Abstract
Men who have sex with men (MSM), especially MSM of color, are disproportionately impacted by HIV/AIDS compared to heterosexuals and Caucasians. Nonetheless, fewer sexual and ethnic minorities participate in prevention interventions for people with HIV. We consider recruitment for Positive Connections, a randomized controlled trial comparing unsafe sex prevention interventions primarily for HIV-positive (HIV+) MSM in six US epicenters. One community-based organization (CBO) in each city recruited adult MSM, particularly men of color and HIV+. Recruitment methods included on-line and print advertising, outreach events, health professionals, and social networks. Data on demographics, HIV status, and recruitment method were collected at registration. We tested for differences in registration proportions and attendance rates by recruitment strategy, stratified on race/ethnicity and serostatus. Of the 1,119 registrants, 889 attended the intervention. The sample comprised 41% African American, 18% Latino/Hispanic, and 77% HIV+. Friend referral was reported by the greatest proportion of registrants, particularly among African American (33%) and HIV+ men (25%). Print advertising yielded the largest proportions of non-Hispanic white (27%) and HIV-negative registrants (25%). Registrants recruited on-line were the least likely to attend (45% versus 69% average); this effect was strongest among Latino/Hispanic (27% attendance) and non-Hispanic white men (36%). Retention during the follow-up period did not differ by serostatus, race/ ethnicity, or recruitment method. Differential attendance and retention according to recruitment strategy, serostatus, and racial/ethnic group can inform planning for intervention sample size goals.
Keywords: Recruitment, Men who have sex with men (MSM), HIV-positive, Minorities
Introduction
In the USA, men who have sex with men (MSM) and, in particular, men of color—specifically African Americans and Latinos—are disproportionately impacted by HIV/ AIDS (Diaz et al. 2001; McCree 2009; Valleroy et al. 2000). Indeed, both African American and Latino MSM account for an increasingly large proportion of AIDS cases, and have the highest mortality rate amongMSM (Diaz et al. 2001; Peterson and Jones 2009). Unfortunately, proportionately fewer HIV-positive (HIV+) African American or Latino MSM participate in behavioral interventions for HIV+ individuals than do Caucasians or heterosexuals (Cargill and Stone 2005; Centers for Disease Control and Prevention 2001, 2005; Yancey et al. 2006).
Given the diversity exhibited by members of racial and ethnic minority groups, it should come as no surprise that no one factor has been consistently associated with the failure to meet recruitment goals in HIV behavioral interventions in these populations (Durant et al. 2007). However, a review of the literature highlights a number of issues, which have been reported by both participants and non-participants during the screening process. Racial minority groups report that the two most prominent barriers to participation in prevention interventions for HIV+ individuals are distrust of the research process and the cultural insensitivity of the recruitment methods (Centers for Disease Control and Prevention 2005; Corbie-Smith et al. 1999; UyBico et al. 2007). It is difficult to estimate the size of the MSM population, in part because MSM may be unwilling to disclose their sexual behaviors because of internalized homonegativity or the desire to avoid being identified as gay (Ross et al. 2008). Therefore, it is challenging to measure whether efforts to recruit HIV+MSM have been effective. To the extent that MSM who agree to participate in prevention interventions for HIV+ individuals are different from the men who do not, there is a potential for selection bias.
Only one intervention for HIV+ individuals reported barriers to recruitment (Rotheram-Borus et al. 2004). The major barrier reported was the difficulty of identifying HIV+ people who did not know they were infected. Consequently, recruitment efforts were restricted to those who were already receiving treatment at AIDS clinics or community-based organizations—with considerable limitations to generalizability.
Crafting best practices for recruiting HIV+ racial and sexual minority populations is a necessary first step towards increasing their participation in prevention-for-positive intervention studies (Murthy et al. 2004; National Institutes of Health 1994). However, very little research has been conducted on the best methods to recruit these HIV+ populations (Lai et al. 2006; Silvestre et al. 2006). A search of the literature revealed no study that directly addressed the issues encountered when recruiting HIV+ racial and sexual minority populations.
This paper attempts to address the research gap by describing strategies found to be effective for the recruitment and retention of a large sample of HIV+ MSM of color in the parent study, the Positive Connections trial. The primary aims of this paper are to (1) compare the effectiveness of various recruitment methods used in Positive Connections, (2) examine differences in method effectiveness by serostatus and race/ethnicity, and (3) report average costs associated with each recruitment method.
Methods
Design of the Parent Study: The Positive Connections Trial
The Positive Connections study is a randomized controlled trial based on the Sexual Health Model (Robinson et al. 2002), which posits that sexually healthy persons will be more likely to make sexually healthy choices. The trial was designed to test two hypotheses. First, a sexual health approach is more affective in reducing high-risk sexual behavior among HIV+ MSM than is a traditional HIV prevention approach. Second, interventions that target HIV+ MSM exclusively are more effective in reducing high-risk sexual behavior of HIV+ MSM than interventions designed for all MSM. The trial randomized participants to one of two sexual health interventions or a contrast condition. These behavioral interventions were as follows:
Man2Man (M2M)
A 2-day, 14- to 16-h weekend intervention designed to help all MSM identify and address their sexual health and HIV risk concerns. M2M used a large-group format, supplemented by facilitated small group discussions. This arm included both HIV-negative (HIV−) and HIV+ MSM so that it could be compared to the intervention targeting HIV+ MSM only (below) as a test of Hypothesis 2. The seronegative men were not the subjects of interest for the parent study, but we consider them here.
