Abstract
After over one decade development, cone beam computed tomography (CBCT) has been widely accepted for clinical application in almost every field of dentistry. Meanwhile, the radiation dose of CBCT to patient has also caused broad concern. According to the literature, the effective radiation doses of CBCTs in nowadays market fall into a considerably wide range that is from 19 µSv to 1073 µSv and closely related to the imaging detector, field of view, and voxel sizes used for scanning. To deeply understand the potential risk from CBCT, this report also reviewed the effective doses from literatures on intra-oral radiograph, panoramic radiograph, lateral and posteroanterior cephalometric radiograph, multi-slice CT, and so on. The protection effect of thyroid collar and leaded glasses were also reviewed.
Keywords: Radiation Dosage; Cone-Beam Computed Tomography; Tomography, Spiral Computed; Radiation Protection
Cone-beam computed tomography (CBCT) has been widely used in dental cilincs for over ten years. While the benefits of CBCT examination have been reported widely, the radiation dose to the patient is also becoming a major concern. In 2010, an article entitled "Radiation worries for children in dentist's chair" was published in The New York Times newspaper. It was the first time a major newspaper brought the radiation dosage of CBCT to the attention of the public.
Then, one may ask: What radiation dose is received by a patient who undergoes a CBCT examination? How high is the radiation dose compared with those obtained with conventional dental radiography and a helical CT examination? Are there methods for reducing the radiation dose without affecting the image quality? Answering these questions requires information on how a radiation dose is measured. Thus, this report includes the following three components: 1) measurement of radiation dosage; 2) comparison of patient radiation dose among CBCT, helical CT, and conventional dental radiography; and 3) patient protection from CBCT radiation.
Measurement of radiation dose
There are three basic concepts associated with the radiation dose: the absorbed dose, equivalent dose, and effective dose. The absorbed dose is used to describe the amount of X-ray energy absorbed by a unit mass (total weight) of tissue. The SI unit is the Gray (Gy). The equivalent dose is used to compare the biologic effect of different types of radiation on tissue or an organ. The SI unit is Sievert (Sv). For a diagnostic X-ray examination, the abosorbed dose is equal to the equivalent dose, that is, 1 Gray equals 1 Sievert. For the estimation of radiation risk, which is the possibility of biological consequences after radiation exposure to human beings, the concept of effective dose is used. The effective dose is a measurement of the degree of harmful effects on the human body of one kind of radiation. The SI unit for the effective dose is the Sievert, but in practice, milli- or micro-Sievert is often used.
To determine the effective dose, a direct method is the use of an anthropomorphic phantom (Fig. 1). The phantom can be made with a real human skull covered with soft tissue-equivalent materials or only made with bone- and soft tissue-equivalent materials. The phantom usually comprises nine sections and in each section there are holes in the places where the tissues are being measured. Thermoluminescent dosimeters (TLDs), optically stimulated luminescent dosimeters (OSLs), or radiophotoluminescence glass dosimeters can be positioned in the holes for the measurement of the absorbed dose of the corresponding tissue. The tissues measured can include the bone marrow, thyroid gland, esophagus, salivary glands, skin, bone surface, brain, pituitary, and eyes, and in most studies,1-14 TLDs are used for the mesasurement of the radiation dose (Fig. 2).
Fig. 1.
The image of one anthropomorphic phantom.
Fig. 2.
The example image of thermoluminescent dosimeters (TLDs).
It is worth noticing that at this stage only the absorbed dose is measured. In order to determine the effective dose, which is used to estimate the risk in human beings, the absorbed dose for individual organs must be translated to an equivelant dose and then multiplied with a weighting factor defined by the International Commission on Radiological Protection (ICRP) for the specific organ. Later, the effective doses of these organs are summed up to obtain a total effective dose. The total dose is used to represent the potential risk of the whole body exposed to radiation. The effective dose is a calculated value rather than a directly measured value.
Comparison of patient radiation dose among CBCT, helical CT, and conventional dental radiograpahy
We have thus shown that the effective dose is a representation of the potential risk of radiation dose to the patient, and in most studies, the effective dose is drived from absorbed dose, which is measured with TLDs by the use of an anthropomorphic phantom. Thus, in the following discussion, only the reported effective dose derived from a phantom is addressed.
