Abstract
OBJECTIVE:
Executive dysfunction after traumatic brain injury (TBI) in children is common and leads to significant problems in functioning across multiple settings. The objective of this study was to evaluate the efficacy of a web-based counselor-assisted problem solving (CAPS) intervention compared with an Internet resource comparison (IRC) for treatment of executive dysfunction within 12 months after complicated mild to severe TBI in adolescents. We hypothesized that CAPS would significantly improve parent ratings of executive dysfunction compared with an IRC.
METHODS:
Participants included 132 adolescents aged 12 to 17 years who sustained a complicated mild to severe TBI within 1 to 6 months before study enrollment. Study design was a multisite, assessor-blinded, randomized controlled trial. Study sites included 3 tertiary pediatric hospitals and 2 tertiary general medical centers. The main outcome measure was primary caregiver Behavioral Rating Inventory of Executive Function Global Executive Composite at baseline and 6-month follow-up. Generalized linear models that controlled for baseline scores were used to compare the CAPS and IRC scores.
RESULTS:
In older teens, the CAPS group showed significant improvement in executive function behaviors at 6-month follow-up compared with the IRC group (F = 6.74, P = .01, Cohen’s d = 0.63).
CONCLUSIONS:
Findings indicate that web-based CAPS improves primary caregiver-rated executive functioning within the first 12 months after TBI in older adolescents. Future research needs to define the optimal timing after injury for delivery of CAPS and characteristics of individuals and families who are most likely to benefit from CAPS.
Keywords: brain injury, online, therapy, executive function, child, adolescent
What’s Known on This Subject:
Cognitive and behavioral problems after pediatric traumatic brain injury lead to poor functioning across multiple settings and can persist long-term after injury. Executive dysfunction is particularly common; however, there is a paucity of evidence-based interventions to guide treatment.
What This Study Adds:
This study is among the largest randomized controlled trials performed in pediatric traumatic brain injury. It demonstrates the ability to use an online problem-solving-based intervention to improve caregiver ratings of executive dysfunction within 12 months after injury.
Traumatic brain injury (TBI) is a worldwide heath problem and is among the most common causes of acquired morbidity and mortality in children.1–5 TBI results in 2685 deaths, 37 000 hospitalizations, and 435 000 emergency department visits in children yearly in the United States.4,5 Because these injuries can occur at an early age, they can have lifelong impact. Neurocognitive and behavioral problems are common after TBI in children and lead to significant problems in functioning across multiple settings.6–13 In particular, executive dysfunction after pediatric TBI is associated with functional problems across home, school, and community settings both in the short- and long-term after injury.6–10,14–20 Better treatment of executive dysfunction after injury may lead to improved functioning in everyday settings.21
Problem-solving training has demonstrated promise in various clinical populations22–26; however, it has only been preliminarily explored in pediatric TBI.27–34 In a small randomized trial of children aged 5 to 17 years (N = 32), findings showed that family-centered online problem-solving therapy improved internalizing behavioral problems after severe TBI.32 Initial evidence suggests that problem-solving interventions can also be delivered effectively through a web-based portal directly to children with TBI.35 In a small randomized-controlled trial of adolescents aged 11 to 18 years (n = 35), teen-directed online problem-solving improved both parent- and self-reported behavioral problems33 but only improved self-ratings, not parent-ratings, of executive dysfunction.34 These studies have been limited by small sample sizes and heterogeneous populations.
The current study sought to build on this previous research and evaluate the efficacy of a web-based counselor-assisted problem solving (CAPS) intervention compared with an Internet resource comparison (IRC) group for treatment of executive dysfunction within the first year after complicated mild to severe TBI in adolescents. Because CAPS provides training to teens and their families to improve problem solving and self-regulation, we hypothesized that CAPS would improve adolescent executive function as rated by parents 6 months after initiation of the intervention. In agreement with Wade et al,36 we hypothesized that CAPS would be most effective in older adolescents. This study expands on previous work and evaluates the efficacy of an online problem solving intervention in a carefully controlled trial with a large (N = 132) sample of adolescents after TBI.
