Abstract
The natural history of Pott’s kyphosis is different from that of other spinal deformities. After healing of the spinal infection, the post-tubercular kyphosis in adults is static but in children variable progression of the kyphosis is seen. The changes occurring in the spine of children, after the healing of the tubercular lesion, are more significant than the changes that occur during the active stage of infection. During growth, there is a decrease in deformity in 44 % of the children, an increase in deformity in 39 % of the children and no change in deformity in 17 % of the children. The critical factor leading to the progress of the deformity is dislocation of the facets. This can be identified on radiographs by the “Spine-at-risk” signs. Dislocation of facets at more than two levels can lead to the “Buckling collapse” of the spine, which is characteristically seen only in severe tubercular kyphosis in children. Age below 10 years, vertebral body loss of more than 1–1.5 pre-treatment deformity angle of greater than 30° and involvement of cervicothoracic or thoracolumbar junction are the other risk factors for deformity progression. In children, the kyphosis can progress even after healing of the spinal infection and hence children with spinal tuberculosis must be followed-up till skeletal maturity.
Keywords: Pott’s spine, Kyphosis, Natural history
Introduction
More than 30 million people are suffering worldwide from overt tuberculosis and more than 2 million of them have the active, spinal form [1]. The discovery of effective antituberculous chemotherapy has largely made uncomplicated spinal tuberculosis a medical disease [2–5]. The Medical Research Council (MRC) trials have shown that ‘favorable status’ (defined as no clinically apparent abscess or sinus, radiologically quiescent, no residual neurological impairment with no impairment of physical activity due to spinal disease) achieved by conservative therapy is similar to that achieved by radical surgery and the status is maintained even at 10-year follow-up [2, 6]. The challenges facing the spinal surgeon nowadays in the management of spinal tuberculosis are the problems of progressive deformity [7] and correction of residual severe deformity [4, 5, 8].
Spinal tuberculosis is the most common cause of a kyphotic spinal deformity in most parts of the world. Although complete cure may be achieved with chemotherapy, patients with spinal tuberculosis treated conservatively have an average increase of 15° in deformity [6, 7] and 3–5 % of the patients develop with a deformity greater than 60° [4, 5, 8]. A severe kyphosis leads to immense cosmetic and psychological disturbance in a growing child and can also result in costo-pelvic