the resilience and PSS questionnaire and were subsequently included in this analysis: mean age was 37 years and range was 18 to 74 years, approximately 67% were female, 94% were African American, 11% were married, 69% had an education of high school or below, 31% were employed, and 63% had a monthly income of less than $1000. Detailed sociodemographic characteristics and a summary of the clinical variables are presented in Table 1. In this sample, 30% (233 of 767) met criteria for PTSD. Exploration of sociodemographic differences by PTSD status yielded one significant finding. Subjects meeting criteria for PTSD on the PSS were more likely to be unemployed (p = .02). There was a trend towards significance with this group being more likely to have less than a high school level education (p = .09).
Table 1.
Characteristics of Study Participants by Posttraumatic Stress Disorder (PTSD) Status (N = 767)a
| Characteristics | %(n) | PTSD % (n)
|
p Value | |
|---|---|---|---|---|
| No | Yes | |||
| Sex | ||||
| Male | 33% (251) | 33% (176) | 32% (75) | .82 |
| Female | 67% (515) | 67% (357) | 68% (158) | |
| Race | ||||
| African American | 94% (711) | 94% (497) | 93% (214) | .94 |
| Others | 6% (49) | 6% (34) | 7% (15) | |
| Marital status | ||||
| Married | 11% (81) | 11% (60) | 9% (21) | .37 |
| Others (single, separated, divorced, widowed) | 89% (677) | 89% (469) | 91% (208) | |
| Education | ||||
| High school or below | 69% (521) | 67% (356) | 72% (165) | .09 (Fisher’s exact) |
| Some college or technical school | 25% (191) | 25% (134) | 25% (57) | |
| College graduates or graduate school | 6% (48) | 8% (40) | 3% (8) | |
| Employment status | ||||
| Employed | 31% (236) | 34% (178) | 25% (58) | .02 |
| Unemployed | 69% (523) | 66% (351) | 75% (172) | |
| Monthly income | ||||
| <$1000 | 63% (458) | 62% (311) | 67% (147) | .16 |
| ≤$1000 and <$2000 | 24% (172) | 24% (119) | 24% (53) | |
| ≥$2000 | 13% (95) | 15% (74) | 10% (21) | |
| Age (mean [95% confidence interval]) | 37 (36, 38) | 36 (35, 38) | 37 (36, 39) | .81 |
| Resilience (median, interquartile range) | 33(10) | 35 (8) | 30 (12) | <.0001 |
| Childhood abuse types in moderate/severe range | ||||
| 0 | 61% (459) | 71% (373) | 38% (86) | <.0001 |
| 1 | 20% (153) | 18% (95) | 26% (58) | |
| ≥2 | 18% (137) | 11% (56) | 36% (81) | |
| Nonchildhood abuse trauma, total types | ||||
| 0 | 16% (122) | 20% (107) | 6% (15) | <.0001 |
| 1 | 25% (190) | 29% (152) | 16% (38) | |
| ≥2 | 59% (450) | 51% (272) | 77% (178) | |
Note that the total per row is sometimes slightly less than 767 due to missing values. However, less than 5% of the participants had some missing values for these variables.
This was a highly traumatized population. Regarding clinical variables, 61% of the participants reported no sexual, physical, or emotional childhood abuse in the moderate or severe range; conversely, 38% reported some level of child abuse. Only 16% report no exposure to nonchildhood abuse trauma, with 84% reporting exposure to significant nonchildhood abuse trauma. Despite these high levels of trauma exposure, self-reported resilience was high in this sample, and the median CDRISC score was 33 with an interquartile range of 10. As expected, there were significant differences between the PTSD and no-PTSD group on each of the clinical variables.
A summary of lifetime exposure to nonchildhood abuse traumatic experiences is shown in Table 2. Interestingly, despite high rates of exposure to nonchildhood abuse trauma (84% of the sample reported 1 or more types of nonchildhood abuse trauma), approximately 70% of the participants had no current diagnosis of PTSD (DSM-IV Text Revision criteria), although they could have had PTSD in the past. In general, the group with PTSD was significantly more likely to have experienced all types of nonchildhood abuse trauma. Of those meeting PSS-based PTSD criteria, the mean (standard deviation) PTSD symptom severity score was 28 (9).