Methods
Subjects
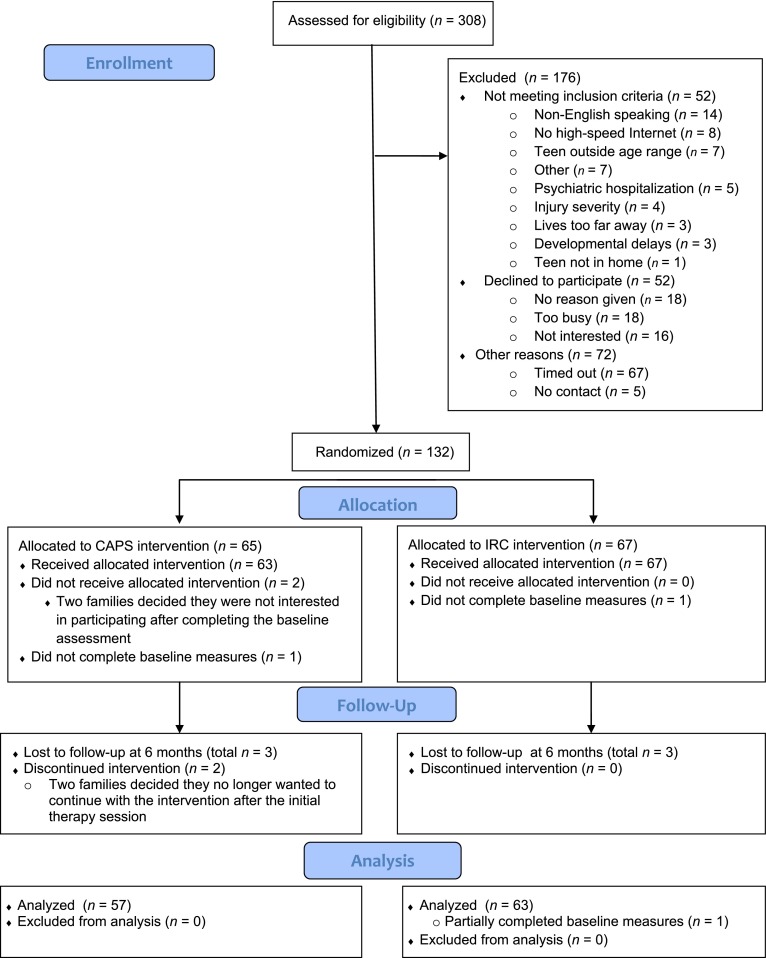
Participants included adolescents aged 12 to 17 years of age who sustained a complicated mild to severe TBI. Complicated mild TBI was defined as Glasgow Coma Scale (GCS) score >12 with evidence of a neurologic insult on MRI or computerized tomography (CT), moderate TBI as GCS score of 9 to 12, and severe TBI defined as GCS score <9.37–39 GCS was used primarily as the measure of injury severity because it was the most consistently obtained clinical variable across multiple sites at the time of participant enrollment. CT scans performed acutely were not used as a marker of severity because CTs are not particularly more predictive of cognitive and behavioral outcomes than GCS or other clinical factors in the subacute period.37,40,41 Exclusion criteria included nonblunt trauma, primary language other than English, history of significant intellectual disability before injury, history of child abuse, insufficient recovery to allow participation in the study, history of parental or child psychiatric hospitalization within 1 year before enrollment, family residence in an area without high-speed Internet access, or child residence outside the home (eg, detention facility). Because baseline assessments and a computer installation and orientation visit were performed in the participants’ homes, participants were also excluded if they resided >3 hours from the study site. Participants were enrolled 1 to 6 months after initial injury. Recruitment was conducted from March 2007 through January 2011. Study sites included 3 tertiary pediatric hospitals and 2 tertiary general medical centers across 4 cities: Cincinnati, OH; Denver, CO; Cleveland, OH; and Rochester, MN. Institutional review board approval was obtained from all participating institutions, and the study was registered with clinicaltrials.gov (identifier: NCT00409448). Three hundred eight participants were assessed for eligibility: 52 did not meet inclusion criteria, 52 declined to participate, 72 timed out of the eligibility period, and 5 were unable to be contacted (see Fig 1). There were no differences between participants and nonparticipants in age: mean (SD) = 14.54 (1.74) for participants and 14.68 (1.74) for nonparticipants. Nonparticipants were significantly more likely to be nonwhite (24.4% vs 19.7%, respectively) and to have less severe TBI as measured by the GCS: mean (SD) = 11.90 (3.89) vs 10.03 (4.56).
FIGURE 1.
CAPS CONSORT Flow Diagram.
Design
Multisite, evaluator-blinded, randomized controlled trial that was conducted according to the Consolidated Standards or Reporting Trials guidelines. Participants were randomly assigned to either CAPS or IRC. Assuming a significance of .05, a priori sample size calculations using analysis of variance methodology for repeated measures determined that 60 per group were required to find an effect size of 0.30 with 84% power. Randomization was carried out by stratifying by both gender and race to ensure these 2 factors were balanced within the sites. An SAS program was created using permuted block sizes for each of the randomizations. A sealed envelope containing group assignment was handed to the participants at the end of the baseline visit. Group assignment was concealed from the research coordinators. All families were provided with a new computer, web camera, and high-speed Internet access, and shown how to log on to the study web site and access the links to TBI resources on the web.
CAPS Intervention
CAPS36 consisted of a 6-month counselor-assisted, web-based, family-centered intervention that focused on problem solving, communication, and self-regulation. During the initial face-to-face session in the family’s home, the psychologist performed his or her evaluation and instructed the family on how to access available treatment modules on the CAPS web site and log on to Skype for subsequent videoconference sessions. The subsequent sessions were completed initially weekly then biweekly for the first 3 months for a total of 6 sessions and consisted of self-guided didactic content regarding problems-solving skills, video clips modeling these skills, and exercises to practice the skills. During these sessions, the therapist reviewed the online materials and practiced problem-solving skills using problems that the family identified. During months 4 and 5 of CAPS, families with persistent concerns could complete up to 4 supplemental sessions. In the seventh online session, all participating parents completed a measure of family burden and a self-assessment of problem solving and communication. On the basis of the results of the self-assessment, the therapist planned individualized sessions for the family with ongoing attention given to injury-related issues that were identified on the questionnaires. Up to four additional supplemental sessions could be provided to address additional unresolved issues. All families were scheduled for a final session with the therapist in the sixth month. Content of the core and supplemental CAPS sessions is listed in Table 1.
TABLE 1.