Positive Sexual Health (PoSH)
Modeled on M2M, PoSH was designed to address HIV risk from the perspective of HIV+ MSM. It also used a large and small group format and was limited to HIV+ participants only.
Men Speaking Out (MSO)
A 3-h group session where participants evaluated six HIV prevention DVDs tailored for MSM. There were no sexually explicit videos, no exercises to help participants contextualize information, no large or small group discussions, and group interaction was kept to a minimum. This arm included only HIV+ participants.
The parent study was implemented in six US cities: Seattle, WA; Washington, DC; Boston, MA; New York, NY; Los Angeles, CA; and Houston, TX. These cities were chosen on the basis of high HIV infection rates among MSM and the availability of partner organizations in each city. Our research team at the University of Minnesota contracted with one community-based organization (CBO) per epicenter city, referred to in this paper as Partner CBOs. We outsourced recruitment to these entities because they were familiar with the local MSM population. Criteria for CBO selection included history of working with MSM, particularly HIV+ MSM of color; favorable reputation in the community; and availability to perform study tasks.
Each seminar was conducted during one weekend by a team comprised of gay-identified health professionals, CBO staff, and community members, all overseen by University of Minnesota research staff. African American and Latino staff members were asked to participate in all aspects of the recruitment process to make it more culturally relevant to potential participants. The seminars were held in the local CBO buildings or in a hotel if that space proved insufficient.
The trial recruited MSM who were 18 years or older, reported at least one occasion of unprotected anal intercourse (UAI) with a man in the past year, spoke English, and were available to attend both days of the weekend trial. Men were excluded from participation if they had attended a M2M seminar within the past 2 years, were uncomfortable viewing sexually explicit videos and material, or were cognitively impaired.
The research was approved by the University of Minnesota and community Institutional Review Boards, and the seminars by the local Community Planning Boards (as appropriate).
Recruitment
Recruitment was carried out by the six CBOs, and began 8 weeks before the seminar’s scheduled date (Fig. 1). Recruitment plans were developed in collaboration with partner CBOs. These detailed all aspects of recruitment: advertising, promotional materials, phone screening, registration, internal resources, collaboration with external organizations, and goals for number of participants to be registered. Each CBO chose to emphasize those strategies that would resonate with the local MSM culture and yield the greatest number of target population members.
Fig. 1.
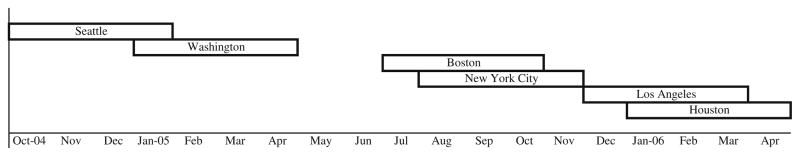
Timeline of the recruitment process by city
The six CBOs spent roughly $142,250 over the 18-month recruitment period. Each city sought to enroll a sample that was more than half men of color. The goal was to enroll 696 HIV+ MSM and 258 HIV− MSM across the six cities (116 and 43 per city, respectively). With a predicted attrition rate of approximately 30%, the retained sample size at 18 months was predicted to be 487 HIV+ MSM and 181 HIV− MSM. In order to collect information on HIV+ MSM of color, we planned to over-sample MSM of color so they would make up between 50% and 60% of the overall sample.
Each of the partner CBOs implemented the following eight recruitment strategies:
Poster and palm cards
Partner CBO staff distributed informational posters and palm cards (post cards) that described the seminar and requested that interested participants contact the local CBO for further information. Materials were distributed at GLBT events and local gay venues such as bars, cafes, community centers, gyms, and bookstores. Approximately $5,000—or 4% of the total cost of recruitment—was spent on these materials for the entire study across all six cities.
Newspapers and magazines
Advertisements were placed in local gay newspapers and magazines with circulation that included men of color. Roughly $22,750 (16% of total expenditures) was spent across all cities.
Partner CBO outreach
Our Partner CBOs reached potential participants through their websites, newsletters, and email listserv. Local staff set up informational tables inside their building, met with people face-to-face at group meetings and CBO events, and placed advertising material around their offices where it could be seen by potential participants. CBO staff also recruited participants through community contacts and by outreach at local community events, gay venues, and gay neighborhoods. CBO outreach staff and other on-site personnel across cities were compensated approximately $108,500 (76% of total recruitment expenditures) for their recruitment-related work.
Partner CBO health professionals
Partner CBOs also recruited participants among the clients of their in-house healthcare professionals (e.g., mental health counselors, physicians, social workers, case workers, and other HIV healthcare providers). No compensation was offered to this specific group.
Other health professionals
Local staff also recruited participants via healthcare professionals and clinics outside of their CBO. This additional outreach required approximately $3,000 (2% of total expenditures) across the cities.