Table 2.
Summary of Lifetime Exposure to Nonchildhood Abuse Traumatic Experiences by Posttraumatic Stress Disorder (PTSD) Statusa
| Nonchildhood Abuse Trauma Type Experienced | Overall Percentage and Frequency of Respondents’ Endorsing Exposure | Percentage Endorsing Exposure by PTSD Status
|
|
|---|---|---|---|
| PTSD % (n) | No PTSD % (n) | ||
| Any significant traumaa | 83.9% (640/762) | 93.6% (218) | 80.0% (427) |
| Natural disastera | 28.5% (215/754) | 38.6% (88) | 24.1% (127) |
| Serious accident or injurya | 41.2% (308/748) | 53.1% (120) | 36.0% (188) |
| Sudden life-threatening illness | 20% (151/755) | 26.3% (60) | 17.3% (91) |
| Military combat | 1.3% (10/752) | 0.9% (2) | 1.5% (8) |
| Witness of murder of close family member or frienda | 15.0% (113/752) | 24.1% (55) | 11.1% (58) |
| Confronted with murder of close family member or frienda | 49.3% (364/738) | 59.3% (134) | 44.9% (23) |
| Attacked with knife, gun, or other weapon by someone other than intimate partnera | 32.2% (224/695) | 41.8% (89) | 28.0% (135) |
| Attacked with knife, gun or other weapon by intimate partnera | 20.5% (154/750) | 35.8% (81) | 13.9% (73) |
| Witnessed family member or friend attacked with knife, gun, or other weapona | 24.5% (184/751) | 37.2% (84) | 19.0% (100) |
| Witnessed non-family member or friend attacked with knife, gun, or other weapona | 29.9% (225/752) | 40.3% (92) | 25.4% (133) |
| Attacked without a weapon by someone other than intimate partnera | 26.8% (202/754) | 30.6% (70) | 25.1% (132) |
| Attacked without a weapon by intimate partnera | 34.2% (256/749) | 56.0% (126) | 24.8% (130) |
| Witnessed family member or friend attacked without a weapon weapona | 35.1% (265/755) | 48.7% (112) | 29.1% (153) |
| Witnessed non-family member or friend attacked without a weapona | 36.2% (273/754) | 46.7% (107) | 31.6% (166) |
| Sexual contact 17 years and older with physical forcea | 7.35% (55/748) | 13.7% (31) | 4.6% (24) |
Differences in exposure by PTSD were assessed using χ2
p < .0001
Logistic regression with PTSD status as the outcome variable (0 = does not meet PTSD criteria, 1 = meets PTSD criteria) ultimately yielded a significant model of 3 factors. Model 1 included our variables of interest as well as potential confounders: age, sex, race, marital status, education, employment, and income. None of the potential confounders were significant; therefore, they were excluded in future models. Model 2 tested for significant interactions between childhood abuse and resilience (p = .48), nonchildhood abuse trauma and resilience (p = .53), or childhood abuse and nonchildhood abuse trauma exposure (p = .08); no interaction terms were significant.
Therefore, our final model (p < .00001), summarized in Table 3, includes significant main effects only. As expected, childhood abuse and nonchildhood abuse trauma increased the odds of having a diagnosis of PTSD, while the CD-RISC measure of resilience decreased the odds. Compared to the reference group of no childhood trauma in the moderate/severe range, 1 type of childhood abuse in moderate/severe range (odds ratio [OR], 2.01; p = .001) and 2 or more types of childhood abuse in moderate/severe range (OR, 4.00; p ≤ .0001) were significantly associated with increased likelihood of PTSD. Compared to the reference group of no reported exposure to nonchildhood abuse trauma, the group with 2 or more types of nonchildhood abuse trauma exposure (OR, 3.33; p < .0001) was significantly associated with increased likelihood of PTSD. Resilience (OR, 0.93; p < .0001), was significantly associated with a decreased likelihood of PTSD. Note that this OR suggests that for every point higher on the CD-RISC score (0–40) there is a 7% decrease in risk for PTSD, assuming scale linearity.
