Abstract
OBJECTIVE:
This study systematically reviewed community-based childhood obesity prevention programs in the United States and high-income countries.
METHODS:
We searched Medline, Embase, PsychInfo, CINAHL, clinicaltrials.gov, and the Cochrane Library for relevant English-language studies. Studies were eligible if the intervention was primarily implemented in the community setting; had at least 1 year of follow-up after baseline; and compared results from an intervention to a comparison group. Two independent reviewers conducted title scans and abstract reviews and reviewed the full articles to assess eligibility. Each article received a double review for data abstraction. The second reviewer confirmed the first reviewer’s data abstraction for completeness and accuracy.
RESULTS:
Nine community-based studies were included; 5 randomized controlled trials and 4 non–randomized controlled trials. One study was conducted only in the community setting, 3 were conducted in the community and school setting, and 5 were conducted in the community setting in combination with at least 1 other setting such as the home. Desirable changes in BMI or BMI z-score were found in 4 of the 9 studies. Two studies reported significant improvements in behavioral outcomes (1 in physical activity and 1 in vegetable intake).
CONCLUSIONS:
The strength of evidence is moderate that a combined diet and physical activity intervention conducted in the community with a school component is more effective at preventing obesity or overweight. More research and consistent methods are needed to understand the comparative effectiveness of childhood obesity prevention programs in the community setting.
Keywords: childhood obesity, community-based, prevention
Childhood obesity represents one of the most important and challenging public health problems in developed countries. Although there appears to be an overall leveling off of the obesity epidemic among the pediatric population in the United States and other developed countries, low socioeconomic groups remain disproportionately affected.1,2 Despite evidence of body weight stabilization in the general population, obesity prevention should remain a priority because current prevalence is high,3 and previous stable phases have historically been followed by additional increases in obesity prevalence.4,5
The drivers of the positive energy balance (driven by either too much energy intake or too little energy expenditure) are increasingly being identified in the environment.6–9 As a result, recent trends in research, in the United States and other developed countries, emphasize the use of community-based settings as an important strategy for preventing obesity. This shift toward a stronger community focus is echoed by the recent Institute of Medicine report Accelerating Progress in Obesity Prevention, which recommends a comprehensive approach to childhood obesity prevention that includes the community.10 This community-based focus is especially important for children who generally have little or no control over the social and environmental factors where they live.
Given that most previous childhood obesity prevention programs have been conducted primarily in schools, the majority of systematic reviews have focused on that setting11–13. An exception is a recent Cochrane review,14 but little attention was devoted to community-based studies. Rather, the majority of included studies in that review were interventions conducted in school settings and interventions implemented for <12 months, an important limitation because of the weakness and bias of data derived from short-term behavior change studies.
In recent years, the body of literature focusing on childhood obesity prevention in the community setting has increased considerably, making the synthesis of this evidence base important. This study contributes to the literature by focusing specifically on community-based childhood obesity prevention programs in high-income countries. To our knowledge, no study has systematically reviewed this evidence base. We defined community-based interventions as those interventions resulting from policy, legislative, built environment, and economic/pricing/food subsidy changes that aimed to reduce population risk of obesity. We selected high-income countries, rather than all countries, given the paucity of intervention studies in other parts of the world. We compared diet, physical activity, or combined diet and physical activity interventions. This study is part of a larger, 2-year project of a systematic review funded by the Agency for Healthcare Research and Quality that examined the effectiveness of childhood obesity prevention studies in developed countries.15
Methods
We used the methods recommended by the Agency for Healthcare Research and Quality Methods Guide for Effectiveness and Comparative Effectiveness Reviews.16
Search Strategy
We searched Medline, Embase, PsychInfo, CINAHL, and the Cochrane Library through August 11, 2012, for relevant studies (the search was not limited to a start date, so all literature was cataloged). We developed a search strategy for Medline based on medical subject headings terms and text words of key articles that we identified a priori. We reviewed the reference lists of all included articles and relevant review articles to identify articles that the database searches might have missed. We uploaded the articles into DistillerSR, a Web-based software package developed for systematic review and data management. Studies published in other languages or unpublished studies were also examined, but none met our inclusion criteria.
Selection of Studies
We identified studies conducted in high-income countries that described the effects of interventions to prevent obesity (or “excessive weight gain”) in children and adolescents aged 2 to 18 years old. We included only randomized controlled trials (RCTs), quasi-experimental studies, and natural experiments. The studies needed to follow children for ≥1 year after the intervention.
