Abstract
“Choosing Healthplans All Together”(CHAT) is a small group decision exercise designed to give the public a voice in priority setting in the face of unsustainable health care costs. It has been used for research, policy, and teaching purposes. Departments of insurance in various states in the United States have used CHAT to determine public opinion about what should be included in basic health insurance packages for the uninsured. Some municipalities have used it to assess public priorities for direct service delivery to the uninsured. Setting up the exercise requires substantial preparation, but the public finds it simple to use and understand.
Keywords: health priorities, insurance benefits, public participation
The united states is well known for citizen participation in government through democratically elected officials, town hall meetings, and other political mechanisms. While engagement of the US public in health decisions is less prevalent and less visible, a cross-national review (Health Canada, 2003) has noted efforts in the United States to promote public consultation in issues related to environmental health risk (Reeder, 2001), the quality of health care (Institute of Medicine, 1998), and personal health choices (http://www.ahd.org/AboutUs.html). Perhaps, one of the best known examples of public participation in health care decisions in the United States was the effort in the state of Oregon to engage the public in discussion of priorities when the state planned to expand coverage for low-income residents through its Medicaid program while eliminating coverage for some treatments (Jacobs et al., 1999).
It is useful to consider public involvement in health decisions as falling under several categories (Health Canada, 2003): identification of values to guide health care; individual participation in clinical care decisions; planning and development of health care; governance (including regionalization, resources allocation/priority setting, and quality improvement); and community development/collaborative practices (Health Canada, 2003). The effort to engage the public in health care decisions that we report here pertains to the category of governance and, in particular, priority setting.
This effort is prompted by the concern that health care costs are unsustainable; action is needed to improve efficiency and reduce the use of unnecessary treatment (Brownlee, 2007). However, even with a meaningful reduction in wasteful spending, medical options will always exceed the available resources. Part of the endeavor to contain costs must include making choices among competing needs and goals.
The public engagement we describe here was motivated by the belief that the public (both as taxpayer and as consumer) should have a voice in prioritizing health care spending. In 1998, we designed a simulation exercise to facilitate informed and prudent decisions by small groups regarding the benefits that ought to be included in health insurance. Called “Choosing Healthplans All Together” (CHAT), the exercise was initially created as a board game (Danis et al., 2002; Goold et al., 2005) and has subsequently been developed into a computer-based exercise (Danis et al., 2005) and a Web-based exercise available at www.chat-health.org (Kantner et al., 2006). Initial funding for creation and testing of the exercise was provided by the Department of Bioethics at the Clinical Center of the National Institutes of Health and the Robert Woods Johnson Foundation.
The underlying premise is that barriers to public participation—complexity of insurance as a topic, disinterested consumers, and minimal understanding of their role both as patients and as citizens—can be overcome if a highly engaging, interactive process is developed to promote thoughtful communal decisions.
DESCRIPTION OF CHAT
The CHAT exercise is an interactive decision tool designed to facilitate deliberation by groups. This focus group addresses the fact that health insurance pools resources to distribute the financial burden of health care costs. The exercise is designed to be easily used and understood by nonprofessionals, but it is often useful for professionals and graduate students to expand their reasoning about priority setting.