CAPS Core and Supplemental Session
| Core sessions |
| 1. Getting Started |
| Implementation and Monitoring |
| Goals |
| 2. Staying Positive |
| 3. Problem Solving |
| 4. Getting Organized and Working With the School |
| 5. Self-management |
| 6. Verbal and Nonverbal Communication |
| 7. Controlling Your Behavior II/Handling Crises |
| Self-Assessment of Skills |
| Identification of Supplemental Sessions |
| 8. Planning for the Future |
| Supplemental sessions (up to 4 per family) |
| Talking With Your Teen |
| Taking Care of You/Marital Communication/Guilt, Grief, and Caregiver |
| Social Skills |
| After High School |
| Sibling Issues |
| Pain Management |
| Sleep Session |
| Memory Session |
IRC Intervention
Families in the IRC36 group also received a computer, web camera, and high-speed Internet access. The web camera was provided to keep the research assistants unaware of group assignment. IRC group received access to a home page with links to online resources. Resources included links to local, state, and national brain-injury associations and to sites specific to pediatric brain injury, such as the Center on Brain Injury Research and Training, Brain Injury Partners and the National Database of Educational Resources on Traumatic Brain Injury. These web sites provided didactic information about brain injury as well as modules about working with schools,42 handling stress, and problem solving around common issues. Families were encouraged to spend at least 1 hour each week accessing information regarding pediatric brain injury on the web throughout the 6-month intervention period and to track the sites that they visited. At follow-up, parents provided information about the TBI-related web sites visited and the time spent at each site. The IRC group did not have access to specific session content provided to the CAPS group.
Follow-up Assessment
A follow-up assessment was completed an average of 6 months after baseline at participants’ homes for both groups and included the same assessments that were completed at baseline. To equate the time between baseline and follow-up assessments between groups and maintain concealment of group assignment, follow-ups were performed without knowledge of group.
Background Questionnaire
Information regarding injury severity was collected from relevant hospital records. Sociodemographic information was collected from the caregiver at the baseline assessment. Parents and primary caregivers completed a baseline interview regarding preinjury diagnoses and treatments, as well as current behavioral and medical treatments.
Outcome Measures
Measures were collected during home visits by trained research coordinators. Baseline measures were collected before treatment group assignment. The Behavior Rating Inventory of Executive Function (BRIEF) was completed by the participant’s family-identified primary caregiver to assess executive function.43–47 The BRIEF has good internal consistency and interrater reliability, and test-retest reliability and has been validated in pediatric TBI.43,47 The BRIEF provides an assessment of executive function in everyday settings and demonstrates good ecological validity.43 The Global Executive Composite (GEC) is a composite of the Behavioral Regulation Index (BRI) and the Metacognition Index (MI) and was used as the primary outcome measure to assess overall executive function. The BRI provides ratings of a child’s ability to appropriately stop his or her own behavior, move freely from one situation to another, and modulate emotional responses appropriately.46 The MI provides ratings of a child’s ability to hold information in mind to complete a task, anticipate future events, carry out tasks in a systematic manner, keep workspace or play areas orderly, assess performance related to goal, and keep track of the effect of his or her behavior on others.46 The BRI and MI are subdivided into specific subscales: BRI subscales are Inhibit, Shift, Emotional Control, and MI subscales are Initiate, Working Memory, Plan/Organization, Organization of Materials, and Monitor. Higher scores indicate more problems in executive function, with a score of 65 or greater indicating significant executive dysfunction.45,46
Analysis
χ2 and t tests were used to compare demographic variables between the IRC and CAPS groups. General linear models (SAS Enterprise Guide 5.1, GLM procedure), which controlled for baseline BRIEF scores (covariate), were used to evaluate for significant differences at follow-up (dependent variable) between the CAPS and IRC groups (independent variable). For the primary outcome (GEC), significance was defined as P < .05. Similar to Wade et al,36 analyses were done for the entire sample and then subdivided into 2 groups: older teens (9th–12th grade) and younger teens (6th–8th grade). Cohen’s d was calculated to determine the effect size of the intervention using G*power 3.1.3.48 Cohen’s d values were interpreted by using the following criteria: 0.2 to 0.49 for a small effect, 0.50 to 0.79 for a medium effect, and ≥0.80 for large effects.49 Secondary analyses that included the BRI, MI, and associated subscales were also performed to elucidate which components of executive function preferentially responded to the intervention. Because the BRI and MI represent 2 distinct constructs of executive function, a corrected P value of .025 (0.05/2) was used to identify associations for response on the BRI, MI, and associated subscales. Strict multiple correction was not performed for the associated subscales because these analyses were exploratory in nature. All analyses were performed with intention to treat.
Results
Participants and Demographics
Baseline demographic characteristics were not different between the IRC and CAPS group (Table 2). Baseline GEC and BRI scores were not different between groups, but MI scores were higher in the IRC group (Table 2). Baseline Plan/Organize and Organization of Materials MI subscale scores were higher in the IRC group (Table 2). One hundred thirty-two participants were randomized to CAPS (n = 65) or IRC (n = 67). In the CAPS group, 2 families dropped out after baseline assessment, 1 did not complete baseline assessments, 2 dropped out after the initial therapy visit, and 3 were lost to follow-up at the 6-month assessment (Fig 1). In the IRC group, 1 participant did not complete the baseline measure, and 3 were lost to follow-up (Fig 1). In the final analysis, 57 participants were included in the CAPS group and 63 in the IRC group. The mean number of sessions completed in the CAPS group was 7.23 (SD: 2.99, range: 0–13). Parent and self-reported time spent viewing information on the web did not differ between groups (data not shown).
TABLE 2.