Effective doses obtained with different CBCT units
Many studies have been performed to estimate the effective doses of different CBCT units. However, a simple comparison cannot be made since, as one researcher has noted, "significant differences in dose for the same examination have been reported for different CBCT units, and significant differences in dose have been reported for different examinations or techniques with the same unit"13 and another has observed that "the results are often difficult to compare when a number of different phantoms and dosimeters have been used together with different assumptions."15
To avoid these research limitations, Ludlow et al5 and Pauwels et al14 investigated the effective dose of 8 and 14 CBCT units, respectively, by using the same phantom and TLD dosimeters. The results from the two studies are summarized in Table 1.
Table 1.
Effective doses from different CBCT units
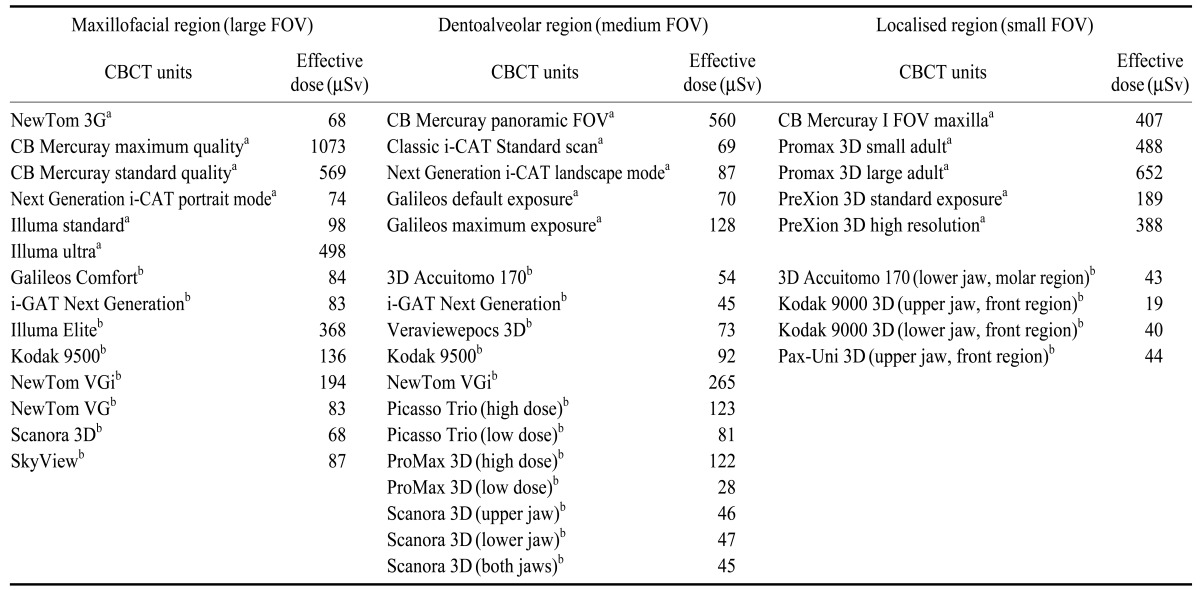
aData from the study by Ludlow et al (2008), bData from the study by Pauwels et al (2012)
Although the phantoms and dosimeters employed in the two studies were different, from Table 1 we can still see that the effective dose is quite different from one CBCT unit to another, irrespective of the size of the field of view (FOV) used. The highest effective dose is 1073 µSv for CB MercuRay with a large FOV scanning for maxillofacial region, while the lowest effective dose is only 19 µSv for the Kodak 9000 3D with a scanning area of the front region of the upper jaw. This is a difference of almost 500 times between the highest and lowest effective doses.
