Abstract
Objective
No studies to date have compared parenting behaviors of men with co-occurring intimate partner violence (IPV) and substance abuse (SA) with community controls. This study was designed to document mediators of differences in parenting behavior of fathers and the emotional-behavioral problems of their children for men with co-occurring SA and IPV.
Method
The self-reported parenting (negative, positive and co-parenting behaviors) and the child emotional-behavioral problems of 43 fathers with children aged 2 to 6 years with a recent history of SA + IPV were compared to a sample of 43 community control fathers with the same socio-economic and cultural backgrounds. Fathers completed measures on their parenting behavior with a target child, co-parenting behavior with the child’s mother, emotion regulation, romantic attachment, psychiatric symptoms, and the behavior of the target child.
Results
Men with co-occurring SA + IPV had significantly less positive co-parenting and more negative parenting behaviors than community control fathers. Negative parenting and co-parenting were mediated by the fathers’ avoidant attachment problems. SA + IPV fathers also reported more emotional and behavioral problems in their children. These poor child outcome differences between groups were mediated by the negative parenting behaviors of the fathers.
Conclusions
These results suggest areas of potential focus in interventions with fathers who have co-occurring SA + IPV issues. Focus on attachment difficulties with his co-parent, which may include affect regulation, coping with emotions, and communication skills training related to co-parenting, may yield significant changes in parenting behaviors and ultimately child functioning.
Although fathering has gained increasing attention in both the clinical and research literature (e.g. Lamb, 2004; Pruett, 1983), there are still significant gaps in our knowledge about the impact of various psychiatric conditions, substance abuse disorders, and personality styles of fathers on child development (Marsiglio, Amato, Day, & Lamb, 2000). This is particularly true in the area of fathers who have histories of intimate partner violence (IPV) and co-occurring substance abuse (SA). The co-occurrence of SA and IPV (SA + IPV) has been shown to be between 40% and 50% (e.g., seenEaston, Swan, & Sinha, 2000) with two recent meta-analytic reviews revealing significant effect sizes for the association of alcohol and drug use with IPV (Foran & O’Leary, 2008; Moore et al., 2008). Additionally, there is substantial evidence to demonstrate the deleterious effects of parental substance abuse and witnessing IPV on children (Edleson, 1999; Edleson et al., 2007; Edleson, Mbilinyi, Beeman, & Hagemeister, 2003; J. L. Johnson & Leff, 1999; Kendall-Tackett, 2004; Peled, Jaffe, & Edleson, 1995; West & Prinz, 1987), and children exposed to IPV are at increased risk for child abuse (Edleson, 2001; Hamby, Finkelhor, Turner, & Ormrod, 2010). Yet, there are few quantitative studies to evaluate the parenting of aggressive, substance-abusing men and few that interview fathers directly. This study was designed as the first to examine the parenting behaviors of fathers of preschool children with co-occurring SA + IPV and document variables that mediate differences in parenting and child symptoms based on father reports.
Substance Abusing or Battering Men as Fathers
Several researchers have shown that alcoholic fathers demonstrate less sensitive parenting with greater negative affect (Eiden, Edwards, & Leonard, 2002), and fewer positive father-child interactions (Eiden, Chavez, & Leonard, 1999; El-Sheikh & Buckhalt, 2003; El-Sheikh & Flanagan, 2001). Blackson and colleagues (Blackson et al., 1999) also noted that when compared to fathers with no history of substance abuse problems, fathers with a history of alcohol and drug abuse reported: poorer father-child communication, greater risk for physical abuse, poorer parent-child relationships, and more parenting stress. Both Zhou, King, and Chassin (2006) and Jacob and colleagues (1991) found less family cohesion and problems in parent-child interactions for adolescents with substance abusing fathers. Fals-Stewart and colleagues (2004) found drug-abusing fathers to self-report more problematic disciplinary practices and less monitoring of their children. In their study, drug-abusing fathers demonstrated the most negative parenting behaviors compared to both alcoholic fathers and men with no history of alcohol or drug abuse. Finally, and contrary to other studies, McMahon, Winkel, and Rounsaville (2008) found the scope of drug abusing fathers involvement to be limited, but no significant differences in the frequency of positive or negative parenting behavior reported by opioid-dependent men on methadone maintenance compared to fathers with no history of alcohol or drug abuse.
There is less research literature specific to the parenting of fathers who perpetrate IPV. There is evidence based on interviews with battered women that some fathers who perpetrate IPV use their children to manipulate their current or former partners and directly involve children in IPV incidents (Bancroft & Silverman, 2002; Edleson, Mbilinyi, Beeman, et al., 2003; Edleson, Mbilinyi, & Shetty, 2003). Two studies, which did interview fathers directly, found that increased partner abuse was associated with lower feelings of parental competence (Baker, Perilla, & Norris, 2001) and fathers with histories of IPV report more hostile-aggressive parenting than fathers without a history of IPV (Fox & Benson, 2004). Still, there is also evidence to suggest some fathers who perpetrate IPV are concerned about the impact of their violence on their children (Rothman, Mandel, & Silverman, 2007), report a significant amount of shame and guilt about the harm they may have caused their children (Litton Fox, Sayers, & Bruce, 2001), and report a wish to be a good father to their children (Mbilinyi et al., 2009).
Characteristics of Men with Co-Occurring Substance Abuse and IPV
Despite substantial evidence of approximately half of men entering substance abuse treatment reporting concurrent IPV(Easton et al., 2000) and vice versa (Stuart, Moore, Kahler, & Ramsey, 2003), little is known about the unique features of this sub-population of men. There is significant co-morbidity of SA with other psychiatric conditions such as depression, PTSD, and anxiety (NIMH, 2003). Impulsivity and problems regulating emotional states are common difficulties for substance abusers (Bonn-Miller, Vujanovic, & Zvolensky, 2008; Cuomo, Sarchiapone, Giannantonio, Mancini, & Roy, 2008; Perry & Carroll, 2008) and those with co-occurring IPV (Easton, Sacco, Neavins, Wupperman, & George, 2008). Studies have found associations between adult attachment problems and subgroups of IPV perpetrators (Holtzworth-Monroe & Meehan, 2004; Roberts, Wolfer, & Mele, 2008; Scott & Babcock, 2010); and insecure attachment styles in romantic relationships have been shown to be significantly associated with child abuse potential in fathers (Howard, 2010). Thus, problems with impulsivity and emotional control, psychiatric symptoms and attachment difficulties of fathers with co-occurring substance abuse and IPV likely significantly impact parenting abilities. Understanding how such characteristics of fathers with co-occurring SA and IPV may contribute to their negative parenting is crucial to the development of appropriate intervention efforts to reduce instances of child maltreatment. Studies of substance abusing mothers (Hans, Bernstein, & Henson, 1999; Luthar & Sexton, 2007) and fathers (Stover, McMahon, & Easton, 2012; Stover, Urdahl, & Easton, 2012) have found psychiatric symptoms to be stronger predictors of negative parenting than SA. Assessment of such problems and their relationship to negative parenting has not been explored in a sample of fathers with co-occurring SA and IPV.