Baseline Demographic and Injury Characteristics by Treatment Group
| Entire Sample | IRC (n = 67) | CAPS (n = 65) | t/χ2 |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Age at injury (y) | 14.67 (1.77) | 14.40 (1.68) | 0.91 |
| n (%) male | 42 (63%) | 44 (68%) | 0.36 |
| Time since injury (y) | |||
| Baseline | 0.29 (0.14) | 0.30 (0.16) | 0.59 |
| 6-mo follow-up | 0.79 (0.14) | 0.80 (0.16) | 0.59 |
| Current grade | 8.94 (1.77) | 8.69 (1.75) | 0.81 |
| n (%) Nonwhite | 13 (20%) | 13 (20%) | 0.01 |
| Lowest GCS score | 10.03 (4.33) | 10.08 (4.85) | 0.06 |
| n (%)severe TBI | 41 (61%) | 40 (62%) | 0.00 |
| Median income | $65 912 (22.84) | $71 325 (32.19) | 1.11 |
| BRIEF GEC | 61.65 (10.51) | 58.61 (10.10) | 1.67 |
| BRIEF BRI | 59.06 (12.05) | 57.78 (11.11) | 0.63 |
| Inhibit | 60.12 (13.58) | 57.25 (12.40) | 1.25 |
| Shift | 56.00 (11.87) | 56.06 (10.89) | 0.03 |
| Emotional Control | 57.26 (11.11) | 57.48 (11.28) | 0.12 |
| BRIEF MI | 62.00 (9.91) | 58.03 (9.54) | 2.32a |
| Initiate | 58.33 (8.77) | 56.42 (9.94) | 1.16 |
| Working Memory | 63.53 (12.82) | 60.17 (11.34) | 1.58 |
| Plan/Organize | 60.47 (10.77) | 56.25 (10.67) | 2.25a |
| Organization of Materials | 58.64 (8.47) | 52.86 (9.19) | 3.73 |
| Monitor | 60.22 (9.63) | 58.91 (10.51) | 1.19 |
P < .05.
Primary Outcome
The CAPS and IRC groups did not differ significantly on the GEC at the follow-up assessment (Table 2). However, in older teens (9th–12th grade), the CAPS group showed significant improvement at follow-up on the GEC compared with the IRC group (Table 3), which corresponded to a Cohen’s d value of 0.63. In younger teens (6th–8th grade), no significant differences were found between CAPS and IRC groups at follow-up (Table 3).
TABLE 3.
Improvements From Baseline to Follow-up on the GEC in the CAPS Versus IRC Treatments in the Entire Sample Older Teens (9th–12th Grade) and Younger Teens (6th–8th Grade)
| CAPS (n = 57) | IRC (n = 62a) | F (df) | Pb | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||||
| Baseline | 6 month | Change | Baseline | 6 month | Change | |||
| Entire sample | 58.61 (10.10) | 56.81 (11.40) | −1.53 (8.75) | 61.65 (10.51) | 60.38 (12.05) | −1.40 (7.43) | 0.17 (118) | .68 |
| Older teens | 60.65 (10.46) | 55.04 (11.36) | −4.78 (6.66) | 61.59 (10.69) | 61.03 (10.77) | −0.86 (5.98) | 6.74 (61) | .01 |
| Younger teens | 56.70 (9.50) | 58.47 (11.37) | 1.40 (9.46) | 61.71 (10.46) | 59.48 (13.77) | −2.11 (9.06) | 1.27 (56) | .27 |
The total study participants for IRC was 63. However, 1 participant did not complete the BRIEF BRI Inhibit subscale; thus the GEC could not be calculated, and this participant was excluded from this analysis.
P values apply to differences between CAPS and IRC groups as measured by general linear models after controlling for baseline scores.
Secondary and Exploratory Analyses
In the entire sample, there were no differences between the CAPS and IRC group on the BRI, MI, or subscales of executive function at follow-up (Table 4). In older teens, there was improvement on the BRI composite and the Emotional Control BRI subscale, whereas the Inhibit and Shift BRI subscales trended toward significant improvement in the CAPS grouped compared with IRC at follow-up (Table 4). In older teens, there was also improvement on the Working Memory and Monitor subscales of the MI, whereas the composite MI score showed a trend toward improvement in the CAPS group compared with IRC (Table 4). In younger teens, there was no improvement in the CAPS compared with the IRC group on the BRI, MI, or subscales (Table 4).
TABLE 4.
Improvements from Baseline to Follow-up on the BRIEF Subscales in the CAPS Versus IRC Treatments in the Entire Sample, Older Teens (9th–12th grade), and Younger Teens (6th–8th Grade)
| Measure | CAPS (n = 57) | IRC (n = 63) | F (df) | Pa | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||||
| Baseline | 6 Month | Change | Baseline | 6 Month | Change | |||
| Entire sample | ||||||||
| BRIEF BRI | 57.78 (11.11) | 56.07 (13.33) | −1.25 (9.38) | 59.06 (12.05) | 58.55 (10.51) | −0.29 (8.46) | 0.50 (118b) | .48 |
| Inhibit | 57.25 (12.40) | 55.91 (14.35) | −0.46 (11.46) | 60.12 (13.58) | 60.30 (14.05) | −0.34 (8.32) | 0.61 (118b) | .44 |
| Shift | 56.06 (10.89) | 54.78 (11.79) | −1.75 (10.12) | 56.00 (11.87) | 55.34 (11.79) | −0.49 (10.40) | 0.30 (119) | .59 |
| Emotional Control | 57.48 (11.30) | 55.31 (12.22) | −1.68 (9.29) | 57.26 (11.11) | 57.52 (12.16) | 0.60 (9.27) | 1.85 (119) | .18 |