When we look futher into the data in Table 1, we can see that the effective dose is closely related to the protocol used for scanning. Since a protocol is a combination of kVp, mAs, and voxel sizes and other factors, the effective dose is in reality closely related to the chosen exposure parameters. In the study performed by Ludlow et al, the effective dose for maximum quality CB MercuRay (1073 µSv) is almost twice that of standard quality CB MercuRay (569 µSv), the effective dose for CBCT unit Galileos obtained at the default exposure (70 µSv) is almost half of that obtained at maximum exposure (128 µSv), and the effective dose for standard and high resolution images from the PreXion 3D were 189 µSv and 388 µSv, respectively. The later data also indicate that with an increase in the spatial resolution, the effective dose is increased as well. This is also confirmed by the study conducted by Davies et al.16
Field of view (FOV) is another factor that plays an important role in the assessment of the effective dose of one CBCT examination. When the exposure parameters such as the kVp and mAs are maintained at the same level, the larger the FOV used, the higher the effective dose obtained. This is substantiated by the effective doses for CB Mercuay in Table 1, where the effective dose is 1073 µSv for a large FOV with maximum quality, 560 µSv for a medium FOV, and 407 µSv for a small FOV. The exposure parameters for all of the three FOV examinations were kept at 120 kVp and 150 mAs. A study by Qu et al13 further discloses the positive relationship between the FOV and effective dose. In this study, 12 protocols that combined different patient size, FOV, kVp, mA, and exposure times were employed for the estimation of effective doses of the ProMax 3D CBCT unit. While holding all of the other exposure parameters constant, the researchers found that for a scanning area of full volume height with a full volume diameter (8 cm×8 cm), the effective dose (298 µSv) is much higher than the effective doses obtained from used other scanning FOVs, specifically, half the volume height (upper jaw) with a full volume diameter (4 cm×8 cm, 131 µSv), half the volume height (lower jaw) with a full volume diameter (4 cm×8 cm, 171 µSv), a full volume height with half the volume diameter (anterior region, 8 cm×4 cm, 127 µSv), and a full volume height with half the volume diameter (posterior region, 8 cm×4 cm, 197 µSv).
The above demonstrates that the effective dose is different from one CBCT unit to another and closely related to the exposure parameters used for scanning; for a given model of a CBCT unit, the larger the FOV used for scannning, the higher the effective dose derived when all the other exposure parameters are kept at the same level. Similarly, the higher the spatial resolution chosen for scanning, the higher the effective dose is.
Effective dose of CBCT and conventional dental radiography
There are few studies focusing on the direct comparison of the effective doses obtained from CBCT and conventional dental radiography. The results from the direct comparison studies were summarized in Table 2, where the effective dose for panoramic radiography is about 22.0 µSv, for lateral cephalometric examination about 4.5 µSv and for CBCT examnation the effective dose is 61-134 µSv. No study has performed a direct comparison of the effective dose from intraoral and CBCT examinations. In the guidelines19 provided by the European Academy of Dento-Maxillofacial Radiology, the suggested effective dose of one intraoral radiograph is 1.5 µSv. Other studies20-26 that exclusively estimated the effective dose of conventional dental radiography have demonstrated that the range of the effective dose for a panoramic radiograph is 3.85-38.0 µSv (Table 3), for a lateral cephalometric examination is 1.1-5.6 µSv (Table 4), for posteroanterior cephalometric radiograph, 5.1µSv, and for one introal examination, 0.65-9.5 µSv (Table 5).
Table 2.
Comparison of effective dose (µSv) of CBCT, panoramic and later cephalometric (ceph.) radiography
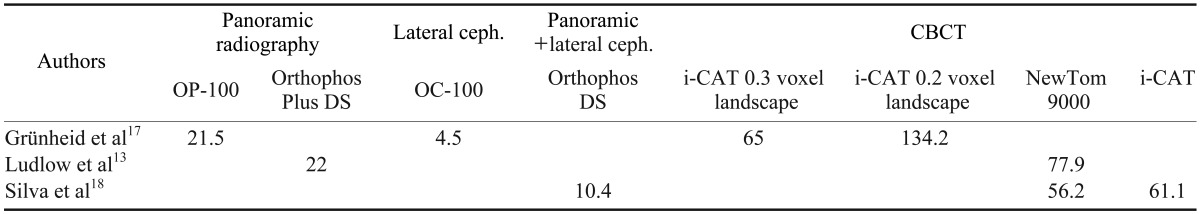
Table 3.