Other CBOs
CBO staff collaborated with other local CBO and AIDS service organizations by hosting informational luncheons and meeting with staff members who worked directly with HIV+ MSM. Expenses from these methods totaled approximately $3,000 (2% of total expenditures) across all six cities.
Friend referral
After participants were successfully screened, CBO staff encouraged them to refer friends who they thought would benefit from the seminar. Friend referrals also were generated from word-of-mouth communication in both gay and HIV+ communities. No compensation was provided to these referrers.
On-line ads and social networking
CBO staff members from Boston, New York, Los Angeles and Houston advertised the seminars through craigslist.org and manhunt.net. These sites were chosen because they are widely known and used by MSM, and allow recruitment to be tailored to the MSM culture of individual cities. Also, CBO staff posted information on blogs and participated in on-line discussions to target potential participants. These listings were free of charge.
Procedures
Potential participants were contacted, screened, and registered by staff of the partner CBOs. At screening, interested men received a description of the study over the phone. Local CBO staff informed potential participants that they would be expected to attend a 14- to 16-h seminar over one weekend and complete five questionnaires: one before the intervention, one immediately after, and three via mail at 6, 12, and 18 months after the intervention. They were told that all information provided would be strictly confidential and that they would receive up to $200 compensation for their time ($100 after completing the intervention, $25 for each follow-up survey, and $25 bonus for completing all surveys). After describing the study, staff asked interested men a series of screening questions to determine eligibility. Potential participants were informed of eligibility only after all screening questions were answered to avoid alerting them to specific requirements for participation in the seminars. Men who met eligibility requirements and indicated they would like to participate were registered for the seminar and sent a confirmation letter with the location and details of the weekend seminar.
On the day of the seminar, attending registrants and eligible men who attended as “walk-up” participants were asked to read and sign the consent form prior to completing a preseminar questionnaire. These paper questionnaires were completed in a group setting, with study staff on hand to assist as needed. After completion of the baseline questionnaire, participants received their randomization assignment to one of the three interventions. Upon completion of the weekend seminar and post-seminar questionnaire, participants received a $100 honorarium in cash. They also provided contact information for two other people so they could remain connected to the study even if they moved.
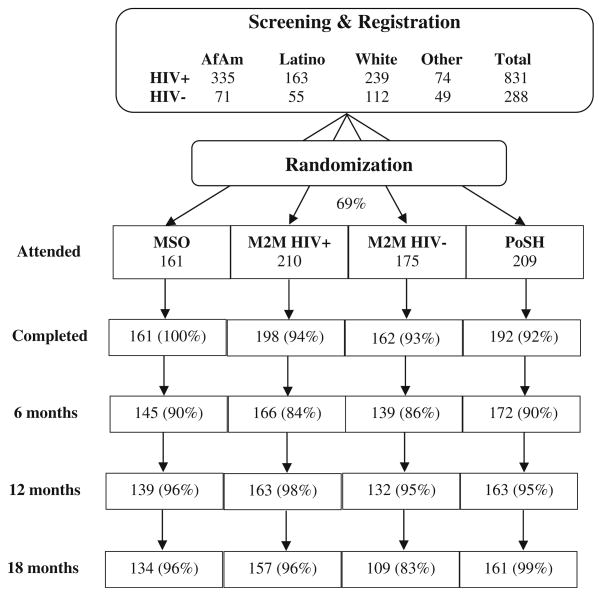
Follow-up data collection occurred via mailed questionnaires at 6, 12, and 18 months following the weekend seminars. Follow-up questionnaires were only sent to men who completed the post-intervention questionnaire. Followup questionnaires were coordinated by research staff at the University of Minnesota. Two weeks prior to each mailing, participants received a telephone call or email to notify them that a follow-up questionnaire would be arriving in the mail with a return-addressed, stamped envelope. If participants did not return the follow-up questionnaires within 3 weeks, they received an email or letter reminder. Additionally, phone calls were placed to remind participants of the questionnaire and offer assistance. If participants could not be reached after three phone calls, alternate contacts were phoned. The flow of participants through these study procedures is summarized in Fig. 2. Data were not collected consistently on screened men who were ineligible or declined to register for other reasons. Note that 110 unregistered “walk-up” participants were not asked how they heard about the study. These men and the 34 registrants who did not provide data on how they heard about the study are not considered below, as our analyses are concerned with recruitment methods.
Fig. 2.
Number of men active at each phase of the parent study. The percentages in each box represent the proportion of men progressing between study phases. Walk-up enrollees and registered men with missing recruitment method data are excluded from this figure
Throughout this paper, we distinguish among men who met the eligibility criteria and pre-registered for the seminar (registrants), men who attended the weekend intervention and signed the consent form on the first day of the seminar (attendees), and men who completed the intervention and thus received follow-up mailings (completers).
Measures
Recruitment method
Potential participants were asked during the screening process how they heard about the study. Their answers were entered into the recruitment database by local staff and later coded by U of M research staff into the following eight categories: (1) Poster/Palm Card, (2) Newspaper/Magazine, (3) Partner CBO Outreach, (4) Partner CBO Health Professional, (5) Other Health Professional, (6) Other CBO, (7) Friend Referral, and (8) On-line Ads/Social Networking Sites.