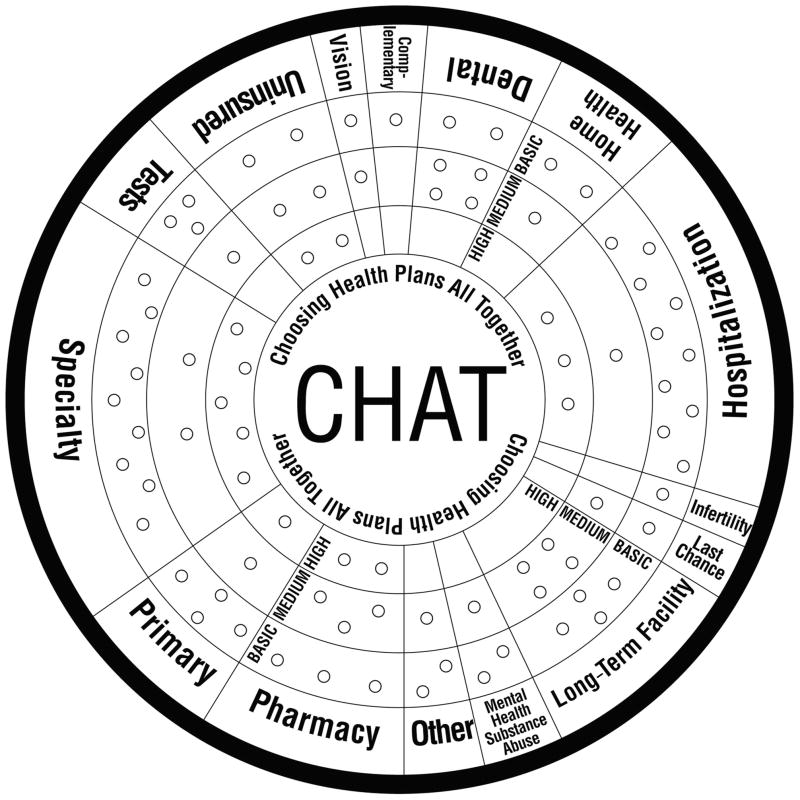
The exercise uses a pie chart in which various components of health insurance benefits such as primary care, hospitalization, and pharmacy are represented as coverage option for participants to choose from (Fig. 1). Participants can choose benefits at as many as 3 levels: basic, medium, and high, which are shown in the outer, middle, and inner rings of the board, respectively. These levels offer increasing degrees of choice, convenience, and expanded services and diminishing degrees of out-of-pocket costs. Each benefit category can be selected at any level by placing the specified number of markers as determined by its actuarial cost.
Figure 1.
CHAT board with service options. See Danis et al. (2002) for details of the service options. Copyright 2000 Board of Regents, University of Michigan, National Institutes of Health, and US Public Health Services. CHAT indicates Choosing Health Plans All Together.
During the exercise, participants are given 50 markers for choosing benefits. These markers represent an amount of money designated by the exercise sponsors and can reflect the policy question of interest. For example, if a publicly funded insurance program is facing the prospect of rising costs, and policy leaders want to explore ways to keep total expenditures from rising, the amount of money that exercise participants might be assigned would be the prevailing per capita expenditure. Benefit options on the board would be presented with the number of markers reflecting estimated future costs. A CHAT exercise designed in this way would allow exercise sponsors to gain information that allows them to run the program at a sustainable level that meets the health care priorities of the population. In general, the benefit options available on the CHAT board in various CHAT projects have had a total monetary value that is in the range of 1.3 to 2.0 times the total monetary value of the markers.
During a CHAT session, 9 to 15 individuals sit at a table, each using either a game board or a computer, depending on the version organized by the sponsor. A trained facilitator guides participants in designing health care benefits packages in 4 rounds: during round 1, participants work individually as though they are choosing for themselves and their families; in round 2, they work in groups of 3 on behalf of, for example, residents of a small community; in round 3, they deliberate about their choices as a group on behalf of all members of a state or another defined population; and in round 4, again individually for themselves and their families.
After rounds 1 and 2, participants are randomly assigned hypothetical health events, depicting illnesses ranging from the mundane to the severe, along with the service and cost consequences of benefit choices. Participants read “health event” cards aloud and discuss them. During round 3, when the entire group decides together, the facilitator displays a large CHAT board at the front of the room. Participants take turns nominating categories and benefit levels and discuss category selection. Groups usually choose priorities by consensus but occasionally vote on particularly controversial decisions if they cannot come to agreement.