Table 3.
Logistic Regression Model for Posttraumatic Stress Disorder
| Variable | df | OR | 95% CI for OR | p |
|---|---|---|---|---|
| Childhood abuse types in moderate/severe range | 2 | |||
| 0 | 1 | – | – | |
| 1 | 2.01 | (1.31–3.09) | .001 | |
| ≥2 | 4.00 | (2.56–6.26) | < .0001 | |
| Nonchildhood abuse trauma, total types | 2 | |||
| 0 | 1 | – | – | |
| 1 | 1.78 | (0.90–3.53) | .098 | |
| ≥2 | 3.33 | (1.79–6.21) | < .0001 | |
| Resilience | 1 | 0.93 | (0.91–0.95) | < .0001 |
Abbreviations: CI, confidence interval; df, degree of freedom; OR, odds ratio.
In order to graphically depict the impact of resilience on the probability of PTSD, we used our model to generate predicted probabilities of PTSD for a given level of resilience. We found that even after adjusting for the main effects of traumatic exposure (nonchildhood abuse trauma and childhood abuse), the probability of PTSD decreases as a function of increasing resilience (Figure).
Figure.
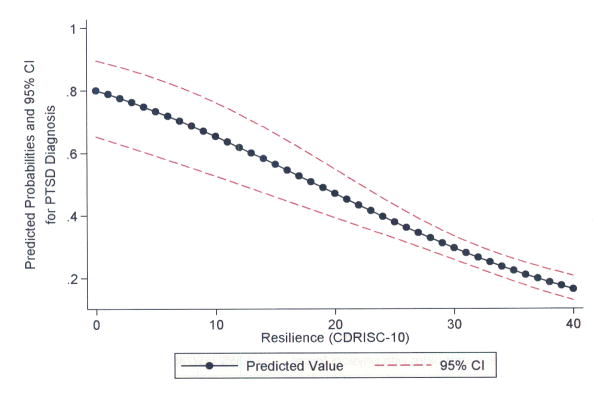
Probability of Posttraumatic Stress Disorder by Resilience (Adjusted for Nonchild Abuse and Childhood Trauma)
DISCUSSION
This study examined the role of resilience in mitigating the impact of traumatic exposures in an urban, low-income, predominantly African American primary care population. We found that despite high levels of trauma exposure and high rates of PTSD compared to the general population, resilience was common. To our knowledge, this is the first study to report the effect of resilience on the likelihood of PTSD given exposure to childhood sexual, physical, and/or emotional abuse and nonchildhood abuse trauma exposure. Other unique aspects of this study include the use of a validated self-report instrument to measure resilience in a vulnerable population.
Our results suggest that resilience is an important factor for clinicians to consider when evaluating a patient’s risk for PTSD given exposure to a significant trauma. Vulnerable populations do bear a disproportionate burden of PTSD risk as a group, yet individuals within this risk strata maintain the capacity to flourish in the face of trauma. Use of self-report instruments such as the 10-item CD-RISC have the potential to aid clinicians in better understanding within-group risk for PTSD, as well as identify patients with low resilience who may benefit from interventions designed to enhance psychological resilience.
The CD-RISC scale of resilience is composed of several different measures. They include constructs that examine optimism, sense of control and perseverance despite obstacles, sense of humor, ability to cope with misfortune and stress, and self-esteem. Many of these components of resiliency may be protective in the face of trauma. By understanding resiliency in an urban, civilian population, we hope to eventually identify approaches to enhancing resiliency in this and similar traumatized populations.
This study has several limitations, which include the cross-sectional study design, potential for recall bias on retrospective rating scales, and potential confounding from unmeasured risk factors such as substance abuse and comorbid medical illness. Additionally, we are unable to gather data, demographic or otherwise, from those who decline entry into the study; however, all data analyzed are between resilient and nonresilient traumatized subjects who did participate. Future studies of this population that involve longitudinal assessment, a multidimensional assessment of stressors and protective factors, and measurement of biological risk and resilience markers are needed to more fully understand the role of risk and resilience in this population.