This study is the first to specifically recruit a sample of fathers with co-occurring SA and IPV and compare their parenting behaviors and report of their child’s symptoms with fathers from the same community without these co-occurring issues. It utilizes a case controlled study design to begin to document what accounts for differences in men with co-occurring SA and IPV. It specifically tested two research hypotheses: (1) When compared with fathers with no history of SA or IPV, fathers with co-occurring SA + IPV will report more negative parenting and co-parenting behaviors and fewer positive parenting behaviors and those group differences will be mediated by differences in emotion regulation, psychiatric symptoms, and attachment difficulties (See Figure 1); and (2) When compared with fathers with no history of SA or IPV, fathers with co-occurring SA + IPV will report more emotional and behavioral difficulty in their children and those group differences will be mediated by differences in the parenting and co-parenting behaviors of the fathers (See Figure 2).
Figure 1.
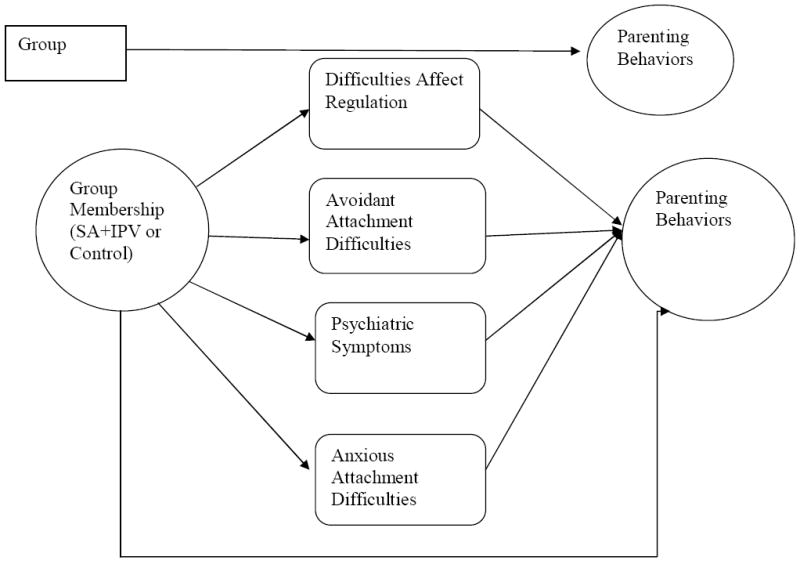
Mediation Model for Parenting Behaviors
Note: Three models were generated with Parent Behavior represented by 1) Co-Parenting, 2) Negative Parenting, and 3) Positive Parenting Behaviors
Figure 2.
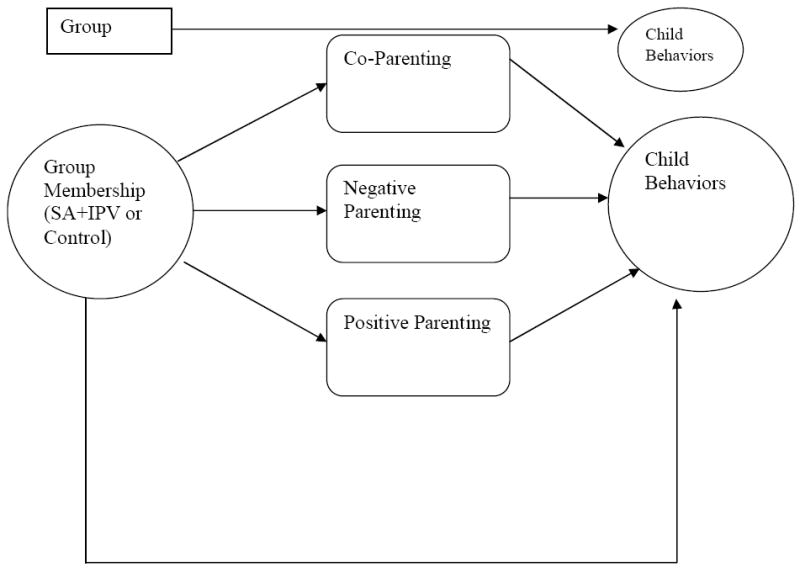
Mediation Models for Child Behaviors
Note: Two models were generated with Child Behaviors measured by 1) DECA Total Problem Behaviors Score and 2) DECA Protective Factors Total Score
Methods
Sample
The study included 86 fathers of children aged two to six years of age, 43 SA + IPV recruited from substance abuse treatment programs and other community settings and 43 fathers living in the same community with no history of alcohol or drug abuse or IPV since the birth of their oldest biological child. SA + IPV fathers: (1) met current DSM-IV criteria for substance abuse of alcohol, cocaine, or marijuana and had used that substance within 30 days based on telephone screening; and (2) reported physical violence in an intimate relationship (pushing, slapping, kicking) within the last 12 months. Community fathers had no evidence of current or past intimate partner violence or substance abuse as reported by the father using standard research questionnaires and verified by the state’s Criminal Justice System’s (CJS) database.
Procedure
Fathers with biological children between the ages of two and six years who either lived with or saw their children for visits at least once per month were recruited via flyers placed in substance abuse or batterer treatment programs, preschools, unemployment offices and community agencies between October 2009 and August 2010. This community based method of recruitment has been shown to be the most effective means of recruiting a representative sample of low-income families for epidemiological studies (Cabral et al., 2003) and has been used in other studies to recruit fathers with substance abuse problems and community comparison fathers (McMahon et al., 2008).
Men were screened by telephone for eligibility and then met in person for a 2 hour session with trained research assistants (RAs) to complete informed consent and study measures, which were read aloud in an interview format. RAs were trained on the meaning of each question and how to rephrase if participants did not understand an item. They offered one or two breaks to participants during the research interview to ensure focus and accurate completion of the measures. If an RA felt there was a concern about data integrity related to an interview or particular question, it was brought to the project director’s attention and a determination was made to exclude those data points from analysis. The focus was on collection of data regarding a biological child aged two to six years. If a father had more than one child in that age range, he was asked to answer the questions related to his oldest child. Participants were paid $50 for their time and the study was approved by the university Human Investigations Committee.
Measures
The Fatherhood and Substance Abuse Structured Research Interview (McMahon, Winkel, Suchman, & Rounsaville, 2007; McMahon et al., 2008) is a structured interview to document a variety of demographic, family and life history variables.
Childhood Trauma Questionnaire-Short Form (CTQ; Bernstein, 1998) is a 28-item measure that was used to asses history of childhood abuse and neglect experienced by the fathers in the study. The CTQ consists of five factors: emotional abuse, emotional neglect, sexual abuse, physical abuse, and physical neglect. The high internal consistency of the CTQ factors has been shown in multiple samples including clinical, community, adult, and adolescent populations. The CTQ has demonstrated excellent convergent and discriminant validity and good sensitivity for all forms of maltreatment (Bernstein, Ahluvalia, Pogge, & Handelsman, 1997; Bernstein, Fink, Handelsman, & Foote, 1994; Bernstein et al., 2003; Scher, Stein, Asmundson, McCreary, & Forde, 2001).
Experiences in Close Relationships Revised (ECR;(Fraley, Waller, & Brennan, 2000) measures how an individual generally feels in romantically close adult relationships. The participant is asked not to respond about their feelings and experiences with their current or most recent partner, but how they feel and respond in general in romantic relationships. Participants respond to each item on a 7-point likert scale. Items are consistent with anxious attachment (e.g. I am afraid I will lose my partner’s love; I worry that romantic partners won’t care about me as much as I care about them) or avoidant attachment behaviors (e.g. I get uncomfortable when a romantic partner wants to be very close; I prefer not to show a partner how I feel deep down) and generate an Anxious and Avoidant Total Score. The ECR-R has excellent test-retest reliability and predictive validity (Sibley, Fischer, & Liu, 2005), good internal consistency and studies support the anxious and avoidant factors of the measure (Fairchild & Finney, 2006; Sibley & Liu, 2004). It has been used in multiple studies of perpetrators of intimate partner violence (Dye & Davis, 2003; Fairchild & Finney, 2006; Goldenson, Geffner, Foster, & Clipson, 2007; Langhinrichsen-Rohling, Palarea, Cohen, & Rohling, 2000) with IPV perpetrators showing greater attachment insecurity on the two factors.