The interventions of interest involved a modification of diet, a modification of physical activity or sedentary activity, or a combination of these. We required that the study reported on the attained differences between the intervention and control groups in weight-related outcomes (discussed subsequently). We excluded studies that targeted only overweight or obese subjects or those with a medical condition such as diabetes or heart disease. We included only articles published in English but reviewed the abstracts of non–English language articles to assess agreement with the results published in English
In particular, studies were eligible for inclusion if they (1) were primarily located in the community setting; (2) targeted at the pediatric population (ages 2–18); (3) had at ≥1 year of follow-up after baseline; (4) compared results from an intervention to a comparison group (eg, usual care, another different intervention, or no intervention); (5) reported differences in weight between the intervention and control groups (eg, BMI, BMI z-score and percentile, waist circumference, percent body fat, skinfold thickness, prevalence of obesity and overweight); (6) described results from RCTs, quasi-experimental studies, and natural experiments, such as those that described outcomes from a community that had a food policy change; or (7) were published in English but reviewed the abstracts of non–English language articles to assess agreement with the results published in English. We focused on prevention but not treatment of overweight and obese children because those studies have been reviewed elsewhere17 and because it is typically harder to lose weight than to prevent an initial weight gain.
Studies were excluded if they were (1) observational (eg, cross-sectional); (2) targeted only at overweight or obese children or adolescents; (3) targeted only at children or adolescents with chronic medical condition (eg, diabetes or heart disease); (4) expressly targeted at weight loss; (5) collected only qualitative results (eg, interviews or focus groups); (6) or published only in abstract form. We differentiated natural experiments from other observational study designs by specifying that a natural experiment was the implementation of a policy or similar intervention at a population level.
We also reviewed the reference lists of all included articles, relevant review articles, and related systematic reviews to identify additional articles.
Definitions of Outcomes
The primary outcomes were adiposity and obesity-related outcomes, which included BMI z-score, BMI, prevalence of obesity and overweight, percent body fat, waist circumference, and skinfold thickness (listed in hierarchical order based on their association with obesity).18–21 For studies that reported multiple body weight outcomes, we only reported the one closest to the top of the list.
The intermediate outcomes were dietary intake (energy intake, fruit and vegetable intake, fatty food intake, and sugar-sweetened beverage intake), physical activity, and sedentary behavior. For each of these outcomes, we also developed a hierarchy of measures and reported only 1 for each category.
Data Extraction
Two independent reviewers conducted title scans and abstract reviews and reviewed the full articles to assess eligibility for inclusion for each study. We created standardized forms for data extraction. Each article received a double review for data abstraction. The second reviewer confirmed the first reviewer’s data abstraction for completeness and accuracy. Reviewers extracted information on study characteristics, study participants, eligibility criteria, interventions, outcome measures, the method of ascertainment, and the outcomes.
Data Synthesis
Included studies were categorized as being implemented in the community only or in the community with other settings (eg, home, school, primary care, child care). For each setting, we organized the data by intervention target (diet only, physical activity only, and combined diet and physical activity) and outcomes (primary weight outcomes and intermediate outcomes). Because of the limited number of studies for each intervention, we did not quantitatively pool the results. We extracted clinical outcomes that are reported in the text of the evidence report (available at www.ahrq.gov).
Risk of Bias Assessment
We used the Downs and Black instrument to assess the risk of bias in the included studies.22 We categorized the studies as having low, moderate, or high risk of bias. We rated a study as having low risk of bias only when it had done all of the following: stated the objective clearly, described the main outcomes, described the characteristics of the enrolled subjects, described the intervention clearly, described the main findings, randomized the subjects to the intervention group, and concealed the intervention assignment until recruitment was complete. Additionally, the study had to have at least partially described the distributions of (potential) principal confounders in each treatment group. If a study did not complete 1 of the above items or if this was difficult to verify, it was classified as having a moderate risk of bias; for a study that definitively did not do ≥2 of the items, it was classified as having a high risk of bias.
Strength of Evidence Assessment
After synthesizing the evidence, we graded the quantity, quality, and consistency of the best available evidence by adapting an evidence grading scheme recommended in the Methods Guide for Conducting Comparative Effectiveness Reviews.16 We assigned grades for all weight-related outcomes by setting up a hierarchy of outcomes. Within this hierarchy, each study contributed only 1 weight-related measure to the grade. The hierarchy was as follows: BMI z-score, BMI, prevalence of obesity and overweight, percent body fat, waist circumference, and skinfold thickness. For example, if a study measured BMI z-score and body fat, we only graded BMI z-score. We chose 6 categories of intermediate outcomes: energy intake, fruit and vegetable intake, fatty food intake, sugar-sweetened beverage intake, physical activity, and sedentary activity.
We considered the 4 recommended domains including risk of bias, directness of the evidence, consistency across studies, and precision of the pooled estimate or the individual study estimates.
We classified evidence into 4 categories: (1) “high” grade (indicating high confidence that the evidence reflects the true effect, and further research is unlikely to change our confidence in the estimate of the effect); (2) “moderate” grade (indicating moderate confidence that the evidence reflects the true effect, and further research may change our confidence in the estimate of the effect and may change the estimate); (3) “low” grade (indicating low confidence that the evidence reflects the true effect, and further research is likely to change our confidence in the estimate of the effect and is likely to change the estimate); and (4) “insufficient” grade (indicating evidence is unavailable, there was only 1 study, and it had moderate to high risk of bias, or a conclusion could not be drawn based on the data).