In conclusion, PTSD in the civilian population is associated with substantial psychiatric and functional morbidity and may significantly increase risk for medical illnesses, metabolic syndrome, and diabetes. An understanding of risk and resilience factors in primary care populations is of utmost importance. As we demonstrated here, the CD-RISC measure of resilience may provide one pragmatic, reliable, and simple means of addressing resilience in such high-risk groups seeking general medical care.
Acknowledgments
Funding/Support: This work was primarily supported by a research fellowship award to Dr Wrenn from the Robert Wood Johnson Foundation Clinical Scholars Program. Support was also received from a research fellowship from the American Psychiatric Institute for Research and Education and a National Institutes of Health (NIH) grant (UL RR025008) to Dr Wingo and the National Institutes of Mental Health (MH071537), the Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01RR00039), the American Foundation for Suicide Prevention (Dr Bradley), and the Burroughs Welcome Fund (Dr Ressler).
We thank the participants who graciously shared their stories and their time, and our colleagues Allen W. Graham, India Karapanou, Angelo Brown, Lamya Koury, Lauren Sands, Justine Phifer, Daniel Crain, Nineequa Blanding, Betsy Crowe, Dorothie Ortigo, Kyle Ortigo, Kate Thomas, and Saleem Sayyar for excellent assistance and support.
References
- 1.DiGrande L, Perrin MA, Thorpe LE, et al. Posttraumatic stress symptoms, PTSD, and risk factors among lower Manhattan residents 2–3 years after the September 11, 2001 terrorist attacks. J Trauma Stress. 2008;21(3):264–273. doi: 10.1002/jts.20345. [DOI] [PubMed] [Google Scholar]
- 2.Alim TN, Charney DS, Mellman TA. An overview of posttraumatic stress disorder in African Americans. J Clin Psychol. 2006;62(7):801–813. doi: 10.1002/jclp.20280. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Sonnega A, Bromet E, Hughes M, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatr. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 4.Bonanno GA, Mancini AD. The Human Capacity to Thrive in the Face of Potential Trauma. Pediatrics. 2008;121(2):369–375. doi: 10.1542/peds.2007-1648. [DOI] [PubMed] [Google Scholar]
- 5.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 6.Alim TN, Feder A, Graves RE, et al. Trauma, Resilience, and Recovery in a High-Risk African-American Population. Am J Psychiatry. 2008;165(12):1566–1575. doi: 10.1176/appi.ajp.2008.07121939. [DOI] [PubMed] [Google Scholar]
- 7.Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG. Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. J Trauma Stress. 2008 Apr;21(2):218–22. doi: 10.1002/jts.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boscarino JA. Posttraumatic Stress Disorder and Physical Illness: Results from Clinical and Epidemiologic Studies. Ann New York Acad Sci. 2004;1032 :141–153. doi: 10.1196/annals.1314.011. Biobehavioral Stress Response: Protective and Damaging Effects. [DOI] [PubMed] [Google Scholar]
- 9.Boscarino JA. Posttraumatic Stress Disorder and Mortality Among US Army Veterans 30 Years After Military Service. Ann Epidemiol. 2006;16(4):248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Krause N, Shaw BA, Cairney JA. Descriptive Epidemiology of Lifetime Trauma and the Physical Health Status of Older Adults. Psychol Aging. 2004;19(4):637–648. doi: 10.1037/0882-7974.19.4.637. [DOI] [PubMed] [Google Scholar]
- 11.Vieweg WV, Julius DA, Fernandez A, Tassone DM, Narla SN, Pandurangi AK. Posttraumatic stress disorder in male military veterans with comorbid overweight and obesity: psychotropic, antihypertensive, and metabolic medications. Prim Care Companion. J Clin Psychiatry. 2006;8(1):25–31. doi: 10.4088/pcc.v08n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kinzie JD, Riley C, McFarland B, et al. High prevalence rates of diabetes and hypertension among refugee psychiatric patients. J Nerv Ment Dis. 2008;196(2):108–112. doi: 10.1097/NMD.0b013e318162aa51. [DOI] [PubMed] [Google Scholar]