| BRIEF MI | 58.03 (9.54) | 56.48 (10.02) | −1.37 (8.06) | 62.00 (9.91) | 60.20 (11.36) | −1.92 (6.98) | 0.03 (119) | .87 |
| Initiate | 56.42 (9.94) | 54.90 (9.88) | −1.74 (10.36) | 58.33 (8.77) | 57.48 (10.88) | 0.89 (9.14) | 0.91 (119) | .34 |
| Working Memory | 60.17 (11.34) | 59.76 (12.01) | −0.33 (9.24) | 63.53 (12.82) | 63.11 (13.97) | −0.67 (9.87) | 0.08 (119) | .77 |
| Plan/Organize | 56.25 (10.67) | 55.14 (10.36) | −0.60 (8.52) | 60.47 (10.76) | 58.67 (11.72) | −1.79 (7.50) | 0.01 (119) | .93 |
| Organization of Materials | 52.86 (9.19) | 53.17 (9.58) | −0.18 (6.82) | 58.64 (8.47) | 55.53 (10.13) | −3.19 (8.15) | 1.62 (119) | .21 |
| Monitor | 58.91 (10.51) | 54.48 (10.15) | −3.81 (10.94) | 60.23 (9.63) | 58.36 (10.64) | −1.92 (8.62) | 2.63 (119) | .12 |
| Older teens | ||||||||
| BRIEF BRI | 59.00 (10.78) | 52.82 (11.73) | −5.00 (7.61) | 59.19 (11.45) | 58.70 (10.39) | −0.26 (7.51) | 6.95 (61b) | .01** |
| Inhibit | 57.26 (11.97) | 52.32 (11.27) | −3.63 (8.95) | 59.14 (13.22) | 59.62 (12.83) | 0.43 (8.75) | 5.01 (61b) | .03* |
| Shift | 57.81 (10.60) | 51.79 (10.50) | −5.89 (9.20) | 57.32 (11.90) | 56.22 (10.77) | −0.64 (9.40) | 5.30 (62) | .03* |
| Emotional Control | 58.32 (10.79) | 53.14 (11.37) | −3.74 (8.34) | 57.74 (9.58) | 58.97 (9.57) | 1.75 (7.84) | 7.91 (62) | .007** |
| BRIEF MI | 60.74 (10.65) | 55.82 (10.83) | −4.33 (6.15) | 62.03 (10.35) | 60.89 (10.44) | −1.39 (5.44) | 5.04 (62) | .03* |
| Initiate | 58.39 (10.57) | 54.11 (10.35) | −4.41 (7.94) | 58.13 (9.24) | 56.78 (9.98) | −1.53 (7.03) | 2.51 (62) | .12 |
| Working Memory | 64.55 (11.38) | 58.86 (12.17) | −5.19 (6.91) | 63.32 (13.42) | 64.62 (12.79) | 0.97 (8.40) | 10.25 (62) | .002** |
| Plan/Organize | 58.29 (11.84) | 55.07 (10.99) | −2.22 (7.61) | 60.26 (11.40) | 58.62 (10.74) | −1.75 (7.06) | 0.44 (62) | .51 |
| Organization of Materials | 53.16 (1.053) | 52.21 (10.44) | −1.63 (5.72) | 59.24 (8.90) | 56.89 (9.41) | −2.61 (6.97) | 0.00 (62) | .95 |
| Monitor | 60.12 (10.31) | 53.04 (10.29) | −6.37 (8.54) | 60.21 (9.72) | 59.27 (10.77) | −0.92 (8.62) | 7.13 (62) | .01** |
| Younger teens | ||||||||
| BRIEF BRI | 56.63 (11.46) | 59.10 (14.19) | 2.13 (9.64) | 58.89 (13.03) | 58.33 (15.77) | −0.33 (9.71) | 0.81 (56) | .37 |
| Inhibit | 57.24 (12.99) | 59.27 (16.19) | 2.40 (12.81) | 61.43 (14.17) | 61.22 (15.79) | 0.22 (7.90) | 0.34 (56) | .57 |
| Shift | 54.42 (11.06) | 57.57 (12.41) | 1.97 (9.60) | 54.21 (11.81) | 54.15 (13.19) | −0.30 (11.78) | 0.94 (56) | .34 |
| Emotional Control | 56.70 (11.83) | 57.33 (12.82) | 0.17 (9.83) | 56.61 (13.05) | 55.52 (14.97) | −0.93 (10.86) | 0.23 (56) | .64 |
| BRIEF MI | 55.48 (7.69) | 57.10 (9.34) | 1.30 (8.71) | 61.96 (9.47) | 59.26 (12.64) | −2.63 (8.69) | 1.26 (56) | .26 |
| Initiate | 54.58 (9.09) | 55.63 (9.54) | 0.67 (11.75) | 58.61 (8.24) | 58.44 (12.14) | −0.04 (11.47) | 0.27 (56) | .61 |
| Working Memory | 56.06 (9.79) | 60.60 (12.01) | 4.03 (8.96) | 63.82 (12.20) | 61.04 (15.44) | −2.85 (11.34) | 4.11 (56) | .05 |
| Plan/Organize | 54.33 (9.21) | 55.20 (9.92) | 0.87 (9.14) | 60.75 (10.01) | 58.74 (13.16) | −1.85 (8.17) | 0.39 (56) | .54 |
| Organization of Materials | 52.58 (7.89) | 54.07 (8.79) | 1.13 (7.53) | 57.82 (7.94) | 53.67 (10.95) | −3.96 (9.59) | 2.52 (56) | .12 |
| Monitor | 57.30 (10.59) | 55.83 (10.00) | −1.50 (12.41) | 60.25 (9.69) | 57.11 (10.53) | −3.26 (8.60) | 0.00 (56) | .98 |
P < .05; ** P < .025.
P values apply to differences between CAPS and IRC groups as measured by general linear models after controlling for baseline scores.
One participant did not complete the BRIEF-BRI Inhibit subscale in the older IRC group and thus was excluded from analysis.
Adverse Events
There were no reported adverse events in IRC or CAPS groups.
Discussion
The findings from this study demonstrate the ability of online problem solving to improve executive function behaviors, as rated by primary caregivers, within the first year after complicated mild to severe TBI in older adolescents compared with individuals who received web-based information only. The intervention was most successful for adolescents who were in grades 9 to 12, and the overall effect size was medium in magnitude. This is one of the largest randomized controlled studies to demonstrate positive effects in reducing problems in executive function after adolescent TBI. It is an important contribution to the paucity of evidence-based interventions available for management of cognitive and behavioral sequelae of pediatric TBI.
