Abstract
The glutathione-S-transferase (GST) family contributes to the inactivation of various toxic compounds formed as secondary metabolites during oxidative stress. GSTP1 accounts for the majority of the GST family enzymatic activity, and the activity of GSTP1 enzyme can be altered by the presence of the Ile105Val polymorphism. In this study, we examined the polymorphic frequency of GSTP1 Ile105Val genotype in 920 breast cancer patients and 783 healthy controls in women of North China. Results showed that GSTP1 105Val allele (Ile/Val and Val/Val) was associated with a higher breast cancer risk (OR = 1.38, 95% CI: 1.14–1.69; P = 0.001) and more aggressive tumors with histological grade III (OR = 1.15, 95% CI: 1.05–1.26; P = 0.001), lymph node metastases (OR = 2.35, 95% CI: 1.72–3.21; P < 0.001), as well as ER negative (OR = 1.77, 95% CI: 1.31–2.39; P < 0.001) than those carrying the Ile/Ile allele. However, the patients with the GSTP1 105Val genotype had a better disease free survival after cyclophosphamide (CTX)-based chemotherapy than those with Ile/Ile (HR = 0.77, 95% CI: 0.45–0.91; P < 0.001). Furthermore, in vitro cellular experiments demonstrated that breast cancer cells with the GSTP1 105Val allele were significantly more sensitive to CTX-induced proliferation inhibition. Thus, we conclude that the GSTP1 105Val allele increases breast cancer risk and aggressiveness and enhance response to CTX-based chemotherapy in women of North China. Detection of the GSTP1 Ile105Val genotype may help screen for high-risk populations and direct individualized therapy.
Introduction
Breast cancer is the most common malignancy and the second leading cause of cancer-related death in women worldwide [1]. In China, an increasingly modern lifestyle has been accompanied by a sharp jump in the breast cancer rate in urban areas. Clinical evidence has shown that women at the same pathologic stages of cancer undergoing the same treatment may have different outcomes [2]. In addition to the known risk factors of age, family history, age at childbirth, menopause and hormone therapy, the individual genetic variability also impacts drug metabolism and subsequent efficacy [3]. Chemotherapy has been established as the standard of care for breast cancer patients [4,5], especially those with locally advanced breast cancer. Among the chemotherapy regimens, CTX-based chemotherapy is recommended by the National Comprehensive Cancer Network (NCCN) as the clinical practice guidelines for breast cancer. Although chemotherapy improves disease-free survival (DFS) and overall survival (OS) of breast cancer patients [6], it is challenging to identify the patients who will benefit from chemotherapy and reduce the use of chemotherapy in those who will not benefit.
Glutathione-S-transferases (GSTs), a superfamily of dimeric phase II metabolic enzymes, are divided into six classes and play important roles in the metabolism of products of oxidative stress including by-products of lipid and DNA oxidation [7–9]. GSTP1 encodes the π-class of enzymes which accounts for approximately 90% of the enzymatic activity of the GST family, and its expression is found in many normal and malignant tissues [10]. The GSTP1 enzymatic activity can be altered by genetic polymorphisms. The GSTP1 Ile105Val (rs1695 or rs947894) single-nucleotide polymorphism (SNP) is a transition from an A to a G at nucleotide position 313 (A313G), leading to an Ile105Val amino acid change located near the substrate binding site of the enzyme [11]. The altered protein expression may lead to subsequent development of a malignant phenotype, whereas may enhance chemotherapy efficacy [11–13]. To date, researches have reported the correlation of GSTP1 Ile105Val polymorphisms with breast cancer risk and chemosensitivity [14,15] Several studies have reported that women with the GSTP1 105Val genotype in Shanghai of Southeast China [15,16], America [17], and India [18,19] have greater breast cancer risks. However, some studies have reported conflicting results in women from Italy [20] and Australia [21]. Thus, the role of GSTP1 in breast cancer is also controversial. In particular, the association of GSTP1 Ile105Val genetic polymorphisms with tumor aggressiveness and response to cyclophosphamide (CTX) and CTX-based chemotherapy remains unidentified.
Among individuals with similar GSTP1 expression levels in somatic cells, enzyme catalytic activity would be expected to vary according to the presence of variant GSTP1 genotypes. We speculate that the breast cancer tumors with the GSTP1 105Val variant genotype may have different biological characteristics and responses to CTX-based treatment because of altered enzymatic activity, which may ultimately lead to survival differences of patients. In current study, we examined the distribution frequencies of the GSTP1 Ile105Val genotype in breast cancer patients and age-matched healthy women of North China and evaluated the association of the genotypes with breast cancer risk, tumor aggressiveness and the survival of patients treated with a CTX-based regimen. Furthermore, we validated the differences of individuals with the GSTP1 105Ile and Val alleles in response to CTX cellular cytotoxicity through in vitro experiments.
Results
Genotypic distribution of GSTP1 Ile105Val in breast cancer patients and control subjects
The alleles and genotypic frequencies of GSTP1 Ile105Val in the control population and patients are shown in Table 1. The genotypic frequencies of GSTP1 Ile105Val in the patient population were 58.7% of Ile/Ile, 35.3% of Ile/Val and 6.0% of Val/Val, while in the control group, the genotypic frequencies of GSTP1 Ile105Val genotypes were 66.3% of Ile/Ile, 29.3% of Ile/Val and 4.4% of Val/Val. There were no deviations from Hardy-Weinberg Equilibrium in either the cases or controls (P > 0.05).
