Abstract
OBJECTIVE:
To examine temporal trend in the national incidence of bronchiolitis hospitalizations, use of mechanical ventilation, and hospital charges between 2000 and 2009.
METHODS:
We performed a serial, cross-sectional analysis of a nationally representative sample of children hospitalized with bronchiolitis. The Kids Inpatient Database was used to identify children <2 years of age with bronchiolitis by International Classification of Diseases, Ninth Revision, Clinical Modification code 466.1. Primary outcome measures were incidence of bronchiolitis hospitalizations, mechanical ventilation (noninvasive or invasive) use, and hospital charges. Temporal trends were evaluated accounting for sampling weights.
RESULTS:
The 4 separated years (2000, 2003, 2006, and 2009) of national discharge data included 544 828 weighted discharges with bronchiolitis. Between 2000 and 2009, the incidence of bronchiolitis hospitalization decreased from 17.9 to 14.9 per 1000 person-years among all US children aged <2 years (17% decrease; Ptrend < .001). By contrast, there was an increase in children with high-risk medical conditions (5.9%–7.9%; 34% increase; Ptrend < .001) and use of mechanical ventilation (1.9%–2.3%; 21% increase; Ptrend = .008). Nationwide hospital charges increased from $1.34 billion to $1.73 billion (30% increase; Ptrend < .001); this increase was driven by a rise in the geometric mean of hospital charges per case from $6380 to $8530 (34% increase; Ptrend < .001).
CONCLUSIONS:
Between 2000 and 2009, we found a significant decline in bronchiolitis hospitalizations among US children. By contrast, use of mechanical ventilation and hospital charges for bronchiolitis significantly increased over this same period.
Keywords: bronchiolitis, trends, hospitalization, incidence, mortality, hospital charge
What’s Known on This Subject:
Bronchiolitis is often cited as the leading cause of hospitalization for young children in the United States Previous studies reported increases in bronchiolitis hospitalizations through the 1990s. There are no recent efforts to assess national trends in bronchiolitis incidence and health care utilization.
What This Study Adds:
Between 2000 and 2009, we found a significant decline in bronchiolitis hospitalizations among US children. By contrast, use of mechanical ventilation and hospital charges for bronchiolitis significantly increased over this same period.
Bronchiolitis is often cited as the leading cause of hospitalization for infants, accounting for 18% of all hospitalizations, in the United States.1–5 Yearly, up to 3% of US infants are hospitalized with bronchiolitis, with reports of increasing hospitalization rates between 1980 and 1996.1 More recent US national estimates were ∼150 000 bronchiolitis hospitalizations annually, with total hospital charges of $1.4 billion in 2002.6
Although its public health burden is significant, previous research on bronchiolitis hospitalizations mainly focused on respiratory syncytial virus (RSV) bronchiolitis instead of bronchiolitis as a clinical diagnosis.7–13 RSV is the most common cause of bronchiolitis; however, many other infectious agents are associated with bronchiolitis.3,14,15 Therefore, estimates derived from samples of RSV bronchiolitis would underestimate hospitalization incidence and health care utilization.6 Furthermore, despite its significant public health burden, there have been no recent efforts to assess temporal trends in incidence, use of mechanical ventilation, and hospital charges of bronchiolitis hospitalizations among US children.
We therefore aimed to examine temporal trends in bronchiolitis hospitalizations between 2000 and 2009 by using a nationally representative sample.
Methods
Study Design and Setting
We performed a serial cross-sectional analysis of pediatric hospitalizations in 2000, 2003, 2006, and 2009, by using the Healthcare Cost and Utilization Project’s (HCUP) Kids’ Inpatient Database (KID), compiled by the Agency for Healthcare Research and Quality.16–19 The KID was designed to report hospital use and outcomes for children and is the only all-payer inpatient care database for children in the United States. The KID is a stratified sample of all pediatric discharges, defined as age ≤20 years, from states that participate in HCUP. States that participate in HCUP provide discharge-level data on all inpatient discharges from all “community” hospitals (ie, nonfederal, short-term, general, and specialty hospitals) in that state. KID contains a 10% stratified sample of uncomplicated in-hospital births and an 80% stratified sample of other pediatric cases. In 2009, the KID contained information for 7.4 million weighted discharges from 4121 hospitals in 44 states. The KID has been used study temporal trends in many populations and has been validated against the National Hospital Discharge Survey.20–22 Additional details of the KID can be found elsewhere.23 The institutional review board of Massachusetts General Hospital approved this analysis.
Identification of Sample
Pediatric discharges for patients age <2 years who had an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for bronchiolitis (466.1) in the primary or secondary diagnosis fields were eligible for our analysis. Bronchiolitis is a clinical diagnosis, with recognized challenges, including potential difficulty distinguishing between bronchiolitis and early asthma in children aged <2 years and potential overlap with pneumonia.24 In addition, to minimize the potential misclassification of transient tachypnea of the newborn or respiratory distress syndrome, hospitalizations for routine births identified using Clinical Classifications Software (CCS) code 218 in the first field were excluded.