A number of features of the exercise are designed both to inform participants about the issue of priority setting and to facilitate their ability in order to set priorities in an informed manner. At the outset of the exercise, the facilitator explains as follows:
Medical care is important to all of us. Because paying for health care out of our pockets is expensive, we have health insurance. Most of us who have health insurance get it through our jobs or a government program. We have very little say about how our health insurance is designed, what it will pay for and what it won’t. We don’t get to say what it will pay for. For example, we might want it to pay for the dentist, but it doesn’t. In this exercise you will participate in today, you make the choices about what your health insurance pays for. But you can’t choose everything! You can’t have insurance for all the medical care you would like. You will have to make some tough choices. We hope this exercise gives you a way to figure out the best choices.
The use of health event cards and the discussion among group participants about their personal experiences with illness and their need for health services are additional elements of the exercise intended to facilitate informed and prudent choices.
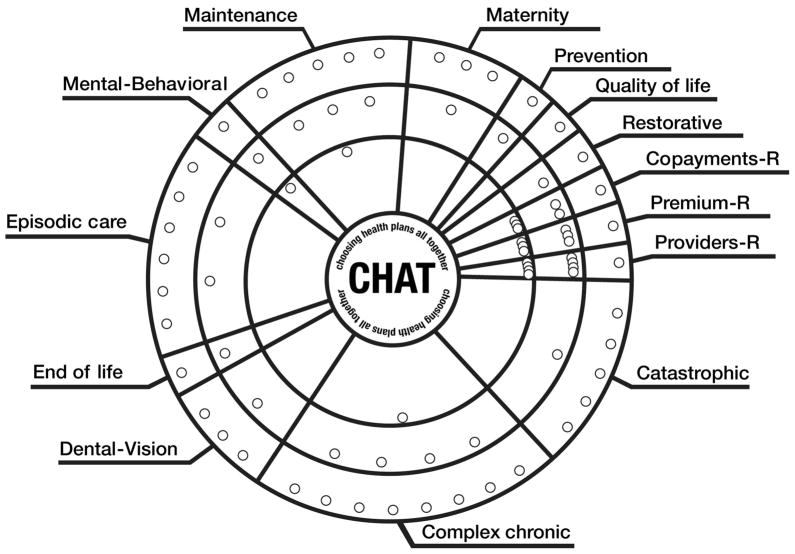
One particular feature of CHAT is the ability to customize it to the needs or interests of sponsoring groups. For example, instead of the pie chart representing options, such as hospital care and pharmacy, they can be presented as various health conditions, such as episodic illness, chronic illness, and terminal illness (Fig. 2; Ginsburg et al., 2006). The 3 different benefit levels can also be designed to vary by other considerations such as cost-effectiveness, strength of medical evidence, or probability of expected clinical benefit. Preparations before the exercise involve consideration of what benefit options will be offered (often with the participation of an advisory committee) and estimation of how much the benefits are expected to cost (as determined by a medical actuary).
Figure 2.
CHAT board with coverage options for health conditions. See Ginsburg et al. (2006) for details of the coverage options. CHAT indicates Choosing Health Plans All Together.
USE OF THE CHAT EXERCISE IN THE UNITED STATES
The CHAT exercise has been used for a variety of research, educational, and policy purposes. The first research project that was conducted in North Carolina examined the insurance preferences of several populations, including low-income uninsured individuals (Danis et al., 2002) and the elderly Medicare population (Danis et al., 2004), and evaluated the exercise from the perspective of participants (Goold et al., 2005). As awareness of the exercise has grown, a number of foundations have sponsored the use of CHAT. The Allina Foundation in Minnesota sponsored a CHAT project with the employees of public and private employers in Minnesota to advance more affordable employer-sponsored insurance. The California HealthCare Foundation, an independent philanthropy in California, funded 4 CHAT projects through the Center for Healthcare Decisions (CHCD, www.chcd.org; formerly, Sacramento Healthcare Decisions). The projects conducted by the CHCD have included a survey of employees of public and private corporations to promote the design of affordable health insurance (Danis et al., 2007a), a survey of disabled Medicaid enrollees to ascertain their priorities for coverage when faced by budget cuts (Danis et al., 2006), a survey of Californians to determine the general public’s opinion about what should be included in a basic benefit package for California’s uninsured (Ginsburg et al., 2006), and a survey of uninsured Californians to determine their priorities for a basic insurance package.