We considered the body of evidence consistent in direction if ≥70% of the studies had an effect in the same direction (ie, showed desirable effect verse not). We considered a study precise if the results for the given outcome were significant at a P < .05 or had narrow confidence intervals that excluded the null. If ≥70% of the studies reported statistically significant results, we considered the body of evidence precise.
Results
Literature Search
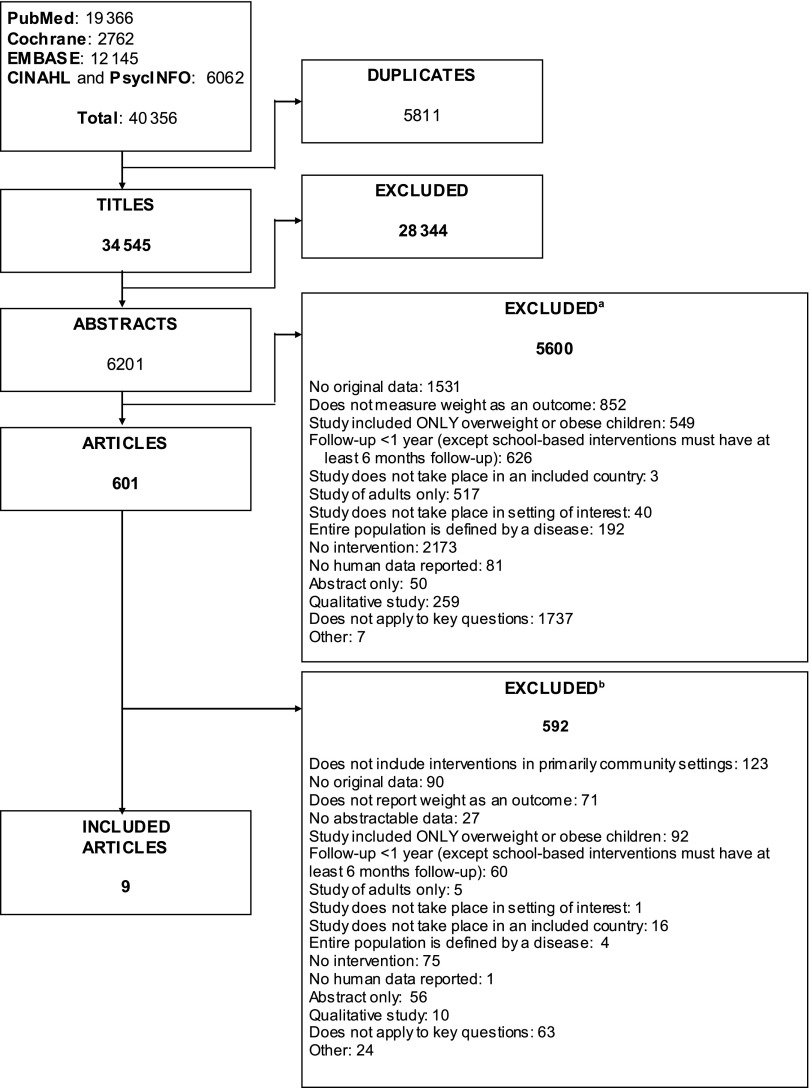
The literature search outlined in the methods identified 40 356 potential articles, including 5791 duplicates (Fig 1). We identified 601 articles that potentially met all criteria as a result of title and abstract screening. Four hundred and seventy articles did not meet the inclusion criteria, and an additional 122 articles were not community-based interventions. Thus, 9 articles were finally included in this review.
FIGURE 1.
Literature search for community-based childhood obesity prevention studies in high-income countries. aSum of excluded abstracts exceeds 5600 because reviewers were not required to agree on reasons for exclusion. bSum of excluded articles exceeds 592 because reviewers were not required to agree on reasons for exclusion.
Study Settings and Intervention Characteristics
The study settings varied considerably; 1 intervention was exclusively in a community setting23 (Table 1). The other studies were implemented in settings that included the community and additional venue(s) (eg, school, home, primary care, child care). The programs delivered a variety of interventions that were administered over a range of 12 months for an exercise resistance program23 to 48 months for complex interventions involving multiple community stakeholders.24 One study reported on a physical activity intervention23; all others reported on combination interventions including both diet and physical activity. Five of the studies were RCTs,23,25–28 and 4 of the studies were quasi-experimental.24,29–31 Six of the studies were conducted in the United States,24,25,27–30 1 in Australia,31 1 in Switzerland,23 and 1 in the Netherlands.26
TABLE 1.
