Abstract
Since the classic description of cam femoroacetabular impingement occurring in the anterolateral quadrant of the proximal femur, there has been growing evidence of cam impingement extending outside of this region. Although anteromedial cam decompression may be performed, posterior cam decompression is at higher theoretic risk of vascular embarrassment with osteonecrosis and/or tensile failure with fracture, leading some investigators to believe that these major deformities require open surgical correction. We present a less invasive method of arthroscopic posterior cam decompression using the modified midanterior portal while avoiding the posterolateral vasculature of the proximal femur.
Cam femoroacetabular impingement (FAI) is recognized as a common cause of painful disability and osteoarthrosis, often in young active patients. The pathomechanism involves chondrolabral damage from mechanical abutment of the proximal femur with the acetabular rim. Arthroscopic treatment of pincer and cam FAI has been successfully performed with outcomes and safety comparing favorably with those of open and mini-open methods.1,2
Cam FAI was classically described as a bump or decrement in offset at the anterolateral quadrant of the femoral head-neck region. Recent evidence suggests that the cam deformity may extend outside of this region with premature anteromedial abutment.3-5 Anteromedial femoroplasty of the anteromedial “critical corner” may improve blocked internal rotation of the flexed hip.6 However, femoroplasty for cam decompression posterior to the mid-coronal plane of the proximal femur may cause iatrogenic damage to the primary vascular supply to the femoral head. A subsynovial retinacular leash of vessels originates from the ascending branch of the medial femoral circumflex artery. A practical landmark demarcating its anterior-most extent is the lateral synovial fold. A vascular safe zone has been described anterior to the mid-coronal plane of the superior femoral neck with a recommendation to avoid crossing this threshold during femoroplasty.7
The typical cam deformity involves the anterior aspect of the proximal femur and is visualized on a variety of lateral-projection radiographs with varying degrees of detection.8-11 The classic pistol-grip deformity was described on the anteroposterior (AP) projection (Fig 1) and implies not only superior involvement but also varying amounts of cam morphology posterior to the mid-coronal plane. Posterior cam FAI may cause pain during activities such as sitting with the hips in a figure-of-4 position or during the frog kick used for the breaststroke and may be detected on flexion–abduction–external rotation (FABER) or hyperextension–external rotation testing12 in static or dynamic mode. It may be nicely assessed with 3-dimensional computed tomographic imaging13 (Fig 2). Failure to sufficiently address residual impingement is the leading reason for revision hip arthroscopy.14,15 Our early experience with cam decompression showed minimal if any radiographic improvement on the AP view because we were not sufficiently resecting the superior or posterosuperior regions of the proximal femur. We noted patients with improved hip internal rotation but little if any improvement in painful external rotation on FABER testing.
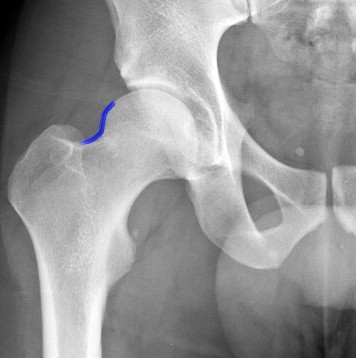
Fig 1.

Detail of preoperative AP pelvis radiograph of a 30-year-old man with symptomatic FAI. One should note the pistol-grip convex deformity (blue line), as well as the ischial spine sign and cephalad crossover sign indicative of focal pincer FAI from acetabular retroversion.
Fig 2.
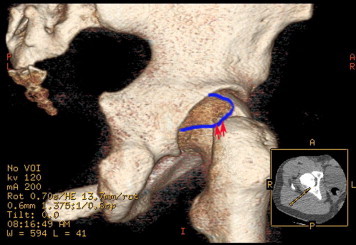
Three-dimensional reconstructed computed tomographic image showing the extension of the cam deformity into the posterosuperior region (blue outline) and perforating holes, which may represent where the posterolateral retinacular vessels enter the femoral head-neck junction (arrows). Some of the deformity is “covered” by the acetabular rim. The inset shows the CT orientation for 3-dimensional reconstructed image. (A, anterior; l, left; p, posterior; r, right.)