impingement, secondary cardiorespiratory problems and late-onset paraplegia [8]. Kyphotic deformities also, more commonly than scoliosis, cause cardio respiratory failure. Correction of an established spinal deformity is both difficult and hazardous with a high rate of complications, even in experienced hands [9]. Hence, prevention of deformity must be an essential aspect of any treatment schedule in spinal tuberculosis [8].
Natural history of progress of deformity
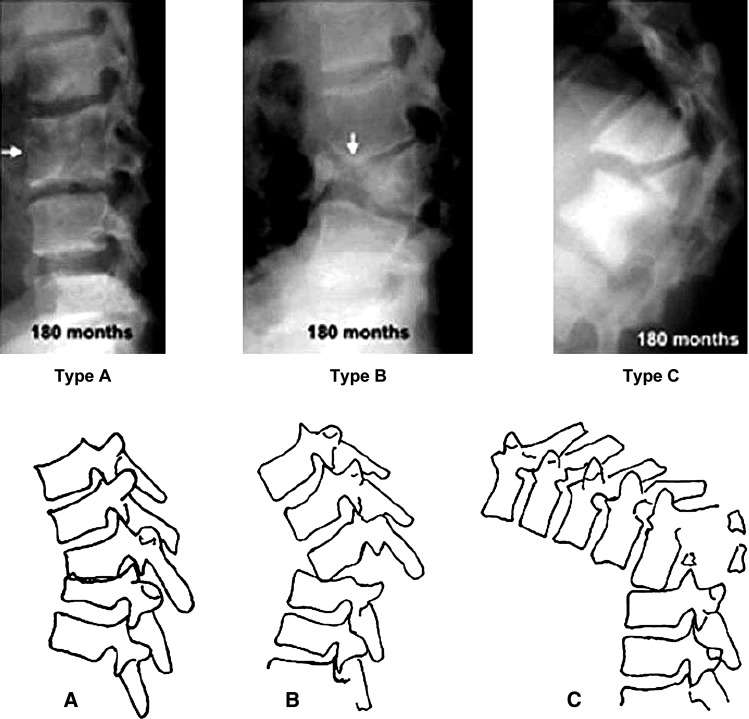
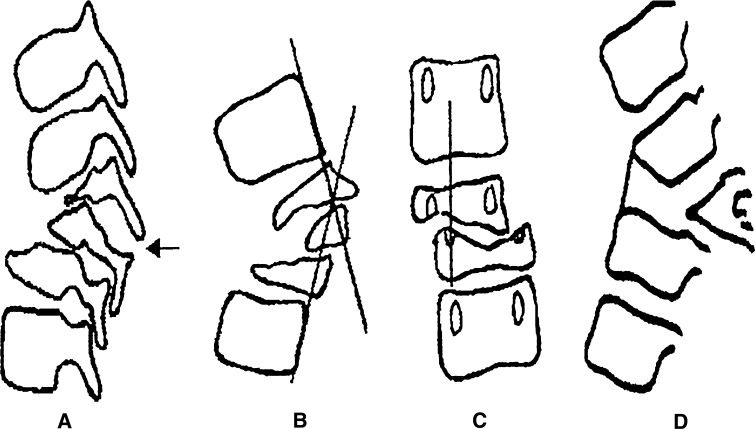
Tuberculosis preferentially affects the anterior segment of the vertebral column in more than 90 % of the patients. Although chemotherapy may inactivate the infectious process, vertebral collapse can continue until the healthy vertebral bodies in the region of the kyphosis approximate anteriorly and consolidate. Depending on the extent of initial vertebral loss, three types of collapse and healing of the anterior column are noted [10], (Table 1; Fig. 1).
Table 1.
Types of restabilization in thoracolumbar spinal tuberculosis
| Type of restabilization | Anterior column contact | Vertebral body loss | Facet joints | Final deformity |
|---|---|---|---|---|
| Type A | Wide | <0.75 | Intact | Spontaneous improvement, if increase <10° |
| Type B | Point contact | 0.75–1.5 | Subluxed or single level dislocation | <60° |
| Type C | By 90° sagittal rotation of superior vertebrae | >1.5 | Dislocation of two or more | Can be more than 100° |
Fig. 1.
Following destruction of the anterior column, restabilization occurs by one of the three methods. a In patients with partially destroyed vertebrae, restabilization occurs with a wide contact area. There is no dislocation of the facet joints. b In patients with dislocation of a single facet joint, restabilization occurs by point contact. c In patients with loss of two or three vertebrae in the thoracolumbar region, the facets dislocate at multiple levels. The superior segment of the vertebral column rotates by 90° so the anterior surface of the superior vertebra rests on the superior surface of the inferior vertebra. The superior segment of the vertebral column becomes horizontal
Type A healing involves partially destroyed vertebral bodies coming into contact with a large contact area between them, in the presence of intact facet joints. This pattern is seen commonly in adults and in the patients with paradiscal type of involvement, where bony destruction is minimal. It is also seen frequently in the lumbar region, where the collapse of the vertebrae is telescopic due to the sagittal alignment of the facet joints. The spinal column here is stable because of consolidation of the anterior column along with intact facet joints posteriorly.