Subsequently, the CHCD has conducted training of departments of insurance in other states, including Ohio, Oklahoma, Montana, and North Dakota, that have used CHAT to engage their public in similar discussions. The CHAT exercise has also been used by 2 municipalities, including Galveston, Texas (http://galvestontx.usachamber.com/virDirEditorAssets/galvestonTX/chamberAccess/docs/3share%202%201%2009.pdf), and Pueblo, Colorado (Amos, 2007), to elicit input on designing low-cost, community-supported packages of core services for the uninsured.
In summary, this use of CHAT has occurred across 9 US states and has involved 12 distinct projects including approximately 300 exercises with more than 4200 people (Table 1). Recruitment for participation in these exercises has varied, depending on the participating population. Participants with employer-sponsored insurance have been recruited through the workplace and have not received a stipend since they have done the exercise during working hours. Other participants have been recruited through professional focus group agencies, community organizations, government entities, and business coalitions or through public advertising and have generally received stipends in the range of $25 to $75 to compensate for their time. The sociodemographic characteristics of these CHAT participants are shown in Table 1.
Table 1.
Characteristics of CHAT Participants in 8 States 1999–2009 (N = 4264)a
| Characteristics | North Carolina | Minnesota | Californiab | Texas | Oklahoma | Montana | Ohio | North Dakotac |
|---|---|---|---|---|---|---|---|---|
| No. of groups | 50 | 59 | 166 | 20 | 81 | 8 | 18 | |
| No. of participants | 562 | 619 | 1794 | 190 | 687 | 94 | 179 | 139 |
| Year | 1999 | 2001 | 2002–2007 | 2004–2005 | 2007–2008 | 2008 | 2008 | 2009 |
| Gender | ||||||||
| Male, % | 53 | 33 | 37 | 34 | 34 | 48 | 32 | 38 |
| Age (mean or range), y | ||||||||
| Mean ± SD | 47 ± 19 | 42 ± 12 | 41 ± 11 | |||||
| 18–39 | 41 | 48 | 29 | 24 | 13 | |||
| 40–59 | 49 | 43 | 51 | 61 | 56 | |||
| 60 and above | 10 | 9 | 19 | 16 | 30 | |||
| Ethnicityd | ||||||||
| Asian | 0 | 1 | 8 | 0 | 0 | 1 | 1 | |
| African American | 40 | 0 | 9 | 27 | 15 | 0 | 34 | |
| Hispanic/Latino | 0 | 0 | 11 | 21 | 7 | 0 | 3 | |
| White | 56 | 94 | 68 | 52 | 66 | 95 | 56 | |
| Other | 2 | 5 | 6 | 0 | 19 | 4 | 7 | |
| Education level | ||||||||
| High school and below | 37 | 12 | 11 | 40 | 30 | 19 | 52 | |
| Some college | 25 | 27 | 30 | 31 | 46 | 34 | 35 | |
| College and above | 39 | 61 | 59 | 29 | 24 | 47 | 13 | |
| Income level,e % | ||||||||
| Low | 45 | 1 | 18 | 16 | 23 | 5 | 73 | 24 |
| Middle | 55 | 42 | 33 | 49 | 36 | 38 | 26 | 27 |
| High | 58 | 48 | 34 | 41 | 3 | 49 | ||
| Insurance status | ||||||||
| Uninsured, % | 22 | 0 | 10 | 100 | 19 | 3 | 96 | 14 |
Colorado had approximately 100 participants, but data are not shown because they are not accurately known.
Results for California reflect 4 projects combined as described in the text.
Information about ethnicity and education was not collected in North Dakota.
Ethnicity is expressed in percentage and may add up to more than 100 because participants may identify with more than 1 ethnicity.