Characteristics of the Included Studies Testing the Effect of Community-Based Childhood Obesity Prevention Programs (n = 9)
| First Author, Year, Country | Setting(s) | RCT | Sample Size | Sample Age (Range or Mean y) | Girls (%) | Intervention Time: Elements Included in the Intervention | Follow-up Perioda (mo) |
|---|---|---|---|---|---|---|---|
| Chang, 2010, United States30 | Community, school, primary care, and child-care components | No | 4595 | 2–17 | NR | 24 mo: social marketing, strategic partnerships, knowledge mobilization, strategies in multiple sectors | NR |
| Chomitz, 2010, United States24 | Community, school | No | 1858 | 8 | 48 | 36 mo: city policies, community awareness campaigns, physical education enhancements, food service reforms, farm-to-school-to-home programs, family outreach, BMI and fitness reports | 36 |
| de Silva-Sanigorski, 2010, Australia31 | Community, home, primary care, child care | No | 43 811 | 2–3.5 | 49 | 48 mo: community capacity building and environmental changes to increase healthy eating and active play | 48 |
| Economos, 2007, United States29 | Community, school, home | No | 1178 | 7 | NR | 10 mo: physical activity options and availability of healthy foods before, during, and after school; social marketing; family outreach and engagement | 36 |
| Eiholzer, 2010, Switzerland23 | Community only | Yes | 46 | 13 | 0 | 4 mo: resistance exercise program | 12 |
| Klesges, 201028 | Community, home | Yes | 303 | 9 | 100 | 20 mo: group behavioral counseling (obesity prevention program) or self-esteem and social efficacy (alternative intervention) | 24 |
| Robinson, 2010, United States27 | Community, home | Yes | 261 | 9 | 100 | 24 mo: dance classes and reduced screen use; health education | 24 |
| Sallis, 2003, United States25 | Community, school | Yes | 24 schools (mean enroll-ment: 1109) | NR | 49 | 24 mo: physical education, physical promotion throughout school day, changes to school food service, social marketing | 24 |
| Singh, 2009, Netherlands26 | Community, school | Yes | 1108 | 13 | 53 | 8 mo: education in biology and physical activity, environmental change options for schools (physical education classes, changes to school cafeteria) | 20 |
The sample size of each study represents the number of children included in the analysis with both baseline and follow-up data available. NR, not reported.
From start of intervention.
Common characteristics found across most of the studies included the use of multiple intervention components (eg, health education and family outreach), the inclusion of settings other than just the community (eg, school, home, primary care, child care), and a focus on children at middle school age or younger. Each of the studies is now described in detail.
Chang et al30 examined a statewide strategy to reduce childhood obesity in the state of Delaware. The study included 4595 children from birth to age 17 years. This community-based population health intervention included policy and practice changes including statewide regulations to reduce sedentary behavior and promote healthy eating/physical activity, implementation of wellness policies in schools, student fitness assessment, training of child care providers about healthy behaviors, and provision of primary care physicians with tools to meet expert committee recommendations about obesity care.
Chomitz et al,24 in a study called Healthy Living Cambridge Kids, assessed the impact of a community-based healthy weight intervention in the United States on child weight and fitness targeting community, school, and home (family and individuals). It included 1858 children in elementary school (grades kindergarten to 5) of whom 37% were African American, 14% were Hispanic, 37% were white, and 10% were Asian; the follow-up period was 36 months. The intervention included community awareness of healthy eating, improvements to food service in schools including new recipes and menu development and cafeteria taste tests, and improving access to appealing physical education programs in the schools.
De Silva-Sanigorski et al,31 in the Romp and Chomp intervention in Australia, examined the effectiveness of an intervention that aimed to reduce obesity and promote healthy eating and active play in children aged 0 to 5 years old. The sample included 16 869 2-year-olds and 12 354 3-year-olds with a follow-up period of 48 months. The intervention included community capacity building and environmental (political, sociocultural, and physical) changes to increase healthy eating and active play in early-childhood care and educational settings. It had 8 specific objectives focused broadly on capacity building, increased awareness, improved diet, and increased physical activity.
Economos et al,29 in Shape Up Sommerville, examined whether a community-based environmental intervention could prevent weight gain in young children. It included 1178 children in grades 1 to 3 attending public elementary schools with a follow-up period of 12 months. The intervention focused on increasing physical activity options and availability of healthful foods within the before-, during-, after-school setting and in the home and community.
Eiholzer et al23 examined whether high-intensity training increases spontaneous physical activity in children in Switzerland. It included 2 junior ice hockey teams consisting of 46 boys with a mean age of 13 years and had a follow-up period of 12 months. The intervention included high-intensity training exercises including supervised 1-hour exercise sessions twice weekly.
Klesges et al,28 in the the Memphis Girls Health Enrichment Multi-Site Study, examined the impact of a community- and family-based obesity prevention program for low-income African American girls. The study included 303 African American girls aged 8 to 10 years and their parents or guardian and a follow-up period of 24 months. The intervention randomized families to 1 of 2 interventions: (1) group behavioral counseling to promote healthy eating and increased physical activity or (2) self-esteem and social efficacy intervention.
Robinson et al’s27 Stanford Girls Health Enrichment Multi-Site Study examined the impact of a community- and family-based obesity prevention program for low-income African American girls. The study included 261 African American girls aged 8 to 10 years and their parents or guardian and a follow-up period of 24 months. The intervention randomized families to 1 of 2 interventions: (1) afterschool hip-hop, African, and step-dance classes and a home/family-based intervention to reduce screen media use or (2) information-based health education.