The Brief Symptom Inventory (BSI; (Derogatis, 1975) covers nine symptom dimensions used to identify the presence of psychological symptoms in adults. It generates a global symptom index that captures the severity of psychiatric symptoms endorsed. It yields 3 global severity measures and nine primary symptom dimensions. Test-retest reliability of the BSI subscales range from .71-.80 and several studies have supported its convergent, discriminant and predictive validity in both community and psychiatric samples (Derogatis & Melisaratos, 1983; Kellett, Beail, Newman, & Frankish, 2003).
The Difficulties with Emotional Regulation (DERS; (Gratz & Roemer, 2004) is a self-report questionnaire designed to assess multiple aspects of emotion dysregulation. Participants answer each item based on a 5-point likert scale. The DERS has high internal consistency, good test–retest reliability, and adequate construct and predictive validity (Gratz & Roemer, 2004)
The Revised Conflict Tactics Scale (CTS2; (Straus, Hamby, Boney-McCoy, & Sugarman, 1996) was administered to fathers to obtain a self-report measure of their use of violence in the last year and over the course of the relationship with the mother of their youngest biological child. The CTS2 was used to assess the presence of IPV. The CTS2 is the most widely used measure in the research literature on IPV.
The Parental Acceptance Rejection Questionnaire (PARQ; (Rohner & Khaleque, 2005) is a self-report measure that documents frequency of hostile-aggressive and rejecting parenting behavior. Respondents rate the occurrence of different parenting behaviors along a 4-point scale. Each subscale contains 15-items and has demonstrated good internal consistency and convergent, discriminant, and construct validity (Rohner, Saavedra, & Granum, 1991). It has now been used in multiple studies with fathers who have perpetrated domestic violence and abused substances (McMahon et al., 2008; Stover, McMahon, et al., 2012; Stover, Urdahl, et al., 2012). For this study, fathers were asked to rate the frequency of specific parenting behaviors occurring in their relationship with their oldest biological child between the ages of two and six years.
Parenting Relationship Questionnaire (PRQ; (Kamphaus & Reynolds, 2006) is a self-report measure of parents’ perspectives on the parent-child relationship. It has a preschool version specifically for parents of children aged 2-6 years and generates standardized T-scores. It is a published measure with good internal consistency and convergent validity (Bloomquist, August, Lee, Piehler, & Jensen, 2012; Bloomquist et al., 2009; Wiggins, Sofronoff, & Sanders, 2009). It contains 6 subscales: Attachment, Communication, Discipline Practices, Involvement, Parenting Confidence, and Relational Frustration. High scores indicate positive parenting behaviors.
Parenting Alliance Inventory (Abidin & Brunner, 1995) was used to assess parents’ perceptions of the support they receive from one another and their motivation to communicate with each other about their child. It has been shown to have high internal consistency and good convergent and discriminant validity (Abidin & Brunner, 1995). It has also been used in studies with both mothers and fathers (Abidin & Brunner, 1995; Bearss & Eyberg, 1998; McBride & Rane, 1998)
Devereux Early Childhood Assessment-Clinical (DECA-C; (LeBuffe & Naglieri, 2003) is a standardized assessment tool to assess children aged 2-6 years of age on social and emotional resiliency factors. The DECA-C was standardized with a sample of 2,000 children from 92 preschools and child care centers across the United States. Internal reliability across the various domains ranged from .78 to .94 (LeBuff & Naglieri, 2003). The DECA-C has shown good psychometric properties in large samples of ethnically diverse Head Start preschool samples (Lien & Carlson, 2009). For purposes of these analyses, the Total Problem Behaviors and Protective Factors T-scores were used.
Analytic Strategy
First, data were screened for outlying cases and truncated to within 2.5 standard deviations from the mean which is one of the standard approaches to handling outliers in small datasets (Johnson, Härdle, & Simar, 2002). Next, preliminary chi-square and ANOVAs were conducted to determine if there were significant group differences between the SA+IPV and control group on any demographic variables or mediation variables of interest (e.g. ethnicity, marital status, age of father, age of child, employment status and income). Parenting measures were taken to conceptually measure positive and negative parenting behaviors. In order to reduce the number of dependent parenting variables that would represent positive and negative parenting, principal factor extraction with varimax rotation was performed on the five parenting scores available (the two indices of Rejection and Hostile-Aggression on the PARQ and the three indices of Frustration, Attachment and Involvement on the PRQ) for the sample of 86 fathers with the aim of identifying a negative parenting behavior and positive parenting behavior factor. This ratio is well above the 5:1 item to subject ratio minimum (Gorusch, 1983; Hatcher, 1994).
Bootstrapping using the SPSS macros developed by Preacher and Hayes were used to test for mediation of group differences. Bootstrapping techniques are recommended for testing mediation in smaller samples of 20 to 80 participants as they are the most powerful of the mediation procedures available (Shrout, 2002; Zhang & Wang, 2008). Five thousand resamples were generated in each analysis. Sampling distributions of total and indirect effects are empirically generated by selecting a subsample, with replacement, of the full data set and then calculating indirect effects in the repeated subsamples. In the present study, bootstrap percentile confidence intervals were further improved using bias-correction and acceleration. We fit five models. The first three tested mediation of group differences in (a) co-parenting, (b) negative parenting behaviors, and (c) positive parenting behaviors by (a) anxious attachment problems, (b) avoidant attachment problems (c) affect regulation difficulties, and (d) psychiatric symptoms (see Figure 1). The last two models tested mediation of group differences in child behavior problems and child protective factors by (a) co-parenting, (b) negative parenting behaviors, and (c) positive parenting behaviors (see Figure 2). Parameter estimates with p values less than .05 were considered statistically significant.
Results
Preliminary Analyses
Men in the sample were 18.6% European American, 57% African American, 14% Latino, and 10.5% other or multiethnic. Fathers reported a mean age of 34.69 (SD = 9.19) years with 12.51 (SD = 1.64) years of education. As a group, approximately 38.4% of the men had been legally married at some point, and they had an average of 2.34 (SD = 1.68) children with 1.05 (SD = 0.99) different women. At the time of the study, the target biological child was an average of 3.70 (SD = 1.33) years, and approximately 48.8% of the fathers were living in the same household as that child. Of those fathers who were not living with the target child, their contact with the child ranged from 1 to 30 days per month. Twenty eight percent of non-resident fathers reported seeing their child daily. An additional 24% saw their child 4 or more days per week, 25% saw their child 2 to 3 days per week, 14% once per week and the remaining 7% saw their child 1 to 3 times per month. There were no differences between groups in terms of the amount of contact with the target child. However, men in the SA + IPV group were more likely to report they did not see their child as much as they would like either because their child’s mother would not allow it or there were limits to visitation based on court order (see Table 1).
Table 1.