Our results expand on previous studies that evaluated the feasibility and efficacy of online problem-solving interventions after pediatric TBI.32–35,50 In a large randomized controlled trial, we documented improvements on ratings of global executive functioning in older but not younger adolescents. On further analysis, it appears that older teens improved in both behavioral regulation and metacognitive aspects of executive functioning. The emotional control component contributed to improvement in behavioral regulation, whereas the working memory and monitoring components contributed to metacognition improvement. The improvement in working memory is of particular interest in view of a previous report of poorer working memory in children with TBI compared with controls at 3 and 12 months after injury, indicating a special vulnerability of this skill to the effects of injury.7 Future research will need to evaluate the longitudinal effects of an early intervention on long-term outcomes related to executive function.
The finding of positive effects of CAPS on executive functioning of older adolescents is similar to results obtained by Wade et al for parent ratings of externalizing behavior.36 Older adolescents may be developmentally more capable of using this training than younger adolescents, which may explain the differential effect. Alternative interventions that are beneficial to younger adolescents need to be explored in the future.
Our findings also contribute further to the telehealth literature by demonstrating the ability to use online counselor assisted therapy in the pediatric TBI population. Children with TBI often have unmet health and behavioral needs,51 and web-based technology may provide easier access to these services. The rapidly increasing use of web-based and telehealth technology in medicine would allow delivery of the CAPS intervention on a wide scale. Implementation studies should be considered in the future to determine the ability to integrate CAPS into standard clinical practice. Because executive dysfunction is one of the most common sequelae of pediatric TBI, early treatment is apt to allow children to be more successful in everyday settings, including the home, school, and community. Integration of CAPS or other problem-solving interventions into the outpatient management of pediatric TBI should be considered.
Limitations
Because outcome measures were based on parent-report only, evaluation of teacher or self-report may provide further insight into the efficacy of the intervention. Additionally, we did not examine the influence of the intervention on laboratory-based measures of executive function; however, the BRIEF has good ecological validity and correlates with functioning in everyday settings.43,52 Although our findings highlight the potential ecological impact of the CAPS intervention for executive dysfunction after pediatric TBI, we were unable to conceal assignment from families/participants; therefore, some effects of the intervention may be attributable to participant and family expectations or biases. Participants had more severe injuries compared with nonparticipants, which may limit the generalizability of the findings to individuals with more severe injuries. A further limitation is that the IRC group did not receive an equal amount of therapist contact; therefore, we are unable to definitively determine if the positive effects are related to the problem-solving intervention itself or generalized involvement of a therapist. The groups reported equal viewing of web information related to TBI; therefore, we can state that the CAPS intervention was more efficacious than the IRC intervention. Additional research needs to be done to elucidate the mechanism of effect. Finally, a relatively low percentage of the population was nonwhite, which may limit the generalizability of the findings
Conclusions
Findings indicate that the CAPS intervention improves executive functioning within the first 12 months after TBI in older adolescents. This is one of the few large, randomized controlled treatment trials performed in pediatric TBI demonstrating the efficacy of an online problems solving intervention for management of executive dysfunction. Use of the CAPS intervention clinically should be considered; however, additional research needs to define the optimal timing after injury for delivery of CAPS and characteristics of individuals and families that are more likely to benefit from CAPS or online problem-solving interventions more broadly. Future analyses are needed to determine whether these effects are maintained over the long term and elucidate factors associated with better maintenance of effects.
Acknowledgments
We acknowledge the contributions of Kendra McMullen, Robert Blaha, Elizabeth Hagesfeld, Michelle Jacobs, Daniel Maier, Mary Ann Toth, and Nina Fox in data collection and entry; Amy Cassedy in data management; and John Stullenberger in web site support. We also acknowledge the contributions of the therapists, JoAnne Carey, PsyD, Britt Nielsen, PsyD, and Brad Jackson, PhD
Glossary
- BRI
Behavioral Regulation Index
- BRIEF
Behavior Rating Inventory of Executive Function
- CAPS
counselor-assisted problem solving
- CT
computerized tomography
- GCS
Glasgow Coma Scale
- GEC
Global Executive Composite
- IRC
Internet Resource Comparison
- MI
Metacognition Index
- TBI
traumatic brain injury
Footnotes
Dr Kurowski conceptualized the hypotheses and analysis for this study, performed all associated analyses, interrupted the analyses, and drafted the initial manuscript; Dr Wade conceptualized the original study design, supervised data collection at all participating sites, assisted in conceptualization and analyses, and critically reviewed and revised the manuscript; Dr Kirkwood coordinated and supervised data collection at one site, and critically reviewed and revised the manuscript; Dr Brown coordinated and supervised data collection at her site, acted as a treating therapist at her site, and critically reviewed and revised the manuscript; Dr Stancin coordinated and supervised data collection at her site, and critically reviewed and revised the manuscript; Dr Taylor coordinated and supervised data collection at his site, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00409448).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by a grant from the Colorado Traumatic Brain Injury Trust Fund Research Program, Colorado Department of Human Services, Division of Vocational Rehabilitation, Traumatic Brain Injury Program. Also supported in part by the National Institutes of Health (NIH) grant R01-MH073764 from the National Institute of Mental Health and NIH grant 2K12 HD001097-16. Funded by the National Institutes of Health (NIH).
