Abstract
In patients with acute kidney injury (AKI), serum creatinine level does not increase until moderate to severe reduction in glomerular filtration rate (GFR) occurs. Thus its use for estimating GFR in early AKI delays detection of kidney damage and making important therapeutic decisions. Moreover, serum cystatin C is not affected by gender, age, race, and muscle mass and also does not suffer from lag period for its rise in early AKI. We studied 200 healthy subjects and 130 AKI patients over a period of 2 years at a tertiary care hospital. Serum creatinine and serum cystatin C were studied and analyzed in relevance to early AKI. We found that 56.2% of patients of AKI group had normal levels of serum creatinine in early phase, while all patients had elevated serum cystatin C at same time. Multiple logistic regression analysis revealed cystatin C-based GFR reflecting decline in GFR with worsening AKI in better than creatinine-based GFR. Serum cystatin C is a better marker of renal function in early stages of AKI and is less affected by age, gender, muscle mass, and ethnicity. Its use helps in early therapeutic intervention and possibly favorable outcome.
Keywords: Acute kidney injury, serum cystatin C, serum creatinine
Introduction
Acute kidney injury (AKI) is characterized by rapid decline in glomerular filtration rate (GFR). GFR is presently being monitored by serum creatinine concentration and calculated creatinine clearance using Cockcroft and Gault equation or Modification of Diet in Renal Disease study (MDRD) formula.[1–3] However, serum creatinine does not increase until the GFR has moderately decreased (about 40 ml/min/1.73 m2). This insensitivity for small to moderate decreases in GFR in creatinine blind GFR area (40-70 ml/min/1.73 m2) gives a false sense of security and leads to late detection of kidney damage. All this makes serum creatinine less reliable for making therapeutic decisions in critically ill patients, such as decision to change nephrotoxic drugs or measures to increase renal perfusion.
Serum cystatin C is a non-glycosylated, 13.3-kDa protein belonging to cystatin protease inhibitors. It has shown promise as a replacement for serum creatinine in estimation of GFR.[4,5] After glomerular filtration, it is fully catabolized in the proximal renal tubule and is not returned to blood. Concentration of serum cystatin C is not affected by gender, age, race, protein intake, and muscle mass, unlike serum creatinine. When GFR decreases, cystatin C level begins to rise proportionately.
In this study, we studied serum creatinine and serum cystatin C levels in AKI to establish its relevance in the early period of AKI.
Materials and Methods
The study was carried out from September 2008 to September 2010 at a tertiary care hospital. The study group consisted of 200 healthy subjects and 130 patients of AKI. After obtaining an informed consent, a screening questionnaire was filled to collect information such as age, gender, height, weight, comorbidities, personal history, drug history, presenting complaints, and laboratory investigations. A detailed physical examination was carried out.
The serum cystatin C and serum creatinine values were measured simultaneously and analyzed. In the AKI study group, they were taken within 24 hours of onset of injury. The “RIFLE” criteria were used for defining the AKI, and the stages “risk” and “injury” constituted the “early AKI.”
GFR was estimated using the Cockcroft-Gault formula for creatinine clearance and Larsson formula for cystatin C-based GFR.
Larsson formula: eGFR = 77.24 × cystatin C−1.2623
The gold standard for measuring GFR viz. inulin clearance, urinary clearance of exogenous radioactive markers (125I-iothalamate and 99mTc-DTPA (diethylene-triamine -pentaacetate)), was not used in this study due to practical limitations.
Statistical analysis was performed using appropriate statistical tests and P value less than 0.05 was considered significant.
Results
The characteristics of our study population are given in Table 1.
Table 1.
Demographic and biochemical characteristics of study population
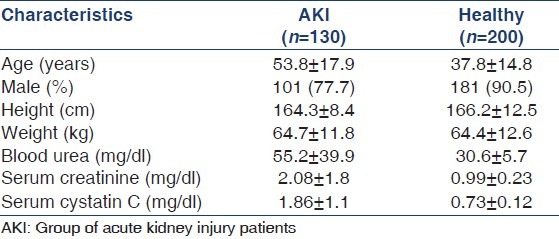
Serum cystatin C had lower standard deviation (1.1) and serum creatinine had higher standard deviation (1.8) in AKI indicating lesser variability of serum cystatin C.