It has been suggested that patients with severe deformities such as posterior cam FAI are best treated with open surgical dislocation rather than hip arthroscopy.16 The presumption has been better relative visualization and osteoplasty of the posterosuperior femoral head-neck region to perform sufficient and safe femoroplasty, minimizing the risks of femoral head osteonecrosis or femoral neck fracture. Indeed, the presence of a pistol-grip deformity seen on an AP radiograph has been considered an indication for open surgical dislocation of the hip rather than hip arthroscopy. Other investigators have suggested the need for a posterolateral portal to perform this procedure; however, the proximity of this portal to the sciatic nerve has been shown.17 We have been performing arthroscopic posterior cam decompression using the modified midanterior portal and demonstrate this procedure with key steps in this technical note.
Technical Note
Supine dual-portal hip arthroscopy is performed with a 70° arthroscope in the anterolateral viewing portal and instrumentation in the modified midanterior working portal (MMAP).18,19 The setup includes standardizing the pelvis to a vertical C-arm device using the fluoroscopic templating technique,20 which we have found helpful for pincer and cam osteoplasties. An arthroscopic pump is used with pressures around 50 mm Hg with hypotensive general anesthesia. The operative hip is placed in 10° of flexion, 20° of abduction (with a padded groin post toward the operative hip), and typically about 30° to 40° of internal rotation (varying with femoral version, bony architecture, and/or capsuloligamentous laxity or restraint). This internally rotated starting position aids access to the anterior central compartment and facilitates posterior femoroplasty by bringing the posterosuperior head-neck junction into the arthroscopic field of view.
After hip distraction, interportal capsulotomy is performed. Relatively more capsule is resected when calcific metaplasia is detected and/or in cases of global pincer and cam FAI. Minimal capsulectomy is performed in patients with acetabular dysplasia, severe femoral anteversion, and/or hyperlaxity. If indicated, arthroscopic acetabuloplasty and labral refixation or reconstruction is performed. Traction of the operative hip and counter-distraction are released. The hip is maintained in relative extension (10° of flexion), and the junction between the normal femoral head articular cartilage and cartilage overlying the cam deformity is demarcated under arthroscopic and fluoroscopic guidance. An initial outline of the planned cam resection is “drawn” with a radiofrequency probe. Posterior femoroplasty begins with the burr in the MMAP. The posterolateral retinacular vessels (Fig 3) are visualized before arthroscopic posterior femoroplasty to avoid inadvertent damage. A 5.5-mm round or flat-top burr (Flat Top burr; Smith & Nephew, Andover, MA) is then used beginning at the superior head-neck junction with care taken to remain proximal to the posterolateral vessels (Fig 4). The initial hip internal rotation and relative extension aid arthroscopic exposure of the superior (and posterosuperior) femoral head-neck junction. Transient reapplication of hip traction (without counter-distraction) is occasionally performed to improve access to the proximal extent of the femoroplasty if it is “covered” by the acetabular rim. Once superior femoroplasty is completed, we perform posterior cam resection, taking advantage of the lowered “floor” of the femoral head-neck junction to improve arthroscopic visualization. Staying proximal to the posterolateral extraosseous vasculature, the surgeon completes the arthroscopic posterior femoroplasty (Fig 5), taking care to avoid unnecessary stress risers that could excessively weaken the tensile side of the proximal femur or excessive bone resection that might compromise in vivo labral fluid seal function. Table 1 lists the key points of the arthroscopic posterior femoroplasty procedure.
Fig 3.
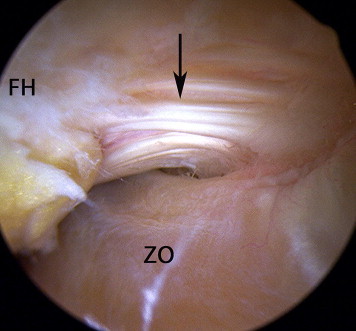
Supine arthroscopic view of patient's right hip viewed from anterolateral portal with a 70° arthroscope directed posteriorly, showing posterolateral retinacular vessels (arrow) and adjacent zona orbicularis (ZO). The femoral head (FH) region is shown for reference.
Fig 4.
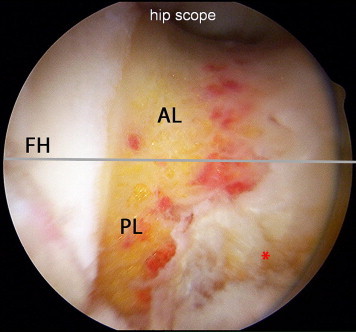
Supine arthroscopic view after arthroscopic posterolateral (PL) femoroplasty has been “blended” with subsequent anterolateral (AL) and anteromedial femoroplasties for complete cam decompression. One should note the posterior cam resection well beyond the virtual threshold (gray line) of the vascular safe zone and the proximal location of the femoroplasty relative to the posterolateral vasculature (asterisk). (FH, femoral head.)