Recruitment success
The number of active participants in the study was tallied at six time points during the study: (1) registration, which usually occurred via telephone; (2) baseline, when participants completed a questionnaire immediately prior to the seminars; (3) post-test, when participants completed a second questionnaire in person; and (4, 5, 6) follow-up at 6, 12, and 18 months, when questionnaires were mailed to and returned by participants. Although these activities were timed similarly in each city (i.e., 8 weeks for recruitment, a single weekend seminar, and 18 months of additional follow-up), they were completed at a different point in calendar time, as summarized in Fig. 1.
Demographics
Demographic variables included race/ ethnicity, city, and HIV status (positive or negative). The race question included the categories used by the US Census Bureau: American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, and White. Also following Census standards, the ethnicity question asked participants to characterize themselves as Hispanic/Latino or not. For purposes of the present analyses, participants were collapsed into four groups: non-Hispanic African American/ Black, non-Hispanic White, Hispanic/Latino (any race), and Other/Multiple race/ethnicity (hereafter, Other/ Multi). The last group comprises men who indicated either a) any single race other than African American or White (non-Hispanic) or b) multiple racial categories (non-Hispanic).
Statistical Analysis
The primary outcome variable was whether a participant was active in the study at a given time point. We report both counts and proportions (rates). The denominator for attendance rate is the number of men who registered. The denominator for completion rate is the number of men who attended the first day of the seminar (i.e., baseline). The denominator for retention rate at 6, 12, and 18 months is the number of men who completed the seminar and immediate post-test questionnaire, since only these participants received follow-up mailings.
The Pearson Chi-square statistic was used to test independence between two categorical variables. When small cell counts made the asymptotic distribution of the test statistic unreliable, p-values were obtained by Monte Carlo simulation using 2000 simulated values (Hope 1968). When an overall test was significant, we identified cells with large (greater than 1.96 in absolute value) standardized residuals (R = [Observed − Expected]/ sqrt [Expected]) in the contingency table. Thus, we identified combinations of the two variables that contributed to the overall significance without the need for all possible posthoc comparison tests.
Results
Overall, recruitment and retention methods were successful in obtaining the sample size estimated for adequate power in Positive Connections. During the trials, we screened approximately 1,695 MSM (67% of whom were of color), registered 1,119 potential participants, and obtained consent from 675 HIV+ MSM and 214 HIV− MSM on the day of the intervention (52% attendance rate). Of these, 69% were MSM of color. At the end of the trials, we retained 527 HIV+ MSM (with 78% retention rate across the three condition arms) and 131 HIV− MSM (with 61% retention rate across the three arms). Of these, 71% were MSM of color.
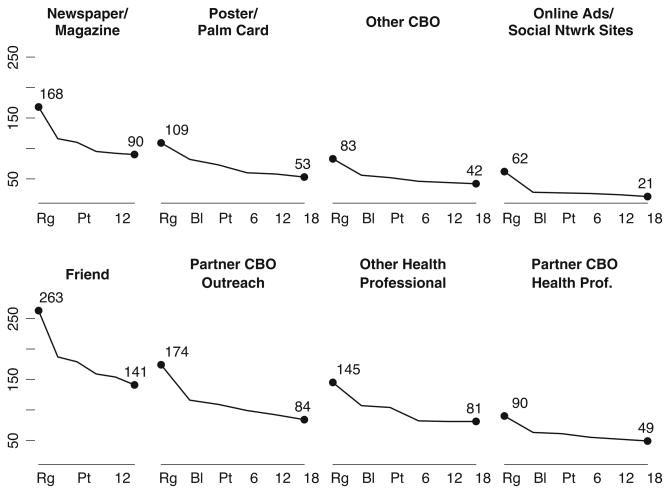
Number of Participants Recruited by Method
Figure 3 reports the number of men active in the study at each time point according to the method by which they were originally recruited. The top row comprises recruitment methods that relied on less personal means (i.e., advertising), while the bottom row contains more personal recruitment methods. Within each of these two broad groups, the plots are sorted in decreasing order of number of registrants reporting that method.
Fig. 3.
Number of participants active in the study at each observation point plotted by recruitment method. Top row shows advertising-based recruitment methods and the bottom row shows in-person recruitment methods. Rg = registration, Bl = baseline, Pt = immediate postintervention, 6=6 months, 12= 12 months, 18=18 months
The method that yielded the most registrants was Referral by a Friend, followed by Partner CBO Outreach, Newspapers/ Magazines, and Other Health Professionals. In general, the personal methods garnered more registrants than the advertising methods.
Comparison of Retention Across Recruitment Methods
The greatest reduction in the sample size occurred when registered men failed to attend the seminar. This is seen by steep negative slopes at the beginning of each line in Fig. 3.
Method of recruitment was associated with attendance (χ2=21.1; 7 df; p=0.004). We found that seminar attendance rate of men who reported On-line recruitment was 24 percentage points below the average attendance (45%, compared to 69%, R=−2.3).
