Abstract
Introduction
Tuberculous spondylitis (TBS) is the most common form of extra-pulmonary tuberculosis. The mainstay of TBS management is anti-tuberculous chemotherapy. Most of the patients with TBS are treated conservatively; however in some patients surgery is indicated. Most common indications for surgery include neurological deficit, deformity, instability, large abscesses and necrotic tissue mass or inadequate response to anti-tuberculous chemotherapy. The most common form of TBS involves a single motion segment of spine (two adjoining vertebrae and their intervening disc). Sometimes TBS involves more than two adjoining vertebrae, when it is called multilevel TBS. Indications for correct surgical management of multilevel TBS is not clear from literature.
Materials and methods
We have retrospectively reviewed 87 patients operated in 10 years for multilevel TBS involving the thoracolumbar spine at our spine unit. Two types of surgeries were performed on these patients. In 57 patients, modified Hong Kong operation was performed with radical debridement, strut grafting and anterior instrumentation. In 30 patients this operation was combined with pedicle screw fixation with or without correction of kyphosis by osteotomy. Patients were followed up for correction of kyphosis, improvement in neurological deficit, pain and function. Complications were noted. On long-term follow-up (average 64 months), there was 9.34 % improvement in kyphosis angle in the modified Hong Kong group and 47.58 % improvement in the group with pedicle screw fixation and osteotomy in addition to anterior surgery (p < 0.001). Seven patients had implant failures and revision surgeries in the modified Hong Kong group. Neurological improvement, pain relief and functional outcome were the same in both groups.
Conclusion
We conclude that pedicle screw fixation with or without a correcting osteotomy should be added in all patients with multilevel thoracolumbar tuberculous spondylitis undergoing radical debridement and anterior column reconstruction.
Keywords: Tuberculous spondylitis, Multilevel, Thoracolumbar, Surgical treatment, Pott’s disease, Caries spine
Introduction
Tuberculous spondylitis (TBS) is the most common form of extra-pulmonary tuberculosis [1, 2]. Most of TBS patients belong to poor socio-economic status, which cannot afford costly treatment and cannot be off job for long time for financial reasons [3]. Incidence of TBS in developed countries has recently been increasing due to travel abroad, immune-compromising diseases caused by viruses like HIV and emergence of multi-drug resistant strains [4]. There are many morphological forms of TBS. In its most common form TBS involves the anterior column of a single motion segment i.e. two adjoining vertebral bodies and their intervening disc (peri-discal). Sometimes TBS involves more than single motion segment and this form is called multilevel (three or more vertebrae), this may be contiguous or non-contiguous. In 2–10 % cases TBS involves either posterior column only (vertebral arch) or a single vertebral body (central) [5].
Mainstay of TBS management is anti-tuberculous treatment (ATT) with multiple drugs for 9–18 months. Most of the patients respond to ATT alone, however in some, surgery is also indicated. Main indications for surgery are; mechanical compression of spinal cord or cauda equina causing neurological compromise, gross deformity causing sagittal imbalance, clinical instability, dead and necrotic bone where blood cannot reach, large abscess and necrotic tissue mass which may take very long time to resolve on ATT alone and unclear diagnosis despite percutaneous biopsy or failure of adequate response to ATT [5–7]. Many studies in the past have proven superior outcome with radical debridement of diseased tissue and anterior strut grafting, with or without addition of instrumentations. However, for correction of deformity posterior approach is superior [8–10].
Most of the literature focuses on most common peri-discal form of TBS involving single motion segment, there is very little data available on surgical management of multilevel thoracolumbar TBS (MLTLTBS). To clearly define surgical management guidelines of contiguous MLTLTBS, we have retrospectively analysed data from our spine unit and also reviewed the available literature in our present paper.
Materials and methods
Eighty-seven patients with MLTLTBS, underwent surgery at our spine unit between 2001 and 2010 (10 years). Data of all these patients were retrieved from spine database of our unit and were analysed. These 87 patients underwent 95 surgeries. Seven patients had multiple surgeries and rest had single surgery. There were 50 males and 37 females with an average age of 36 years (range 1–82 years). All patients had at least three contiguous vertebral involvements with TBS. ASIA impairment scale (AIS) was used for assessment of neurological status. Eleven patients (12.64 %) were neurologically intact (AIS-E). Twenty patients (22.99 %) had complete neurological deficit (AIS-A). Fifty-six patients (64.37 %) had incomplete neurological deficit (10 AIS-B, 27 AIS-C, and 19 AIS-D). Seven patients (8.04 %) were treated for active pulmonary tuberculosis.