Table 1. The genotypic frequencies of the GSTP1 Ile105Val SNP in women of North China: the breast cancer versus control groups.
| Genotype of GSTP1 Ile105Val |
|
|
OR (95% CI) | P-value |
|---|---|---|---|---|
| Ile/Ile | 540 (58.7) | 519 (66.3) | 1.00 | |
| Ile/Val | 325 (35.3) | 230 (29.3) | 1.36 (1.10-1.67) | 0.004 |
| Val/Val | 55 (6.0) | 34 (4.4) | 1.55 (1.00-2.42) | 0.050 |
| Ile/Val and Val/Val | 380 (41.3) | 264 (33.7) | 1.38 (1.14-1.69) | 0.001 |
Association between GSTP1 Ile105Val genotype and breast cancer risk
The comparison between control and breast cancer patient subjects revealed a significant difference among the three GSTP1 Ile105Val genotypes (Ile/Ile, Ile/Val and Val/Val). Logistic regression analysis showed that women carrying the Ile/Val and Val/Val had a OR of 1.36 (95% CI: 1.10-1.67; P = 0.004) and 1.55 (95% CI: 1.00-2.42; P = 0.050), respectively, suggesting that genotypes with the Val allele (Ile/Val and Val/Val) led to an increased risk of breast cancer development (OR = 1.38, 95% CI: 1.14-1.69; P = 0.001; Table 1).
Association between GSTP1 Ile105Val genotypes and clinicopathological characteristics
To further characterize the significance of the GSTP1 Ile105Val genotypes in breast cancer, the associations with various clinicopathological characteristics including patient age, clinical staging, histopathological grading, as well as ER, PR and HER2 status, were analyzed. The results showed that the Ile/Val and Val/Val genotypes of GSTP1 Ile105Val significantly correlated with patient age, histological grade, lymph node involvement, and ER status. The tumors with the Val allele more frequently were histological grade III (OR = 1.15, 95% CI: 1.05-1.26; P = 0.001), ER negative (OR = 1.77, 95% CI: 1.31-2.39; P < 0.001), as well as involved lymph node metastases (OR = 2.35, 95% CI: 1.72-3.21; P <0.001) than tumors with the Ile/Ile allele. No further significant associations were observed between the SNP genotypes and other clinic pathological features (Table 2).
Table 2. The association between GSTP1 Ile105Val genotype and clinicopathological characteristics.
| Characteristics | Genotype of GSTP1
Ile105Val
|
|||
|---|---|---|---|---|
| Ile/Ile (%) | Ile/Val (%) | Val/Val (%) | Ile/Val and Val/Val (%) | |
| Age (year) | ||||
| >=55/<55 | 180 (54.1)/360 (61.3) | 129 (38.7)/196 (33.4) | 24 (7.2)/31 (5.3) | 153 (45.9)/227 (38.7) |
| OR (95% CI) | 1.00 | 1.32 (0.99-1.75) | 1.55 (0.88-2.72) | 1.35 (1.03-1.77) |
| P-value | 0.059 | 0.125 | 0.031 | |
| Histological grade | ||||
| III/I+II | 112 (51.6)/388 (64.1) | 103 (47.5)/202 (33.4) | 32 (14.7)/15 (2.5) | 105 (48.4)/217 (35.9) |
| OR (95% CI) | 1.00 | 1.17 (1.07-1.29) | 2.43 (1.60-3.70) | 1.15 (1.05-1.26) |
| P-value | 0.001 | < 0.001 | 0.001 | |
| Clinical stage | ||||
| III+IV/I+II | 92 (55.4)/447 (62.3) | 62 (37.3)/230 (32.1) | 12 (7.2)/40 (5.6) | 74 (44.6)/270 (37.6) |
| OR (95% CI) | 1.00 | 1.31 (0.92-1.88) | 1.46 (0.74-2.89) | 1.33 (0.95-1.87) |
| P-value | 0.140 | 0.277 | 0.099 | |
| Lymph node involvement | ||||
| Pos. / Neg. | 98 (44.7)/424 (65.5) | 99 (45.2)/193 (29.8) | 22 (10.0)/30 (4.6) | 121 (55.3)/223 (34.5) |
| OR (95% CI) | 1.00 | 2.22 (1.60-3.08) | 3.17 (1.76-5.74) | 2.35 (1.72-3.21) |
| P-value | 0.001 | < 0.001 | < 0.001 | |
| ER status | ||||
| Neg. / Pos. | 114 (46.0)/340 (60.1) | 104 (41.9)/206 (36.4) | 30 (12.1)/20 (3.5) | 134 (54.0)/226 (39.2) |
| OR (95% CI) | 1.00 | 1.51 (1.10-2.07) | 4.47 (2.45-8.19) | 1.77 (1.31-2.39) |
| P-value | 0.011 | < 0.001 | < 0.001 | |
| PR status | ||||
| Neg. / Pos. | 132 (57.1)/334 (57.3) | 83 (35.9)/225 (38.6) | 16 (6.9)/24 (4.1) | 99 (42.8)/249 (42.7) |
| OR (95% CI) | 1.00 | 0.93 (0.68-1.29) | 1.69 (0.87-3.28) | 1.01 (0.74-1.37) |
| P-value | 0.675 | 0.119 | 0.970 | |
| HER2 status | ||||
| Pos. / Neg. | 106 (56.4)/338 (54.0) | 68 (36.2)/252 (40.3) | 14 (7.4)/36 (5.8) | 82 (43.6)/288 (46.0) |
| OR (95% CI) | 1.00 | 0.86 (0.61-1.22) | 1.24 (0.64-2.39) | 0.91 (0.65-1.26) |
| P-value | 0.394 | 0.519 | 0.564 | |
Association between the GSTP1 Ile105Val genotype and DFS in breast cancer patients
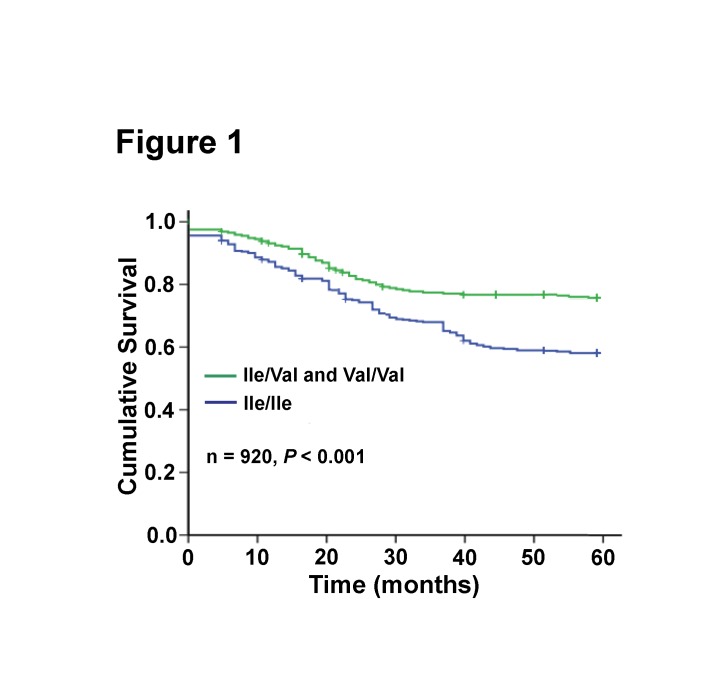
To analyze the relationship between the GSTP1 Ile105Val genotype of breast cancer patients and their prognosis after CTX-based chemotherapy, we compared the 5-year DFS rate between patients with Val allele and those with Ile/Ile genotype. The results indicated that the 5-year DFS rate of patients with the Val allele was higher than those with the Ile/Ile genotype (HR = 0.76, 95% CI: 0.61-0.93; P = 0.008; Table 3). Further Kaplan-Meier DFS analysis showed that the GSTP1 genotype was associated with DFS after analysis with the Cox proportional hazards model (Figure 1).