Income categories differed slightly among projects, with the low range varying from less than 15 000 to less than 21 000, and the high range always defined as greater than 60 000 and are expressed as percentages of participants with incomes in the given range, dollar amounts are multiples of $10,000.
The University of Michigan, which established copyright of the exercise, has licensed the exercise for use by others who wish to use it (www.chat-health.org). While aggregate use of CHAT by licensees has not been systematically recorded, we can summarize by reporting that there have been a small number of employers who have conducted CHAT exercises to facilitate negotiation about health insurance benefits with their employees, including a county school system and a university.
Several universities have used CHAT to teach college, medical, nursing, and health administration students about the challenges of allocating finite resources. It has also been used for leadership training. For example, the Society of Actuaries held workshops demonstrating the CHAT exercise at 3 of its annual conferences in 2008–2009. Other workshops have included the Institute of Medicine Health Policy committee and the Robert Wood Johnson health policy fellows.
Several notable features of the evolving use of the CHAT exercise are its initial use as a research tool to address policy questions; its subsequent use by key disseminators with funding from nongovernmental organizations (NGOs); and, following this, its use by state and local governments in efforts to find affordable insurance for the uninsured in their jurisdictions. While we have reported here on the use of CHAT in the United States, it has also been used by a district health board in New Zealand and it has been used in India to design affordable microinsurance (Danis et al., 2007b; Dror et al., 2007; http://www.microinsuranceacademy.org/).
RESULTS AND IMPACT OF CHAT EXERCISES
The various CHAT projects have used different benefit options as part of their exercise. Thus, a summary of public opinion about health care priorities cannot be easily derived. We therefore focus on the priorities of participants in the largest project, the Just Coverage CHAT project, to demonstrate the trade-offs they made. We then highlight some key findings from other projects and suggest patterns among project findings.
The Just Coverage CHAT project was designed to determine what Californians consider the most essential health care services that must be made available to all (Ginsburg et al., 2006). The benefit categories that were offered in the exercise were services related to various health conditions, as mentioned previously (Fig. 2). Participants were given enough markers to select 2/3 of the available benefits. Among the health insurance benefits that project participants chose to forgo are the following: screening tests that have a small likelihood of being helpful for prevention; interventions that do not adhere to practice guidelines in the course of managing chronic illness; and intensive care that prolongs life for only a few days at the end of life (Table 2). These findings are illustrative of the way the exercise facilitates the public setting of limits on health care under cost constraints.
Table 2.
Health care Coverage Chosen by Participants in the Just Coverage CHAT projecta
| Health care Need | Coverage |
|---|---|
| Catastrophic care | Covers treatment of unexpected, severe illness or injury, such as sudden liver failure from food poisoning or massive injuries from an accident. |
| Not covered: Treatments that are not likely to help but are the “only hope” left if all else fails. | |
| Chronic illness | Covers treatment of chronic conditions with effective, least costly interventions; more expensive ones are used only if others are not sufficient. |
Not covered:
| |
| Dental care | Covers yearly dental cleanings and radiography, plus 80% of basic services. Maximum coverage is $1000 per year per person. |
| End-of-life care | Covers home or facility-based hospice services and comfort measures. |
| Not covered: Costly, intensive measures, such as cardiopulmonary resuscitation, breathing machines, or placement in an intensive care unit, that may delay death for a few days, weeks, or months. | |
| Episodic care | Covers treatment for common short-term problems. Emergencies are dealt with quickly, but patients may wait several weeks or longer for routine visits, tests, and surgery. |
| Mental and behavioral health | Covers treatment of mental illness, including inpatient care for severe illness. Covers outpatient treatment for smoking, substance abuse, and obesity. |
| Not covered: Inpatient substance abuse treatment and bariatric surgery. | |
| Maternity | Covers all pre- and postnatal care that meets national standards, including preventing, detecting, or treating complications that may arise with childbirth. |
| Not covered: Less essential services, such as multiple sonograms of a normal baby, newborn circumcision, and 2-d hospital stay after normal delivery. | |
| Prevention | Covers wellness examinations, immunizations, and screening tests that meet national standards of effectiveness. |
| Not covered: Screening tests in which chances are small that the screening will be useful (eg, mammograms for low-risk women younger than 40 y) and for uncommon conditions, such as testing all newborns for very rare diseases. | |
| Quality of lifeb | Not covered: Problems in function, appearance, or comfort that are not seriously disabling but impact personal quality of life. For example, infertility, impotence, injuries that affect only athletic performance, growth hormones for children of below-average height, and nail fungus. |
| Restorative | Covers rehabilitation therapy after a disabling illness or accident to improve essential functioning, such as walking, speaking, personal care, and critical work-related tasks. |
| Not covered: In-home equipment needed for daily activities (such as crutches or wheelchairs). | |
| Vision | Yearly refractions, as needed, and $75 toward glasses every 2 y. |
Participants in the Just Coverage CHAT (Ginsburg et al., 2006) chose from 14 benefit categories (shown in Fig. 2). Abbreviated descriptions of the coverage categories are shown as specified by the decisions of the majority of the participants during the final round of CHAT.