Measurements
The KID contains information on patient characteristics, such as age, gender, race/ethnicity, primary insurance type (payer), admission day, discharge diagnoses and procedures, total charge for inpatient services, hospital length of stay, and disposition. To describe the socioeconomic status and burden of health care utilization, primary payer was included. Primary payer was grouped into public sources (Medicaid and Medicare), private payers, and other types. Additionally, race/ethnicity was categorized into non-Hispanic white, non-Hispanic black, Hispanic, and other. Diagnoses and procedures were available using ICD-9-CM and CCS, a methodology developed by the Agency for Healthcare Research and Quality to group ICD-9-CM codes into clinically sensible and mutually exclusive categories. High-risk medical condition was defined as history of prematurity (ie, ≤36 weeks’ gestation) or ≥1 complex medical condition, previously defined by using ICD-9-CM codes in 9 categories of illness (eg, neuromuscular, cardiovascular, and respiratory).25
Hospital characteristics include US region, urban-rural status, teaching status, and designation as a children’s hospital. Geographic regions (Northeast, South, Midwest, and West) were defined according to Census Bureau boundaries.26 Children’s hospital designation was determined from the National Association of Children’s Hospitals and Related Institutions classification criteria: non–children’s hospital and children’s hospital (children’s general hospital, children’s specialty hospital, and children’s unit in general hospital).27
Outcome Measures
The primary outcome measures were incidence of bronchiolitis hospitalization, use of mechanical ventilation (invasive or noninvasive ventilation, including bilevel/continuous positive airway pressure ventilation), and hospital charges. Other outcomes of interest included in-hospital management such as intravenous antibiotics and chest radiographs; length of stay; in-hospital mortality; and direct medical cost. Use of mechanical ventilation was identified by CCS code 216. Total hospital charges reflected the total facility fees reported for each discharge record. We identified in-hospital use of intravenous antibiotics (ICD-9-CM code 00.14, 99.21, and 99.22) and chest radiographs (ICD-9-CM code 87.44 and 87.49). In-hospital mortality was defined as the number of deaths divided by total number of bronchiolitis discharges. Because cost data were not available in the early part of the study period, we calculated direct medical costs by using hospital-specific cost-charge ratios for 2009 hospitalizations. Cost information was obtained from the hospital accounting reports collected by the Centers for Medicare and Medicaid Services. Because of incomplete hospital cost-charge ratio data, cases without hospital-specific cost-charge ratios were excluded, and data were appropriately reweighted to analyzed cost according to the HCUP recommendations.19
Statistical Analysis
All analyses used SAS-callable SUDAAN, version 11.0 (Research Triangle Institute, Research Triangle Park, NC) to obtain proper variance estimations that accounted for the complex sampling design.
We described changes in the weighted estimate of all outcomes in 2000, 2003, 2006, and 2009. To obtain incidence rates of bronchiolitis hospitalization, the annual number of estimated bronchiolitis hospitalizations were divided by population estimates from the US Census Bureau.28 Additionally, to address a possibility that diagnostic substitution may partially explain the temporal trend in bronchiolitis hospitalization rates, we examined temporal trends for pneumonia and asthma by using CCS codes 122 and 128 in the primary or secondary diagnosis field, respectively. Poisson regression was used to assess for temporal trend in incidence rates.
To examine temporal trends in use of mechanical ventilation and in-hospital mortality, we fit 2 analytical models. First, we developed an unadjusted model that included only calendar year as the independent variable. Second, we examined the independent association between calendar year and each outcome by using multivariable logistic regression. We adjusted for both patient-level variables (ie, age, gender, race/ethnicity, primary payer, admission day, and high-risk medical conditions) and hospital-level characteristics (region, urban and rural distinction, hospital teaching status, and children’s hospital designation).
To facilitate direct comparisons between years for hospital charges, we converted all charges to 2009 US dollars by using the medical care component of the Consumer Price Index.29 Because hospital charges were not normally distributed, we calculated the weighted geometric mean and median of charges.30 The geometric mean is the average of the logarithmic values of a data set, which is then converted back to a base-10 number; it is less influenced by extreme values than the arithmetic mean. We estimated total charges as a weighted sum of case-level charges. We performed linear regression for models of log-transformed charges to test temporal trends.
We then conducted a series of sensitivity analyses to assess the consistency of temporal trend in each primary outcome and in-hospital mortality among diagnostic subgroups. First, to minimize the potential misclassification of asthma, we repeated the analysis in cases with bronchiolitis as the primary diagnosis and in children <1 year of age. Second, we conducted the analysis excluding cases with high-risk medical conditions. Third, we repeated analytical models for cases with both primary diagnosis of bronchiolitis aged <1 year and no high-risk conditions. Two-sided P < .05 was considered statistically significant; all data were reported with 95% confidence intervals (CIs).
Results
Temporal Trends in Incidence of Bronchiolitis
We identified 325 494 patient discharges of bronchiolitis in the United States, corresponding to a weighted estimate of 544 828 discharges in the 4 data sets (2000, 2003, 2006, and 2009). This accounted for 16.2% (95% CI: 15.7%–16.6%) of all hospitalizations for children aged <2 years and 18.1% (95% CI: 17.5%–18.5%) for those <1 year after excluding all routine births.