Table 3. The association between the GSTP1 Ile105Val genotype and 5-year DFS (n = 879).
| Genotype of GSTP1 Ile105Val | Cases | 5-year DFS | HR (95% CI) | P-value |
|---|---|---|---|---|
| Ile/Ile | 518 | 322 | 1.00 | |
| Ile/Val | 309 | 251 | 0.77 (0.62-0.95) | 0.017 |
| Val/Val | 52 | 46 | 0.70 (0.46-1.07) | 0.102 |
| Ile/Val and Val/Val | 361 | 297 | 0.76 (0.61-0.93) | 0.008 |
Figure 1. Kaplan-Meier analysis of DFS among patients with GSTP1 Ile105Val genotypes treated with a CTX-based regimen.
Multivariate analysis for GSTP1 Ile105Val genotype and DFS in breast cancer patients
To determine whether the GSTP1 Ile105Val genotype is an independent factor associated with DFS in breast cancer patients, we performed multivariate analyses. Patient characteristics including the GSTP1 Ile105Val genotype, age, histological grade, clinical stage, lymph node involvement, ER status, PR status, and HER2 status were first evaluated with a univariate analysis. Only the variables with a P < 0.05 in the univariate analysis were included in the multivariate analysis using a backward stepwise Cox proportional hazards regression model (n = 788). Result showed that the GSTP1 Ile105Val genotype was an independent factor associated with the DFS of breast cancer patients (RR = 0.77, 95% CI: 0.45-0.91; P < 0.001; Table 4).
Table 4. Univariate and multivariate analysis of clinicopathological variables affecting 5-year DFS.
| Variable | Comparison | RR (95% CI) | P-value |
|---|---|---|---|
| Univariate | |||
| Age (year) | <55 vs. >=55 | 1.17 (0.49-2.73) | 0.723 |
| Histological grade | III vs. I+II | 1.43 (0.26-4.52) | 0.842 |
| Clinical stage | III+IV vs. I+II | 1.77 (1.29-2.43) | < 0.001 |
| Lymph node status | Pos. vs. Neg. | 2.41 (1.32-3.48) | < 0.001 |
| ER status | Neg. vs. Pos. | 1.32 (0.64-1.62) | 0.419 |
| PR status | Neg. vs. Pos. | 1.27 (0.80-4.62) | 0.217 |
| HER2 status | Pos. vs. Neg. | 1.24 (0.82-3.47) | 0.180 |
| GSTP1 Ile105Val | Ile/Val+Val/Val vs. Ile/Ile | 0.46 (0.34-0.61) | < 0.001 |
| Multivariate (n = 788) | |||
| Clinical stage | III+IV vs. I+II | 1.23 (1.19-1.43) | 0.002 |
| Lymph node status | Pos. vs. Neg. | 1.51 (1.10-3.62) | 0.005 |
| GSTP1 Ile105Val | Ile/Val+Val/Val vs. Ile/Ile | 0.77 (0.45-0.91) | <0.001 |
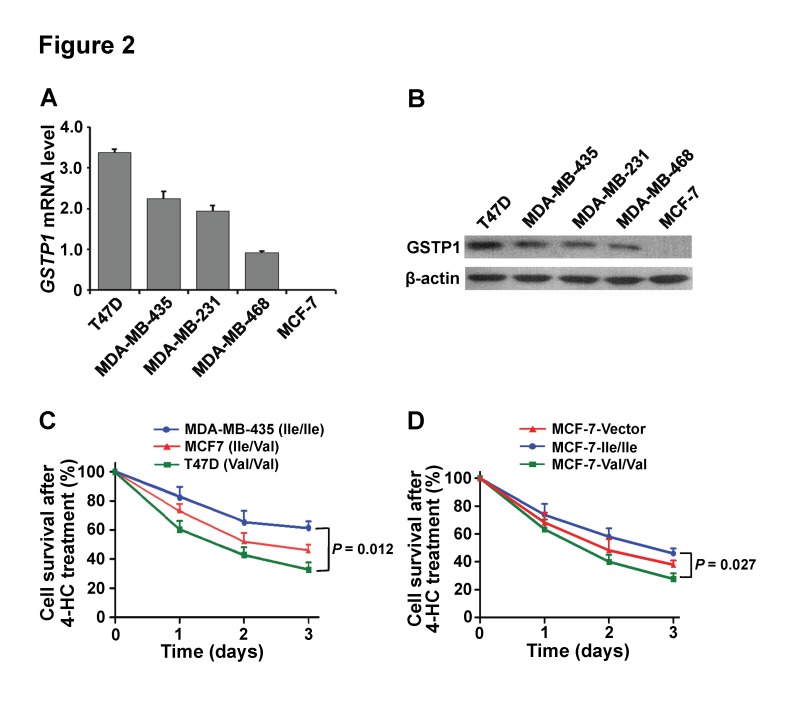
The GSTP1 Ile105Val polymorphism affects the breast cancer cell response to CTX
To investigate the effects of the GSTP1 Ile105Val genotype on breast cancer drug resistance in vitro, we analyzed the mRNA expression levels, protein levels and the GSTP1 Ile105Val genotype in different breast cancer cell lines. The results indicated that GSTP1 mRNA levels were high in T47D, MDA-MB-435, MDA-MB-231 and MDA-MB-468, but were barely detectable in MCF-7 cells (Figure 2A). The same tendency was found in their protein levels (Figure 2B). The GSTP1 Ile105Val genotype was Val/Val in T47D, Ile/Ile in MDA-MB-435, MDA-MB-231 and MDA-MB-468, Ile/Val in MCF-7 cells. Since CTX was activated by hepatic cytochrome P450 enzymes and 4-hydroperoxycyclophosphamide (4-HC) is an active derivative of CTX in vivo, the 4-HC was used to treat the breast cancer cells with different genotype of GSTP1 105Val allele in vitro. The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) cell proliferation assays showed that the T47D cells with Val/Val genotype were more sensitivity to 4-HC-induced proliferation inhibition than the MCF-7 cells with Ile/Val genotype and MDA-MB-435 cells with Ile/Ile genotype (T47D vs. MDA-MB-435, P = 0.012; Figure 2C). Furthermore, the GSTP1 non-expressing MCF-7 cells were transiently transfected with the GSTP1 105Ile/Ile and GSTP1 105 Val/Val GFP fusion plasmids, and than they were treated by 4-HC. The MTT cell proliferation assays confirmed that the GSTP1 105Val/Val genotype enhanced the sensitivity to 4-HC-induced proliferation inhibition compared to the GSTP1 105Ile/Ile genotype in MCF-7 transfected cells (P = 0.027; Figure 2D). The results indicate that GSTP1 Ile105Val affects breast cancer cell response to CTX in vivo.