Sallis et al25 evaluated the effects of environmental, policy, and social marketing interventions on physical activity and fat intake of middle school students in the United States. It included 24 middle schools with mean enrollments of 1109 children with 44% nonwhite students and a follow-up period of 24 months. The intervention included physical activity (increased physical activity in physical education classes and throughout the school day), nutrition (provided low-fat foods at all school food sources), and engagement of school staff and students in policy change efforts.
Singh et al’s26 Dutch Obesity Intervention in Teenagers (DoiT) examined the impact of a multicomponent health promotion intervention for Dutch adolescents (aged 12–14) on body composition and dietary and physical activity behavior. It included 1108 adolescents (mean age 12.7 years) with a follow-up period of 20 months. The intervention consisted of an individual component (ie, an educational program) and an environmental component (ie, encouraging that schools offer additional physical education classes and changes in and around school cafeterias).
With the exception of 2 studies, which received active interventions,27,28 the control groups for these studies received no intervention.
Primary Adiposity- and Obesity-Related Outcomes
The primary weight outcomes are described in Table 2. Overall, desirable and significant changes in BMI or BMI z-score were found in 4 of 9 studies, indicated by a checkmark in the far right column of the table. In general, the studies that found significant changes were characterized by a relatively longer follow-up time, a focus on younger children (middle school or younger), a quasi-experimental design that allowed for the inclusion of multiple intervention components, and the inclusion of settings other than just the community. As indicated in the footnote to Table 2, the comparison group was an active intervention in 2 studies.27,28
TABLE 2.
Primary Weight Outcomes in 9 Studies Testing Community-Based Childhood Obesity Prevention Interventions
| Study, Year | Primary Outcome | Reported Outcome at End of Follow-up | Difference in Change From Baseline (Control vs Intervention) | Significance of the Control vs Intervention Difference | Desirable Intervention Effect | |
|---|---|---|---|---|---|---|
| Control Group | Intervention Group | |||||
| Chang, 201030 | Prevalence of obesity (%) | NA | 24.2 | NR | NR (authors indicate the change was not significant) | |
| Chomitz, 201024 | BMI change from baseline, BMI z-score | 0.67 | 0.63 | −0.04 | P < .001 | ✓ |
| de Silva-Sanigorski, 201031 | BMI change (kg/m2) | Age 2 y: 16.6; 3.5 y: 16.2 | Age 2 y: 16.8; 3.5 y: 16.2 | Age 2 y: –0.02; 3.5 y: –0.06 | Age 2 y: CI (–0.06 to 0.01); 3.5 y: CI (–0.10 to –0.01) | ✓ |
| Economos, 200729 | BMI change from baseline, BMI z-score | CG 1: Boys, 0.76; girls: 0.62. CG 2: Boys: 1.11; girls: 0.69 | Boys: 0.88; girls: 0.76 | −0.1005 | CI (–0.12 to –0.086) | ✓ |
| Eiholzer, 201023 | Fat mass, kg | 0.65a | 0.39a | P = .34 | ||
| Sallis, 200325 | BMI change (kg/m2) | Boys: 20.0; girls: 19.7 | Boys: 19.8; girls: 19.9 | Boys: 0.83; girls: –0.12 | Boys: P = .044; girls: P = .77 | ✓ |
| Singh, 200926 | BMI change (kg/m2) | Boys: 20.0; girls: 20.9 | Boys: 19.4; girls: 20.2 | Boys: 0.2; girls: 0.2 | Boys: CI (–0.1 to 0.4); girls: CI (–0.1 to 0.5) | |
| Klesges, 201028b | BMI change (kg/m2) | NR | NR | −0.06 | CI (-0.87 to 0.75) | |
| Robinson, 201027b,c | BMI change (kg/m2) | NR | NR | 0.04 | CI (-0.18 to 0.27) | |
CG, control group; NA, not applicable, NR, not reported.
Change from baseline.
The comparison group is an active intervention. For the Kelsges et al study, group behavioral counseling (obesity prevention program) is compared with self-esteem and social efficacy (alternative intervention). For the Robinson et al study, dance classes and reduced screen use are compared with health education.
This intervention had no control; the health education intervention is reported in the control column. and the dance and screen time reduction intervention is reported in the intervention column.
Chang et al’s study,30 conducted in a community in Delaware with components in the school, primary care, and child-care settings, showed no significant change in the prevalence of obesity. The Chomitz et al study (Healthy Living Cambridge Kids),24 conducted in Cambridge, Massachusetts, in the community setting with school involvement, demonstrated significant reductions in BMI z-score from 0.67 (sd = 1.06) to 0.63 (sd = 1.03), P < .001). De Silva-Sanigorski et al’s study,31 conducted in the community setting with participation from family, primary care physician, and child care, observed a significant reduction in BMI for children aged 3.5 years (β = –0.06 kg/m2; 95% CI: –0.10 to –0.01 kg/m2). Economos et al (Shape Up Sommerville),29 conducted in the community setting with school and home components, observed a significant reduction in BMI z-score (β = –0.1005; 95% CI: –0.1151 to –0.0859). Eiholzer et al,23 conducted in the community among 2 boys’ ice hockey teams, showed no significant change in body fat. Kresges et al’s study,28 conducted in the community with a home component, did not observe significant differences in BMI between the 2 groups. Robinson et al,27 conducted in the community with a home component, did not observe significant differences in BMI between the 2 groups. The study was conducted among a small sample of African American girls. The health education and physical activity interventions were conducted in different study groups; therefore, the participants did not receive both the diet and physical activity intervention. Sallis et al’s study,25 conducted in the community with a school component, demonstrated a significant reduction in BMI for boys (from 20.1 to 19.8 kg/m2, P = .044) but not girls. Singh et al’s study,26 conducted in the community with a school component, did not observe significant differences in BMI.