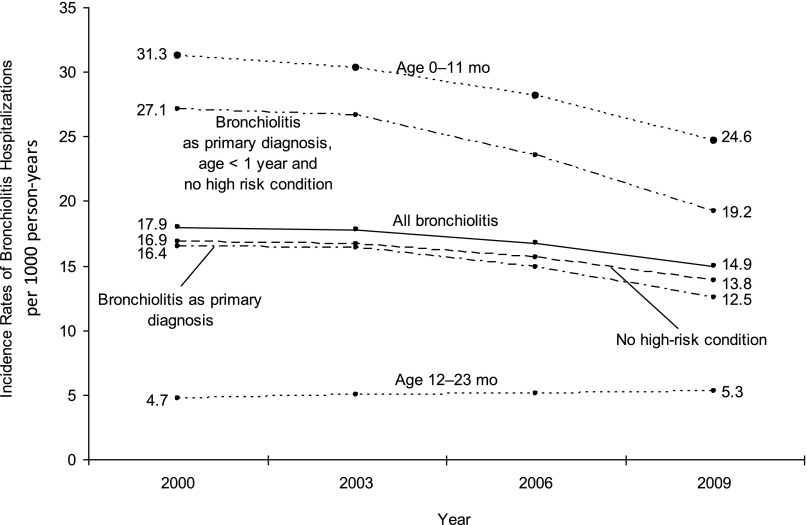
Between 2000 and 2009, the annual proportion of bronchiolitis hospitalizations among the total hospitalizations was relatively constant (Ptrend = .48; Table 1) for children aged <2 years and decreasing (5% decrease; Ptrend = .02) for those <1 year after excluding all routine births. Overall, there was a decrease in the incidence rate of bronchiolitis hospitalization, from 17.9 (95% CI: 16.9–19.1) to 14.9 (95% CI: 14.1–15.8) per 1000 person-years (17% decrease; Ptrend < .001; Fig 1). This finding was due largely to a decline in the incidence among infants (21% decrease; Ptrend < .001). Similarly, the decreasing temporal trends in bronchiolitis hospitalizations persisted across all subgroups (Ptrend < .001) except for children aged from 12 months to 23 months (13% increase; Ptrend < .001).
TABLE 1.
Patient and Hospital Characteristics of US Children <2 Years With Bronchiolitis, 2000–2009a
| Variables | 2000 | 2003 | 2006 | 2009 | P for Trend |
|---|---|---|---|---|---|
| Age 0–23.9 mo | |||||
| Weighted sample, n | 136 769 | 142 118 | 137 777 | 128 164 | |
| % of total hospitalizationsb | 16 (16–17) | 16 (16–17) | 16 (15–16) | 16 (16–17) | .48 |
| Age 0–11.9 mo | |||||
| Weighted sample, n | 118 910 | 121 411 | 116 200 | 104 985 | |
| % of total hospitalizationsc | 19 (18–19) | 18 (17–18) | 18 (17–18) | 18 (17–18) | .02 |
| Patient | |||||
| Age | <.001 | ||||
| 0–11.9 mo | 87 (84–86) | 86 (85–86) | 85 (84–85) | 82 (81–83) | |
| 12–23.9 mo | 13 (12–14) | 14 (14–15) | 15 (15–16) | 18 (17–19) | |
| Male gender | 59 (59–60) | 59 (59–60) | 58 (58–59) | 59 (58–59) | .03 |
| Race or ethnic group | |||||
| Non-Hispanic white | 42 (39–45) | 34 (32–36) | 35 (32–37) | 38 (36–41) | .05 |
| Non-Hispanic black | 13 (12–15) | 12 (11–13) | 11 (10–12) | 14 (12–16) | .57 |
| Hispanic | 21 (19–24) | 20 (18–23) | 22 (19–25) | 25 (22–27) | .01 |
| Other or unknown | 24 (21–26) | 34 (31–37) | 33 (29–36) | 23 (20–26) | .74 |
| Type of health insurance | |||||
| Public | 53 (51–55) | 57 (56–59) | 60 (58–61) | 63 (62–65) | <.001 |
| Private | 41 (39–43) | 37 (35–39) | 34 (33–38) | 31 (30–33) | <.001 |
| Other | 6 (6–7) | 6 (5–2) | 6 (5–7) | 6 (5–7) | .74 |
| Admission day | .001 | ||||
| Weekdayd | 78 (77–78) | 77 (77–78) | 77 (77–78) | 77 (76–77) | |
| Weekend | 22 (22–23) | 23 (22–23) | 22 (22–23) | 23 (23–24) | |
| Any high-risk conditione | 6 (5–6) | 6 (5–6) | 7 (6–7) | 8 (7–8) | <.001 |
| Hospital | |||||
| Region | |||||
| Northeast | 18 (15–22) | 16 (14–18) | 17 (15–20) | 18 (15–22) | .90 |
| Midwest | 18 (14–21) | 22 (19–25) | 23 (19–26) | 20 (17–24) | .15 |
| South | 40 (36–44) | 42 (38–45) | 39 (36–43) | 39 (35–44) | .06 |
| West | 24 (20–28) | 20 (17–24) | 21 (17–24) | 22 (19–26) | .28 |
| Location/teaching status | |||||
| Rural | 20 (18–23) | 20 (18–22) | 16 (15–18) | 17 (15–18) | .005 |
| Urban nonteaching | 31 (28–35) | 33 (30–36) | 31 (28–35) | 33 (29–36) | .82 |
| Urban teaching | 48 (44–52) | 47 (43–50) | 52 (49–56) | 51 (47–55) | .06 |
| Hospital designation | <.001 | ||||
| Non–children’s hospital | 72 (67–77) | 72 (70–76) | 65 (61–69) | 64 (59–68) | |
| Children’s hospital | 28 (23–33) | 28 (24–32) | 35 (31–40) | 36 (32–41) |
Data are expressed as % (95% CI) otherwise indicated.