Figure 2. The GSTP1 Ile105Val polymorphism affects breast cancer cell response to cyclophosphamide.
(A) The GSTP1 mRNA expression levels in breast cancer cell lines were detected using RT-QPCR. (B) The GSTP1 protein expression levels in breast cancer cell lines were detected using western blot. (C) MDA-MB-435 (Ile/Ile), MCF-7 (Ile/Val), and T47D (Val/Val) cells lines were treated with 4-HC (15 µg/mL) for indicated time, and cell survival rates were analyzed using MTT assay at the indicated time points. (D) MCF-7 cells transfected with pEGFP (Vector), pEGFP-GSTP1 105Ile (Ile/Ile), pEGFP-GSTP1 105Val (Val/Val) were treated with 4-HC (15 µg/mL) for indicated time, and cell survival rates were analyzed using MTT assay at the indicated time points. The cells were tested in three independent assays with each containing triplicates and the calculated data of experiments are expressed as mean ± SD.
Discussion
The genotypic distributions of GSTP1 Ile105Val were evaluated based on a large cohort of women with breast cancer and healthy populations in North China. In the healthy control group, the genotypic distributions were 66.3% of Ile/Ile, 29.3% of Ile/Val and 4.4% of Val/Val. The frequency of Val (Ile/Val and Val/Val) alleles (33.7%) is similar to other reports of a Chinese population in Shanghai in Southeast China (33.2%) [15] and Taiwan (33%) [22], but lower than that reported in Indian (54.0%) [19], Slovakian (51.8%) [23], European-American (58%) and African-American populations (65%) [22], and a little higher than that for Englishmen (28%) [11] and Italian (30%) [24] These data indicate that the genotypic distributions of GSTP1 Ile105Val in Chinese populations differ from those in Western and certain other Asian populations. It is known that the allelic frequencies of metabolic genes are not equally distributed throughout human populations, and the frequencies might follow diverse ethnic and/or geographic-specific patterns [23].
Genetic polymorphisms in genes coding metabolic enzymes have been thought to be related to breast cancer susceptibility [25]. In this study, we observed that the GSTP1 105Val (Ile/Val and Val/Val) allele carriers had a higher risk of breast cancer than those with the homozygous Ile/Ile(OR = 1.38). These results are consistent with results from studies of Americans [17], Indians [18,19], and Chinese in Shanghai in Southeast China [16]. However, in several studies on African-Americans [20], white women in North Carolina [26] and Caucasians [21], no significant differences were found between the GSTP1 Ile105Val polymorphism and breast cancer risk. Studies of the Finnish [27] and Koreans [14] showed that the GSTP1 105Val allele was associated with a lower risk of breast cancer. A recent meta-analysis showed that GSTP1 105Val was associated with an increased breast cancer risk in Chinese populations but not in non-Chinese populations [28], which is consistent with our results. The GSTP1 enzyme plays an important role in the metabolism and inactivation of various toxic compounds [29]. The Ile105Val polymorphism is a transition from an A to a G in nucleotide position 313 (A313G), leading to an Ile105Val amino acid change located near the substrate binding site of the enzyme. The altered protein expression may lead to subsequent accumulation of carcinogens in the body, resulting in the development of a malignant phenotype. The environmental pollution in developing countries such as China and India caused by increasing population levels and changes in modern lifestyle may contribute to the increased breast cancer risk in those with the GSTP1 105Val allele.
In addition, we found that breast cancer patients with the GSTP1 105Val allele were more likely to bear a tumor with histological grade III, lymph node metastases, as well as ER negative than those carrying the Ile/Ile allele. Our evidence indicates that the GSTP1 with the 105Val variant lost or reduced enzyme activity compared with Ile/Ile genotype leading to the accumulation of toxic substances in the body. The toxic damage to genomic DNA in somatic cells not only induces carcinogenesis [30] but also causes tumors with more aggressive characteristics such as poor differentiation, hormone-independent growth and metastatic potential.