Type B healing is seen in patients with loss of one or one and a half vertebral body. Here during the process of collapse, the facet joints are subluxed or dislocated at one level before the contact of normal vertebra can occur. The superior vertebra rotates in the sagittal plane during the process of descent so that its anteroinferior margin comes into point contact with the superior surface of the inferior normal vertebra. There is growth suppression at the point of contact with a moderate increase in deformity due to continued growth posteriorly. The final kyphosis is usually less than 60°. When the deformity crosses 40°, associated growth disturbances are usually seen in the normal vertebral segments within the arc of kyphosis with wedging of the anterior half of the vertebral bodies due to the increased compressive force, which further contributes to an increase in the deformity.
Type C healing occurs when more than two vertebral bodies are lost. The large anterior column defect necessitates the dislocation of two or more facet joints before anterior column healing can occur. The superior normal vertebra descends along with 90° rotation in the sagittal plane so that the anterior surface of the superior vertebra comes into contact with the superior surface of the inferior vertebra. Secondary growth disturbances which are commonly seen in both the fusion mass and the adjacent normal vertebral segments allow a gradual increase in deformity even after complete cure of the disease [10]. This type of stabilization is seen especially in children less than 7 years of age and in those with thoracolumbar disease.
In a 15-year follow-up study, the deformity was analysed as Active phase (Phase I) changes, which included the progress during the active phase of the disease and Healed phase (Phase II) changes, which included the changes following the achievement of disease cure.
Factors affecting the progression of deformity
Influence of age on deformity
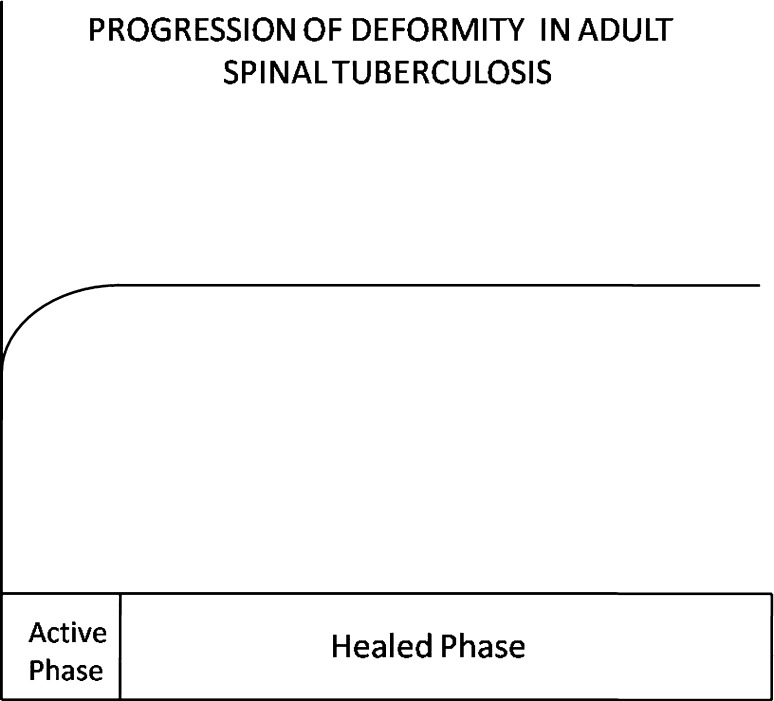
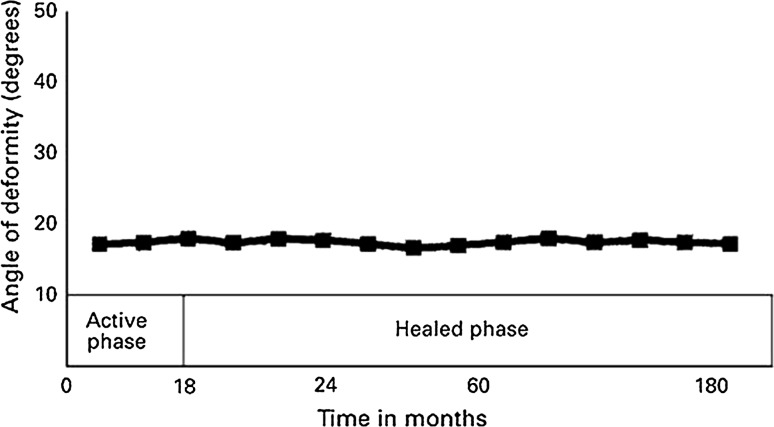