Effective doses from panoramic radiography
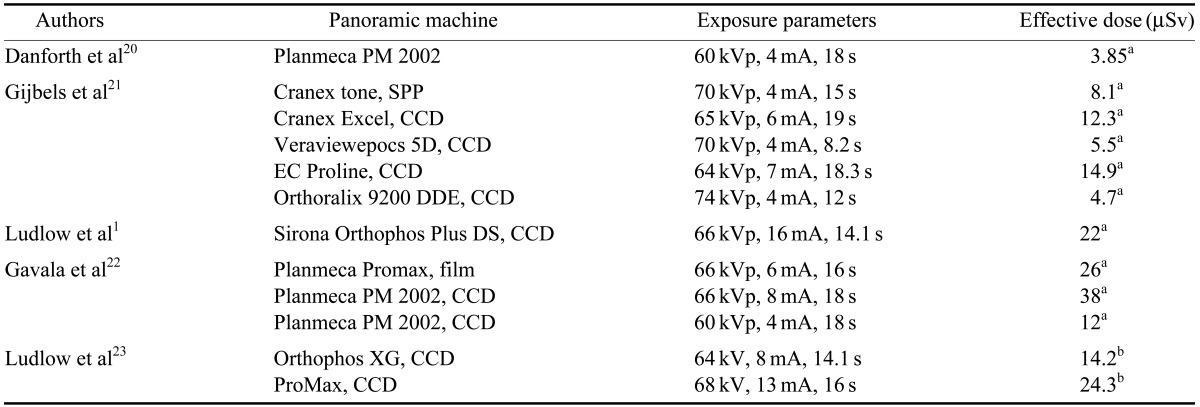
a: ICRP60 1990, b: ICRP103 2007, CCD: charge-coupled device, SPP: storage phosphor plate
Table 4.
Effective doses from lateral cephalometric radiography
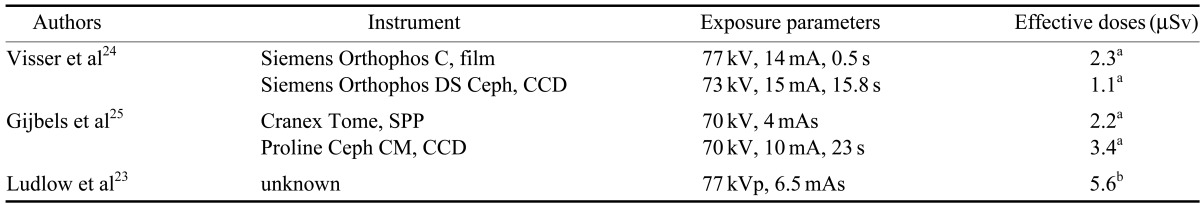
a: ICRP60 1990, b: ICRP103 2007, CCD: charge-coupled device, SPP: storage phosphor plate
Table 5.
Effective doses from intra-oral examinations
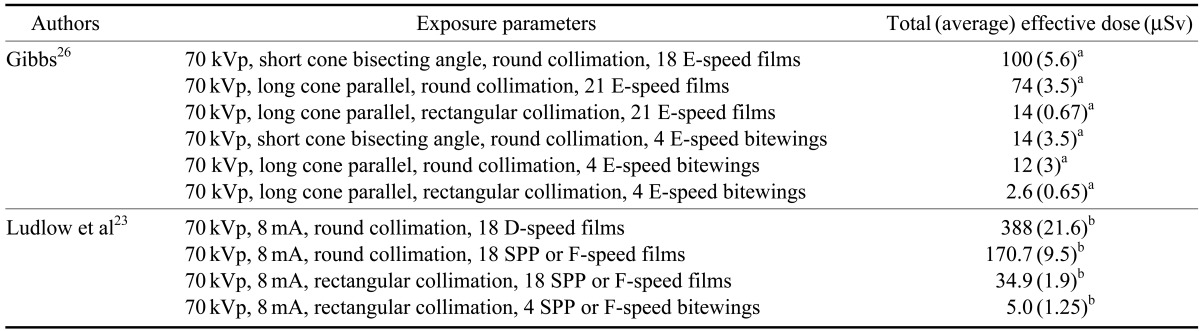
a: ICRP60 1990, b: ICRP103 2007, SPP: storage phosphor plate
These data indicate that the effective dose of CBCT is several to hundreds of times higher than the effective dose from a conventional dental radiographic examination.