At the four subsequent observation points (post-seminar, 6, 12, 18 months), the proportions of men active in the study who had been originally recruited by each of the eight methods were similar to the baseline proportions. That is, attrition during and after the seminar was similar among men recruited across all methods.
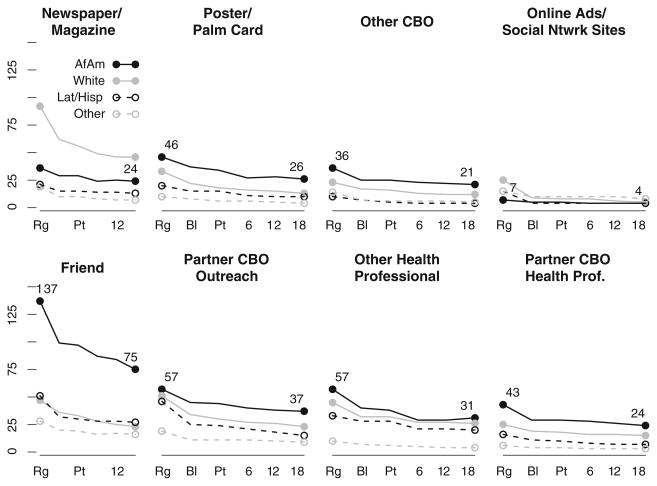
Stratifying Registration and Attendance by Race
Figure 4 presents the number of men active in the study according to the method by which they were recruited and their race/ethnicity. We observed differences in the method of recruitment reported by registered men according to race/ ethnicity (χ2=118.4; 21 df; p-value<0.001). In particular, African American registrants were more likely than expected to report recruitment by a Friend (33%, R=3.6) and less likely to report Newspaper (9%, R=−3.5) or Online (2%, R=−3.4) recruitment. White registrants were more likely than expected to report recruitment by Newspaper/Magazine (27%, R=5.5) and less likely to report Friend recruitment (14%, R=−3.9). Men of other/ multiple race/ethnicity reported Online recruitment in a greater than expected proportion (12%, R=3.1).
Fig. 4.
Number of participants active in the study at each observation point plotted by recruitment method and race/ethnicity. Dark solid lines are African American, light solid lines are white, dark dashed lines are Hispanic/Latino, and light dashed lines are men of other/ mixed race/ethnicity. Top row shows advertising-based recruitment methods and the bottom row shows in-person recruitment methods. Rg = registration, Bl = baseline, Pt = immediate post-intervention, 6= 6 months, 12=12 months, 18=18 months
Patterns of seminar attendance among registered men varied by race (χ2=8.2; 3 df; p-value<0.05). African American registered men had the highest attendance proportion (74%), but the standardized residual, the largest in the table, was only 1.2.
Further, we observed race/ethnicity-stratum-specific relationships between recruitment method and attendance of registered men. Among Latino men, attendance was associated with recruitment method (χ2=19.2, Monte Carlo p-value< 0.01). Those who reported On-line Ads/Social Networking recruitment had the smallest attendance rate (27%, non-attendance R=2.5), and those referred by Other Health Professionals had the greatest attendance rate (85%, non-attendance R=−1.95). Among non- Hispanic white men, we also observed significant differences (χ2=14.7, Monte Carlo p-value<0.05). Men who reported On-line Ads/Social Networking recruitment had smaller than expected attendance (36%, non-attendance R=2.8). African American and men of the Other/Multi group did not show differential attendance rates by recruitment method.
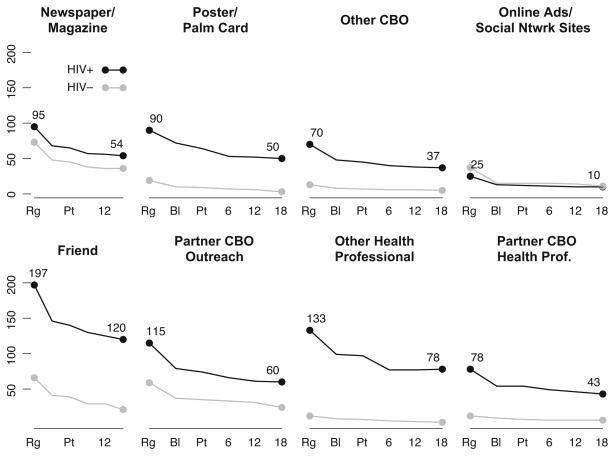
Stratifying Registration and Attendance by HIV Serostatus
Figure 5 shows the number of active study participants at each point by HIV serostatus and recruitment method. There was a significant association between method of recruitment and the serostatus of registered men (χ2= 107.1, 7 df, p-value<0.001). Greater than expected proportions of registered HIV− men reported recruitment by Newspaper/Magazine (25%, R=4.2) and Online Ads (13%, R=5.1). A larger proportion of registered HIV+ men than expected reported recruitment by Other Health Professionals (17%, R=2.6).
Fig. 5.