There is moderate strength of evidence that community-based interventions that include a school component effectively prevent obesity or overweight in children (Table 3). Two of the 3 studies24,25 implemented in the community with school involvement, which tested combined diet and physical activity interventions, detected a statistically significant beneficial effect of the intervention. The evidence is insufficient to support the benefit of other interventions conducted in the community alone or with involvement from other settings (eg, home, primary care, child care) that use physical activity or combination approaches for obesity prevention in children.
TABLE 3.
Summary of the Strength of Evidence for Interventions in the Community: Primary Weight Outcomes
| Setting, N | Intervention | Year(s) of Study | Enrolled Participants | Studies With Low/Moderate/High Risk of Bias (n) | % With Favorablea Outcome | Evidence Statement |
|---|---|---|---|---|---|---|
| Community only, 1 | PA | 2010 | 46 | 0/1/0 | W | Insufficient |
| Community, school, 3 | D and PA | 1997–2010 | 2966 and 24 schools (mean enrollment of 1109 | 0/3/0 | 2 | Moderate |
| Community, school, home, 2 | D and PA | 2007–2008 | 1326 | 0/1/1 | 1 | Insufficient |
| Community, home, 2 | PA | 2008–2010 | 564 | 0/0/2 | 0 | Insufficient |
| Community, home, primary care and child care, 1 | D and PA | 2010 | 43 811 | 0/1/0 | 1 | Insufficient |
| Community, school, primary care, and child care components, 1 | D | 2010 | 4595 | 0/0/1 | 1 | Insufficient |
D, diet intervention; PA, physical activity intervention.
“Favorable” indicates statistically significant.
Intermediate Outcomes—Behavioral Outcomes
The reported types of intermediate outcomes varied considerably across studies with only 1 study finding a significant effect (Table 4). As indicated in the footnote to Table 4, for 2 studies, the comparison group was an active intervention.27,28 The de Silva-Sanigorski et al study31 observed a statistically marginally significant (P < .010) increase in servings of vegetables in the intervention group compared with the control (by 0.10, P = .07). The Eiholzer study in Switzerland detected a statistically significant benefit of high-intensity training on spontaneous physical activity in the intervention group compared with the control (–0.01 kcal/min vs 0.23 kcal/min, P = .02).23
TABLE 4.
Secondary Weight Outcomes for Community-Based Childhood Obesity Prevention Studies in High-Income Countries (n = 9)
| Study, Year | Secondary Outcome | Measurement of Secondary Outcome at Follow-up | Magnitude of Change From Baselinea | Significance of Change From Baselinea | |
|---|---|---|---|---|---|
| Control | Intervention | ||||
| Chang, 201030 | NR | ||||
| Chomitz, 201024 | NR | ||||
| de Silva-Sanigorski, 201031 | Servings of vegetables | NR | NR | 0.10 | P = .07 |
| Servings of fruit | NR | NR | 0.07 | P = .14 | |
| Economos, 200729 | NR | ||||
| Eiholzer, 201023 | Change in physical activity (SpAEE), kcal/min | −0.01 | 0.23 | NR | P = .02 |
| Change in physical activity (TrAEE), kcal/min | −0.21 | 0.30 | NR | P = .48 | |
| Sallis, 200325 | Student fatty foods | Boys: 9.7 | Boys:8.9 | Boys: –0.13 | Boys: P = .76 |
| Girls: 8.2 | Girls: 8.0 | Girls: –0.03 | Girls: P = .94 | ||
| Moderate to vigorous physical activity | Boys: 104 | Boys: 115 | Boys: 0.09 | Boys: P = .84 | |
| Girls: 91 | Girls: 93 | Girls: 0.25 | Girls: P = .55 | ||
| Sedentary h/d/student | Boys:3.87 | Boys: 4.42 | Boys: 0.17 | Boys: P = .69 | |
| Girls:4.61 | Girls: 4.64 | Girls: 0.11 | Girls: P = .71 | ||
| Singh, 200926 | Change in SSB consumption (mL/d) | 714 | 689 | −88 | CI (–203 to 28) |
| Active commuting to school, min/d | 42 | 46 | −2 | CI (–10 to 5) | |
| Screen-viewing behavior (television viewing and computer use), min/d | 248 | 258 | −2 | CI (–9 to 5) | |
| Klesges, 201028b | Mean total energy intake, kcal | NR | NR | −78 | CI (–186.3 to 31.1) |
| Servings of vegetables | NR | NR | 0.2 | CI (–0.0 to 0.3) | |
| Servings of fruit | NR | NR | −0.0 | CI (–0.2 to 0.2) | |
| Moderate to vigorous activity, min | NR | NR | 0.6 | CI (–1.3 to 2.4) | |
| Robinson, 201027b | Mean total energy intake, kcal | NR | NR | −27.3 | CI (–69.9 to 15.0) |
| Weekday accelerometer counts, counts/min | NR | NR | 3.18 | CI (–11.6 to 17.9) | |
| Weekly total screen time, h | NR | NR | −2.65 | CI (–5.42 to 0.13) | |
NA, not applicable; NR, not reported; SpAEE, spontaneous physical activity energy expenditure; SSB, sugar sweetened beverages; TrAEE, training activity energy expenditure.