The variation of serum creatinine was significantly greater than that of serum cystatin C in both groups. The standard deviation of serum creatinine (0.23) is double that of serum cystatin C (0.12) in the healthy group, which indicates a wide fluctuation in serum creatinine compared to serum cystatin C in healthy population too.
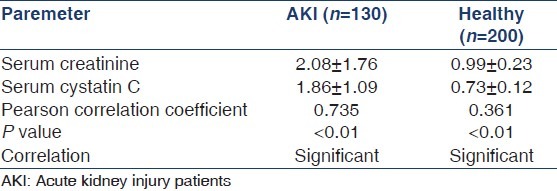
Although the correlation between serum creatinine and serum cystatin C was significant in both groups, a high strength of correlation was observed in the AKI group [Table 2]. This implies that small changes in serum creatinine are best reflected by a proportionate rise in serum cystatin C in AKI, especially at lower values.
Table 2.
Correlation between serum creatinine and serum cystatin C
In our study, it was found that in the AKI group majority (56.2%) had normal creatinine values (0.9–1.4 mg/dl). This subset was in “creatinine blind” range where serum creatinine values are normal with elevated cystatin C levels. All 130 patients with AKI had deranged cystatin C levels [Table 3, Figure 1]. This confirms the finding that serum cystatin C is elevated much before serum creatinine levels start rising and does not suffer from the disadvantage of creatinine blind area. In this way it helps for early detection of kidney injury.
Table 3.
Distribution of serum creatinine and serum cystatin C in acute kidney injury
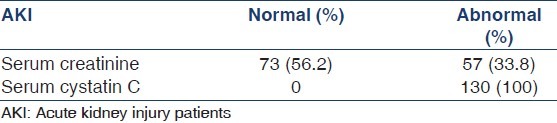
Figure 1.
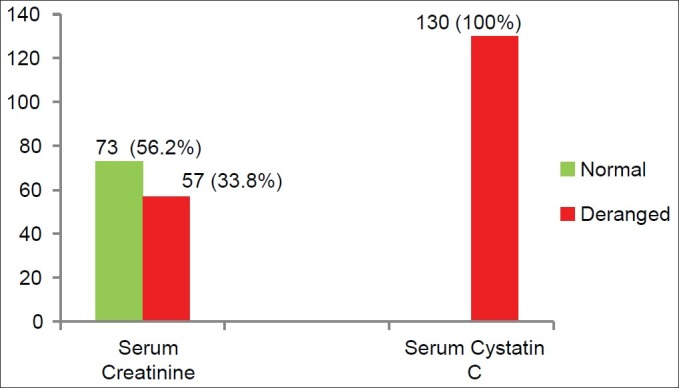
Distribution of serum creatinine and serum cystatin C in acute kidney injury
Multiple logistic regression applied to GFR calculated by Cockroft-Gault using serum creatinine and GFR-calculated serum cystatin C in AKI group gave a correlation coefficient (R) of 0.822 [Table 4]. This showed a good positive correlation between creatinine-based GFR and cystatin C-based GFR. Correlation coefficient of creatinine-based GFR is -0.00213 and that of cystatin C-based GFR is -0.00673. Cystatin C-based GFR resulted in more negative correlation compared to creatinine-based GFR in the AKI group. It means cystatin C-based GFR reflects a decline in GFR with worsening AKI in a much better way compared to creatinine-based GFR. The P value was significant (P < 0.01) for both cystatin C- and creatinine-based GFR.
Table 4.
Multiple logistic regression for glomerular filtration rate using serum creatinine and cystatin C in acute kidney injury patients
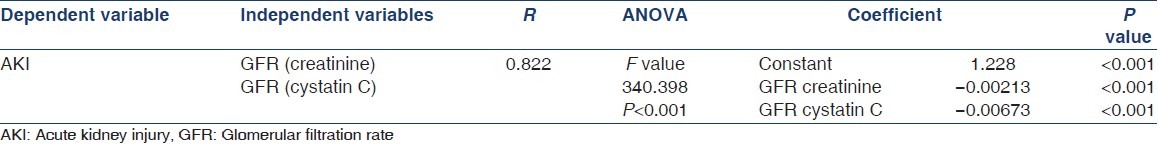
Thus in the AKI group, cystatin C-based GFR was better compared to creatinine-based GFR in early detection of worsening clinical status. This suggests the utility of serum cystatin C over serum creatinine in predicting early decline in GFR and thereby helping in early therapeutic intervention.