Number of participants active in the study at each observation point plotted by recruitment method and serostatus. Dark lines are HIV-positive subjects, light lines are HIVnegative subjects. Top row shows advertising-based recruitment methods and the bottom row shows in-person recruitment methods. Rg = registration, Bl = baseline, Pt = immediate postintervention, 6=6 months, 12= 12 months, 18=18 months
The seminar attendance rates of men differed by serostatus (χ2=13.0, 1 df, p-value<0.001). Registered HIV− MSM were significantly less likely to attend (60%, non-attendance R=2.6) than registered HIV+ MSM (72%). However, the recruitment methods were not significantly associated with seminar attendance in either serostatus group. That is, we observed no stratum effects of the sort seen for race/ethnicity above.
Discussion
Overall, the primary difference among recruitment methods appears between registration and attendance on the day of the weekend seminars. On-line Ads/Social Networking method was associated with significantly lower attendance compared to the other methods. The greatest number of seminar participants was recruited by a Friend, particularly in the HIV+ group. Completion of the seminars did not vary by recruitment method (as measured at post-test), and retention differences across methods throughout the follow-up were minimal. Hispanic/Latino men recruited by Other Health Professionals had the greatest attendance rate across the racial/ethnic categories and recruitment methods. Registered HIV− men were less likely to attend the seminar than HIV+ men, but were retained at comparable rates.
In this study, only basic word-of-mouth recruitment (i.e., suggesting that registered men encourage their friends to register for the seminar) was undertaken. Nonetheless, the utilization of pre-existing social networks seems to be more effective than mainstream marketing efforts for reaching marginalized and minority men, particularly African American and Latino MSM, and HIV+ MSM. Such a finding is not surprising, considering that these groups are stigmatized for their sexual behavior and/or health condition within their communities. Therefore, it is unlikely that they would openly admit their sexual orientation or serostatus to a CBO recruiter. This, in turn, reduces their chances of being invited to participate in an HIV prevention intervention. However, if the invitation to participate in an HIV prevention intervention comes through a friend— someone who is already familiar with the potential participant’s sexual orientation and serostatus—it is much more likely that the invitation will be accepted. Of course, this word-of-mouth utilization of existing social networks allows only for a convenience sample of MSM. However, as mentioned previously, MSM participants in all HIV prevention interventions are convenience samples because it is impossible to estimate the population size of MSM in a given area. Therefore, recruitment through a friend appears to be quite efficient in recruiting MSM into HIV prevention interventions (compared to other recruitment methods), and yet are not worse than other recruitment methods when it comes to sample representativeness.
The numbers of men recruited, enrolled, and retained by each method reflect a combination of the effectiveness of the method and the resources devoted to it. The approximate cost of each recruitment strategy, when combined with the number of participants who attended thanks to each method, indicates how cost-effective each method was. In particular, the free utilization of existing social networks to recruit under-represented African American and HIV+ MSM populations was promising.
The Positive Connections study recruited proportionately more HIV+ MSM than did other interventions that were tailored to serve the same population and used the same recruitment and retention strategies. However, its retention rates were similar to those reported for the other interventions. As mentioned before, 52% of all screened men attended the weekend intervention and 78% of HIV+ MSM were retained throughout the follow-up period. The Healthy Living Project enrolled 616 HIV+ MSM out of the 1,910 potential participants screened (32% enrollment rate), and retained 193 (64%) participants in the intervention and 232 (74%) in the wait-list control (Morin et al. 2008). The Seropositive Urban Men’s Intervention Trial (SUMIT) screened 1,922 potential participants and enrolled a total of 811 participants (42% enrollment rate). At the 3- and 6-month time points, the study had retained approximately 85% and 90% of the baseline sample, respectively (Wolitski et al. 2005).
We also compared Positive Connections to other prevention-for-positives interventions on the number of people of color recruited. At baseline, our sample was composed of 41% African Americans, 18% Latino and 10% Other/Multi. The intervention studies most similar to our own (Healthy Living Project and SUMIT) enrolled 36% and 23% African Americans, 14% and 17% Latino, and 8% and 9% Other/Multi, respectively (Morin et al. 2008; Wolitski et al. 2005). Neither of the two interventions purposefully planned to over-sample men of color. The Positive Connections study shows that such recruitment goals are feasible when they are planned a priori and carried out through tailored recruiting.
Other interventions varied in the proportion of people of color included. Differences are due to each study’s population of interest and geographical location. Proportions of African American participants vary between 83% in Georgia and Alabama among HIV+ women (Wingood et al. 2004) and 15% in California among HIV+ people engaging in unprotected intercourse (Patterson et al. 2003). Latino participants made up between 42%of the HIV+ youths sampled in California and New York (Rotheram-Borus et al. 2004) and 7% of the HIV+ substance abusers sampled in another California-based study (Sorensen et al. 2003). Calculating the proportion of other races and ethnicities in these studies is difficult because of the different compositions of this group. Indeed, some interventions do not report the number ofOther/Multi participants. However, where reported, the proportion of this group sampled varies between 2% among HIV+ blood donors (Cleary et al. 1995) and 9% among HIV+ MSM (Wolitski et al. 2005). Again, none of these studies reported intentionally over-sampling people of color into their intervention.