Fig 5.
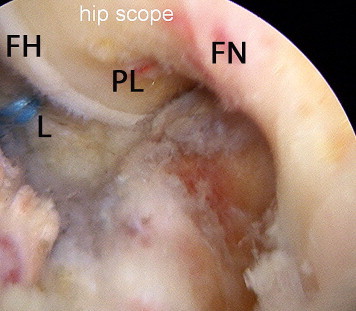
Supine arthroscopic view with 70° arthroscope aimed posteriorly showing area of posterior cam decompression (PL), femoral head (FH) and neck (FN), and posterolateral labrum (L), which has undergone refixation.
Table 1.
Keys to Arthroscopic Posterior Femoroplasty
| Step | Rationale |
|---|---|
| Perform central-compartment diagnostics | Arthroscopy confirms whether posterior acetabular chondrolabral pathology is present. |
| Perform any indicated acetabuloplasty | Reduction of coexisting acetabular overcoverage aids proximal femoroplasty of posterosuperior femoral head-neck junction. |
| Begin femoroplasty without traction with hip in relative extension and internal rotation | This hip position brings posterosuperior femoral head-neck junction into arthroscopic field of view. |
| Visualize posterolateral vessels | Iatrogenic direct damage to main vascular supply to femoral head is avoided. |
| Begin with superior femoroplasty | Better arthroscopic visualization is enabled as the “floor” of superior bony resection is lowered for subsequent improved posterior femoroplasty. |
| Perform proximal posterosuperior femoroplasty | Iatrogenic direct damage to main vascular supply to femoral head is avoided. |
| Add transient hip distraction (optional) | Transient hip distraction can be added if more proximal cam decompression is needed. |
| Seamless progression to anterior femoroplasty | Stress risers are minimized as femoroplasty continues into anterolateral and possibly anteromedial regions for complete cam decompression with progressive hip flexion and external rotation. |
| Obtain fluoroscopic confirmation on AP view with neutral and internal hip rotation | Arthroscopic confirmation of sufficient posterosuperior cam decompression is facilitated. |
Anterolateral and, if needed, anteromedial femoroplasty is then seamlessly performed in an incremental manner in mid flexion with increasing amounts of external rotation, with intermittent arthroscopic dynamic examinations. We desire 120° of hip flexion; 30° or, preferably, 40° of flexed hip internal rotation; and unobstructed figure-of-4 or FABER testing. Optimal arthroscopic visualization during dynamic testing and incremental femoroplasty is facilitated by fine-tuning the suction outflow level on the adjacent burr. Further burr resection is readily performed until impingement-free motion is confirmed. The arthroscopic lens is then aimed posteriorly to assess eradication of posterosuperior impingement, and AP fluoroscopic views in neutral and internal rotation (with the lesser trochanter in profile) are obtained for confirmation. Video 1 highlights key principles and technical pearls and pitfalls of arthroscopic posterior cam decompression.
Discussion
Posterior (or perhaps more accurately posterosuperior) femoroplasty may be performed with arthroscopic techniques while avoiding the extraosseous posterolateral retinacular vessels supplying the femoral head. Our technique is efficient and adds perhaps 10 minutes to our surgery time. The MMAP enables a seamless transition from central-compartment to peripheral-compartment surgery without interportal exchange of the arthroscope or instruments. Maintaining the hip in the original setup position simplifies an inherently challenging procedure. Relative hip extension (10° of flexion) rather than the typical mid-flexed position facilitates visualization of the superior femoral head-neck junction and permits the safe reapplication of hip distraction if needed. Sciatic palsy is more likely with traction applied to the mid-flexed hip. Hip internal rotation, likewise maintained, enables visualization and controlled osteoplasty of the posterosuperior quadrant and avoids external rotation, which may compromise blood flow to the femoral head during open surgical dislocation.21
Although the adequacy (or inadequacy) of posterosuperior cam decompression may be assessed with postoperative 3-dimensional computed tomographic reconstructions, we typically use standard postoperative radiographs. On an AP projection, a gradual concavity at the superior femoral head-neck junction (Fig 6) should replace the preoperative pistol-grip convexity.