- 13.Goodwin RD, Davidson JR. Self-reported diabetes and posttraumatic stress disorder among adults in the community. Prev Med. 2005;40(5):570–574. doi: 10.1016/j.ypmed.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 14.Jakovljevic M, Crncevi Z, Martinac M, Maslov B, Topi R. Metabolic syndrome and depression in war veterans with post-traumatic stress disorder. Psychiatria Danubina. 2008;200(3):406. [PubMed] [Google Scholar]
- 15.Weiss T, Skelton K, Phifer J, Jovanovic T, Gillespie CF, et al. Posttraumatic stress disorder is a risk factor for metabolic syndrome in an impoverished urban population. Gen Hosp Psychiatr. 2011 doi: 10.1016/j.genhosppsych.2011.01.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jakovljevic M, Na S, Topi R, Vuksan-usa B. Metabolic syndrome, somatic and psychiatric comorbidity in war veterans with post-traumatic stress disorder: Preliminary findings. Psychiatria Danubina. 2006;18(69) [PubMed] [Google Scholar]
- 17.Jin H, Lanouette NM, Mudaliar S, et al. Association of Posttraumatic Stress Disorder With Increased Prevalence of Metabolic Syndrome. J Clin Psychopharmacol. 2009;29(3):210–215. doi: 10.1097/JCP.0b013e3181a45ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maia DB, Marmar CR, Mendlowicz MV, et al. Abnormal serum lipid profile in Brazilian police officers with post-traumatic stress disorder. J Affect Disord. 2008;107(1–3):259–263. doi: 10.1016/j.jad.2007.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solter V, Thaller V, Karlovic D, Crnkovic D. Elevated serum lipids in veterans with combat-related chronic posttraumatic stress disorder. Croatian Med J. 2002;43(6):683–689. [PubMed] [Google Scholar]
- 20.Bradshaw BG, Richardson GE, Kulkarni K. Thriving with diabetes: an introduction to the resiliency approach for diabetes educators. Diabetes Educ. 2007;33(4):643–649. doi: 10.1177/0145721707303808. [DOI] [PubMed] [Google Scholar]
- 21.Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000;(71):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrow FH, Armstrong Ml, Vargo A, Boothroyd RA. Understanding the findings of resilience-related research for fostering the development of African American adolescents. Child Adolesc Psychiatr Clin N Am. 2007;16(2):393–413. ix–x. doi: 10.1016/j.chc.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Wadsworth ME, Santiago CD. Risk and resiliency processes in ethnically diverse families in poverty. J Fam Psychol. 2008;22(3):399–410. doi: 10.1037/0893-3200.22.3.399. [DOI] [PubMed] [Google Scholar]
- 24.White N, Bichter J, Koeckeritz J, Lee YA, Munch KL. A cross-cultural comparison of family resiliency in hemodialysis patients. J Transcult Nurs. 2002;13(3):218–227. doi: 10.1177/10459602013003011. [DOI] [PubMed] [Google Scholar]
- 25.Bradley R, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatr. 2008;65(2):190–200. doi: 10.1001/archgenpsychiatry.2007.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Binder EB, Bradley R, Liu W, et al. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA. 2008;299(11):1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bernstein DP, Fink L. Childhood Trauma Questionnaire Manual. San Antonio, TX: Psychological Corp; 1998. [Google Scholar]
- 28.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 29.Schwartz AC, Bradley R, Sexton M, Sherry A, Ressler KJ. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatr Serv. 2005;56(2):212–215. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- 30.Gillespie CF, Bradley RG, Mercer K, et al. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatr. 2009;31(6):505–14. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell-Sills L, Stein M. Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 32.Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 33.Foa EB, Tolin DF. Comparison of the PTSD Symptom Scale–Interview Version and the Clinician-Administered PTSD Scale. J Trauma Stress. 2000;13(2):181–191. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- 34.Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder. The Behavior Therapist. 1993;16:161–162. [Google Scholar]
- 35.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]