The GSTP1 105Val genotype is an unfavorable factor for healthy females, however, it is a favorable factor for the cytotoxic efficacy of chemotherapy for breast cancer patients. Thus, the patients with the 105Val genotype may have better prognosis than those homozygous for Ile/Ile. The report in Shanghai revealed that breast cancer patients with the GSTP1 105Val allele had a 60% reduction in mortality risk after chemotherapy (HR = 0.4, 95% CI: 0.2-0.8) [30]. Our results further demonstrated that the GSTP1 105Val genotype provided a good prognosis for breast cancer patients in a Chinese population after receiving CTX-based chemotherapy (HR = 0.77, 95% CI: 0.45-0.91). However, this genotype was not associated with prognosis in breast cancer patients receiving CTX-containing chemotherapy in North American [31]. The GSTP1 enzyme exhibits specific and high activity in the conjugation of CTX and its toxic metabolites [32]. The SNP of GSTP1 Ile105Val substitutions in the coding sequence results amino acid changes within the GSTP1 substrate-binding site [10,33]. Evidence has demonstrated that the GSTP1 105Val variant is associated with a lower thermal stability and altered catalytic activity to a variety of substrates compared with GSTP1 105Ile [30] and presents a reduced ability to detoxify chemotherapeutic agents, which results in lower clearance and better efficacy. We further investigated the effect of the GSTP1 Ile105Val genotype on breast cancer drug resistance through in vitro cellular experiments. The results confirmed that the breast cancer cells with the GSTP1 105Val/Val genotype exhibited increased sensitivity to 4-HC, which is an active derivative of CTX in vivo, than the cells with the Ile/Ile genotype. The results provide further evidence that the GSTP1 Ile105Val genotype affects the therapeutic response and survival of breast cancer patients treated with CTX.
In summary, our results demonstrated that among women in North China, the GSTP1 105Val allele carries a higher breast cancer risk and a risk of more aggressive tumors. However, patients with this allele have a trend toward improved survival after treatment with CTX-based chemotherapy. Therefore, the GSTP1 Ile105Val genotype could serve as a molecular test to screen for a high risk of breast cancer, to evaluate breast cancer aggressiveness and to predict the efficacy of CTX-based chemotherapy in Chinese populations. Due to the limited number of cases with rare genotype Val/Val of GSTP1 lle105Val in this study, the preventive, diagnostic and therapeutic values of the genetyping for women and breast cancer patients should be further evaluated and confirmed by large multicenter studies.
Materials and Methods
Patients
A total of 920 breast cancer patients (aged 24-65 years, mean age 54.3 years) and 783 healthy women (aged 21-69 years, mean age 53.2 years) were recruited for this study. A t-test indicated that the mean age of these two population groups was equal (P = 0.120). All patients and control individuals were genetically unrelated women from North China. A total of 796 patients underwent unilateral mastectomy and dissection of axillary lymph nodes in Tianjin Medical University Cancer Institute and Hospital (TMUCIH; Tianjin, China) from January 2005 to January 2007, and diagnoses were confirmed based on pathological examinations. The remaining 124 patients were post-surgical re-examination at TMUCIH. All cases were diagnosed as invasive carcinoma. Detailed clinicopathological information including patient age, clinical stage, tumor size, histological grade, lymph node involvement, as well as estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) statuses are presented in Table 5. ER, PR and HER2 statuses in breast cancer tissues were determined through immunohistochemical staining. All patients received CTX-based chemotherapy for at least 4 cycles. CTX was administered through an intravenous injection line. The doses were within the standard range of 500–600 mg/m2. The imaging examination (ultrasound, X-ray, MRI, ECT and CT) and/or pathological diagnosis were performed to monitor for DFS status in the follow-up. DFS was defined as the time interval between primary surgery and any relapse (local-regional, contra-lateral and/or distant), or terminal time of follow-up without any relapse events. 879 of 920 cases were followed-up with over five years. This study was approved by the Institutional Review Board of TMUCIH, and written consent was obtained from all participants.
Table 5. Clinicopathological characteristics of breast cancer patients.
|
Characteristics
|
Cases (%) | |
|---|---|---|
| Age (year) | < 55 | 587 (63.8) |
| > = 55 | 333 (36.2) | |
| Clinical stage | I+II | 717 (77.9) |
| III+IV | 166 (18.0) | |
| Unknown | 37 (4.1) | |
| Lymph node status | Negative | 647 (70.3) |
| Positive | 219 (23.8) | |
| Unknown | 54 (5.9) | |
| Histological grade | I+II | 605 (65.7) |
| III | 217 (23.6) | |
| Unknown | 98 (10.7) | |
| ER status | Positive | 566 (61.5) |
| Negative | 248 (27.0) | |
| Unknown | 106 (11.5) | |
| PR status | Positive | 583 (63.4) |
| Negative | 231 (23.1) | |
| Unknown | 106 (11.5) | |
| HER2 status | Negative | 626 (68.1) |
| Positive | 188 (20.4) | |
| Unknown | 106 (11.5) | |
| 5-years DFS | Negative | 619 (67.3) |
| Positive | 260 (28.3) | |
| Unknown | 41 (4.4) | |
Note: “Unknown” represents the number (%) of cases for which the corresponding information was not available.
Cell culture
The breast cancer cell lines MCF-7, T-47D, MDA-MB-468, MDA-MB-231 and MDA-MB-435 were obtained from the American Type Culture Collection (ATCC). The cells were cultured in RPMI 1640 (MCF-7 and MDA-MB-231) or DMEM/F12 (T-47D, MDA-MB-468 and MDA-MB-435) medium supplemented with 10% fetal bovine serum, 100 units/mL penicillin and 100 µg/mL streptomycin (Invitrogen, Carlsbad, CA, USA) and incubated in a humidified atmosphere with 5% CO2 at 37°C.
Specimens and genomic DNA extraction
A volume of 2 mL of peripheral blood was collected from each individual and treated with EDTA-K2 anticoagulant. Nucleated cells were then separated by hypotonic lysis of red blood cells as described previously [34]. Genomic DNA from nucleated cells and cultured cells was extracted according to standard methods using proteinase K followed by phenol/chloroform/isopropanol treatment or using QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA, USA). DNA concentrations were determined with a UV spectrophotometer. DNA integrity and purity were assayed through 1.5% agarose gel electrophoresis. TE buffer (10 mM Tris-HCl and 1.0 mM EDTA, pH 8.0) was used for resuspending DNA, with the final concentration adjusted to 200-500 ng/µL. The DNA solutions were frozen and stored at −80°C.