Effective dose of CBCT and helical CT
More attention is paid to the effective dose of CBCT and multislice CT (MSCT) since both techniques provide three dimensional images. The effective doses from the literature on CBCT and MSCT are shown in Table 6. Generally, the effective dose of MSCT is much higher than that of CBCT. However, in some of the studies, the scanning area, i.e. the FOV was not well defined. To avoid the effect of the FOV on the assessment of effective dose, Qu et al13 strictly defined the scanning area for both MSCT and CBCT examinations in their study. The results showed that the effective doses of MSCTs are about several to ten times higher than those of CBCTs. For example, when scaning both the maxilla and mandible, the effective dose is about 94.9 µSv for CBCT NewTom 9000, 249.1 µSv for CBCT DCT-Pro, and 1066.1 for GE 8-slice MSCT. Similar results were also observerd in other studies, as shown in Table 6.
Table 6.
Effective dose (µSv) of CBCT and MSCT from literatures
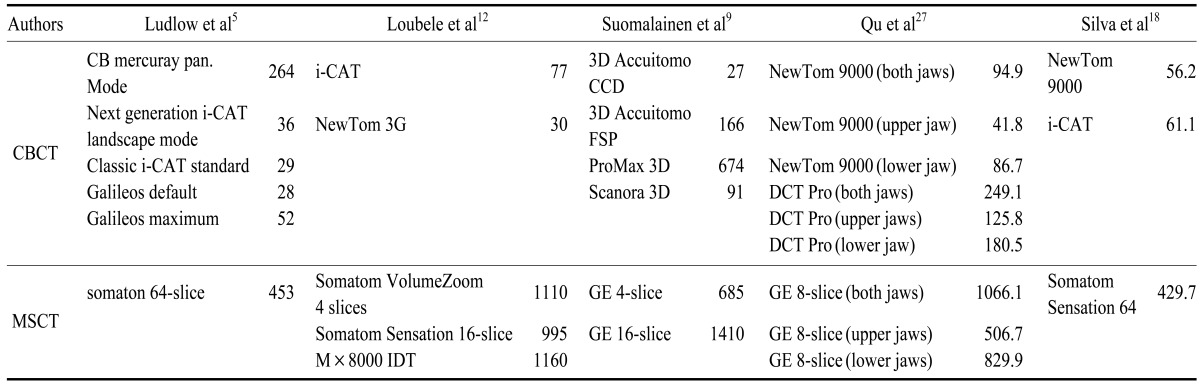
MSCT: multi-slice CT
However, it should be borne in mind that although the effective dose of MSCT is much higher than that of CBCT, the image qualities for the two techniques are quite different. For hard tissue, such as bone and tooth, the image quality of CBCT is equal to or better than the image quality of MSCT, but for soft tissues, the image from CBCT is not satisfactory due to the inherent drawbacks of the technique.
Patient radiation protection from CBCT
To perform one medical X-ray examination, three main factors must be taken into account: the X-ray unit, patient for examination, and receptor used for capturing the image of the patient. Therefore, when an X-ray examination is indicated for a patient, the patient dose can be reduced by the reduction of the X-ray intensity emitted from the employed x-ray unit, increasing of the imaging receptor capturing speed and collimation, or shielding of the x-ray beam to the patient. This section will only focus on the shielding devices for the reduction of the radiation dose.
The shielding devices include a leaded thyroid collar for the protection of the thyroid gland, leaded glasses for the protection of the eye lens, a leaded hat for the protection of the brain, and a leaded apron for the protection of the body trunk. It is well known that a thyroid collar is effective for the protection of the thyroid gland in an intraoral examination. However, for a CBCT examination, is it still effective when the X-ray unit rotates around the patient?
With this question in mind, two studies were conducted. One study was mainly aimed to identify the effectiveness of a thyroid collar on the dose redution of the thyroid gland.28 In this study, five conditions were tested as follows: 1) without a collar around the neck; 2) with one collar loosely on the front of the neck; 3) with two collars loosely on the front and back of the neck; 4) with one collar tightly on the front of the neck; and 5) with two collars tightly on the front and back of the neck. The results showed that when the thyroid collars were used loosely around the neck, no effective organ dose reduction was observed. When one thyroid collar was used tightly on the frontof the neck, the effective organ dose to the thyroid gland and esophagus were reduced to 15.9 µSv (48.7% reduction) and 1.4 µSv (41.7% reduction), respectively. A similar organ dose reduction (46.5% and 41.7%) was achieved when CBCT scanning was performed with two collars tightly affixed to the front and back of the neck. The study supported the use of a thyroid collar during a CBCT scan. In a subsequent study, different oral and maxillofacial regions were scanned with the phantom tightly wearing one or two thyroid collars.29 The results also supported the use of thyroid collars (61% thyroid dose reduction for a large view examination, 72% thyroid dose reduction for a medium FOV, and 70% thyroid dose reduction for a small FOV) and further disclosed that the total effective dose for medium and small FOV examinations were also significantly reduced by the use of a thyroid collar.