Fig 6.
Detail of postoperative AP pelvis radiograph showing the area of posterosuperior cam decompression (concave part of blue line) that would not be seen with femoroplasty remaining anterior to the mid-coronal plane. One should also note the presence of some acetabular rim reduction.
We are not aware of any reported instances of osteonecrosis from documented direct damage to the retinacular vessels from open, mini-open, or arthroscopic femoroplasty. Theoretically, osteonecrosis after hip arthroscopy may result from traction on vessels supplying the femoral head, direct injury to such vessels during portal entrance, raised intra-articular pressure, prolonged operating time, and damage to vessels during bony resection or osteochondroplasty for FAI. Isolated case reports of osteonecrosis after hip arthroscopy have been reported in non-femoroplasty cases and have been attributed to vascular compromise from traction22-24 and/or excessive intra-articular fluid pressure.23 Recent anatomic studies suggest variable contribution to femoral head vascularity from the inferior gluteal artery.25 Along with typically 2 to 4 posterolateral retinacular vessels and possible collateral circulation, the femoral head may be somewhat “protected” from vascular insult. However, we emphasize the need to respect the extraosseous posterolateral vasculature, performing posterior cam resection only when deemed necessary and remaining proximal to these vessels in such instances. The visualization of pulsatile bleeding from a single retinacular vessel should prompt the immediate cessation of any further posterior cam decompression regardless of approach, and one should stay proximal to any visualized vascular foramina.26
One may reasonably question whether any gain in posterior cam decompression is worth the potential risk of osteonecrosis (whether performed in an open manner or arthroscopically). Further clinical investigation is required to answer this. However, we believe that the arthroscopic visualization of the posterolateral vessels with subsequent posterior femoroplasty proximal to these vessels is a less invasive option to open surgical dislocation of the hip, eliminating the risk of trochanteric nonunion or the more common need for postoperative hardware removal. We do not believe that direct open visualization offers an advantage over controlled arthroscopic femoroplasty because the resection is in the same region and more distal resection is not gained with the former method because of the same limiting vascular anatomy. However, we believe that this arthroscopic equivalent should be performed by surgeons with significant experience in arthroscopic anterior cam decompression. The avoidance of direct damage to the posterolateral vasculature may not ensure the prevention of osteonecrosis; excessive traction time and force27 and excessive arthroscopic fluid pressures must also be avoided.
No longer is the pistol-grip deformity an obligatory indication for open surgical hip dislocation. Posterior cam decompression through controlled arthroscopic femoroplasty of the posterosuperior femoral head-neck junction is a challenging but feasible procedure. The key is to remain proximal to the posterolateral retinacular vessels regardless of the preferred method.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Key principles and technical pearls and pitfalls of arthroscopic posterior cam decompression.
References
- 1.Matsuda D.K., Carlisle J.C., Arthurs S.C., Wierks C.H., Philippon M.J. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27:252–269. doi: 10.1016/j.arthro.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Botser I.B., Smith T.W., Jr., Nasser R., Domb B.G. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: A comparison of clinical outcomes. Arthroscopy. 2011;27:270–278. doi: 10.1016/j.arthro.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Audenaert E.A., Mahieu P., Pattyn C. Three-dimensional assessment of cam engagement in femoroacetabular impingement. Arthroscopy. 2011;27:167–171. doi: 10.1016/j.arthro.2010.06.031. [DOI] [PubMed] [Google Scholar]
- 4.Bedi A., Dolan M., Hetsroni I. Surgical treatment of femoroacetabular impingement improves hip kinematics: A computer assisted model. Am J Sports Med. 2011;39:43S–49S. doi: 10.1177/0363546511414635. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A., Dolan M., Magennis E., Lipman J., Buly R., Kelly B.T. Computer-assisted modeling of osseous impingement and resection in femoroacetabular impingement. Arthroscopy. 2012;28:204–210. doi: 10.1016/j.arthro.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Matsuda DK, Calipusan CP, Burchette, MS. The critical corner of cam femoracetabular impingement: An arthroscopic pilot study. e-Poster 727. ISHA Annual meeting, Boston, MA, Sept 27-29, 2012.