Denis scale was used for assessment of pain and function. In this scale both pain and function is graded from zero to five. Grade 0 being no pain and complete recovery of functional status with return to premorbid levels. Grade 1 is intermittent mild pain which does not require medication and only mild limitation to returning to previous occupation. Grade 2 in frequent mild pain, requiring occasional medication, and there is severe limitation to returning to previous occupation. Grade 3 is moderate pain requiring continuous non-narcotics; functionally these patients adopt a modified job and need energy-saving life style. Grade 4 is a severe pain requiring continuous pain medication with intermittent narcotics and there is significant loss of function and activities of daily living. Grade 5 is an excruciating pain requiring continuous narcotic intake and there is complete loss of function [11].
All patients had raised erythrocyte sedimentation rate and positive intradermal test for tuberculosis (Mantoux test). All patients had consistent X-rays and MRI or CT findings with MLTLTBS. At the time of surgery specimen was sent for culture and histopathology. All patients had positive histopathology for TBS showing chronic granulomatous inflammation with multinucleate Langerhans giant cells, however, only nine patients had positive culture for Mycobacterium tuberculosis (MTB). Kyphosis angle was measured by longitudinal lines passing through the upper end plate of upper and lower endplate of lower vertebrae. In lumbar spine, kyphosis angle was adjusted to cater for normal lumbar lordosis by adding 10° per level of deformity.
All patients had at least 4 weeks of ATT prior to surgery and were continued with same or modified regimen for at least 1 year in total. First line drugs included a combination of rifampicin, isoniazid, ethambutol and pyrazinamide. These four drugs were continued for 3 months and then pyrazinamide was dropped and rest of the three were continued for 9 more months at least. In resistant cases six-drug regimen was used initially for 4 months with addition of levofloxacin and amikacin. Indications for surgery included; neurological deficit due to mechanical compression, deformity, instability, severe or excruciating pain, large diseased tissue mass or necrotic bone, failure to respond to ATT and bed rest or diagnosis not confirmed by biopsy.
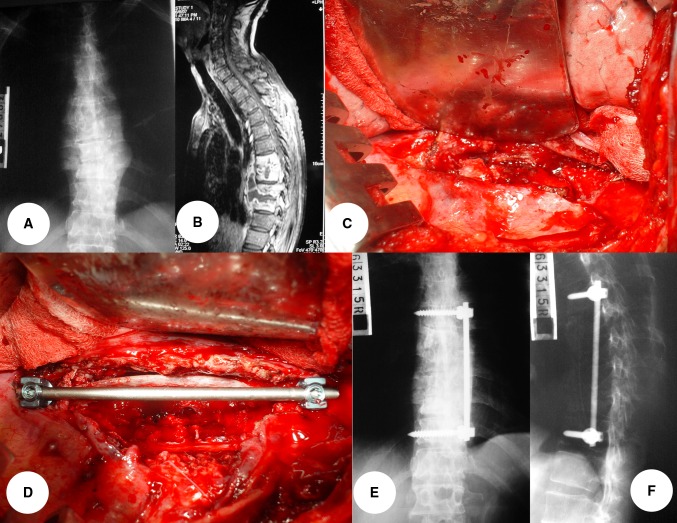
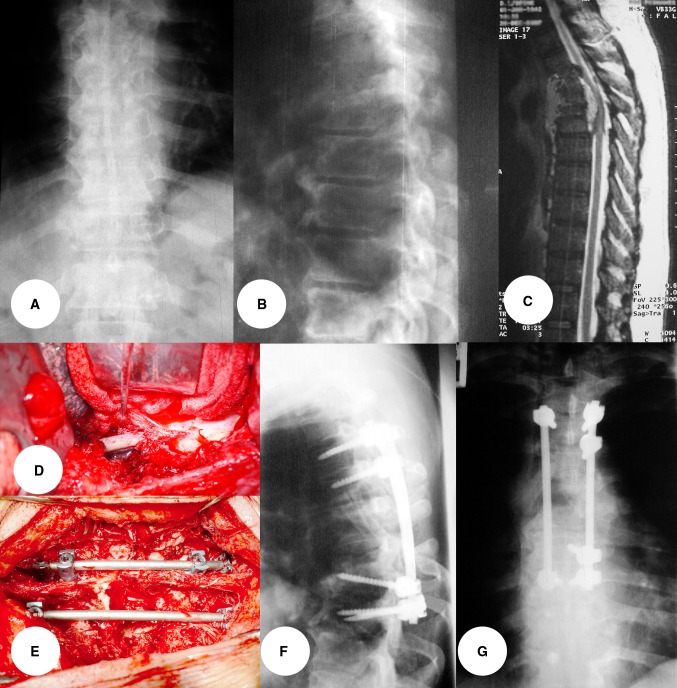
Two types of surgical procedures were performed for these patients depending upon the degree of kyphosis present. For clinically un-remarkable kyphosis only modified Hong Kong operation (MHK) was performed (n = 57) (Fig. 1). In this operation spine was approached antero-laterally by a trans-thoracic, trans-diaphragmatic or trans-abdominal retroperitoneal approach, and radical debridement and strut grafting (RDSG) was performed. Strut grafting was done either with 2–3 locally harvested rib graft or a free fibular graft. This was reinforced with lateral body screw rod construct. For clinically appreciable kyphosis, in addition to RDSG, a posterior approach was used with pedicle screw fixation (PSF + RDSG) (n = 30) (Fig. 2).