Annual proportion of bronchiolitis hospitalizations among the total hospitalizations for children aged <2 y, after excluding routine birth.
Annual proportion of bronchiolitis hospitalizations among the total hospitalizations for children aged <1 y, after excluding routine birth.
Admission on Monday, Tuesday, Wednesday, Thursday, and Friday.
High-risk medical condition was defined as history of prematurity or ≥1 complex medical condition, previously defined by using ICD-9-CM codes in 9 categories of illness (ie, neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematology or immunologic, metabolic, malignancy, and other congenital or genetic defect disorders).
FIGURE 1.
Incidence rates of US bronchiolitis hospitalizations per 1000 children according to age group and different definitions, 2000–2009. Overall, there was a decrease in the incidence rate of bronchiolitis hospitalization (17% decrease; Ptrend < .001) between 2000 and 2009. Similarly, there was a decrease in the incidence rate in children aged <12 months (21% decrease; Ptrend < .001), cases with primary diagnosis of bronchiolitis aged <12 months without high-risk medical conditions (29% decrease; Ptrend < .001), cases with bronchiolitis as the primary diagnosis (18% decrease; Ptrend < .001), and cases with no high-risk medical conditions (24% decrease; Ptrend < .001). By contrast, the incidence rate among children from 12 months to 23 months increased (13% increase; Ptrend < .001).
To determine whether a shift in diagnostic preference could have played a role in the increase in bronchiolitis hospitalizations, pneumonia and asthma hospitalizations were examined. Between 2000 and 2009, the observed decline in overall bronchiolitis hospitalization rate was mirrored by decreases in that for pneumonia and asthma (all Ptrend < .001; Supplemental Fig 3).
Patient and Hospital Characteristics
The patient and hospital characteristics of the population of children with bronchiolitis in the four 1-year periods are shown in Table 1. Children with bronchiolitis in more recent years were less likely to be aged <1 year and male and more likely to have high-risk medical conditions (from 5.9% in 2000 to 7.9% in 2009; 34% increase; Ptrend < .001). Over the study period, patients with bronchiolitis also had a higher frequency of admission to children’s hospitals (27.7% in 2000 to 36.1% in 2009; 30% increase; Ptrend < .001).
Temporal Trends in Health Care Utilization and In-hospital Mortality
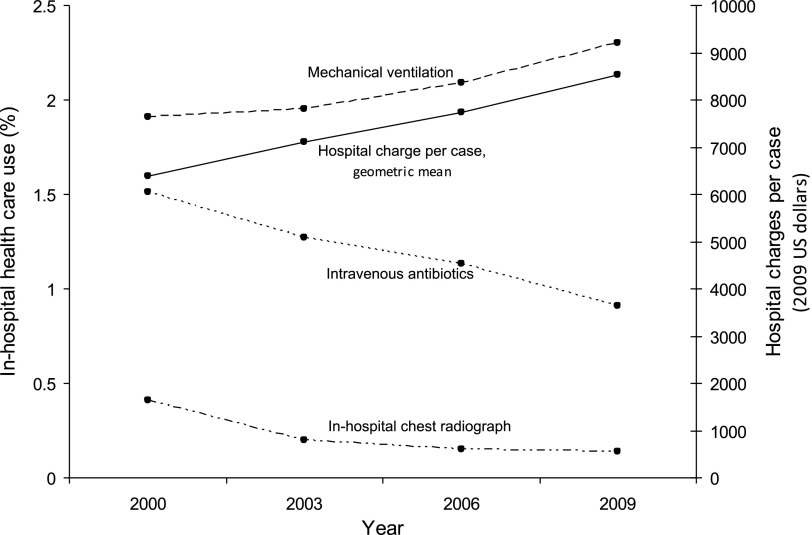
Between 2000 and 2009, the rate of children with bronchiolitis who underwent mechanical ventilation increased significantly from 1.9% in 2000 to 2.3% in 2009 (unadjusted odds ratio [OR] for comparison of 2009 with 2000, 1.21; 95% CI: 1.04–1.41; P = .01; Fig 2 and Supplemental Table 4). By contrast, the temporal trend became nonsignificant after adjustment for covariates (adjusted OR for comparison of 2009 with 2000, 0.98; 95% CI: 0.84–1.15; P = .92; Supplemental Table 5). Use of mechanical ventilation was associated with younger age (infant), white race, Medicaid or Medicare insurance, hospitalization during weekends, presence of high-risk medical conditions, and admission to urban hospitals and children’s hospitals. The in-hospital use of intravenous antibiotics and chest radiograph declined significantly over the study period (both Ptrend ≤ .01; Fig 2). The length of stay remained relatively unchanged for bronchiolitis during the study period, or, if anything, slightly decreased (2.5 days in 2000 and 2.4 days in 2009; Ptrend = .10).
FIGURE 2.
In-hospital health care utilization and hospital charges for US children with bronchiolitis, 2000–2009. Between 2000 and 2009, there was a significant decline in the use of intravenous antibiotics (40% decrease; Ptrend = .009) and chest radiograph (66% decrease; Ptrend = .010), whereas use of mechanical ventilation increased (21% increase; Ptrend = .008). The geometric mean of hospital charges per case increased significantly (34% increase; Ptrend < .001), adjusted for inflation.