Not covered.
There are several findings that are ubiquitous across projects. One is that groups select a slightly broader array of benefits than individuals, since they must accommodate a broader array of preferences. We also find that group decisions are more community-minded than individual decisions. For instance, groups in Minnesota were more likely than individuals in the groups to forgo some of their benefits to expand health insurance to the uninsured (Goold et al., 2004). Importantly, the exercise increases understanding that benefits need to be limited in order to limit health care spending (Danis et al., 2007a). In addition, participants are more likely to give priority during the final round of decision making to services such as mental health care and rehabilitation because they become more aware of the need for and the benefits of such services over the course of the exercise (Danis et al., 2007a). Whenever measured, at least 85% of participants are willing to abide by group decisions.
The impact of CHAT on coverage policy has been most demonstrable in Texas where a project that began at a municipal level grew into a statewide effort. Beginning in one city and expanding from there, the Galveston 3-Share Plan illustrates the many ingredients that contribute to successful policy implementation following a CHAT exercise. The University of Texas Medical Branch in Galveston, Texas, collaborated with business leaders and others in their community to develop a low-cost plan to cover health benefits for low-income employees of small businesses in Galveston County (http://www.utmb.edu/3share/pdfs/affordable-healthcare-coverage.pdf). A funding structure was developed that involved 3-way cost sharing among employees, employers, and federal government funds at a cost of $180 per covered individual. Approval for this plan was arranged through a request by Galveston County for a Health Insurance Flexibility and Accountability waiver (http://www.ssa.gov/OPHome/ssact/title11/1115.htm). The Galveston 3-Share Plan initially had a maximum capacity of 500 participants and enrolled 486. Additional funding was obtained to expand the program to 1000 participants. Subsequently, the CHAT exercise has been used throughout Texas for planning the start-up of 3-Share Plans in all the major metropolitan areas.
The impact of CHAT projects in other states has been more difficult to translate into policy changes. In Montana, for example, the Department of Insurance conducted CHAT exercises with employees of small businesses who were enrolled in the Insure Montana Program (http://www.sao.mt.gov/InsureMontana/index.asp). As a largely rural state, one of the most noticeable findings was that CHAT participants in the most rural communities voiced concern about the small size of the provider network. These comments were used as feedback in subsequent negotiations between the Montana Department of Insurance and the selected insurance carrier, but the realities of rural practice make it difficult to accommodate this concern. In Ohio, CHAT exercises were conducted as part of its government-sponsored State Coverage Initiative program in an effort to understand how the uninsured prioritize elements of coverage when resources are limited. Subsequently, the state appointed a Healthcare Coverage and Quality Council whose job is to advise the governor and the legislature on how to move toward universal coverage. The results of CHAT are intended to inform these recommendations. More detailed information about the benefit options and impact of CHAT projects in various states is available from the authors.