The use of leaded glasses during a CBCT examinaiton was also investigated.30 In the study peformed by Prins et al, three phantoms representing an adult male, an adult female, and a child were employed. The results showed that the radiation dose to the eye lens could be reduced by over 60% without having a deleterious effect on the image quality in the area of clinical significance for dental imaging.
Considering the above, one conclusion that could be drawn was that a thyroid collar and leaded glasses should be used during a CBCT examination, given that diagnostic information and image quality are not reduced.
Summary
The effective dose of CBCT, conventional dental radiography, and multislice CT and the effect of a thyroid collar and leaded glasses on the dose reduction was presented in this paper. Based on the above analysis, we can conclude the following:
The patient radiation dose is much lower for CBCT than for helical CT;
The patient radiation dose is closely related to the FOV and exposure parameters used for a CBCT examination. Without alteration of any other exposure parameters, the larger the FOV used for scanning, the higher the radiation dose is;
Compared with conventional dental radiography, the effective dose of CBCT is several to hundreds of times higher;
To reduce the patient dose to the greatest possible extent, the chosen CBCT scanning protocol should be in accordance with the dignostic task at hand;
A thyroid collar should be used for CBCT scanning; wearing leaded glasses is recommended when it does not detract from imaging quality.
References
- 1.Ludlow JB, Davies-Ludlow LE, Brooks SL. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol. 2003;32:229–234. doi: 10.1259/dmfr/26310390. [DOI] [PubMed] [Google Scholar]
- 2.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol. 2004;33:83–86. doi: 10.1259/dmfr/28403350. [DOI] [PubMed] [Google Scholar]
- 3.Tsiklakis K, Donta C, Gavala S, Karayianni K, Kamenopoulou V, Hourdakis CJ. Dose reduction in maxillofacial imaging using low dose Cone Beam CT. Eur J Radiol. 2005;56:413–417. doi: 10.1016/j.ejrad.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 4.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226. doi: 10.1259/dmfr/14340323. [DOI] [PubMed] [Google Scholar]
- 5.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:106–114. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 6.Palomo JM, Rao PS, Hans MG. Influence of CBCT exposure conditions on radiation dose. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:773–782. doi: 10.1016/j.tripleo.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 7.Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Grondahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol. 2008;37:72–79. doi: 10.1259/dmfr/60375385. [DOI] [PubMed] [Google Scholar]
- 8.Hirsch E, Wolf U, Heinicke F, Silva MA. Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. Dentomaxillofac Radiol. 2008;37:268–273. doi: 10.1259/dmfr/23424132. [DOI] [PubMed] [Google Scholar]
- 9.Suomalainen A, Kiljunen T, Kaser Y, Peltola J, Kortesniemi M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac Radiol. 2009;38:367–378. doi: 10.1259/dmfr/15779208. [DOI] [PubMed] [Google Scholar]
- 10.Chau AC, Fung K. Comparison of radiation dose for implant imaging using conventional spiral tomography, computed tomography, and cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:559–565. doi: 10.1016/j.tripleo.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol. 2009;82:35–40. doi: 10.1259/bjr/31419627. [DOI] [PubMed] [Google Scholar]
- 12.Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009;71:461–468. doi: 10.1016/j.ejrad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Qu XM, Li G, Ludlow JB, Zhang ZY, Ma XC. Effective radiation dose of ProMax 3D cone-beam computerized tomography scanner with different dental protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:770–776. doi: 10.1016/j.tripleo.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 2012;81:267–271. doi: 10.1016/j.ejrad.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 15.Thilander-Klang A, Helmrot E. Methods of determining the effective in dental radiology. Radiat Prot Dosimetry. 2010;139:306–309. doi: 10.1093/rpd/ncq081. [DOI] [PubMed] [Google Scholar]