Genotyping by the TaqMan allelic discrimination assay
The primers and TaqMan probes for the genotypic analysis of GSTP1 Ile105Val were designed and optimized using Oligo 6.0 software (Molecular Biology Insights, West Cascade, USA), and synthesized by Sangon Biological Engineering Technology & Services Co, Ltd. (Shanghai, China). The PCR-TaqMan allelic discrimination assays were performed using the Platinum Quantitative PCR SuperMix-UDG System (Invitrogen) according to the manufacturer’s instructions with the ABI 7500 TaqMan system (Applied Biosystems, Carlsbad, CA, USA).
DNA sequencing
To validate the data generated by PCR-TaqMan assay, 10% of the samples were randomly sequenced. The sequencing reactions were performed according to the conventional dideoxy chain-termination method using an ABI PRISMTM 3130 Genetic Analyzer (Applied Biosystem).
Construction and transfection of GSTP1 105 Ile and Val expression plasmids
The GSTP1 Ile105Val genotypes of the breast cancer cells MCF-7, T-47D, MDA-MB-231 and MDA-MB-435 were detected using the TaqMan allelic discrimination assay and were confirmed through DNA sequencing. PCR was performed to amplify GSTP1 105Ile (A/A) and Val (G/G) full-length cDNAs from cell lines with the corresponding genotype. The primers were 5’-CCAAGCTTACCATGCCGCCCTACACC-3’ (forward) and 5’-CCGGATCCTGTTTCCCGTTGCCAT-3’ (reverse), with BamHI and HindIII restriction endonuclease recognition sites (underlined) on the 5’ ends. The PCR reactions were performed in a volume of 50 µL at 95°C for 2 min and 35 cycles of 95°C for 30s, 58°C for 1 min, and 72°C for 1 min, followed by 72°C for 10 min. The PCR products were subcloned into the pCR2.1 plasmids (Invitrogen) and expanded in DH5 alpha E. coli. Full-length cDNAs with GSTP1 105Ile and Val genotypes were digested from pCR2.1 using restriction endonucleases and subcloned into the NH2-terminus of green fluorescent protein (GFP) of the mammalian expression plasmid pEGFP-N1 (Clontech, Palo Alto, CA, USA). The GSTP1s sequences in the recombinant plasmids were confirmed through DNA sequencing, and GSTP1s expression levels were detected using reverse transcription-quantitative polymerase chain reaction (RT-QPCR) and western blot assays. For transient transfection, 2×105 MCF7 cells per well in 6-well plates were cultured without antibiotics overnight and then transfected with recombinant plasmids using Lipofectamine 2000 reagent (Invitrogen) according to the manufacturer’s instructions.
RT-QPCR
Total RNA from cultured cells was extracted with TRIZOL reagent, reverse transcription (RT) was performed using the SuperScript First-Strand cDNAs Synthesis kit, and real-time quantitative PCR (QPCR) was performed using Platinum SYBR Green qPCR SuperMix-UDG. All reagents were Invitrogen products, and the reactions were performed according to the manufacturer’s instructions. The primers for GSTP1 cDNA amplification were 5’-AGGACCTCCGCTGCAAATACATCT-3’ and 5’-TCTCCCACAATGAAGGTCTTG-3’. The primers for the housekeeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH) were as previously described [35]. QPCR was performed with the parameters of 50°C for 2 min, pre-denaturation at 95°C for 3 min, and 45 cycles at 95°C for 30 sec and 62°C for 1 min. Target gene expression quantification in samples was accomplished by measuring the fractional cycle number at which the amount of expression reached a fixed threshold (CT). Triplicate CT values were averaged, and GAPDH CT was subtracted from GSTP1 CT to obtain ΔCT. The relative amount of GSTP1 mRNA was calculated as 2-ΔCT.
Western blot
Cultured cells were solubilized with protein lysis buffer. The proteins were separated by size using SDS-PAGE and transferred to polyvinyldifluoride membranes (Pierce, Rockford, IL, USA). The membranes were blocked with 5% milk in TBST (10 mM Tris, 150 mM NaCl, 0.05% Tween 20, pH 8.3) for 60 min at room temperature and incubated with a 1:1000 dilution of rabbit polyclonal anti-GSTP1 antibody (Sigma, St. Louis, MO, USA) in TBST-milk overnight at 4 °C. Non-bound primary antibody was removed by washing in TBST, and bound antibody was detected using HRP-conjugated goat anti-rabbit IgG. The immunoreactive protein bands were visualized by enhanced chemiluminescence (ECL) reagents (GE Healthcare).
MTT assay
To assess the effect of the GSTP1 Ile105Val genotype on anti-cancer drug resistance, MDA-MB-435 (Ile/Ile), MCF-7 (Ile/Val) and T47D (Val/Val) cells lines were assessed using the MTT assay. T47D cells (Val/Val), MDA-MB-435 cells (Ile/Ile) and MCF-7 cells (Ile/Val) were treated by 4-HC and analyzed the cell proliferation using MTT assay. MCF-7 cells, which do not express GSTP1, were transfected with pEGFP-GSTP1 105Ile (Ile/Ile), pEGFP-GSTP1 105Val (Val/Val), and the vector control pEGFP-N1, and then also were treated by 4-HC and analyzed using MTT assay. All the cells were plated at 1×104 cells per well in 96-well plates and incubated with 15 µg/mL 4-HC for 24, 48 and 72 h. Then, 10 µL of MTT (5 g/L in PBS) was added to each well and incubated at 37 °C for 4 h, and the medium was replaced by 100 µL DMSO to dissolve the formazan. Absorbance was measured at 570 nm using a spectrophotometer. Cell viability was calculated as the value relative to control cultures. The cells were tested in three independent assays with each containing triplicates
Statistical analyses
The Chi-square (χ2) test or Fisher’s exact test was used to compare the SNP genotypic distributions between the breast cancer group and the healthy controls, among cancer patients with various clinicopathological parameters, and for analysis of the Hardy-Weinberg equilibrium. Polytomous logistic regression was used to estimate the odds ratios (OR) and 95 percent confidence intervals (95% CI) as measures of association between the genotypes and breast cancer risk subtypes or to compare case subtypes to all controls. Survival analyses were performed according to the Kaplan and Meier methods and assessed using the log-rank test. All prognostic variables in the multivariate survival analysis were performed using a backward stepwise Cox proportional hazards regression model, and hazard ratio (HR) and relative risk (RR) were calculated from the Cox model. Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS, version 19.0). P-values less than 0.05 were considered statistically significant. All calculated data of experiments in vitro are expressed as mean ± standard deviation (SD).