Between 2000 to 2009, unadjusted in-hospital mortality did not change significantly (0.06% in 2000 to 0.03% in 2009; OR for comparison of 2009 with 2000, 0.56; 95% CI: 0.31–1.03; P = .06). In contrast, multivariable-adjusted mortality declined significantly (adjusted OR, 0.38; 95% CI: 0.20–0.72; P = .003; Table 2). Similarly, we observed a consistent, significant decline in adjusted mortality across all subgroups. For example, the adjusted OR for death in children <1 year of age, without high-risk conditions, and who had primary diagnosis of bronchiolitis was 0.25 (95% CI: 0.07–0.88; P = .003).
TABLE 2.
Multivariable OR of In-hospital Death in US Children With Bronchiolitis, According to Various Definitions, 2000–2009a
| Weighted Sample, n | Adjusted OR (95% CI) for In-hospital Mortality | ||||
|---|---|---|---|---|---|
| 2000 | 2003 | 2006 | 2009 | ||
| All bronchiolitis | 544 828 | 1.00 (reference) | 0.63 (0.36–1.10) | 0.56 (0.33–0.96) | 0.38 (0.20–0.72) |
| Sensitivity analyses | |||||
| Bronchiolitis as primary diagnosis | 485 656 | 1.00 (reference) | 0.53 (0.29–0.97) | 0.52 (0.30–0.91) | 0.31 (0.16–0.63) |
| Age <1 y | 461 506 | 1.00 (reference) | 0.68 (0.37–1.26) | 0.53 (0.28–1.00) | 0.37 (0.18–0.78) |
| No high-risk conditionb | 509 127 | 1.00 (reference) | 0.35 (0.13–0.96) | 0.31 (0.13–0.76) | 0.31 (0.11–0.84) |
| Bronchiolitis as primary diagnosis, age <1 y and no high-risk conditionb | 388 559 | 1.00 (reference) | 0.36 (0.12–1.05) | 0.16 (0.05–0.55) | 0.25 (0.07–0.88) |
Logistic regression adjusting for age, gender, race/ethnicity, primary payer, admission day (weekend versus weekday), comorbidities, US region, hospital location, teaching status, and children’s hospital designation.
High-risk medical condition was defined as history of prematurity or ≥1 complex medical condition, previously defined by using ICD-9-CM codes in 9 categories of illness (ie, neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematology or immunologic, metabolic, malignancy, and other congenital or genetic defect disorders).
Temporal Trends in Hospital Charges for Bronchiolitis
Between 2000 and 2009, the total hospital charges for bronchiolitis hospitalization were estimated to have increased from $1.34 billion (95% CI: $1.27–$1.41 billion) to $1.73 billion (95% CI: $1.64–$1.83 billion) nationally, adjusted for inflation (30% increase; Ptrend < .001). The geometric mean of hospital charges per case increased from $6380 (95% CI: $6140–$6630) to $8530 (95% CI: $8180–$8890; 34% increase; Ptrend < .001; Fig 2 and Supplemental Table 6).
In 2009, the total direct cost of the bronchiolitis hospitalization was $545 million (95% CI: $518–$573 million) nationally (Table 3). Children <1 year accounted for most of this annual cost. By contrast, children with bronchiolitis who underwent mechanical ventilation accounted for 2% of all bronchiolitis hospitalizations and 18% ($100 million, 95% CI: $91–$110 million) of the total annual cost.
TABLE 3.
Total Cost and Mean Cost for US Bronchiolitis Hospitalizations, According to Various Definitions, 2009
| Weighted Sample, n | Total Direct Cost (95% CI), $US (millions) | Cost Per Hospitalization, $US | ||
|---|---|---|---|---|
| Geometric mean (95% CI) | Median (IQR) | |||
| All bronchiolitis | 127 877 | 545 (518–573) | 2815 (2720–2910) | 2626 (1702–4298) |
| Sensitivity analyses | ||||
| Bronchiolitis as primary diagnosis | 106 476 | 444 (420–469) | 2756 (2658–2853) | 2575 (1672–4201) |
| Age <1 y | 105 011 | 463 (439–486) | 2868 (2766–2970) | 2667 (1719–4409) |
| No high-risk conditiona | 117 968 | 439 (420–457) | 2668 (2583–2753) | 2537 (1666–4058) |
| Bronchiolitis as primary diagnosis, age <1 y, no high-risk condition | 81 787 | 305 (291–319) | 2656 (2565–2747) | 2527 (1652–4065) |
| Stratification by use of MV | ||||
| Children without MV | 124 990 | 445 (427–463) | 2686 (2601–2771) | 2578 (1686–4140) |
| Children with MV | 2887 | 100 (91–110) | 21 323 (19 247–23 400) | 23 822 (11 598–40 426) |
IQR, interquartile range; MV, mechanical ventilation.
High-risk medical condition was defined as history of prematurity or ≥1 complex medical condition, previously defined by using ICD-9-CM codes in 9 categories of illness (ie, neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematology or immunologic, metabolic, malignancy, and other congenital or genetic defect disorders).
Discussion
By using a large, nationally representative database of US pediatric hospitalizations between 2000 and 2009, we found a significant decline in bronchiolitis hospitalization incidence and in-hospital mortality. Concurrent with these declines was a marked increase in use of noninvasive/invasive mechanical ventilation and hospital charges. Other notable temporal trends during this 10-year period included increasing comorbidity and more frequent hospitalization to children’s hospitals.