Fig. 1.
A 57-year-old male patient with tuberculous spondylitis involving T8–11 vertebrae. Presented with back pain and paraplegia. a, b Preoperative X-ray and MRI showing spondylodiscitis and paravertebral abscess. c, d Showing modified Hong Kong operation after radical debridement and strut grafting with two pieces of ribs, stabilized with body screw rod construct. e, f X-rays on follow-up showing solid fusion. He had complete relief of pain and became neurologically normal
Fig. 2.
A 65-year-old male patient with tuberculous spondylitis T5–7 presented with back pain and paraplegia. a–c Pre-op X-rays and MRI showing collapse of vertebrae, abscesses and cord compression. d, e Anterior radical debridement and bone grafting with two pieces of ribs and posterior spinal osteotomy to correct kyphosis and pedicle screw fixation as an one-stage procedure. f, g Post-op X-rays on follow-up showing solid fusion. This patient had complete neurological recovery and was pain free
Pre-op and post-op data were available for all patients from spine unit database. For final follow-up patients were contacted on telephone. Only 54 patients (62.07 %) could be contacted on telephone. They were asked to visit the clinic for final follow-up. Only 40 patients (45.98 %) turned up for final follow-up and their complete data were available. Average follow-up was for 64 months, range 16–132 months. Following parameters were assessed on follow-up; neurological status using AIS, pain and function status using Denis scale, spinal fusion and kyphosis angle using plain X-rays, and complications following surgery.
Results
Out of 87 patients, thoracic spine was involved in 55 patients (63.22 %), thoracolumbar in 26 patients (29.89 %), and lumbar spine was involved in six patients (6.90 %). Vertebral level involvement is shown in Table 1.
Table 1.
Surgical data showing vertebral involvement in multilevel thoracolumbar tuberculous spondylitis
| No. of vertebrae involved | No. of patients | Percentage (%) |
|---|---|---|
| 3 | 50 | 57.47 |
| 4 | 19 | 21.84 |
| 5 | 7 | 8.05 |
| 6 | 5 | 5.75 |
| 7 | 1 | 1.15 |
| 8 | 2 | 2.30 |
| 9 | 3 | 3.45 |
| Total | 87 | 100.00 |
Out of the 40 patients with complete follow-up data, 25 were in MHK group and 15 in PSF + RDSG group. Both groups matched for age and sex distribution. Average duration of surgery and blood loss in both groups were as follows:
- Duration of surgery
- MHK = 125 min
- PSF + RDSG = 344 min
- Blood loss
- MHK = 1254 ml
- PSF + RDSG = 2213 ml
In MHK, average pre-op kyphosis angle was 26.41°, this improved to 18.89° post-operatively but fell down to 23.95° on last follow-up (over all 9.34 % improvement in kyphosis angle). In PSF + RDSG group, average pre-op kyphosis angle was 51.05°, this improved to 22.31° post-operatively and on last follow-up it was 24.29° (over all 47.58 % improvement in kyphosis angle). These differences were highly statistically significant between two groups (P < 0.001).
All patients improved neurologically after surgery and there was no difference between two groups. Overall improvement in ASIA impairment scale was highly significant (P < 0.001). Details are shown in Table 2.
Table 2.