These comparisons underscore that participants of color can be recruited in adequate proportions into prevention-for- positives HIV interventions—if the target population reflects the desired ethnic compositions. If this is not the case, recruitment of minority populations is likely to remain deficient unless a specific recruitment plan for people of color is implemented. When recruiting MSM, these racial differences in enrollment are even more striking. White MSM seem to be less likely than MSM of other races to report internalized homonegativity (Ross et al. 2008). Therefore, they may be more willing to identify as gay and participate inMSM-tailored studies. Consequently, often they are better represented than other races in HIV interventions. In addition, the Positive Connection trial shows that it is possible to retain a considerable proportion of MSM of color throughout the study. This finding should assuage fears that the over-recruitment of racial minority MSM participants will lead to lower retention rates that those reported in a study where White MSM are the majority.
Therefore, to recruit a sample that is ethnically representative of the current HIV epidemic, future prevention-for- positives interventions should consider setting specific recruitment targets for each racial/ethnic group, as well as creating a targeted advertising campaign that is delivered by a well-known local CBO serving HIV+ MSM of color. These organizations can be invaluable in planning allocation of available recruitment resources and implementing the recruitment strategies in the local community. However, our experience suggests that if analysis of recruitment and retention data is anticipated, research staff—rather than CBOs—should undertake both screening and registration procedures to maintain consistency in data collection.
The major limitation of this paper is the post-hoc nature of the analysis. Since the primary purpose of Positive Connections was the evaluation of the seminar, we did not plan data collection with the intention of examining recruitment methods. Missing data include the characteristics and numbers of men screened but not registered, either for ineligibility or lack of interest; the intervention assignments of men who did not attend; and the recruitment method of walk-up enrollees. The results of this subanalysis are purely descriptive and should not be interpreted as suggesting causal inference.
A second limitation is the lack of detailed information on the recruitment efforts carried out in each city. University staff outsourced all recruitment efforts to the local CBOs because of their superior knowledge of the local MSM community. Therefore, we can report the funding that was allotted to the CBOs for each recruitment method, but not the cost of individual recruitment items.
A final limitation is the lack of information about recruitment and retention issues and methods for studies targeting HIV+ people. Consequently, it is not possible to draw firm parallels between the Positive Connections recruitment methods and those of other prevention-for--positives interventions, or to determine which ones were most efficient.
These results represent an initial contribution to addressing the gap in empirical research on recruitment methods for under-represented populations. We have seen that through a variety of methods it is possible to recruit and retain a large, racially diverse sample of men from a stigmatized sexual minority. From an intervention planning perspective, knowing attendance rates by method may improve the ability of hosting organizations to accurately plan for interventions. Future work should investigate the cost-effectiveness of these techniques more rigorously.
Acknowledgments
Positive Connections was funded by the National Institute of Mental Health, Office on AIDS Research, grant #MH064412. The Positive Connections Team comprises faculty, staff, and students at the University of Minnesota; consultants from AIDS Service Organizations and other universities who provided specialist guidance and direction; and a national leadership team of HIV-positive gay and bisexual men who partnered with this project at every stage from conceptualization to submission of findings. As a multi-site trial, this study was conducted under the oversight of the University of Minnesota Institutional Review Board (IRB), study # 0302S43321, and five other community-based IRBs. We acknowledge with gratitude our community-based partners and staff who included Howard Brown Health Center, Chicago, IL, USA; Gay City Health Project, Seattle, WA, USA; Whitman Walker Clinic, Washington, DC, USA; Fenway Community Health Center, Boston, MA, USA; Gay Men’s Health Crisis, New York, NY, USA; AIDS Project Los Angeles and Black AIDS Institute, Los Angeles, CA, USA; and Legacy Community Health Services, Houston, TX, USA.
Contributor Information
Laura A. Hatfield, Division of Biostatistics, University of Minnesota, Minneapolis, MN, USA
Margherita E. Ghiselli, Email: ghise001@umn.edu, Division of Epidemiology and Community Health, University of Minnesota, Minneapolis, MN, USA
Scott M. Jacoby, Program in Human Sexuality, Department of Family Medicine and Community Health, University of Minnesota Medical School, Minneapolis, MN, USA
Anne Cain-Nielsen, Division of Epidemiology and Community Health, University of Minnesota, Minneapolis, MN, USA.
Gunna Kilian, Division of Epidemiology and Community Health, University of Minnesota, Minneapolis, MN, USA.
Tara McKay, AIDS Project Los Angeles, Los Angeles, CA, USA. Department of Sociology, University of California, Los Angeles, CA, USA.