Age at a start of treatment had a significant effect on the progress of deformity [11]. Adult patients had a lesser deformity at presentation and a lesser increase in deformity as compared to children, during Phase I for each vertebral body loss. Also adults had virtually no change in the deformity after cure of the disease [12] (Fig. 2). The final deformity was usually less than 30°. Children as against, had a higher deformity at presentation, a significantly greater tendency for collapse during the active phase of the disease, and continued and variable progression even after the infection was cured and growth completed [10]. In a 15-year follow-up study of patients treated with ambulant chemotherapy, the vertebral body loss at the beginning of treatment in children under 15 years of age (1.9) was nearly twice that of adults (0.96). Similarly, the degree of collapse that occurred in the first 18 months per vertebral body loss in patients, under 10 years of age was nearly double than that seen in adults [13]. This is probably due to the increased susceptibility of the pediatric spine to destruction and its increased flexibility in comparison to that of the adult spine.
Fig. 2.
The pattern of progress of deformity in spinal tuberculosis in an adult is shown. The increase in deformity is limited to the active stage of the disease during which time consolidation and healing occurred. There is no additional change in deformity after 18 months
Changes in the healed phase
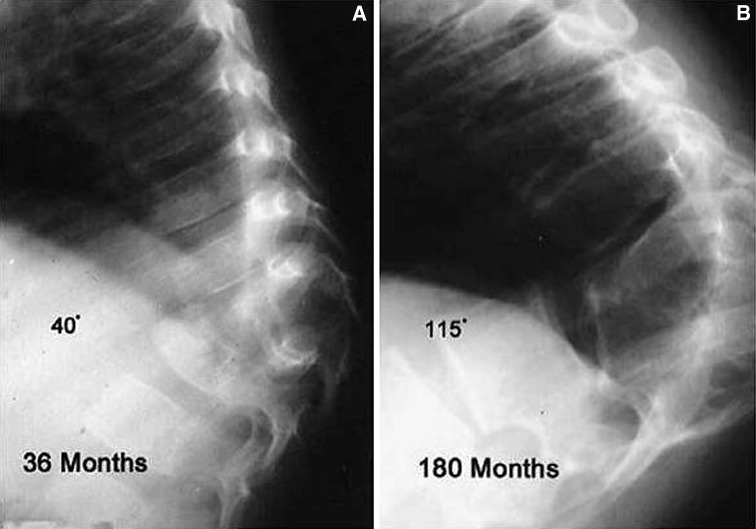
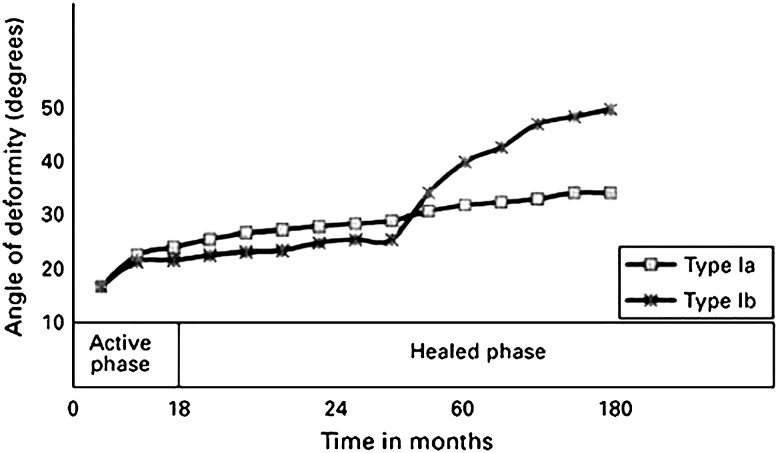
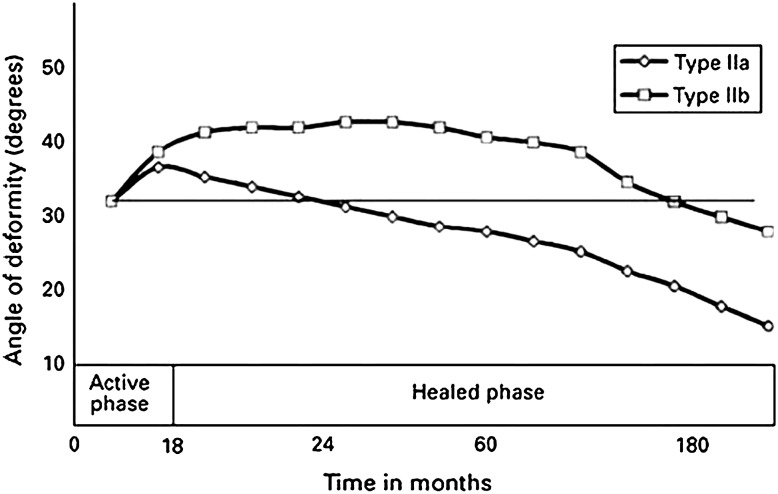
Spinal deformity in children also differs in its potential to worsen even after the infection is cured. Unlike adults in whom the deformity is static after cure of the disease [14], post-tuberculous kyphosis in children is a dynamic deformity with variable progression throughout the growth phase of the child (Fig. 3). In a longitudinal study on the progress of deformity in children with tuberculosis of the spine, Rajasekaran [12] found