In several CHAT projects sponsored by employers, results were used to help inform their employee coverage decisions. One was a local school district whose benefits committee members acknowledged that the results from 5 CHAT sessions involving school employees influenced their subsequent benefits decisions. The other was a large for-profit corporation that contracted for a CHAT program designed specifically for them.
ADVANTAGES AND DISADVANTAGES OF THE CHAT EXERCISE
The major advantage of the exercise is that it makes the very complicated prospect of allocating limited health care resources understandable to the public. CHAT participants uniformly find the exercise easy, informative, and fun to use. It also informs people about the concept of getting value for money. They can understand, for example, that by restricting pharmacy benefit on the basis of cost-effectiveness, they could afford to include other desired benefits that they would otherwise have to exclude. The paper version of the exercise is simple and relatively inexpensive to administer. New facilitators can easily learn to run this version of the exercise with the prepared facilitator script, and it can be as short as 1 hour if one is simply using the exercise for educational purposes in a classroom. The computer-based version can be used in locations such as public libraries, schools, or community centers, where computers are available, and allows for automatic data collection and simple analysis. The exercise yields public opinion about priorities and trade-offs that can, in some circumstances, be incorporated into policy decisions.
There are several disadvantages to the exercise. Unless one chooses to use benefit options and actuarial data from a prior project, the background preparation for conducting a CHAT project is extensive, with considerable time required to create a particular CHAT board, conduct the actuarial analysis, and train 1 or more facilitators. Participation in the exercise usually requires 2 to 3 hours. With this significant time commitment for each session, we find it necessary and appropriate to pay participants a stipend, particularly if they are low-income earners or otherwise difficult to recruit. While small group exercises do not provide a representative sample of a population, the Web-based version of the exercise can potentially be used to do so.
DISCUSSION
The CHAT exercise has been used for research, educational, and policy purposes. Despite the time commitment required to adapt CHAT, train facilitators, recruit participants, and organize and conduct the sessions, states and communities have used the exercise because it provides something so few other public engagement strategies are able to do: take the complex social issue of designing affordable and acceptable health insurance benefits, bring it to the general public in a way they can understand, and capture a more informed public voice.
The initial dissemination of the CHAT exercise by NGOs perhaps illustrates the importance of NGOs as change makers (Bornstein, 2007). Its successful use at the municipal level illustrates the greater ease with which public engagement in priority setting is incorporated into policy at the local level. Overall, the slow accumulation of attention to the process may reflect the hesitance to accept limits and set priorities in the United States. We anticipate that as the need to limit health care costs continues, the use of the CHAT exercise could be valuable.
Acknowledgments
The authors thank all those who gave their time, effort, expertise, and financial resources to CHAT projects over the last decade. This effort was supported in part by the Intramural Research Program of the National Institutes of Health; the University of Michigan; several nonprofit foundations, including the Robert Wood Johnson Foundation, the Allina Foundation, the California Health-Care Foundation, the Kvar foundation, and the Houston Endowment; Departments of Insurance in several US states; and many businesses, particularly in Minnesota and California. The authors particularly thank the many participants in and organizers of CHAT exercises who gave their time anonymously.
Footnotes
Disclaimer: The views expressed here are those of the authors and do not necessarily reflect the policies of the National Institutes of Health or the US Department of Health and Human Services.