Control vs intervention.
The comparison group is an active intervention. For the Kelsges et al study, group behavioral counseling (obesity prevention program) is compared with self-esteem and social efficacy (alternative intervention). For the Robinson et al study, dance classes and reduced screen use are compared with health education.
Discussion
This systematic review identified 9 relevant studies. Four of the studies, which used combined diet and physical activity approaches, reported significant reduction in adiposity and weight-related outcomes as a result of the intervention.24,25,29,31 One of the studies reported significant improvements in intermediate weight-related outcome (physical activity) as a result of the intervention.23 There are currently not enough studies with consistent methods and outcomes to determine the impact of community-based childhood obesity prevention programs on primary or secondary weight outcomes. However, the evidence suggests that combination interventions implemented in multiple settings may be more effective at preventing weight gain in children than single-component interventions located in the community only. In particular, we found moderate evidence that community-based interventions that include a school component and use interventions focused on both diet and physical activity effectively prevent obesity or overweight in children, regardless of the design of the study (ie, RCT or non-RCT). The completeness with which interventions are implemented has been associated with program impact.32 There is considerable heterogeneity across the study designs, which may contribute to the inconsistent findings. The studies used different units of analysis (eg, child, school), different methodologies (eg, RCTs vs quasi-experimental studies), were located in nonuniform settings, and used different interventions (eg, physical activity or combined diet and physical activity).
The studies that observed a significant decline in adiposity outcomes generally enrolled more participants and had longer follow-up periods, a focus on children middle school age or younger, the inclusion of settings other than just the community, and less rigorous study designs; 3 of the 4 studies that demonstrated significant reductions is child weight were quasi-experimental.
This review has some limitations. Many studies published in this area have suboptimal study designs, which may lead to biased results. Unsuccessful programs may not have been included in the analysis because of a lack of published data. As a result, there may be some publication bias, which may have affected the magnitude of the results. Our study was restricted to articles published in English but examined abstracts of studies in other languages as well. Our study was also restricted to interventions located primarily in the community setting, which excluded a number of studies that included the community as a secondary component.
This study has a number of strengths. A range of community-based childhood obesity prevention interventions from different countries were included. Robust review methods were used including the use of multiple databases to identify articles and paired reviewers. The findings from this review can help guide future research strategies as well as decision-making for researchers, clinicians, public health practitioners, and policy makers about the most appropriate setting and types of interventions to focus on to maximize efforts to prevent childhood obesity in developed countries.
More generally, understanding the effectiveness of community-based childhood obesity prevention programs is an important area of study. Even if interventions have a modest effect on individual body weight, the cumulative impact across the population has the potential to yield significant public health benefits.
In conclusion, the strength of evidence is moderate that community-based childhood obesity prevention programs with a school component focusing on both diet and physical activity is more effective at preventing obesity or overweight. More research and more consistent methods are needed to understand the comparative effectiveness of these intervention programs.
Glossary
- CI
confidence interval
- RCT
randomized controlled trials
Footnotes
Dr Bleich conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted; Dr Segal conceptualized and designed the study and critically reviewed and revised the manuscript; Ms Wu reviewed and revised the manuscript; Ms Wilson coordinated and supervised data the systematic review; she also reviewed and revised the manuscript; and Dr Wang conceptualized and designed the study and critically reviewed and revised the manuscript.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This project was funded under contract 290-2007-10061-I from the Agency for Healthcare Research and Quality, US Department of Health and Human Services. The authors of this report are responsible for its content. Statements in the report should not be construed as endorsement by the Agency for Healthcare Research and Quality or the US Department of Health and Human Services. This work was also supported by a grant from the National Heart, Lung, and Blood Institute at the National Institutes of Health (1K01HL096409). Funded by the National Institutes of Health.
COMPANION PAPER: A companion to this article can be found on page e193, online at www.pediatrics.org/cgi/doi/10.1542/peds.2013-0786.