Funding Statement
This study was supported by the National Natural Science Foundation of China (No. 30872518 and No. 81272357), the Major Program of Applied Basic Research Projects of Tianjin (No. 06YFJMJC12900 and No. 09JCZDJC19800) and the Technology Program of Tianjin Health Bureau (No. 2011kZ83). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Jemal A, Siegel R, Ward E, Hao Y, Xu J et al. (2009) Cancer statistics, 2009. CA Cancer J Clin 59: 225-249. doi:10.3322/caac.20006. PubMed: 19474385. [DOI] [PubMed] [Google Scholar]
- 2. Collaborative Group on Hormonal Factors in Breast Cancer (2002) Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet 360: 187-195. doi:10.1016/S0140-6736(02)09454-0. PubMed: 12133652. [DOI] [PubMed] [Google Scholar]
- 3. Eichelbaum M, Ingelman-Sundberg M, Evans WE (2006) Pharmacogenomics and individualized drug therapy. Annu Rev Med 57: 119-137. doi:10.1146/annurev.med.56.082103.104724. PubMed: 16409140. [DOI] [PubMed] [Google Scholar]
- 4. Ragaz J, Olivotto IA, Spinelli JJ, Phillips N, Jackson SM et al. (2005) Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst 97: 116-126. doi:10.1093/jnci/djh297. PubMed: 15657341. [DOI] [PubMed] [Google Scholar]
- 5. Chia S, Swain SM, Byrd DR, Mankoff DA (2008) Locally advanced and inflammatory breast cancer. J Clin Oncol 26: 786-790. doi:10.1200/JCO.2008.15.0243. PubMed: 18258987. [DOI] [PubMed] [Google Scholar]
- 6. Levine MN, Whelan T (2006) Adjuvant chemotherapy for breast cancer--30 years later. N Engl J Med 355: 1920-1922. doi:10.1056/NEJMe068204. PubMed: 17079767. [DOI] [PubMed] [Google Scholar]
- 7. Schröder KR, Wiebel FA, Reich S, Dannappel D, Bolt HM et al. (1995) Glutathione-S-transferase (GST) theta polymorphism influences background SCE rate. Arch Toxicol 69: 505-507. doi:10.1007/s002040050205. PubMed: 8526747. [DOI] [PubMed] [Google Scholar]
- 8. Hayes JD, Strange RC (1995) Potential contribution of the glutathione S-transferase supergene family to resistance to oxidative stress. Free Radic Res 22: 193-207. doi:10.3109/10715769509147539. PubMed: 7757196. [DOI] [PubMed] [Google Scholar]
- 9. Zhang J, Tian Q, Yung Chan S, Chuen Li S, Zhou S et al. (2005) Metabolism and transport of oxazaphosphorines and the clinical implications. Drug Metab Rev 37: 611-703. doi:10.1080/03602530500364023. PubMed: 16393888. [DOI] [PubMed] [Google Scholar]
- 10. Townsend DM, Tew KD (2003) The role of glutathione-S-transferase in anti-cancer drug resistance. Oncogene 22: 7369-7375. doi:10.1038/sj.onc.1206940. PubMed: 14576844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harries LW, Stubbins MJ, Forman D, Howard GC, Wolf CR (1997) Identification of genetic polymorphisms at the glutathione S-transferase Pi locus and association with susceptibility to bladder, testicular and prostate cancer. Carcinogenesis 18: 641-644. doi:10.1093/carcin/18.4.641. PubMed: 9111193. [DOI] [PubMed] [Google Scholar]
- 12. Smith G, Stanley LA, Sim E, Strange RC, Wolf CR (1995) Metabolic polymorphisms and cancer susceptibility. Cancer Surv 25: 27-65. PubMed: 8718512. [PubMed] [Google Scholar]
- 13. White DL, Li D, Nurgalieva Z, El-Serag HB (2008) Genetic variants of glutathione S-transferase as possible risk factors for hepatocellular carcinoma: a HuGE systematic review and meta-analysis. Am J Epidemiol 167: 377-389. doi:10.1093/aje/kwm315. PubMed: 18065725. [DOI] [PubMed] [Google Scholar]
- 14. Kim SU, Lee KM, Park SK, Yoo KY, Noh DY et al. (2004) Genetic polymorphism of glutathione S-transferase P1 and breast cancer risk. J Biochem Mol Biol 37: 582-585. doi:10.5483/BMBRep.2004.37.5.582. PubMed: 15479622. [DOI] [PubMed] [Google Scholar]
- 15. Egan KM, Cai Q, Shu XO, Jin F, Zhu TL et al. (2004) Genetic polymorphisms in GSTM1, GSTP1, and GSTT1 and the risk for breast cancer: results from the Shanghai Breast Cancer Study and meta-analysis. Cancer Epidemiol Biomarkers Prev 13: 197-204. doi:10.1158/1055-9965.EPI-03-0294. PubMed: 14973092. [DOI] [PubMed] [Google Scholar]
- 16. Lee SA, Fowke JH, Lu W, Ye C, Zheng Y et al. (2008) Cruciferous vegetables, the GSTP1 Ile105Val genetic polymorphism, and breast cancer risk. Am J Clin Nutr 87: 753-760. PubMed: 18326615. [DOI] [PubMed] [Google Scholar]
- 17. Kadouri L, Kote-Jarai Z, Hubert A, Baras M, Abeliovich D et al. (2008) Glutathione-S-transferase M1, T1 and P1 polymorphisms, and breast cancer risk, in BRCA1/2 mutation carriers. Br J Cancer 98: 2006-2010. doi:10.1038/sj.bjc.6604394. PubMed: 18542066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Saxena A, Dhillon VS, Raish M, Asim M, Rehman S et al. (2009) Detection and relevance of germline genetic polymorphisms in glutathione S-transferases (GSTs) in breast cancer patients from northern Indian population. Breast Cancer Res Treat 115: 537-543. doi:10.1007/s10549-008-0098-y. PubMed: 18574688. [DOI] [PubMed] [Google Scholar]