Pre-op versus post-op ASIA impairment scale (AIS)
| AIS | Pre-op pts | Pre-op (%) | Post-op pts | Post-op (%) |
|---|---|---|---|---|
| A | 11 | 27.50 | 0 | 0.00 |
| B | 4 | 10.00 | 1 | 2.50 |
| C | 15 | 37.50 | 4 | 10.00 |
| D | 8 | 20.00 | 5 | 12.50 |
| E | 2 | 5.00 | 30 | 75.00 |
| Total | 40 | 100.00 | 40 | 100.00 |
Denis pain scale was improved by 61.75 % in MHK group and 67.5 % in PSF + RDSG group (P = 0.535). Denis function scale was improved by 56.25 % in MHK group and 61.5 % in PSF + RDBG (P = 0.165). All patients showed solid fusion on X-rays at last follow-up. Seven patients had revision surgeries as shown in Table 3.
Table 3.
Revision surgeries
| Pt no. | Group | First revision | Second revision | Third revision |
|---|---|---|---|---|
| 1 | MHK | Implant failure–revised | Removal of implants for second implant failure | Pedicle subtraction osteotomy for recurrent deformity |
| 2 | MHK | Removal of implant for failure | Pedicle subtraction osteotomy for persistent deformity | |
| 3 | MHK | Pedicle subtraction osteotomy for deformity | ||
| 4 | MHK | Removal of implant for failure | ||
| 5 | MHK | Removal of implant for failure | ||
| 6 | MHK | Removal of implant for failure | ||
| 7 | MHK | Removal of implant for failure | ||
Discussion
There is consensus on medical management of tuberculous spondylitis (TBS); however, literature is quite divided on surgical management of multilevel TBS. Some people recommend conservative treatment others focus on anterior, posterior or combined surgeries [1, 4, 6, 8–10, 12–16]. Goals of surgical management include radical debridement, decompression of spinal cord or cauda equina, prevention or correction of deformity, bone grafting to achieve solid fusion, stable internal fixation to allow early ambulation and return of patient back to society and occupation as soon as possible [4, 6, 7, 17].
Though ATT and conservative management is sufficient in most of the cases, there are definite indications for surgery in some patients. As TBS is most of the time disease of anterior column of spine, anterior approaches give direct access to pathological area and maximum chance for clearance of neurological tissues [16–19]. Reconstruction can be done with autologous rib, iliac crest or fibular grafts. Allograft bone has been used by some people and so are titanium and stainless steel cages [18–20]. For stabilization of various types of plates, rod screw constructs are available. Many studies have shown biocompatibility of these metals and their use in infected focus [19, 20]. Though anterior approach gives good chance of clearance of disease and decompression of cord and roots, it cannot correct or prevent deformity to any appreciable extent. Anterior debridement can be done minimally invasively as well [21].
Main benefit of posterior approach is better fixation for implants and good correction of kyphotic deformity, however, neurological decompression and excision of diseased tissue is quite inadequate most of the times by posterior approach alone and an anterior approach is needed either at the same time or at an earlier or late stage. Some people have shown good results by using single posterior approach to achieve all above goals in one sitting but this needs a lot of experience and work load of TBS patients [9, 14, 22, 23]. Furthermore, these combined approaches add to operating time and blood loss and need intensive care time for the operated patient.
Our study has shown that anterior approach cannot significantly correct deformity and posterior approach gives better correction of deformity. All implant-related complications in our study occurred only in anterior alone group, which further strengthens the concept of better stability with posterior instrumentation in multilevel TBS. There is no significant difference in neurological improvement, pain relief or functional outcome between two approaches, however, these outcomes need further evaluation by bigger studies with more comprehensive follow-ups.
In conclusion, we suggest that in multilevel tuberculous spondylitis, posterior instrumentation should be added in all cases to prevent long-term progression of deformity and anterior implant failure.
Acknowledgments
Conflict of interest
None.