B. R. Simon Rosser, Division of Epidemiology and Community Health, University of Minnesota, Minneapolis, MN, USA
References
- Cargill V, Stone V. HIV/AIDS: A minority health issue. Medical Clinics of North America. 2005;89:895–912. doi: 10.1016/j.mcna.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV testing among racial/ethnic minorities—United States, 1999. Morbidity and Mortality Weekly Report. 2001;50:1054–1058. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV prevalence, unrecognized infection, and HIV testing among men who have sex with men: Five US cities, June 2004–April 2005. Morbidity and Mortality Weekly Report. 2005;54:597–601. [PubMed] [Google Scholar]
- Cleary PD, VaDevanter N, Steilen M, Stuart A, Shipton-Levy R, McMullen W, et al. A randomized trial of an education and support program for HIV-infected individuals. AIDS. 1995;9:1271–1278. doi: 10.1097/00002030-199511000-00009. [DOI] [PubMed] [Google Scholar]
- Corbie-Smith G, Thomas S, Williams S, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. Journal of General Internal Medicine. 1999;14:537–546. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz RM, Ayala G, Bein E, Henne J, Marin BV. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 US cities. American Journal of Public Health. 2001;91:927–932. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durant R, Davis R, George DS, Williams I, Blumental C, Corbie-Smith G. Participation in research studies: Factors associated with failing to meet minority recruitment goals. Annals of Epidemiology. 2007;17:634–642. doi: 10.1016/j.annepidem.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope ACA. A simplified Monte Carlo significance test procedure. Journal of the Royal Statistical Society Series B. 1968;30:582–598. [Google Scholar]
- Lai G, Gary T, Tilburt J, Bolen S, Baffi C, Wilson R, et al. Effectiveness of strategies to recruit underrepresented populations into cancer clinical trials. Clinical Trials. 2006;3:133–141. doi: 10.1191/1740774506cn143oa. [DOI] [PubMed] [Google Scholar]
- McCree DH. A plan of action for tackling HIV/AIDS among African Americans (Editorial) American Journal of Public Health. 2009;99:972. doi: 10.2105/AJPH.2009.162727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin SF, Shade SB, Steward WT, Carrico AW, Remien RH, Rotheram-Borus MJ, et al. the Healthy Living Project Team. A behavioral intervention reduces HIV transmission risk by promoting sustained serosorting practices among HIV-infected men who have sex with men. Journal of Acquired Immune Deficiency Syndromes. 2008;49:544–551. doi: 10.1097/QAI.0b013e31818d5def. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy V, Krumholz H, Gross C. Participation in cancer clinical trials: Race-, sex-, and age-based disparities. Journal of the American Medical Association. 2004;291:2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. NIH Guide. 1994. NIH guidelines on the inclusion of women and minorities as subjects in clinical research; p. 23. [Google Scholar]
- Patterson TL, Shaw WS, Semple SJ. Reducing the sexual risk behaviors of HIV+ individuals: Outcome of a randomized control trial. Annals of Behavioral Medicine. 2003;25:137–145. doi: 10.1207/S15324796ABM2502_10. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Jones KT. HIV prevention for black men who have sex with men in the United States. American Journal of Public Health. 2009;99:976–980. doi: 10.2105/AJPH.2008.143214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson BE, Bockting WO, Rosser BRS, Rugg DL, Miner MH, Coleman E. A sexological approach to HIV prevention: The sexual health model. Health Education Research. 2002;17:43–57. doi: 10.1093/her/17.1.43. [DOI] [PubMed] [Google Scholar]
- Ross MW, Rosser BRS, Neumaier ER. The relationship of internalized homonegativity to unsafe sexual behavior in HIV seropositive men who have sex with men. AIDS Education and Prevention. 2008;20:547–557. doi: 10.1521/aeap.2008.20.6.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Comulada WS, Weiss RE, Lee M, Lightfoot M. Prevention for substance-using HIV-positive young people: Telephone and in-person delivery. Journal of Acquired Immune Deficiency Syndromes. 2004;37:S68–S77. doi: 10.1097/01.qai.0000140604.57478.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvestre A, Hylton J, Johnson L, Houston C, Witt M, Jacobson L, Ostrow D. Recruiting minority men who have sex with men for HIV research: Results from a 4-city campaign. American Journal of Public Health. 2006;96:1020–1027. doi: 10.2105/AJPH.2005.072801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen JL, Dilley J, London J, Okin RL, Delucchi KL, Phibbs CS. Case management for substance abusers with HIV/AIDS: A randomized clinical trial. American Journal of Drug and Alcohol Abuse. 2003;29:133–150. doi: 10.1081/ada-120018843. [DOI] [PubMed] [Google Scholar]
- UyBico S, Pavel S, Gross C. Recruiting vulnerable populations into research: A systematic review of recruitment interventions. Journal of General Internal Medicine. 2007;22:852–863. doi: 10.1007/s11606-007-0126-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, et al. HIV prevalence and associated risks in young men who have sex with men. Journal of the American Medical Association. 2000;284:198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Mikhail I, Lang DL, McCree DH, Davies SL, et al. A randomized controlled trial to reduce HIV transmission risk behaviors and sexually transmitted diseases among women living with HIV: The WiLLOW program. Journal of Acquired Immune Deficiency Syndromes. 2004;37:S58–S67. doi: 10.1097/01.qai.0000140603.57478.a9. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Gomez CA, Parsons JT the SUMIT Study Group. Effects of a peer-led behavioral intervention to reduce HIV transmission and promote serostatus disclosure among HIV-seropositive gay and bisexual men. AIDS. 2005;19:S99–S109. doi: 10.1097/01.aids.0000167356.94664.59. [DOI] [PubMed] [Google Scholar]
- Yancey A, Ortega A, Kumanyika S. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]