References
- 1.Olds TS, Tomkinson GR, Ferrar KE, Maher CA. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int J Obes (Lond). 2010;34(1):57–66 [DOI] [PubMed] [Google Scholar]
- 2.Rokholm B, Baker JL, Sørensen TIA. The levelling off of the obesity epidemic since the year 1999—a review of evidence and perspectives. Obes Rev. 2010;11(12):835–846 [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249 [DOI] [PubMed] [Google Scholar]
- 4.Olds TS, Harten NR. One hundred years of growth: the evolution of height, mass, and body composition in Australian children, 1899–1999. Hum Biol. 2001;73(5):727–738 [DOI] [PubMed] [Google Scholar]
- 5.Keith SW, Redden DT, Katzmarzyk PT, et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int J Obes (Lond). 2006;30(11):1585–1594 [DOI] [PubMed] [Google Scholar]
- 6.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280(5368):1371–1374 [DOI] [PubMed] [Google Scholar]
- 7.Nestle M, Jacobson MF. Halting the obesity epidemic: a public health policy approach. Public Health Rep. 2000;115(1):12–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80(4):569–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bleich SN, Thorpe RJ, Jr, Sharif-Harris H, Fesahazion R, Laveist TA. Social context explains race disparities in obesity among women. J Epidemiol Community Health. 2010;64(5):465–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institute of Medicine Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: Institute of Medicine; 2012 [Google Scholar]
- 11.Katz DL, O’Connell M, Njike VY, Yeh MC, Nawaz H. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis. Int J Obes (Lond). 2008;32(12):1780–1789 [DOI] [PubMed] [Google Scholar]
- 12.Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev. 2012;13(3):214–233 [DOI] [PubMed] [Google Scholar]
- 13.Nixon CA, Moore HJ, Douthwaite W, et al. ToyBox-study group . Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4–6-year-olds: a systematic review. Obes Rev. 2012;13(suppl 1):106–117 [DOI] [PubMed] [Google Scholar]
- 14.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011; (12):CD001871. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Wu Y, Wilson R, et al. Childhood Obesity Prevention Programs: A Comparative Effectiveness Review and Meta-analysis. Rockville, MD: Agency for Healthcare Research and Quality; 2012 [PubMed] [Google Scholar]
- 16.Agency for Healthcare Quality and Research. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2012 [PubMed]
- 17.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–e418 [DOI] [PubMed] [Google Scholar]
- 18.Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr. 2002;75(6):978–985 [DOI] [PubMed] [Google Scholar]
- 19.Noppa H, Andersson M, Bengtsson C, Bruce A, Isaksson B. Body composition in middle-aged women with special reference to the correlation between body fat mass and anthropometric data. Am J Clin Nutr. 1979;32(7):1388–1395 [DOI] [PubMed] [Google Scholar]
- 20.Sarría A, García-Llop LA, Moreno LA, Fleta J, Morellón MP, Bueno M. Skinfold thickness measurements are better predictors of body fat percentage than body mass index in male Spanish children and adolescents. Eur J Clin Nutr. 1998;52(8):573–576 [DOI] [PubMed] [Google Scholar]
- 21.Garrido-Chamorro RP, Sirvent-Belando JE, Gonzalez-Lorenzo M, Martin-Carratala ML, Roche E. Correlation between body mass index and body composition in elite athletes. J Sports Med Phys Fitness. 200;49(3):278–284 [PubMed]
- 22.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eiholzer U, Meinhardt U, Petrò R, Witassek F, Gutzwiller F, Gasser T. High-intensity training increases spontaneous physical activity in children: a randomized controlled study. J Pediatr. 2010;156(2):242–246 [DOI] [PubMed] [Google Scholar]
- 24.Chomitz VR, McGowan RJ, Wendel JM, et al. Healthy Living Cambridge Kids: a community-based participatory effort to promote healthy weight and fitness. Obesity (Silver Spring). 2010;18(suppl 1):S45–S53 [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, McKenzie TL, Conway TL, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. Am J Prev Med. 2003;24(3):209–217 [DOI] [PubMed] [Google Scholar]
- 26.Singh AS, Chin A Paw MJ, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163(4):309–317 [DOI] [PubMed] [Google Scholar]
- 27.Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;164(11):995–1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klesges RC, Obarzanek E, Kumanyika S, et al. The Memphis Girls’ health Enrichment Multi-site Studies (GEMS): an evaluation of the efficacy of a 2-year obesity prevention program in African American girls. Arch Pediatr Adolesc Med. 2010;164(11):1007–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Economos CD, Hyatt RR, Goldberg JP, et al. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity (Silver Spring). 2007;15(5):1325–1336 [DOI] [PubMed] [Google Scholar]
- 30.Chang DI, Gertel-Rosenberg A, Drayton VL, Schmidt S, Angalet GB. A statewide strategy to battle child obesity in Delaware. Health Aff (Millwood). 2010;29(3):481–490 [DOI] [PubMed] [Google Scholar]
- 31.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91(4):831–840 [DOI] [PubMed] [Google Scholar]
- 32.Te Velde SJ, Brug J, Wind M, et al. Effects of a comprehensive fruit- and vegetable-promoting school-based intervention in three European countries: the Pro Children Study. Br J Nutr. 2008;99(4):893–903 [DOI] [PubMed] [Google Scholar]