References
- 1.Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282(7):677–686. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 3.Janssens JP, de HR. Spinal tuberculosis in a developed country. A review of 26 cases with special emphasis on abscesses and neurologic complications. Clin Orthop Relat Res. 1990;257:67–75. [PubMed] [Google Scholar]
- 4.Luk KD. Tuberculosis of the spine in the new millennium. Eur Spine J. 1999;8(5):338–345. doi: 10.1007/s005860050185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradford LC, Frank JE. Infections of the spine. In: Herkowitz HN, Garfin SR, Balderston RA, Eismont FJ, Bell GR, Wiesel SW, editors. spine. 4. Saunders: W. B; 1999. pp. 1207–1258. [Google Scholar]
- 6.Moon Tuberculosis of the spine. Controversies and a new challenge. Spine (Phila Pa 1976) 1997;22(15):1791–1797. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 7.Ge Z, Wang Z, Wei M. Measurement of the concentration of three antituberculosis drugs in the focus of spinal tuberculosis. Eur Spine J. 2008;17(11):1482–1487. doi: 10.1007/s00586-008-0778-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erturer E, Tezer M, Aydogan M, Mirzanli C, Ozturk I. The results of simultaneous posterior—anterior—posterior surgery in multilevel tuberculosis spondylitis associated with severe kyphosis. Eur Spine J. 2010;19(12):2209–2215. doi: 10.1007/s00586-010-1481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Zhang Y, Zhang X, Wang Z, Mao K, Chen C, et al. Posterior-only multilevel modified vertebral column resection for extremely severe Pott’s kyphotic deformity. Eur Spine J. 2009;18(10):1436–1441. doi: 10.1007/s00586-009-1067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang HQ, Guo CF, Xiao XG, Long WR, Deng ZS, Chen J. One-stage surgical management for multilevel tuberculous spondylitis of the upper thoracic region by anterior decompression, strut autografting, posterior instrumentation, and fusion. J Spinal Disord Tech. 2007;20(4):263–267. doi: 10.1097/01.bsd.0000211281.68400.1b. [DOI] [PubMed] [Google Scholar]
- 11.Denis F, Armstrong GW, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984;189:142–149. [PubMed] [Google Scholar]
- 12.Ekere AU, Yellowe BE, Echem RC. Conservative management of tuberculous spondylitis in a developing country. Niger J Med. 2005;14(4):386–389. [PubMed] [Google Scholar]
- 13.Jin D, Qu D, Chen J, Zhang H. One-stage anterior interbody autografting and instrumentation in primary surgical management of thoracolumbar spinal tuberculosis. Eur Spine J. 2004;13(2):114–121. doi: 10.1007/s00586-003-0661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajasekaran S, Vijay K, Shetty AP. Single-stage closing–opening wedge osteotomy of spine to correct severe post-tubercular kyphotic deformities of the spine: a 3-year follow-up of 17 patients. Eur Spine J. 2010;19(4):583–592. doi: 10.1007/s00586-009-1234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Louw JA. Spinal tuberculosis with neurological deficit. Treatment with anterior vascularised rib grafts, posterior osteotomies and fusion. J Bone Joint Surg Br. 1990;72(4):686–693. doi: 10.1302/0301-620X.72B4.2380228. [DOI] [PubMed] [Google Scholar]
- 16.Ozdemir HM, Us AK, Ogun T. The role of anterior spinal instrumentation and allograft fibula for the treatment of pott disease. Spine (Phila Pa 1976); 2003;28(5):474–479. doi: 10.1097/01.BRS.0000048666.17934.17. [DOI] [PubMed] [Google Scholar]
- 17.Eighth Report of the Medical Research Council Working Party on Tuberculosis of the Spine (1982) A 10-year assessment of a controlled trial comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong Kong. J Bone Joint Surg Br 64(4):393–398 [DOI] [PubMed]
- 18.Cavusoglu H, Kaya RA, Turkmenoglu ON, Tuncer C, Colak I, Aydin Y. A long-term follow-up study of anterior tibial allografting and instrumentation in the management of thoracolumbar tuberculous spondylitis. J Neurosurg Spine. 2008;8(1):30–38. doi: 10.3171/SPI-08/01/030. [DOI] [PubMed] [Google Scholar]
- 19.Benli IT, Acaroglu E, Akalin S, Kis M, Duman E, Un A. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J. 2003;12(2):224–234. doi: 10.1007/s00586-002-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine (Phila Pa 1976) 1993;18(13):1890–1894. doi: 10.1097/00007632-199310000-00028. [DOI] [PubMed] [Google Scholar]
- 21.Lu G, Wang B, Li J, Liu W, Cheng I. Anterior debridement and reconstruction via thoracoscopy-assisted mini-open approach for the treatment of thoracic spinal tuberculosis: minimum 5-year follow-up. Eur Spine J. 2012;21(3):463–469. doi: 10.1007/s00586-011-2038-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rajasekaran S, Rishi Mugesh KP, Shetty AP. Closing–opening wedge osteotomy for severe, rigid, thoracolumbar post-tubercular kyphosis. Eur Spine J. 2011;20(3):343–348. doi: 10.1007/s00586-010-1526-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang HQ, Lin MZ, Shen KY, Ge L, Li JS, Tang MX, et al. Surgical management for multilevel noncontiguous thoracic spinal tuberculosis by single-stage posterior transforaminal thoracic debridement, limited decompression, interbody fusion, and posterior instrumentation (modified TTIF) Arch Orthop Trauma Surg. 2012;132(6):751–757. doi: 10.1007/s00402-012-1473-z. [DOI] [PubMed] [Google Scholar]