a decrease in deformity in 44 % of the children, an increase in deformity in 39 % of the children and no change in deformity in 17 % of the children. Five distinct types of progression were seen during the growth phase [12]. Type I (Fig. 4) progression shows continued increase in deformity through the entire period of growth. This increase could occur continuously after Phase I (Type Ia) or begin 3–6 years after the disease was cured (Type Ib). Type Ib progression is important because the increase in deformity was maximal and also because the lag period during which the deformity was static may result in the progression being missed. It is common practice to follow up children for only 2–3 years after the disease is cured and the delayed onset of progression in deformity usually is missed. Type II (Fig. 5) progression shows regression during growth with a decrease in deformity after healing of the disease. This can occur immediately after Phase1 (Type IIa) or begin after 3–6 years (Type IIb). Children with Type IIa progression had the best outcome as they had a lesser increase during Phase I, and a significant improvement during Phase II. In Type III (Fig. 6) progression, children who had minimal destruction of the vertebral bodies did not have any major change in the deformity during the active phase and the healed phase.
Fig. 3.
Radiographs showing a healed thoracic lesions in a 3-year-old girl with a deformity of 40° at 3-year follow-up, b this progressed to 115° at 15 years
Fig. 4.
Graph showing that Type I progression showed deterioration in the deformity even after healing of the disease. In Type Ia this deterioration continued through-out growth whereas in Type Ib progression there was a lag period of a few years before the deterioration started. The progression was more severe in Type Ib
Fig. 5.
Graph showing that type II progression had a decrease in deformity during the healed phase. In type IIa the improvement started soon after healing of the disease and in type IIb after a lag period of a few years
Fig. 6.