- 19. Samson M, Swaminathan R, Rama R, Sridevi V, Nancy KN et al. (2007) Role of GSTM1 (Null/Present), GSTP1 (Ile105Val) and P53 (Arg72Pro) genetic polymorphisms and the risk of breast cancer: a case control study from South India. Asian Pac J Cancer Prev 8: 253-257. PubMed: 17696741. [PubMed] [Google Scholar]
- 20. Vogl FD, Taioli E, Maugard C, Zheng W, Pinto LF et al. (2004) Glutathione S-transferases M1, T1, and P1 and breast cancer: a pooled analysis. Cancer Epidemiol Biomarkers Prev 13: 1473-1479. PubMed: 15342448. [PubMed] [Google Scholar]
- 21. Curran JE, Weinstein SR, Griffiths LR (2000) Polymorphisms of glutathione S-transferase genes (GSTM1, GSTP1 and GSTT1) and breast cancer susceptibility. Cancer Lett 153: 113-120. doi:10.1016/S0304-3835(00)00361-X. PubMed: 10779639. [DOI] [PubMed] [Google Scholar]
- 22. Watson MA, Stewart RK, Smith GB, Massey TE, Bell DA (1998) Human glutathione S-transferase P1 polymorphisms: relationship to lung tissue enzyme activity and population frequency distribution. Carcinogenesis 19: 275-280. doi:10.1093/carcin/19.2.275. PubMed: 9498276. [DOI] [PubMed] [Google Scholar]
- 23. Sivonova M, Waczulikova I, Dobrota D, Matakova T, Hatok J et al. (2009). Polymorphisms of glutathione-S-transferase M1, T1, P1 and the risk of prostate cancer: a case-control study. J Exp Clin Cancer Res 28: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hohaus S, Di Ruscio A, Di Febo A, Massini G, D’Alo’ F et al. (2005) Glutathione S-transferase P1 genotype and prognosis in Hodgkin’s lymphoma. Clin Cancer Res 11: 2175-2179. doi:10.1158/1078-0432.CCR-04-1250. PubMed: 15788664. [DOI] [PubMed] [Google Scholar]
- 25. Saxena A, Dhillon VS, Shahid M, Khalil HS, Rani M et al. (2013) GSTP1 methylation and polymorphism increase the risk of breast cancer and the effects of diet and lifestyle in breast cancer patients. Exp Ther Med 4: 1097-1103. PubMed: 23226781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Millikan R, Pittman G, Tse CK, Savitz DA, Newman B et al. (2000) Glutathione S-transferases M1, T1, and P1 and breast cancer. Cancer Epidemiol Biomarkers Prev 9: 567-573. PubMed: 10868690. [PubMed] [Google Scholar]
- 27. Mitrunen K, Jourenkova N, Kataja V, Eskelinen M, Kosma VM et al. (2001) Glutathione S-transferase M1, M3, P1, and T1 genetic polymorphisms and susceptibility to breast cancer. Cancer Epidemiol Biomarkers Prev 10: 229-236. [PubMed] [Google Scholar]
- 28. Sergentanis TN (2010) Economopoulos KP GSTT1 and GSTP1 polymorphisms and breast cancer risk: a meta-analysis. Breast Cancer Res Treat 121: 195-202. doi:10.1007/s10549-009-0520-0. PubMed: 19760040. [DOI] [PubMed] [Google Scholar]
- 29. Hayes JD, Flanagan JU, Jowsey IR (2005) Glutathione transferases. Annu Rev Pharmacol Toxicol 45: 51-88. doi:10.1146/annurev.pharmtox.45.120403.095857. PubMed: 15822171. [DOI] [PubMed] [Google Scholar]
- 30. Yang G, Shu XO, Ruan ZX, Cai QY, Jin F et al. (2005) Genetic polymorphisms in glutathione-S-transferase genes (GSTM1, GSTT1, GSTP1) and survival after chemotherapy for invasive breast carcinoma. Cancer 103: 52-58. doi:10.1002/cncr.20729. PubMed: 15565566. [DOI] [PubMed] [Google Scholar]
- 31. Yao S, Barlow WE, Albain KS, Choi JY, Zhao H et al. (2010) Gene polymorphisms in cyclophosphamide metabolism pathway,treatment-related toxicity, and disease-free survival in SWOG 8897 clinical trial for breast cancer. Clin Cancer Res 16: 6169-6176. doi:10.1158/1078-0432.CCR-10-0281. PubMed: 21169260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dirven HA, van Ommen B, van Bladeren PJ (1994) Involvement of human glutathione S-transferase isoenzymes in the conjugation of cyclophosphamide metabolites with glutathione. Cancer Res 54: 6215-6220. PubMed: 7954469. [PubMed] [Google Scholar]
- 33. Johansson AS, Stenberg G, Widersten M, Mannervik B (1998) Structure-activity relationships and thermal stability of human glutathione transferase P1-1 governed by the H-site residue 105. J Mol Biol 278: 687-698. doi:10.1006/jmbi.1998.1708. PubMed: 9600848. [DOI] [PubMed] [Google Scholar]
- 34. Chen XH, Li XQ, Chen Y, Feng YM (2011) Risk of aggressive breast cancer in women of Han nationality carrying TGFB1 rs1982073 C allele and FGFR2 rs1219648 G allele in North China. Breast Cancer Res Treat 125: 575-582. doi:10.1007/s10549-010-1032-7. PubMed: 20640597. [DOI] [PubMed] [Google Scholar]
- 35. Feng Y, Sun B, Li X, Zhang L, Niu Y et al. (2007) Differentially expressed genes between primary cancer and paired lymph node metastases predict clinical outcome of node-positive breast cancer patients. Breast Cancer Res Treat 103: 319-329. doi:10.1007/s10549-006-9385-7. PubMed: 17123152. [DOI] [PubMed] [Google Scholar]