Means Standard Deviations and Group Comparisons (N=86)
| SA+IPV | Comparison | ||||
|---|---|---|---|---|---|
| Mean(SD)/Percent | Mean (SD) | F | χ2 | Effect Size | |
| Father Age | 34.58(9.93) | 34.79(8.50) | .011 | -- | -.02 |
| Child Age | 3.51(1.22) | 3.98(1.56) | 2.85 | -- | .34 |
| Years of Education | 12.05(1.40) | 12.98(1.74) | 7.48* | -- | -.59 |
| Monthly Income | 1486.25(1343.61) | 1895.10(1947.10) | 1.28 | -- | -.24 |
| Number of times married | 0.35(0.57) | 0.60(0.76) | 3.11 | -- | -.37 |
| Total # women with whom they have children | 1.97(.95) | 1.93(.99) | .048 | -- | .04 |
| Number of biological children | 2.42(1.88) | 2.26(1.47) | .201 | -- | .09 |
| Number of Days Month See Child | 20.50(10.24) | 21.40(9.06) | .186 | -- | -.09 |
| CPS Involvement with child | 50% | 21% | -- | 9.60** | .33 |
| Courts or Mother limit Visits | 22% | 5% | -- | 3.40* | .20 |
| Biological Father had Drug Problem | 30% | 14% | -- | 8.76* | .32 |
| Biological Father IPV | 33% | 14% | -- | 10.67** | .35 |
| Childhood Abuse | 42.84(15.83) | 37.21(16.00) | 2.72 | -- | .35 |
| Attachment Anxiety | 66.00(23.77) | 49.02(21.40) | 11.70** | -- | .75 |
| Attachment Avoidance | 67.02(18.82) | 49.76(16.61) | 19.66*** | -- | .97 |
| BSI Global Symptom Score | 1.73(0.51) | 1.35(0.29) | 17.27*** | -- | .92 |
| Difficulties Emotion Reg. | 98.21(14.38) | 88.88(10.88) | 11.33** | -- | .73 |
Note:
p<.05,
p<.01,
p<.001
BSI=Brief Symptom Inventory
Within the SA+IPV group, 48% of men reported alcohol as their primary drug of choice, 27.6% reported marijuana, 6.3% cocaine, and 3.2% PCP, heroin or poly-substance use. Twenty eight percent of the men who were abusing substances stated they were in treatment. Of those, 73% had been in treatment for a one month or less. Men self-reported a mean of 9.33(SD=11.33) on the physical violence scale of the CTS2 and 88% had been arrested at least once for domestic violence charges. Of those arrested, 86% reported their children were home at the time of police intervention.
Comparison of men with SA + IPV to community controls revealed SA+IPV fathers had significantly less education but no statistical differences in age, income level or employment status. As expected men in the SA + IPV group were significantly more likely than the control group to have been investigated by child protective services and to have been involved in court proceedings related to visitation with their children than the control group. They were also significantly more likely to have biological fathers who abused drugs and perpetrated domestic violence, but they did not report more experiences of childhood abuse and neglect. Groups were not significantly different on any of the other demographic variables of interest (e.g. ethnicity, relationship status, age and gender of child, whether they were living with their child, amount of time spent with the child) (see Table 1).
Next, parenting measures were taken to conceptually measure positive and negative parenting. Principal component analysis with varimax rotation was performed to reduce the 5 parenting outcomes variables. When looking at a one or three factor solution, a two factor solution fit the data best. Communality values were good ranging from .62 for Relational Frustration to .82 for Hostility. With a cutoff of .60 for inclusion of a variable in interpretation of a factor, all 5 variables loaded onto the two factors. Rejection (.88), Hostility-Aggression (.86) and Relational Frustration (.67) made up the negative parenting factor, while Attachment (.80) and Involvement (.78) made up the positive parenting factor. These two weighted factors were the dependent variables in subsequent mediation models.
Group Differences in Parenting Behavior
SA+IPV fathers reported significantly higher psychiatric symptoms on the BSI, more problems with emotion regulation and impulsivity on the DERS, and more difficulties in their adult attachment relationships than the control group (see Table 1). Bivariate correlations displayed in Table 2 indicate moderate correlations among the group of mediating variables (anxious attachment, avoidant attachment, difficulties with emotion regulation and psychiatric symptoms). There were no associations between group status (SA+IPV vs. controls) and whether they were living with or had more frequent contact with the child. Living with the child was not associated with self-reported parenting behaviors or child behavior, but was negatively associated with psychiatric symptoms and attachment avoidance. Fathers with more psychiatric symptoms and greater attachment avoidance were less likely to be living with their children, but there was no association between days of contact per month and any of the variables of interest (see Table 2).
Table 2.
Correlation Matrix of Study Variables (N=86)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Group | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| 2. Attachment Anxiety | .355** | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| 3. Attachment Avoidance | .442** | .436** | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| 4. Difficulties Emotion Regulation | .347** | .425** | .323** | --- | --- | --- | --- | --- | --- | --- | --- |
| 5. BSI Global Symptoms | .417** | .595** | .512** | .533** | --- | --- | --- | --- | --- | --- | --- |
| 6. Positive Parenting | -.370** | -.132 | -.294** | -.008 | -.190 | --- | --- | --- | --- | --- | --- |
| 7. Negative Parenting | .338** | .257* | .392** | .389** | .339** | .000 | --- | --- | --- | --- | --- |
| 8. Co-Parenting Total Score | -.222* | -.434** | -.586** | -.247* | -.429** | .152 | -.432** | --- | --- | --- | --- |
| 9. Child Protective Factors | -.208 | -.302** | -.442** | -.346** | -.364** | .276* | -.207 | .429** | --- | --- | --- |
| 10. Child Behavioral Problems | .314** | .369** | .337** | .214 | .348** | -.095 | .333** | -.186 | -.151 | --- | --- |
| 11. Living with Child | .068 | -.081 | -.229* | -.066 | -.244* | .081 | -.006 | .129 | .100 | -.149 | --- |
| 12. In person contact with child in days per month | -.047 | .040 | -.044 | -.007 | .048 | -.058 | -.185 | .049 | .093 | -.002 | .269* |
p < .05.
p < .01
Note: BSI=Brief Symptom Inventory
The bootstrap results reported in Table 3 indicate that the total effect of SA+IPV group membership on their co- parenting behaviors became non-significant when fathers’ affect regulation, anxious attachment, avoidant attachment and psychiatric symptoms were included as mediators in the model. The four variables fully mediated the association between SA + IPV group and co-parenting behaviors. The specific indirect effects of each proposed mediator showed that difficulties with avoidant attachment in romantic relationships was the only unique mediator; whereas difficulties with emotion regulation, psychiatric symptoms and anxious attachment problems did not add to the overall model.
Table 3.