References
- 1.Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728–741 [DOI] [PubMed] [Google Scholar]
- 2.Styrke J, Stålnacke BM, Sojka P, Björnstig U. Traumatic brain injuries in a well-defined population: epidemiological aspects and severity. J Neurotrauma. 2007;24(9):1425–1436 [DOI] [PubMed] [Google Scholar]
- 3.Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J. A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien). 2006;148(3):255–268, discussion 268 [DOI] [PubMed] [Google Scholar]
- 4.Langlois J, Rutland-Brown W, Thomas K. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: US Department of Health and Human Servicies, CDC; 2004 [Google Scholar]
- 5.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. 2010, March. Available at: www.cdc.gov/TraumaticBrainInjury. Accessed April 21, 2011
- 6.Nadebaum C, Anderson V, Catroppa C. Executive function outcomes following traumatic brain injury in young children: a five year follow-up. Dev Neuropsychol. 2007;32(2):703–728 [DOI] [PubMed] [Google Scholar]
- 7.Sesma H, Slomine B, Ding R, McCarthy M, Grp CS. Executive functioning in the first year after pediatric traumatic brain injury. Pediatrics 2008;121(6). Available at: www.pediatrics.org/cgi/content/full/121/6/E1686 [DOI] [PubMed]
- 8.Levin HS, Hanten G. Executive functions after traumatic brain injury in children. Pediatr Neurol. 2005;33(2):79–93 [DOI] [PubMed] [Google Scholar]
- 9.Ganesalingam K, Yeates KO, Taylor HG, Walz NC, Stancin T, Wade S. Executive functions and social competence in young children 6 months following traumatic brain injury. Neuropsychology. 2011;25(4):466–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chapman LA, Wade SL, Walz NC, Taylor HG, Stancin T, Yeates KO. Clinically significant behavior problems during the initial 18 months following early childhood traumatic brain injury. Rehabil Psychol. 2010;55(1):48–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaffe KM, Fay GC, Polissar NL, et al. Severity of pediatric traumatic brain injury and early neurobehavioral outcome: a cohort study. Arch Phys Med Rehabil. 1992;73(6):540–547 [PubMed] [Google Scholar]
- 12.Massagli TL, Jaffe KM, Fay GC, Polissar NL, Liao S, Rivara JB. Neurobehavioral sequelae of severe pediatric traumatic brain injury: a cohort study. Arch Phys Med Rehabil. 1996;77(3):223–231 [DOI] [PubMed] [Google Scholar]
- 13.Fay GC, Jaffe KM, Polissar NL, Liao S, Rivara JB, Martin KM. Outcome of pediatric traumatic brain injury at three years: a cohort study. Arch Phys Med Rehabil. 1994;75(7):733–741 [PubMed] [Google Scholar]
- 14.Kurowski BG, Taylor HG, Yeates KO, Walz NC, Stancin T, Wade SL. Caregiver ratings of long-term executive dysfunction and attention problems after early childhood traumatic brain injury: family functioning is important. PM R. Sep 2011;3(9):836–845 [DOI] [PMC free article] [PubMed]
- 15.Kurowski BG, Taylor HG, Stancin T, Kirkwood M, Brown TM, Wade SL. Executive dysfunction after moderate and severe pediatric traumatic brain injury predicts functional impairment on the child and adolescent functional assessment scale. Am J Phys Med Rehabil. 2011;90(4):347–348 [Google Scholar]
- 16.Hanks RA, Rapport LJ, Millis SR, Deshpande SA. Measures of executive functioning as predictors of functional ability and social integration in a rehabilitation sample. Arch Phys Med Rehabil. 1999;80(9):1030–1037 [DOI] [PubMed] [Google Scholar]
- 17.Donders J, Warschausky S. Neurobehavioral outcomes after early versus late childhood traumatic brain injury. J Head Trauma Rehabil. 2007;22(5):296–302 [DOI] [PubMed] [Google Scholar]
- 18.Anderson V, Catroppa C. Recovery of executive skills following paediatric traumatic brain injury (TBI): a 2 year follow-up. Brain Inj. 2005;19(6):459–470 [DOI] [PubMed] [Google Scholar]
- 19.Struchen MA, Clark AN, Sander AM, Mills MR, Evans G, Kurtz D. Relation of executive functioning and social communication measures to functional outcomes following traumatic brain injury. NeuroRehabilitation. 2008;23(2):185–198 [PubMed] [Google Scholar]
- 20.Muscara F, Catroppa C, Anderson V. Social problem-solving skills as a mediator between executive function and long-term social outcome following paediatric traumatic brain injury. J Neuropsychol. 2008;2(pt 2):445–461 [DOI] [PubMed] [Google Scholar]
- 21.Galvin J, Mandalis A. Executive skills and their functional implications: approaches to rehabilitation after childhood TBI. Dev Neurorehabil. 2009;12(5):352–360 [DOI] [PubMed] [Google Scholar]
- 22.Blake CS, Hamrin V. Current approaches to the assessment and management of anger and aggression in youth: a review. J Child Adolesc Psychiatr Nurs. 2007;20(4):209–221 [DOI] [PubMed] [Google Scholar]
- 23.Clarke SA, Calam R. The effectiveness of psychosocial interventions designed to improve health-related quality of life (HRQOL) amongst asthmatic children and their families: a systematic review. Qual Life Res. 2012;21(5):747–764 [DOI] [PubMed]
- 24.Eccleston C, Palermo TM, Fisher E, Law E. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2012;8:CD009660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lochman JE, Powell NP, Boxmeyer CL, Jimenez-Camargo L. Cognitive-behavioral therapy for externalizing disorders in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20(2):305–318 [DOI] [PubMed] [Google Scholar]
- 26.Robin AL. Family intervention for home-based problems of adolescents with attention-deficit/hyperactivity disorder. Adolesc Med. 2008;19(2):268–277, ix [PubMed]