Previous studies reported increases in bronchiolitis hospitalizations through the 1990s in the United States1 and in the early 2000s within local populations.2,31 By contrast, between 2000 and 2009, we found a 17% decrease in the incidence of bronchiolitis hospitalizations nationally. The reasons for the reversal of the upward trend are unclear. The decrease in hospitalizations could reflect decreases in disease incidence and severity. Alternatively, nonbiological factors may have contributed, such as trends in child care practice or altered criteria for hospitalizations. In particular, one might surmise that physicians would have changed coding for hospitalizations attributable to lower respiratory tract illnesses. If diagnostic-coding variations during the study period substantially influenced the decrease in bronchiolitis hospitalization rate, we would expect a compensatory increase in hospitalization rates for other lower respiratory tract diseases with clinical representations similar to bronchiolitis. However, hospitalization rates for pneumonia and asthma also decreased between 2000 and 2009. Therefore, it is difficult to postulate that diagnostic substitution fully explains the decrease in bronchiolitis hospitalization rates.
We also demonstrated a more than twofold decrease in adjusted in-hospital mortality among US children with bronchiolitis; the mortality finding occurred despite an increase in children with high-risk medical conditions. The etiology of the mortality decline is probably multifactorial. The improvement in survival may have been driven by change in coding practice, with less severe cases of bronchiolitis being recognized and coded in more recent years. However, the incidence of bronchiolitis declined and the proportion of patients with comorbidity increased, both arguing against this possibility. The significant reductions in bronchiolitis mortality were large and persisted across various subgroups, including “classic bronchiolitis” (ie, primary diagnosis of bronchiolitis in infants without high-risk medical conditions), a finding that further supports the validity of these findings. The increase in the use of noninvasive and invasive mechanical ventilation raises the possibility that advanced respiratory support is being performed at an earlier phase on less critically ill patients with bronchiolitis,32 thereby leading to a reduction in observed mortality rates.
Previous studies that examined temporal trends in bronchiolitis-associated outcomes have reported a decline33 and no change in mortality.12 These studies were conducted in the 1990s and focused on bronchiolitis due to RSV infections, although approximately one-third of bronchiolitis hospitalizations are caused by other infectious agents.14 In contrast, our findings reflect outcomes of bronchiolitis as a clinical diagnosis from a large number of discharges drawn from most recent nationally representative samples. The observed temporal trend toward improved bronchiolitis-associated survival over time may be due to overall improvement in the quality of health care in US hospitals.34 Additionally, an increasing proportion of hospitalizations in children’s hospitals may reflect an improvement of regional systems of health care for critically ill children, similar to trauma care and neonatal intensive care, contributing to the decline in mortality through increased coordination of care.35,36
The apparent decrease in the incidence of hospitalization and in-hospital mortality contrasts sharply with our findings that national hospital charges related to bronchiolitis increased over time, even after adjusting for inflation. Despite the public health burden of bronchiolitis, there have been no recent studies examining temporal trends in hospital charges. By using broad definitions of bronchiolitis, previous studies estimated national hospital charges between $430 million and $690 million in 1998 US dollars,9 and $1.4 billion in 2002 US dollars.6 We observed a 30% increase in national charges from $1.3 billion in 2000 to $1.7 billion in 2009. This increase was driven by increases in the average hospital charge per case-day because the volume of hospitalizations declined and the length of stay remained constant (or slightly declined) during the study period. However, reasons for increasing hospital charges per case are likely multifactorial. The population of bronchiolitis may be similar in severity, but their inpatient use may be increasing. Alternatively, the prevalence of children with chronic medical conditions in the US population may be increasing.25 This potential mechanism may explain the noticeable rise in the proportion of bronchiolitis hospitalizations with high-risk medical conditions, thereby leading to more intensive resource use, such as noninvasive and invasive respiratory support. Indeed, the attenuation of the temporal trends in mechanical ventilation use after adjustment for high-risk medical conditions suggests an important contribution of this variable to more intensive resource use. Additionally, a lack of consensus among clinicians as to best practices suggested by a wide variation in diagnosis and management for bronchiolitis might, in part, contribute to this phenomenon.24,37,38
Although surveillance data are unable to explore more granular issues of clinical care, these results can better inform a system of care for children with severe bronchiolitis. At the population or health system level, our observation should facilitate studies that evaluate determinants of the rising hospital charges and seek better systems of care to achieve high-quality cost-effective health care to the largest number of sick children.39 At the individual patient level, evidence to guide the provision of optimal inpatient health care for children with bronchiolitis remains limited. High-quality research into the diagnosis, indications and outcomes of intensive management, and risk stratification, coupled with dissemination of these findings, could substantially improve care for children with bronchiolitis requiring hospitalization.
Our study has several potential limitations. First, we used an administrative database of discharge-level data, without clinical information beyond that captured in ICD-9-CM and CCS codes. We might have underestimated the frequency of bronchiolitis hospitalization and misdiagnosed with pneumonia, asthma, or febrile illness.24 However, we have conducted sensitivity analyses to address this issue, and the results did not materially change. Similarly, the observed in-hospital use of antibiotics and chest radiograph was lower than that of a previous study in children’s hospitals.38 This discrepancy can be attributed, at least in part, to the difference in patient population, potential undercoding of these process measures, and the absence of information in the KID database about health care utilization in emergency departments and clinics before the index hospitalization. Interestingly, we observed a significant decline in in-hospital use of antibiotics and chest radiographs over time despite an increasing use of electronic health record technology in the United States that likely would capture more information from hospitalizations. This observed decline warrants additional studies. Second, the KID contains discharge-level records and not patient-level records. Lack of patient identifiers precludes us from examining longer-term outcomes, such as readmissions. It is possible that a small proportion of patients might have been hospitalized multiple times in the same year. In this case, because mortality events are not recurrent, the number of deaths should not change. Third, as with any observational study, the observed decline in mortality might be confounded by unmeasured factors, such as favorable changes in parental smoking, household crowding, child care attendance, and immunoprophylaxis with palivizumab for children at high risk.40–42 Lastly, hospital billing practices might change over time, accounting for the reported increase in mechanical ventilation use and hospital charge for bronchiolitis.