Summary of mediation analyses
| Independent variable X | Mediating variable M1–Mj | Dependent variable Y | Effect of X on M(a) | Effect of M on Y(b) | Indirect effect (ab) | Lower 95% Conf. | Upper 95% conf. | Direct effect (c′) | Total effect (c) |
|---|---|---|---|---|---|---|---|---|---|
| IPV+ SA Group | Attachment Avoidance | Co-Parenting Conflict | 17.19(3.94)*** | -.37*** | -6.28(2.25)* | -11.80 | -2.71 | 1.79(3.19) | -8.01(3.29)* |
| Attachment Anxiety | 17.68(4.98)*** | .-12 | -2.18(1.58) | -6.34 | .20 | ||||
| Psychiatric Symptoms | .39(.09)*** | -3.91 | -1.52(2.26) | -5.64 | 3.42 | ||||
| Difficulties Affect Regulation | 9.54(2.95)** | .02 | .19(1.60) | -3.56 | 3.01 | ||||
| IPV+ SA Group | Attachment Avoidance | Negative Parenting | 17.19(3.94)*** | .01(.01) | .20(.13)* | .01 | .56 | .23(.23) | .64(.21)** |
| Attachment Anxiety | 17.68(4.98)*** | -.00(.01) | -.01(.09) | -.22 | .17 | ||||
| Psychiatric Symptoms | .39(.09)*** | .10(.31) | .05(.15) | -.30 | .30 | ||||
| Difficulties Affect Regulation | 9.54(2.95)** | .02(.01)* | .18(.14) | -.01 | .65 | ||||
| IPV+ SA Group | Attachment Avoidance | Positive Parenting | 17.19(3.94)*** | .01(.01) | -.16(.14) | -.51 | .07 | -.72(.24)** | -.77(.21)*** |
| Attachment Anxiety | 17.68(4.98)*** | .00(.01) | .03(.13) | -.19 | .33 | ||||
| Psychiatric Symptoms | .39(.09)*** | -.17(.32) | -.07(.16) | -.39 | .22 | ||||
| Difficulties Affect Regulation | 9.54(2.95)** | .01(.01) | .15(.10)* | .02 | .46 | ||||
| IPV+ SA Group | Co-parenting | Child Problem Behaviors | -8.55(.3.54)* | .04(.07) | -.40(.63) | -2.22 | .49 | 2.92(2.09) | 5.06(1.87)** |
| Positive Parenting | -.75(.22)*** | -1.17(.97) | .88(.78) | -.34 | 2.86 | ||||
| Negative Parenting | .61(.22)** | 2.68(1.06)* | 1.65(.83)* | .37 | 3.77 | ||||
| IPV+ SA Group | Co-parenting | Child Protective Factors | -8.55(.3.54)* | .29(.09)** | -2.44(1.26)* | -5.92 | -.65 | -.26(2.82) | -4.83(2.70) |
| Positive Parenting | -.75(.22)*** | 2.42(1.31) | -1.82(1.08)* | -4.44 | -.13 | ||||
| Negative Parenting | .61(.22)** | -.51(1.44) | -.31(.88) | -2.59 | 1.07 |
Note: Significant coefficients:
p < 0.05,
p < 0.01,
p < 0.001;
The coefficients are not standardized values. Values represent parameter estimates with their 95% confidence intervals. The bootstrapped distribution of the parameter estimates was used to derive bias corrected bootstrap confidence intervals. The confidence intervals are not symmetric because they account for the asymmetrical distribution of the parameter estimates. Confidence intervals that do not include 0 were considered statistically significant. Values in parentheses represent standard errors.
The bootstrap results indicated that the total effect of SA+IPV group membership on their negative parenting behaviors became non-significant when the set of four mediators were included in the model. Analyses revealed, with 95% confidence, the four variables fully mediated the association between SA + IPV group and negative parenting behaviors. The specific indirect effects of each proposed mediator showed that attachment avoidance and difficulties with emotion regulation were unique mediators in the model (see Table 3).
Bootstrap results indicated that the total effect of SA+IPV group membership on fathers’ positive parenting behaviors was significant and remained significant when the four mediators were included in the model. Thus the four variables did not mediate the relationship between SA+IPV group and positive parenting behaviors.
Group Differences in Child Behavior
The bootstrap results indicated that the total effect of SA+IPV group membership on children’s problem behaviors became non-significant when fathers’ co-parenting, negative and positive parenting were included as mediators in the model. There was a significant unique mediation for negative parenting, but not positive parenting or co-parenting (see Table 3). The total effect of SA+IPV group membership on children’s positive adjustment behaviors showed a trend but was not significant at the .05 level.
All mediation models tested were also run including whether the child was living with the father as a covariate. The addition of this covariate did not change the relationships or significance of findings in any of the models, so was not presented here.
Discussion
Fathers with co-occurring SA and IPV self-report significantly more negative parenting, less positive parenting behaviors, poorer co-parenting relationships, and more problematic behaviors in their preschool children than community control fathers. This is consistent with other studies reporting more hostile-aggressive parenting of men with histories of IPV (Fox & Benson, 2004) and problematic co-parenting relationships that may be a result of the IPV or involve manipulation of the children (Bancroft & Silverman, 2002; Edleson, Mbilinyi, Beeman, et al., 2003). However, SA + IPV fathers also report significantly more psychiatric symptoms, problems with emotion regulation, and romantic attachment difficulties. These characteristics and symptoms mediate some of the differences between the SA+ IPV fathers and controls.
In particular, an avoidant attachment style in romantic relationships had the strongest association with co-parenting problems and negative parenting behaviors and significantly mediated the association between SA+IPV group membership and negative parenting and co-parenting. The avoidant attachment styles of these fathers are characterized as fearful, with avoidance used as a means of self-protection. These findings are consistent with a body of literature on the association of insecure attachment to IPV and negative parenting (Bartholomew & Allison, 2006; Holtzworth-Monroe & Meehan, 2004; Howard, 2010; Sonkin & Dutton, 2003) and support prior work that indicates for some men with histories of IPV, psychodynamic/attachment focused approaches may be beneficial as a component of their treatment (Saunders, 1996). Men in the SA + IPV group had significant histories of exposure to IPV and substance abuse by their biological fathers, which likely are associated with their attachment difficulties. Whether exploration of these issues in combination with cognitive behavioral skills building, that is an important and typical component of batterer intervention programs (Gondolf, 2012), would result in better treatment outcomes is a question to be answered by future research.
There is currently controversy in the field about the efficacy of interventions for men who perpetrate IPV and a debate about the best approaches to improving court mandated interventions (Gondolf, 2012). The current data point to potential areas of intervention target for a specific subset of men with a history of IPV and co-occurring substance abuse issues who are fathers of young children. Avoidant attachment issues and difficulties with affect regulation are two significant areas of difficulty for these men which greatly impact their parenting. Researchers in the field have suggested a need to tailor intervention to this subpopulation of offenders (Easton et al., 2007; Murphy & Maiuro, 2009; Murphy & Ting, 2010). This subset of men with addiction and IPV issues who are parents may benefit from an approach that incorporates a focus on fathering and attachment relationships (Stover, McMahon, & Easton, 2010). Studies have found that men with histories of IPV are concerned about their children and have a wish to be good fathers (Litton Fox et al., 2001; Mbilinyi et al., 2009; Rothman et al., 2007; Stover, Easton, & McMahon, 2011). This paired with studies indicating motivational interviewing designed to enhance participation in traditional IPV treatment has shown promise (Murphy & Ting, 2010) make consideration of fatherhood status important as a potential motivator for treatment (Mbilinyi et al., 2009; Stover et al., 2010; Stover & Spink, in press).
Behavior problems exhibited by the children of SA+IPV fathers were significantly mediated by the parenting behaviors of their fathers. More negative parenting was associated with more problem behaviors of children. This suggests a need for parenting intervention for fathers to target decreasing negative parenting behaviors. Programs that focus on increasing positive involvement alone without specific focus on hostile and aggressive behaviors are not sufficient. Fathers need to take responsibility for their violent behaviors and denounce violence against women and the impact on children (Bancroft & Silverman, 2002). Some emerging parenting programs include a focus on restorative parenting, which when included as a part of treatment for men with SA+IPV issues may be of benefit (Scott & Crooks, 2007; Stover, in press). A three pronged approach that serves to increase positive parenting and improve the co-parenting relationships while decreasing negative parenting behaviors may yield the most significant treatment outcomes for children.