- 27.Chan DY, Fong KN. The effects of problem-solving skills training based on metacognitive principles for children with acquired brain injury attending mainstream schools: a controlled clinical trial. Disabil Rehabil. 2011;33(21–22):2023–2032 [DOI] [PubMed] [Google Scholar]
- 28.Kehle TJ, Clark E, Jenson WR. Interventions for students with traumatic brain injury: managing behavioral disturbances. J Learn Disabil. 1996;29(6):633–642 [DOI] [PubMed] [Google Scholar]
- 29.Suzman KB, Morris RD, Morris MK, Milan MA. Cognitive-behavioral remediation of problem solving deficits in children with acquired brain injury. J Behav Ther Exp Psychiatry. 1997;28(3):203–212 [DOI] [PubMed] [Google Scholar]
- 30.Wade SL, Walz NC, Carey JC, Williams KM. Preliminary efficacy of a Web-based family problem-solving treatment program for adolescents with traumatic brain injury. J Head Trauma Rehabil. 2008;23(6):369–377 [DOI] [PubMed] [Google Scholar]
- 31.Wade SL, Walz NC, Carey JC, Williams KM. Brief report: Description of feasibility and satisfaction findings from an innovative online family problem-solving intervention for adolescents following traumatic brain injury. J Pediatr Psychol. 2009;34(5):517–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wade SL, Michaud L, Brown TM. Putting the pieces together: preliminary efficacy of a family problem-solving intervention for children with traumatic brain injury. J Head Trauma Rehabil. 2006;21(1):57–67 [DOI] [PubMed] [Google Scholar]
- 33.Wade SL, Walz NC, Carey J, et al. Effect on behavior problems of teen online problem-solving for adolescent traumatic brain injury. Pediatrics. 2011;128(4). Available at: www.pediatrics.org/cgi/content/full/128/4/e947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wade SL, Walz NC, Carey J, et al. A randomized trial of teen online problem solving for improving executive function deficits following pediatric traumatic brain injury. J Head Trauma Rehabil. 2010;25(6):409–415 [DOI] [PubMed] [Google Scholar]
- 35.Wade SL, Wolfe C, Brown TM, Pestian JP. Putting the pieces together: preliminary efficacy of a web-based family intervention for children with traumatic brain injury. J Pediatr Psychol. 2005;30(5):437–442 [DOI] [PubMed] [Google Scholar]
- 36.Wade SL, Stancin T, Kirkwood M, Brown TM, McMullen KM, Taylor HG. Counselor-assisted problem solving (CAPS) improves behavioral outcomes in older adolescents with complicated mild to severe TBI [published online ahead of print May 1, 2013]. J Head Trauma Rehab. PMID: 23640543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: postacute effects on cognitive and school readiness skills. J Int Neuropsychol Soc. 2008;14(5):734–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20(1):42–57 [DOI] [PubMed] [Google Scholar]
- 39.Fletcher JM, Ewing-Cobbs L, Miner ME, Levin HS, Eisenberg HM. Behavioral changes after closed head injury in children. J Consult Clin Psychol. 1990;58(1):93–98 [DOI] [PubMed] [Google Scholar]
- 40.Sherer M, Stouter J, Hart T, et al. Computed tomography findings and early cognitive outcome after traumatic brain injury. Brain Inj. 2006;20(10):997–1005 [DOI] [PubMed] [Google Scholar]
- 41.Suskauer SJ, Huisman TA. Neuroimaging in pediatric traumatic brain injury: current and future predictors of functional outcome. Dev Disabil Res Reviews. 2009;15(2):117–123 [DOI] [PMC free article] [PubMed]
- 42.McLaughlin KA, Glang A, Beaver SV, Gau JM, Keen S. Web-based training in family advocacy [published online ahead of print June 8, 2012]. J Head Trauma Rehabil. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gioia GA, Isquith PK. Ecological assessment of executive function in traumatic brain injury. Dev Neuropsychol. 2004;25(1-2):135–158 [DOI] [PubMed] [Google Scholar]
- 44.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function. Child Neuropsychol. Sep 2000;6(3):235–238 [DOI] [PubMed]
- 45.Gioia G, Espy KA, Isquith PK. BRIEF-P: Behavior Rating Inventory of Executive Function—Preschool Version. Lutz, FL: Psychological Assessment Resources; 2003 [Google Scholar]
- 46.Gioia G, Isquith PK, Guy SC, Kenworthy L. BRIEF: Behavior Rating Inventory of Executive Function. Lutz, FL: Psychological Assessment Resources; 2000 [Google Scholar]
- 47.Donders J, DenBraber D, Vos L. Construct and criterion validity of the Behaviour Rating Inventory of Executive Function (BRIEF) in children referred for neuropsychological assessment after paediatric traumatic brain injury. J Neuropsychol. 2010;4(pt 2):197–209 [DOI] [PubMed] [Google Scholar]
- 48.Faul F, Erdfelder E, Lang AG, Buchner AG. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191 [DOI] [PubMed] [Google Scholar]
- 49.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- 50.Wade SL, Wolfe CR, Brown TM, Pestian JP. Can a web-based family problem-solving intervention work for children with traumatic brain injury? Rehabil Psychol. 2005;50(4):337–345 [Google Scholar]
- 51.Slomine BS, McCarthy ML, Ding R, et al. CHAT Study Group . Health care utilization and needs after pediatric traumatic brain injury. Pediatrics. 2006;117(4):e663–e674 [DOI] [PubMed] [Google Scholar]
- 52.Vriezen ER, Pigott SE. The relationship between parental report on the BRIEF and performance-based measures of executive function in children with moderate to severe traumatic brain injury. Child Neuropsychol. 2002;8(4):296–303 [DOI] [PubMed]