Conclusions
By using a nationally representative database of US pediatric hospitalizations between 2000 and 2009, we found a significant decline in the incidence of bronchiolitis hospitalizations and mortality among children with bronchiolitis. In contrast to these declines, use of mechanical ventilation and hospital charges for bronchiolitis hospitalizations increased markedly. Although these data suggest a net improvement in severe bronchiolitis, continued efforts to evaluate its determinants and to standardize diagnosis and management may yield additional improvement in clinical outcomes. For policy makers, because bronchiolitis continues to be a public health burden in an already-stressed health care system, the rising hospital charges call for the development of more cost-effective approaches to the management of severe bronchiolitis.
Supplementary Material
Glossary
- CCS
Clinical Classifications Software
- CI
confidence interval
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- KID
Kids’ Inpatient Database
- OR
odds ratio
- RSV
respiratory syncytial virus
Footnotes
Dr Hasegawa conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted; Dr Tsugawa carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted; and Drs Brown, Mansbach, and Camargo conceptualized and designed the study, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Drs Hasegawa and Tsugawa were supported in part by St Luke’s Life Science Institute (Tokyo, Japan). Drs Mansbach and Camargo were supported in part by National Institutes of Health grant U01 AI-87881 (Bethesda, MD). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Funded by the National Institutes of Health (NIH).
References
- 1.Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980–1996. JAMA. 1999;282(15):1440–1446 [DOI] [PubMed] [Google Scholar]
- 2.Carroll KN, Gebretsadik T, Griffin MR, et al. Increasing burden and risk factors for bronchiolitis-related medical visits in infants enrolled in a state health care insurance plan. Pediatrics. 2008;122(1):58–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zorc JJ, Hall CB. Bronchiolitis: recent evidence on diagnosis and management. Pediatrics. 2010;125(2):342–349 [DOI] [PubMed] [Google Scholar]
- 4.Counihan ME, Shay DK, Holman RC, Lowther SA, Anderson LJ. Human parainfluenza virus-associated hospitalizations among children less than five years of age in the United States. Pediatr Infect Dis J. 2001;20(7):646–653 [DOI] [PubMed] [Google Scholar]
- 5.Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008;121(2):244–252 [DOI] [PubMed] [Google Scholar]
- 6.Pelletier AJ, Mansbach JM, Camargo CA, Jr. Direct medical costs of bronchiolitis hospitalizations in the United States. Pediatrics. 2006;118(6):2418–2423 [DOI] [PubMed] [Google Scholar]
- 7.Hall CB, Weinberg GA, Iwane MK, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360(6):588–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall G, McDonald L, Majowicz SE, et al. Respiratory symptoms and the case definition of gastroenteritis: an international analysis of the potential impact on burden estimates. Epidemiol Infect. 2010;138(1):117–124 [DOI] [PubMed] [Google Scholar]
- 9.Stang P, Brandenburg N, Carter B. The economic burden of respiratory syncytial virus-associated bronchiolitis hospitalizations. Arch Pediatr Adolesc Med. 2001;155(1):95–96 [DOI] [PubMed] [Google Scholar]
- 10.Leader S, Kohlhase K. Recent trends in severe respiratory syncytial virus (RSV) among US infants, 1997 to 2000. J Pediatr. 2003;143(suppl 5):S127–S132 [DOI] [PubMed] [Google Scholar]
- 11.Leader S, Kohlhase K. Respiratory syncytial virus-coded pediatric hospitalizations, 1997 to 1999. Pediatr Infect Dis J. 2002;21(7):629–632 [DOI] [PubMed] [Google Scholar]
- 12.Shay DK, Holman RC, Roosevelt GE, Clarke MJ, Anderson LJ. Bronchiolitis-associated mortality and estimates of respiratory syncytial virus-associated deaths among US children, 1979–1997. J Infect Dis. 2001;183(1):16–22 [DOI] [PubMed] [Google Scholar]
- 13.Stockman LJ, Curns AT, Anderson LJ, Fischer-Langley G. Respiratory syncytial virus-associated hospitalizations among infants and young children in the United States, 1997–2006. Pediatr Infect Dis J. 2012;31(1):5–9 [DOI] [PubMed] [Google Scholar]
- 14.Mansbach JM, Piedra PA, Teach SJ, et al. MARC-30 Investigators . Prospective multicenter study of viral etiology and hospital length of stay in children with severe bronchiolitis. Arch Pediatr Adolesc Med. 2012;166(8):700–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mansbach JM, McAdam AJ, Clark S, et al. Prospective multicenter study of the viral etiology of bronchiolitis in the emergency department. Acad Emerg Med. 2008;15(2):111–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Healthcare and Cost Utilization Project Kids’ Inpatient Database, 2000. Rockville, MD: Agency for Healthcare Research and Quality; 2003 [Google Scholar]