Limitations and Future Directions
This paper is one of the first to interview fathers with co-occurring substance abuse and IPV directly about their co-parenting, parenting, and behaviors of their children and to compare their responses to those of community control fathers. Still, these findings are based solely on the self-report of a small sample of fathers. Inclusion of collateral information from mothers or direct observation of fathers and children would have added further validity to these findings. Although the measures selected were intended to assess a range of parenting behaviors, they were not designed to assess behaviors specific to the context of IPV such as: whether children were used as a weapon against the other parent, was manipulated or pressured by the father to provide information about the mother, or had their housing, schooling or other basic needs disrupted by their father’s behavior. These kinds of behaviors by fathers would certainly be associated with poor outcomes for children and may significantly impact these findings. Future studies should include measures of these kinds of behaviors and their association to other parenting and child measures. A larger sample with greater variability in severity of IPV and SA and inclusion of fathers with SA without IPV and vice versa would provide a better understanding of the association of IPV with the variables studied and increased power to detect differences. Participants were also at varying stages of addiction treatment as some men responded to advertisements posted in substance abuse treatment clinics. Although most of the SA+IPV men were either not in treatment or just initiating treatment, how substance abuse treatment might impact these findings is unclear. Further exploration of the impact of different substance abuse treatment approaches on parenting of fathers is needed.
Conclusions
Men with SA + IPV had significantly less positive parenting and co-parenting and higher negative parenting behaviors than community control fathers. Negative parenting and co-parenting were mediated by the fathers’ avoidant attachment behaviors. SA + IPV fathers also reported more behavioral problems in their children. These poor child outcome differences between groups were mediated by the negative parenting behaviors of the fathers. Taken together, these results suggest areas of potential intervention target when attempting to work with fathers who have co-occurring SA + IPV issues. Focus on affect regulation and coping with emotions related to their romantic attachment relationships and cognitive behavioral communication skills training related to co-parenting may yield significant changes in parenting behaviors and ultimately child functioning (Kelley & Fals-Stewart, 2002, 2008; Stover, 2009, in press).
References
- Abidin RR, Brunner JF. Development of a parenting alliance inventory. Journal of Clinical Child Psychology. 1995;24(1):31–40. doi: 10.1207/s15374424jccp2401_4. [DOI] [Google Scholar]
- Baker C, Perilla JL, Norris FH. Parenting stress and parenting competence among Latino men who batter. Journal of Interpersonal Violence. 2001;16(11):1139–1157. [Google Scholar]
- Bancroft L, Silverman JG. The batterer as parent: Assessing the impact of domestic violence on family dynamics. Psychology and Law. 2002;9(2):284–285. [Google Scholar]
- Bartholomew K, Allison CJ. An Attachment Perspective on Abusive Dynamics in Intimate Relationships. In: M M, Goodman GS, editors. Dynamics of romantic love: Attachment, caregiving, and sex. New York, NY, US: Guilford Press; 2006. pp. 102–127. [Google Scholar]
- Bearss KE, Eyberg S. A Test of the Parenting Alliance Theory. Early Education & Development. 1998;9(2):179–185. doi: 10.1207/s15566935eed0902_5. [DOI] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an Adolescent Psychiatric Population. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(3):340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Zule W, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Blackson TC, Butler T, Belsky J, Ammerman RT, Shaw DS, Tarter RE. Individual traits and family contexts predict sons’ externalizing behavior and preliminary relative risk ratios for conduct disorder and substance use disorder outcomes. Drug and Alcohol Dependence. 1999;56:115–131. doi: 10.1016/s0376-8716(99)00030-7. [DOI] [PubMed] [Google Scholar]
- Bloomquist M, August G, Lee S, Piehler T, Jensen M. Parent Participation Within Community Center or In-Home Outreach Delivery Models of the Early Risers Conduct Problems Prevention Program. Journal of Child and Family Studies. 2012;21(3):368–383. doi: 10.1007/s10826-011-9488-6. [DOI] [Google Scholar]
- Bloomquist M, Horowitz J, August G, Lee C-Y, Realmuto G, Klimes-Dougan B. Understanding Parent Participation in a Going-to-Scale Implementation Trial of the Early Risers Conduct Problems Prevention Program. Journal of Child and Family Studies. 2009;18(6):710–718. doi: 10.1007/s10826-009-9277-7. [DOI] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Zvolensky MJ. Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Substance Use & Misuse. 2008;43(11):1653–1665. doi: 10.1080/10826080802241292. [DOI] [PubMed] [Google Scholar]
- Cabral DN, Napoles-Springer AM, Miike R, McMillan A, Sison JD, Wrensch MR, Wiencke JK, et al. Population- and Community-based Recruitment of African Americans and Latinos: The San Francisco Bay Area Lung Cancer Study. American Journal of Epidemiology. 2003;158:272–279. doi: 10.1093/aje/kwg138. [DOI] [PubMed] [Google Scholar]
- Cuomo C, Sarchiapone M, Giannantonio MD, Mancini M, Roy A. Aggression, impulsivity, personality traits, and childhood trauma of prisoners with substance abuse and addiction. The American Journal of Drug and Alcohol Abuse. 2008;34(3):339–345. doi: 10.1080/00952990802010884. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Clinical Psychometric Research. Vol. 49. Baltimore, MD: 1975. Brief Symptom Inventory. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13(03):595–605. doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- Dye ML, Davis KE. Stalking and Psychological Abuse: Common Factors and Relationship-Specific Characteristics. Violence and Victims. 2003;18(2):163–180. doi: 10.1891/vivi.2003.18.2.163. [DOI] [PubMed] [Google Scholar]
- Easton C, Swan S, Sinha R. Prevalence of family violence in clients entering substance abuse treatment. Journal of Substance Abuse Treatment. 2000;18:23–28. doi: 10.1016/s0740-5472(99)00019-7. [DOI] [PubMed] [Google Scholar]
- Easton CJ, Mandel DM, Hunkele K, Nich C, Rounsaville BJ, Carroll KM. A cognitive behavioral therapy for alcohol dependent domestic violence offenders: An integrated substance abuse-domestic violence treatment approach (SADV) The American Journal on Addictions. 2007;16:24–31. doi: 10.1080/10550490601077809. [DOI] [PubMed] [Google Scholar]
- Easton CJ, Sacco KA, Neavins TM, Wupperman P, George TP. Neurocognitive Performance Among Alcohol Dependent Men With and Without Physical Violence Toward Their Partners: A Preliminary Report. The American Journal of Drug and Alcohol Abuse. 2008;34(1):29–37. doi: 10.1080/00952990701764326. [DOI] [PubMed] [Google Scholar]
- Edleson JL. Children’s witnessing of adult domestic violence. Journal of Interpersonal Violence. 1999;14:839–970. [Google Scholar]