References
- Amos J. The Pueblo Chieftain. 2007. Jan 20, Puebloans craft health plans for working poor; pp. 1A–3A. [Google Scholar]
- Bornstein D. How to change the world: Social entrepreneurs and the power of new ideas. New York: Oxford University Press; 2007. (Updated ed.) [Google Scholar]
- Brownlee S. Overtreated: Why too much medicine is making us sicker and poorer. New York: Bloomsbury Press; 2007. [Google Scholar]
- Danis M, Benavides E, Nowak M, Goold SD. Development and evaluation of a computer decision exercise for consumer participation in insurance benefit planning. Forum for Family and Consumer Issues. 2005;10(2) Retrieved January 8, 2009, from http://www.ces.ncsu.edu/depts/fcs/pub/ltc.html. [Google Scholar]
- Danis M, Biddle A, Goold SD. Insurance benefit preferences of the low-income uninsured. Journal of General Internal Medicine. 2002;17:125–133. doi: 10.1046/j.1525-1497.2002.10609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danis M, Biddle AK, Goold SD. Enrollees choose priorities for Medicare. The Gerontologist. 2004;44:58–67. doi: 10.1093/geront/44.1.58. [DOI] [PubMed] [Google Scholar]
- Danis M, Binnendijk E, Vellakkal S, Ost A, Koren R, Dror D. Eliciting health insurance benefit choices of low income groups. Economic and Political Weekly. 2007b;62(32):3331–3339. Retrieved from http://www.epw.org.in. [Google Scholar]
- Danis M, Ginsburg M, Goold SD. The coverage priorities of disabled adult Medi-Cal beneficiaries. Journal of Health Care for the Poor and Underserved. 2006;17:592–609. doi: 10.1353/hpu.2006.0103. [DOI] [PubMed] [Google Scholar]
- Danis M, Goold SD, Parise C, Ginsburg M. Enhancing employee capacity to prioritize health insurance benefits. Health Expectations. 2007a;10:236–247. doi: 10.1111/j.1369-7625.2007.00442.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dror D, Koren R, Ost A, Binnendijk E, Vellakkal S, Danis M. Health insurance benefit packages that low income clients in India prioritize: Three criteria to estimate effectiveness of choice. Social Science and Medicine. 2007 Feb;64(4):884–896. doi: 10.1016/j.socscimed.2006.10.032. [DOI] [PubMed] [Google Scholar]
- Ginsburg M, Goold SD, Danis M. (De)constructing “Basic”: Consumers define the core elements of coverage. Health Affairs. 2006;25:1648–1655. doi: 10.1377/hlthaff.25.6.1648. [DOI] [PubMed] [Google Scholar]
- Goold SD, Biddle AK, Danis M. Will insured citizens give up benefit coverage to include the uninsured? Journal of General Internal Medicine. 2004;19:868–874. doi: 10.1111/j.1525-1497.2004.32102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goold SD, Biddle AK, Klipp G, Hall CN, Danis M. Choosing Healthplans All Together: A deliberative exercise for allocating limited health care resources. Journal of Health Politics, Policy, and Law. 2005;30:563–601. doi: 10.1215/03616878-30-4-563. [DOI] [PubMed] [Google Scholar]
- Health Canada. Exploring the link between public involvement/citizen engagement and quality health care. 2003 Retrieved January 8, 2009, from http://www.hc-sc.gc.ca/hcs-sss/pubs/qual/2003-qual-simces/2003-qual-simces-7-eng.php.
- Institute of Medicine. Measuring the quality of health care. 1998 Retrieved May 16, 2010, from http://www.iom.edu/Reports/1998/Measuring-the-Quality-of-Health-Care.aspx.
- Jacobs L, Marmor T, Oberlander J. The Oregon health plan and the political paradox of rationing: What advocates and critics have claimed and what Oregon did. Journal of Health Politics, Policy, and Law. 1999;24:161–180. doi: 10.1215/03616878-24-1-161. [DOI] [PubMed] [Google Scholar]
- Kantner L, Goold SD, Nowak M, Monroe-Gatrell L, Danis M. Web tool for health insurance design by small groups: Usability study. Proceedings of the SIGCHI Conference on Human factors in Computing Systems; 2006. Retrieved January 8, 2009, from http://www.acm.org/dl. [Google Scholar]
- Reeder FS. Citizens as Partners: OECD Handbook on Information, Consultation and Public Participation in Policy-Making. Paris: Organisation for Economic Co-operation and Development; 2001. Access to information on the environment in the United States; pp. 163–176. [Google Scholar]