- 16.Davies J, Johnson B, Drage NA. Effective doses from cone beam CT investigation of the jaws. Dentomaxillofac Radiol. 2012;41:30–36. doi: 10.1259/dmfr/30177908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grünheid T, Kolbeck Schieck JR, Pliska BT, Ahmad M, Larson BE. Dosimetry of a cone-beam computed tomography machine compared with a digital x-ray machine in orthodontic imaging. Am J Orthod Dentofacial Orthop. 2012;141:436–443. doi: 10.1016/j.ajodo.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 18.Silva MA, Wolf U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone-beam computed tomography for routine orthodontic treatment planning: a radiation dose evaluation. Am J Orthod Dentofacial Orthop. 2008;133:640.e1–640.e5. doi: 10.1016/j.ajodo.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 19.SEDENTEXCT Guideline Development Panel. Radiation protection No 172. Cone beam CT for dental and maxillofacial radiology. Evidence based guidelines. Luxembourg: European Comminssion Directorate-General for Energy; 2012. [Google Scholar]
- 20.Danforth RA, Clark DE. Effective dose from radiation absorbed during a panoramic examination with a new generation machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:236–243. doi: 10.1067/moe.2000.103526. [DOI] [PubMed] [Google Scholar]
- 21.Gijbels F, Jacobs R, Bogaerts R, Debaveye D, Verlinden S, Sanderink G. Dosimetry of digital panoramic imaging. Part I: Patient exposure. Dentomaxillofac Radiol. 2005;34:145–149. doi: 10.1259/dmfr/28107460. [DOI] [PubMed] [Google Scholar]
- 22.Gavala S, Donta C, Tsiklakis K, Boziari A, Kamenopoulou V, Stamatakis HC. Radiation dose reduction in direct digital panoramic radiography. Eur J Radiol. 2009;71:42–48. doi: 10.1016/j.ejrad.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. J Am Dent Assoc. 2008;139:1237–1243. doi: 10.14219/jada.archive.2008.0339. [DOI] [PubMed] [Google Scholar]
- 24.Visser H, Rödig T, Hermann KP. Dose reduction by direct-digital cephalometric radiography. Angle Orthod. 2001;71:159–163. doi: 10.1043/0003-3219(2001)071<0159:DRBDDC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Gijbels F, Sanderink G, Wyatt J, Van Dam J, Nowak B, Jacobs R. Radiation doses of indirect and direct digital cephalometric radiography. Br Dent J. 2004;197:149–152. doi: 10.1038/sj.bdj.4811532. [DOI] [PubMed] [Google Scholar]
- 26.Gibbs SJ. Effective dose equivalent and effective dose: comparison for common projections in oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:538–545. doi: 10.1067/moe.2000.109189. [DOI] [PubMed] [Google Scholar]
- 27.Qu XM, Li G, Zhang ZY, Ma XC. Comparative dosimetry of dental cone-beam computed tomography and multi-slice computed tomography for oral and maxillofacial radiology. Zhonghua Kou Qiang Yi Xue Za Zhi. 2011;46:595–599. [PubMed] [Google Scholar]
- 28.Qu XM, Li G, Sanderink GC, Zhang ZY, Ma XC. Dose reduction of cone beam CT scanning for the entire oral and maxillofacial regions with thyroid collars. Dentomaxillofac Radiol. 2012;41:373–378. doi: 10.1259/dmfr/30200901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qu X, Li G, Zhang Z, Ma X. Thyroid shields for radiation dose reduction during cone beam computed tomography scanning for different oral and maxillofacial regions. Eur J Radiol. 2012;81:e376–e380. doi: 10.1016/j.ejrad.2011.11.048. [DOI] [PubMed] [Google Scholar]
- 30.Prins R, Dauer LT, Colosi DC, Quinn B, Kleiman NJ, Bohle GC, et al. Significant reduction in dental cone beam computed tomography (CBCT) eye dose through the use of leaded glasses. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:502–507. doi: 10.1016/j.tripleo.2011.04.041. [DOI] [PubMed] [Google Scholar]