- Edleson JL. Studying the co-occurence of chid maltreatment and domestic violence. In: Graham-Berman SA, Edleson JL, editors. Domestic violence in the lives of children: The future of research, intervention, and social policy. Washington, DC: American Psychological Association; 2001. pp. 91–110. [Google Scholar]
- Edleson JL, Ellerton AL, Seagren EA, Kirchberg SL, Schmidt SO, Ambrose AT. Assessing child exposure to adult domestic violence. Children and Youth Services Review. 2007;29(7):961–971. doi: 10.1016/j.childyouth.2006.12.009. [DOI] [Google Scholar]
- Edleson JL, Mbilinyi LF, Beeman SK, Hagemeister AK. How Children Are Involved in Adult Domestic Violence. Journal of Interpersonal Violence. 2003;18(1):18–32. doi: 10.1177/0886260502238538. [DOI] [Google Scholar]
- Edleson JL, Mbilinyi LF, Shetty S. Parenting in the context of domestic violence. San Francisco: Judicial Council of California; 2003. [Google Scholar]
- Eiden RD, Chavez F, Leonard KE. Parent-infant interactions among families with alcoholic fathers. Development and Psychopathology. 1999;11:745–762. doi: 10.1017/s0954579499002308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Edwards EP, Leonard KE. Mother-infant and father-infant attachment among alcoholic families. Development and Psychopathology. 2002;14:253–278. doi: 10.1017/s0954579402002043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA. Parental problem drinking and children’s adjustment: Attachment and family functioning as moderators and mediators of risk. Journal of Family Psychology. 2003;17:510–520. doi: 10.1037/0893-3200.17.4.510. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Flanagan E. Parental problem drinking and children’s adjustment: Family conflict and parental depression as mediators and moderators of risk. Journal of Abnormal Child Psychology. 2001;29:417–432. doi: 10.1023/a:1010447503252. [DOI] [PubMed] [Google Scholar]
- Fairchild AJ, Finney SJ. Investigating Validity Evidence for the Experiences in Close Relationships-Revised Questionnaire. Educational and Psychological Measurement. 2006;66(1):116–135. doi: 10.1177/0013164405278564. [DOI] [Google Scholar]
- Fals-Stewart W, Kelley ML, Fincham FD, Golden JC, Logsdan T. The emotional and behavioral problems of children living with drug-abusing fathers: Comparisons of children living with alcohol-abusing and non-substance-abusing fathers. Journal of Family Psychology. 2004;18:319–330. doi: 10.1037/0893-3200.18.2.319. [DOI] [PubMed] [Google Scholar]
- Foran HM, O’Leary KD. Alcohol and intimate partner violence: A meta-analytic review. Clinical Psychology Review. 2008;28:1222–1234. doi: 10.1016/j.cpr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Fox GL, Benson ML. Violent men, bad dads? Fathering profiles of men involved in intimate partner violence. In: Day RD, Lamb ME, editors. Conceptualizing and measuring father involvement. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 359–384. [Google Scholar]
- Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. Journal of Personality and Social Psychology. 2000;78:350–365. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- Goldenson J, Geffner R, Foster SL, Clipson CR. Female Domestic Violence Offenders: Their Attachment Security, Trauma Symptoms, and Personality Organization. Violence and Victims. 2007;22(5):532–545. doi: 10.1891/088667007782312186. [DOI] [PubMed] [Google Scholar]
- Gondolf EW. The Future of Batterer Programs. Boston, MA: Northeastern University Press; 2012. [Google Scholar]
- Gorusch RL. Factor Analysis. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation:Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Hamby S, Finkelhor D, Turner H, Ormrod R. The overlap of witnessing partner violence with child maltreatment and other victimizations in a nationally representative survey of youth. Child Abuse & Neglect. 2010;34(10):734–741. doi: 10.1016/j.chiabu.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Hans SL, Bernstein VJ, Henson LG. The role of psychopathology in the parenting of drug-dependent women. Development and Psychopathology. 1999;11(04):957–977. doi: 10.1017/s0954579499002400. [DOI] [PubMed] [Google Scholar]
- Hatcher L. A Step-by-Step Approach to Using the SAS® System for Factor Analysis and Structural Equation Modeling. Cary, N. C.: SAS Institute Inc; 1994. [Google Scholar]
- Holtzworth-Monroe A, Meehan JC. Typologies of Men Who Are Naritally Violent: Scientific and Clinical Applications. Journal of Interpersonal Violence. 2004;19:1369–1389. doi: 10.1177/0886260504269693. [DOI] [PubMed] [Google Scholar]
- Howard K. Paternal attachment, parenting beliefs and children’s attachment. Early Child Development and Care. 2010;180(1):157–171. [Google Scholar]
- Jacob T, Kahn GL, Leonard K. Parent-child interactions in families with alcoholic fathers. Journal of Consulting and Clinical Psychology. 1991;59:176–181. [PubMed] [Google Scholar]
- Johnson JL, Leff M. Children of substance abusers: Overview of research finding. Pediatrics. 1999;103:1085–1099. [PubMed] [Google Scholar]
- Johnson RA, Härdle W, Simar L. Applied Multivariate Statistical Analysis 2002 [Google Scholar]
- Kamphaus RW, Reynolds CR. Parenting relationship questionnaire manual. Minneapolis, MN: NCS Pearson Inc; 2006. [Google Scholar]
- Kellett S, Beail N, Newman DW, Frankish P. Utility of the Brief Symptom Inventory in the Assessment of Psychological Distress. Journal of Applied Research in Intellectual Disabilities. 2003;16(2):127–134. doi: 10.1046/j.1468-3148.2003.00152.x. [DOI] [Google Scholar]
- Kelley ML, Fals-Stewart W. Couples-versus individual-based therapy for alcohol and drug abuse: Effects on children’s psychosocial functioning. Journal of Consulting and Clinical Psychology. 2002;70:417–427. doi: 10.1037//0022-006x.70.2.417. [DOI] [PubMed] [Google Scholar]
- Kelley ML, Fals-Stewart W. Treating paternal drug abuse using learning sobriety together: Effects on adolescents versus children. Drug and Alcohol Dependence. 2008;92:228–238. doi: 10.1016/j.drugalcdep.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett KA. Health consequences of abuse in the family: A clinical guide for evidence-based practice. Washington, D. C.: American Psychological Association; 2004. [Google Scholar]
- Lamb ME. The role of the father in child development. 4. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- Langhinrichsen-Rohling J, Palarea RE, Cohen J, Rohling ML. Breaking Up is Hard To Do: Unwanted Pursuit Behaviors Following the Dissolution of a Romantic Relationship. Violence and Victims. 2000;15(1):73–90. [PubMed] [Google Scholar]
- LeBuffe PA, Naglieri JA. The Devereux Early Childhood Assessment Clinical Form (DECA-C): A measure of behaviors related to risk and resilience in preschool children. Lewisville, NC: Kaplan Press; 2003. [Google Scholar]
- Lien MT, Carlson JS. Psychometric Properties of the Devereux Early Childhood Assessment in a Head Start Sample. Journal of Psychoeducational Assessment. 2009;27(5):386–396. doi: 10.1177/0734282909331754. [DOI] [Google Scholar]
- Litton Fox G, Sayers J, Bruce C. Beyond bravado: Redemption and rehabilitation in the fathering accounts of men who batter. Marriage & Family Review. 2001;32(3-4):137–163. [Google Scholar]