- 17.Healthcare and Cost Utilization Project. Kids’ Inpatient Database, 2003. Rockville, MD: Agency for Healthcare Research and Quality; 2005 [Google Scholar]
- 18.Healthcare and Cost Utilization Project. Kids’ Inpatient Database, 2006. Rockville, MD: Agency for Healthcare Research and Quality; 2008 [Google Scholar]
- 19.Healthcare and Cost Utilization Project. Kids’ Inpatient Database, 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2011 [Google Scholar]
- 20.Lee GE, Lorch SA, Sheffler-Collins S, Kronman MP, Shah SS. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126(2):204–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HUCP Kids’ Inpatient Database Comparison Report. Healthcare cost and utilization project. Rockville, MD: Agency for Healthcare Research and Quality. Available at: www.hcup-us.ahrq.gov/db/nation/kid/kidrelatedreports.jsp. Accessed January 15, 2013
- 23.Related Reports KID. Healthcare cost and utilization project. Rockville, MD: Agency for Healthcare Research and Quality. Available at: www.hcup-us.ahrq.gov/kidoverview.jsp. Accessed January 15, 2013
- 24.Mansbach JM, Espinola JA, Macias CG, Ruhlen ME, Sullivan AF, Camargo CA, Jr. Variability in the diagnostic labeling of nonbacterial lower respiratory tract infections: a multicenter study of children who presented to the emergency department. Pediatrics. 2009;123(4). Available at: www.pediatrics.org/cgi/content/full/123/4/e573 [DOI] [PubMed] [Google Scholar]
- 25.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6). Available at: www.pediatrics.org/cgi/content/full/107/6/e99 [DOI] [PubMed] [Google Scholar]
- 26.United States Bureau of the Census. Census regions and divisions of the United States. Available at: www.census.gov/geo/www/us_regdiv.pdf. Accessed January 15, 2013
- 27.The National Association of Children’s Hospitals and Related Institutions Classification Criteria. Available at: www.childrenshospitals.net. Accessed January 15, 2013
- 28.US Census Bereau. Population estimates. Available at: www.census.gov/popest/. Accessed January 15, 2013
- 29.Consumer Price Index. US Department of Labor, Bureau of Labor Statistics. Available at: www.bls.gov/cpi/home.htm. Accessed January 15, 2013
- 30.Lagu T, Rothberg MB, Shieh MS, Pekow PS, Steingrub JS, Lindenauer PK. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2012;40(3):754–761 [DOI] [PubMed] [Google Scholar]
- 31.García CG, Bhore R, Soriano-Fallas A, et al. Risk factors in children hospitalized with RSV bronchiolitis versus non-RSV bronchiolitis. Pediatrics. 2010;126(6). Available at: www.pediatrics.org/cgi/content/full/126/6/e1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ganu SS, Gautam A, Wilkins B, Egan J. Increase in use of non-invasive ventilation for infants with severe bronchiolitis is associated with decline in intubation rates over a decade. Intensive Care Med. 2012;38(7):1177–1183 [DOI] [PubMed] [Google Scholar]
- 33.Panickar JR, Dodd SR, Smyth RL, Couriel JM. Trends in deaths from respiratory illness in children in England and Wales from 1968 to 2000. Thorax. 2005;60(12):1035–1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams SC, Schmaltz SP, Morton DJ, Koss RG, Loeb JM. Quality of care in U.S. hospitals as reflected by standardized measures, 2002–2004. N Engl J Med. 2005;353(3):255–264 [DOI] [PubMed] [Google Scholar]
- 35.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283(15):1990–1994 [DOI] [PubMed] [Google Scholar]
- 36.Rautava L, Lehtonen L, Peltola M, et al. PERFECT Preterm Infant Study Group . The effect of birth in secondary- or tertiary-level hospitals in Finland on mortality in very preterm infants: a birth-register study. Pediatrics. 2007;119(1). Available at: www.pediatrics.org/cgi/content/full/119/1/e257 [DOI] [PubMed] [Google Scholar]
- 37.Mansbach JM, Emond JA, Camargo CA, Jr. Bronchiolitis in US emergency departments 1992 to 2000: epidemiology and practice variation. Pediatr Emerg Care. 2005;21(4):242–247 [DOI] [PubMed] [Google Scholar]
- 38.Christakis DA, Cowan CA, Garrison MM, Molteni R, Marcuse E, Zerr DM. Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics. 2005;115(4):878–884 [DOI] [PubMed] [Google Scholar]
- 39.Lorch SA, Myers S, Carr B. The regionalization of pediatric health care. Pediatrics. 2010;126(6):1182–1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McConnochie KM, Roghmann KJ. Parental smoking, presence of older siblings, and family history of asthma increase risk of bronchiolitis. Am J Dis Child. 1986;140(8):806–812 [DOI] [PubMed] [Google Scholar]
- 41.The IMpact-RSV Study Group . Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. The IMpact-RSV Study Group. Pediatrics. 1998;102(3 pt 1):531–537 [PubMed] [Google Scholar]
- 42.Mansbach JM, Piedra PA, Stevenson MD, et al. MARC-30 Investigators . Prospective multicenter study of children with bronchiolitis requiring mechanical ventilation. Pediatrics. 2012;130(3). Available at: www.pediatrics.org/cgi/content/full/130/3/e492 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.