Graph showing that type III progression had only a minimal increase in deformity during the active phase and little change during the healed phase. This was found in children with only minimal structural involvement
Influence of the level of lesion
The level of the lesion in the spine plays an important influence on the presentation and progression of spinal deformity. The thoracic lesions and thoracolumbar lesions have a significantly greater deformity at presentation [12] and are more likely to progress than lumbar or lumbosacral lesions. The average angle of deformity per vertebral loss at the start of treatment was 20.3° in the thoracic region, while it was 19.5° in the thoracolumbar region and only 2.8° in the lumbar region [12]. At 15-year follow-up the deformity per vertebral loss was 26.7° in the thoracic region, 27.6° in the thoracolumbar region and only 9.2° in the lumbar region [12]. This difference is due to the sagittal curvature of the spine, where the natural thoracic kyphosis allows progression of the disease and the lumbar lordosis offers protection against a kyphotic collapse. In the lumbar region, because of the larger size of the disc, the vertical orientation of the articular facets and the relative narrowness of the pedicle, healing is usually by a telescopic collapse. In the thoracic spine, the more horizontally oriented articular facets allow earlier subluxation of the facet joints leading to a rapid collapse.
Buckling collapse
In children with severe spinal destruction, a peculiar pattern of collapse is seen which has been termed as “Buckling Collapse” [15]. These children had complete destruction of more than two vertebral bodies. During collapse, dislocation of facet joints occurred at multiple levels leading to a kyphosis of more than 120°. Vertebral stabilisation occurred by the contact of the anterior surface of many vertebral segments above and below the deformity and the entire spine was converted into two large compensatory curves. Many vertebral segments thus became horizontally oriented with stress shielding of their growth plates. Longitudinal overgrowth of vertebral segments (Fig. 7) were noted leading to stretching of the spinal cord at the apex of the kyphosis with possible secondary late onset paraplegia [10, 12].
Fig. 7.

An example of buckling collapse, the cephalad arm of the kyphosis is completely horizontal. Longitudinal overgrowth of multiple segments, a cause of late-onset paraplegia, is seen
Risk factors for buckling collapse included an age of less than 7 years at the time of the disease, thoracolumbar involvement, loss of more than two vertebral bodies, and the presence of radiographic spine-at-risk signs. Children at risk for buckling collapse must be carefully watched and the spine stabilized to avoid a massive increase in deformity [15].
Patients at risk for severe deformity
Identifying the subset of patients at risk for progression of deformity is essential as early surgical intervention can avoid development of severe deformity. Risk factors for severe progression are as follows [6, 10, 12, 15]:
An age below 10 years
Vertebral body loss of more than 1–1.5
A pre-treatment deformity angle of greater than 30°, especially in children
Cervical thoracic and thoracolumbar junctional lesions
The presence of ‘spine-at-risk’ radiological signs
“Spine-at-risk” signs
Rajasekaran described four simple radiological signs which reliably predict and identify children who are at risk for severe deformity. These signs are (Fig. 8) (a) “Separation of the facet joint” the facet joint separates at the apex of the curve, causing instability and loss of alignment. (b) “Retropulsion” the posterior retropulsion of the diseased vertebral segment is identified by drawing two lines along the posterior surfaces of the first upper and lower normal vertebra. (c) “Lateral translation” is confirmed, when the line drawn through the middle of the pedicle of the lower vertebra does not touch the pedicle of the superior vertebra. (d) “Toppling” in the initial stages of collapse, the line drawn along the anterior surface of the lower normal vertebra intersects the inferior surface of the upper normal vertebra. Toppling has occurred when the line intersects above the middle of the anterior surface of the upper vertebra. All these signs represent the presence of spinal instability due to dislocation of the facet joints. Each sign is given a score of 1 with a maximum possible score of 4. A spinal instability score of more than 2 is associated with a significantly larger final deformity. A score of 3 or more accurately predicts an increase in the angles of deformity and kyphosis of more than 30° and a final deformity of more than 60° [10, 14].
Fig. 8.
“Spine-at-risk” radiological signs. a Separation of the facet joint, b retropulsion, c lateral translation, d toppling
These signs have immense practical value in clinical management as they appear very early in the course of the disease, even during the active phase [10]. This allows for spinal stabilization to be performed before the progress of deformity.