- Luthar SS, Sexton CC. Maternal drug abuse versus maternal depression: Vulnerability and resilience among school-age and adolescent offspring. Development and Psychopathology. 2007;19(01):205–225. doi: 10.1017/S0954579407070113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsiglio W, Amato P, Day R, Lamb M. Scholarship on the fatherhood in the 1990s and beyond. Journal of Marriage and the Family. 2000;62:1173–1191. [Google Scholar]
- Mbilinyi L, Walker D, Neighbors C, Roffman R, Zegree J, Edleson J. Motivating substance involved perpetrators of intimate partner violence to seek treatment: A focus on fathers. In: Murphy C, Maiuro R, editors. Motivational Interviewing and Stages of Change in Intimate Partner Violence. New York, NY: Springer Publishing; 2009. pp. 181–197. [Google Scholar]
- McBride BA, Rane TR. Parenting Alliance as a Predictor of Father Involvement: An Exploratory Study. Family Relations. 1998;47(3):229–236. [Google Scholar]
- McMahon, Winkel J, Suchman N, Rounsaville B. Drug-abusing fathers: patterns of pair bonding, reproduction, and paternal involvement. Journal of Substance Abuse Treatment. 2007;33:295–302. doi: 10.1016/j.jsat.2006.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon TJ, Winkel JD, Rounsaville BJ. Drug-abuse and responsible fathering: A comparative study of men enrolled in methadone maintenance treatment. Addiction. 2008;103:269–283. doi: 10.1111/j.1360-0443.2007.02075.x. [DOI] [PubMed] [Google Scholar]
- Moore TM, Stuart GL, Meehan JC, Rhatigan D, Hellmuth JC, Keen SM. Drug abuse and aggression between intimate partners: A meta-analytic review. Clinical Psychology Review. 2008;28:247–274. doi: 10.1016/j.cpr.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Murphy C, Maiuro RD, editors. Motvational Interviewing and Stages of Change in Intimate Partner Violence. New York, NY: Springer Publishing; 2009. [Google Scholar]
- Murphy CM, Ting LA. Interventions for Perpetrators of Intimate Partner Violence: A Review of Efficacy Research and Recent Trends. Partner Abuse. 2010;1(1):26–44. doi: 10.1891/1946-6560.1.1.26. [DOI] [Google Scholar]
- NIMH. Men and depression: National Institue of Mental Health 2003 [Google Scholar]
- Peled E, Jaffe PG, Edleson JL. Ending the cycle of violence: Community responses to children of battered women. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- Perry JL, Carroll ME. The role of impulsive behavior in drug abuse. Psychopharmacology. 2008;200(1):1–26. doi: 10.1007/s00213-008-1173-0. [DOI] [PubMed] [Google Scholar]
- Pruett K. Infants of primary nurturing fathers. Psychoanalytic Study of the Child. 1983;38:257–281. doi: 10.1080/00797308.1983.11823392. [DOI] [PubMed] [Google Scholar]
- Roberts JC, Wolfer L, Mele M. Why Victims of Intimate Partner Violence Withdraw Protection Orders. Journal of Family Violence. 2008;23:369–375. doi: 10.1007/s10896-008-9161-z. [DOI] [Google Scholar]
- Rohner RP, Khaleque A. Handbook for the study of parental acceptance and rejection. 4. Storrs, CT: Rohner Research Publications; 2005. [Google Scholar]
- Rohner RP, Saavedra JM, Granum EO. Handbook for the Study of Parental Acceptance and Rejection. Storrs, CT: Center for the Study of Acceptance and Rejection; 1991. Parental acceptance-rejection questionnaire: Test manual; pp. 17–48. [Google Scholar]
- Rothman E, Mandel DG, Silverman JG. Abuser’s perceptions of the effect of their intimate partner violence on children. Violence Against Women. 2007;13:1179–1191. doi: 10.1177/1077801207308260. [DOI] [PubMed] [Google Scholar]
- Saunders D. Feminist-Cognitive-Behavioral and Process-Psychodynamic Treatment for Men Who Batter: Interaction of abuser traits and treatment models. Violence and Victims. 1996;11(4):393–414. [PubMed] [Google Scholar]
- Scher CD, Stein MB, Asmundson GJG, McCreary DR, Forde DR. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal of Traumatic Stress. 2001;14:843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Scott KL, Crooks CV. Preliminary evaluation of an intervention program for maltreating fathers. Brief Treatment and Crisis Intervention. 2007;7(3):224–238. [Google Scholar]
- Scott S, Babcock JC. Attachment as a Moderator Between Intimate Partner Violence and PTSD Symptoms. Journal of Family Violence. 2010;25:1–9. doi: 10.1007/s10896-009-9264-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological methods. 2002;7(4):422. [PubMed] [Google Scholar]
- Sibley CG, Fischer R, Liu JH. Reliability and Validity of the Revised Experiences in Close Relationships (ECR-R) Self-Report Measure of Adult Romantic Attachment. Personality and Social Psychology Bulletin. 2005;31(11):1524–1536. doi: 10.1177/0146167205276865. [DOI] [PubMed] [Google Scholar]
- Sibley CG, Liu JH. Short-term temporal stability and factor structure of the revised experiences in close relationships (ECR-R) measure of adult attachment. Personality and Individual Differences. 2004;36(4):969–975. doi: 10.1016/s0191-8869(03)00165-x. [DOI] [Google Scholar]
- Sonkin DJ, Dutton D. Treating Assaultive Men from an Attachment Perspective. Journal of Aggression, Maltreatment & Trauma. 2003;7(1-2):105–133. doi: 10.1300/J146v07n01_06. [DOI] [Google Scholar]
- Stover C, McMahon TJ, Easton C. The impact of fatherhood on treatment response for men with co-occurring alcohol dependence and intimate partner violence. The American Journal of Drug and Alcohol Abuse. 2010;0(0):1–5. doi: 10.3109/00952990.2010.535585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stover CS. Integrated father treatment for domestic violence; Paper presented at the National Summitt on the Intersection of Domestic Violence and Child Maltreatment; Jackson Hole, WY. 2009. [Google Scholar]
- Stover CS. Fathers for Change: A new approach to working with father with histories of intimate parnter violence and substance abuse. Journal of the American Academy of Psychiatry and the Law. in press. [PMC free article] [PubMed] [Google Scholar]
- Stover CS, McMahon TJ, Easton CJ. Fathers entering substance abuse treatment: An examination of substance abuse, trauma symptoms and parenting behaviors. Journal of Substance Abuse Treatment. 2012 doi: 10.1016/j.jsat.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stover CS, Spink A. Affective awareness in parenting of fathers with co-occurring substance abuse and intimate partner violence. Journal of Advances in Dual Diagnosis. doi: 10.1108/17570971211241903. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stover CS, Urdahl A, Easton CJ. Depression as a Mediator of the Association Between Substance Abuse and Negative. American Journal of Drug and Alcohol Abuse. 2012 doi: 10.3109/00952990.2011.649221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Stuart GL, Moore TM, Kahler CW, Ramsey SE. Substance Abuse and Relationship Violence Among Men Court-Referred to Batterers’ Intervention Programs. Substance Abuse. 2003;24(2):107–122. doi: 10.1023/a:1023736732766. [DOI] [PubMed] [Google Scholar]
- West MO, Prinz RJ. Parental alcoholism and childhood psychopathology. Psychological Bulletin. 1987;102:204–218. [PubMed] [Google Scholar]
- Wiggins TL, Sofronoff K, Sanders MR. Pathways Triple P-Positive Parenting Program: Effects on Parent-Child Relationships and Child Behavior Problems. Family Process. 2009;48(4):517–530. doi: 10.1111/j.1545-5300.2009.01299.x. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Wang L. Methods of evaluating mediation effects: Rationale and comparison. In: Shigemasu K, Okada A, Imaizumi T, Hosino T, editors. New Trends in Psychometrics. Tokyo: Universal Academy Press; 2008. pp. 595–604. [Google Scholar]