- 7.McCormick F., Kleweno C.P., Kim Y.J., Martin S.D. Vascular safe zones in hip arthroscopy. Am J Sports Med. 2011;39(suppl):64S–71S. doi: 10.1177/0363546511414016. [DOI] [PubMed] [Google Scholar]
- 8.Dudda M., Albers C., Mamisch T.C., Werlen S., Beck M. Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res. 2009;467:651–659. doi: 10.1007/s11999-008-0617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barton C., Salineros M.J., Rakhra K.S., Beaulé P.E. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469:464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Konan S., Rayan F., Haddad F.S. Is the frog lateral plain radiograph a reliable predictor of the alpha angle in femoroacetabular impingement? J Bone Joint Surg Br. 2010;92:47–50. doi: 10.1302/0301-620X.92B1.22359. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda D.K. The case for cam surveillance: The arthroscopic detection of cam femoroacetabular impingement missed on preoperative imaging and its significance. Arthroscopy. 2011;27:870–876. doi: 10.1016/j.arthro.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Signorelli C., Lopomo N., Bonanzinga T. Relationship between femoroacetabular contact areas and hip position in the normal joint: An in vitro evaluation. Knee Surg Sports Traumatol Arthrosc. 2013;21:408–414. doi: 10.1007/s00167-012-2151-y. [DOI] [PubMed] [Google Scholar]
- 13.Beaulé P.E., Zaragoza E., Motamedi K., Copelan N., Dorey F.J. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 14.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 15.Heyworth B.E., Shindle M.K., Voos J.E., Rudzki J.R., Kelly B.T. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Jäger M., Bittersohl B., Zilkens C. Surgical hip dislocation in symptomatic cam femoroacetabular impingement: What matters in early good results? Eur J Med Res. 2011;16:217–222. doi: 10.1186/2047-783X-16-5-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Byrd J.W., Pappas J.N., Pedley M.J. Hip arthroscopy: An anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy. 1995;11:418–423. doi: 10.1016/0749-8063(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 18.Matsuda D.K. Protrusio acetabuli: Contraindication or indication for hip arthroscopy? And the case for arthroscopic treatment of global pincer impingement. Arthroscopy. 2012;28:882–888. doi: 10.1016/j.arthro.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 19.Matsuda D.K. Arthroscopic labral reconstruction with gracilis autograft. Arthrosc Tech. 2012;1:e15–21. doi: 10.1016/j.eats.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuda D.K. Fluoroscopic templating technique for precision arthroscopic rim trimming. Arthroscopy. 2009;25:1175–1182. doi: 10.1016/j.arthro.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 21.Nötzli H.P., Siebenrock K.A., Hempfing A., Ramseier L.E., Ganz R. Perfusion of the femoral head during surgical dislocation of the hip. Monitoring by laser Doppler flowmetry. J Bone Joint Surg Br. 2002;84:300–304. doi: 10.1302/0301-620x.84b2.12146. [DOI] [PubMed] [Google Scholar]
- 22.Scher D.L., Belmont P.J., Jr., Owens B.D. Case report: Osteonecrosis of the femoral head after hip arthroscopy. Clin Orthop Relat Res. 2010;468:3121–3125. doi: 10.1007/s11999-010-1256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sener N., Gogus A., Akman S., Hamzaoglu A. Avascular necrosis of the femoral head after hip arthroscopy. Hip Int. 2011;21:623–626. doi: 10.5301/HIP.2011.8693. [DOI] [PubMed] [Google Scholar]
- 24.Sampson T.G. Complications of hip arthroscopy. Clin Sports Med. 2001;20:831–835. doi: 10.1016/s0278-5919(05)70288-x. [DOI] [PubMed] [Google Scholar]
- 25.Kalhor M., Horowitz K., Gharehdaghi J., Beck M., Ganz R. Anatomic variations in femoral head circulation. Hip Int. 2012;22:307–312. doi: 10.5301/HIP.2012.9242. [DOI] [PubMed] [Google Scholar]
- 26.Dy C.J., Thompson M.T., Usrey M.M., Noble P.C. The distribution of vascular foramina at the femoral head/neck junction: Implications for resurfacing arthroplasty. J Arthroplasty. 2012;27:1669–1675. doi: 10.1016/j.arth.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 27.Telleria J., Safran M., Gardi J., Harris A.H.S., Glick J. Traction injury risk in hip arthroscopy—Duration or amount? An intraoperative nerve monitoring study (SS-42) Arthroscopy. 2012;28:e23–e24. doi: 10.2106/JBJS.K.01597. (abstr) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Key principles and technical pearls and pitfalls of arthroscopic posterior cam decompression.