Conclusion
Prevention of deformity is the primary aim in the treatment of spinal tuberculosis as availability of potent antituberculous drugs has made uncomplicated tuberculosis a medical disease. The severity of deformity in spinal tuberculosis depends on the extent of vertebral destruction, level of lesion and age of the patient with more severe deformities seen in children and in lesions involving the thoracolumbar spine. Identification of the type of anterior column collapse and healing can help to predict the extent of final deformity. Thoracic and thoracolumbar lesions are more likely to progress than lumbar or lumbosacral lesions. In children, deformity may continue to progress during growth even after the disease is cured and they should be followed up till completion of growth. The presence of two or more “spine-at-risk” radiological signs and “pretreatment” deformity of 30° are the harbingers of severe late collapse and deformity, especially in children.
Conflict of interest
None.
References
- 1.Satyasri S. Global epidemiology of tuberculosis. In: Sathyasri S, editor. Text book of pulmonary and extra-pulmonary tuberculosis. Madras: Interprint; 1993. pp. 13–18. [Google Scholar]
- 2.Medical Research Council A 15-year assessment of controlled trials of the management of tuberculosis of the spine in Korea and Hong Kong. J Bone Joint Surg [Br] 1998;80-B:456–462. doi: 10.1302/0301-620x.80b3.8544. [DOI] [PubMed] [Google Scholar]
- 3.Moon MS, Woo YK, Lee KS, et al. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine. 1995;20:1910–1916. doi: 10.1097/00007632-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Moon MS. Tuberculosis of the spine, controversies and a new challenge. Spine. 1997;22:1791–1797. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 5.Moon MS, Kim I, Woo YK, Park YO. Conservative treatment of tuberculosis of the thoracic and lumbar spine in adults and children. Int Orthop. 1987;11:315–322. doi: 10.1007/BF00271307. [DOI] [PubMed] [Google Scholar]
- 6.Parathasarathy R, Sriram K, Satha T, et al. Short course chemotherapy for tuberculosis of the spine: a comparison between ambulant treatment and radical surgery. J Bone Joint Surg. 1999;81B:464–471. doi: 10.1302/0301-620X.81B3.9043. [DOI] [PubMed] [Google Scholar]
- 7.Moon MS, Lee MK. The changes of the kyphosis of the tuberculous spine in children following ambulant treatment. Korean Orthop Assoc. 1971;6:203–208. [Google Scholar]
- 8.Tuli SM. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop. 1995;19:327–331. doi: 10.1007/BF00181121. [DOI] [PubMed] [Google Scholar]
- 9.Yau ACMC, Hsu LCS, O’Brien JP, Hodgson AR. Tuberculosis kyphosis—correction with spinal osteotomy, halo-pelvic distraction and anterior and posterior fusion. J Bone Joint Surg. 1974;56A:1419–1434. [PubMed] [Google Scholar]
- 10.Rajasekaran S. The natural history of post-tubercular kyphosis in children: radiological signs which predict late increase in deformity. J Bone Joint Surg. 2001;83B:954–962. doi: 10.1302/0301-620X.83B7.12170. [DOI] [PubMed] [Google Scholar]
- 11.Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg. 1989;71A:1314–1323. [PubMed] [Google Scholar]
- 12.Rajasekaran S (1999) A longitudinal study on the progress of deformity in children with spinal tuberculosis. PhD Thesis. Dr. MGR Medical University, Chennai
- 13.Rajasekaran S, Shanmugasundaram TK, Dheenadhayalan J, Shetty DK. Tuberculosis lesions of the lumbosacral region: a 15-year follow-up of patients treated by ambulant chemotherapy. Spine. 1999;23:1163–1167. doi: 10.1097/00007632-199805150-00018. [DOI] [PubMed] [Google Scholar]
- 14.Rajasekaran S. The Problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002;398:85–92. doi: 10.1097/00003086-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Rajasekaran S. Buckling collapse of the spine in childhood spinal tuberculosis. Clin Orthop Relat Res. 2007;460:86–92. doi: 10.1097/BLO.0b013e31806a9172. [DOI] [PubMed] [Google Scholar]