Discussion
Creatinine production changes significantly according to the muscle mass of the body and dietary factors. Creatinine is filtered by the glomeruli, and also secreted by the renal tubules. This tubular secretion contributes approximately 20% of the total creatinine excretion by the kidney and it can increase as GFR decreases. All of these factors explain why serum creatinine concentration may not be a good parameter for accurate determination of GFR, especially at lower rates.[6]
Cystatin C production in the body is a stable process that is not influenced by renal conditions, increased protein catabolism, or dietetic factors. Moreover, it does not change with age or muscle mass like creatinine does. Its biochemical characteristics allow free filtration in the renal glomerulus, and subsequent metabolism and reabsorption by the proximal tubule. For these reasons, serum cystatin C has been suggested to be an ideal endogenous marker of GFR.[7–9] However, few studies demonstrate that older age is independently associated with higher serum cystatin C levels after adjusting for creatinine clearance.[10]
Serum creatinine had higher standard deviation the, serum cystatin C in both subgroups AKI, and healthy, respectively. The variation of serum creatinine is significantly greater than that of serum cystatin C in both the groups. Serum creatinine level increases with increase in muscle mass and protein intake, whereas tubular secretion increases with fall in GFR, blunting its rise. Thus serum creatinine concentration may not be a good parameter for accurate determination of GFR, especially at lower rates. This proves superiority of serum cystatin C over serum creatinine in AKI. Similar observations were found in many studies, especially in a meta-analysis by Dharnidharka et al,[11] and Kyhse-Andersen et al.[4]
In the AKI group, more than half the patients (56.2%) had normal creatinine values, but they had elevated cystatin C and were in creatinine blind area. Moreover, all AKI patients had deranged cystatin C. This confirms the finding that serum cystatin C is elevated much before serum creatinine levels start rising. Serum cystatin C has a higher sensitivity in identifying early kidney dysfunction, which is missed by relying on serum creatinine alone.
The creatinine blind area is the range between 40 and 70 ml/min/1.73 m2 where a decrease in GFR starts to occur. Early reduction in GFR will not be shown up with creatinine testing, whereas cystatin C will show a true positive reduction in GFR. The creatinine test will give a false negative result. The cystatin C test will give a true positive. Cystatin C does not have a blind area. Early diagnosis of AKI based on serum cystatin C helps in timely intervention to have favorable outcome. Cystatin C indicates a more real-time functional state of the kidney and without the lag period as in the case with creatinine measurement. Cystatin C-based GFR gives a direct and accurate measurement of GFR independent of age and muscle mass.[12–14]
GFR in critically ill individuals can change rapidly because of, for example, renal hypoperfusion secondary to shock or the use of nephrotoxic agents. Despite this, it is not uncommon to see changes in the serum creatinine for up to several days until the stabilization phase is reached. This may also explain the poor diagnostic usefulness of serum creatinine in early hours of AKI, as seen in our study compared with that In other studies.[8,15] The delay that usually exists between the decline in GFR and that in serum creatinine makes the latter test poorly reliable for making therapeutic decisions in critically ill patients, such as a decision to change nephrotoxic agents or to increase renal perfusion.
This study has some limitations. This is a cross-sectional study with assessment carried out at a single point of time; a old standard comparison for estimation of GFR viz. inulin clearance, urinary clearance of exogenous radioactive markers (125I-iothalamate and 99mTc-DTPA), has not been used in this study due to practical constraints, and we used RIFLE criteria for defining the AKI instead of Acute Kidney Injury Network (AKIN) criteria as the current study uses eGFR which is not incorporated in the latter.
Conclusion
To conclude, serum cystatin C is a better marker of renal function in early stages of AKI and is less affected by age, gender, muscle mass, and ethnicity. Use of serum cystatin C-based GFR may be more accurate and useful for early therapeutic intervention and possibly a favorable outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 2.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- 3.Froissart M, Rossert J, Jacquot C, Paillard M, Houillier P. Predictive performance of the modification of diet in renal disease and Cockcroft-Gault equations for estimating renal function. J Am Soc Nephrol. 2005;16:763–73. doi: 10.1681/ASN.2004070549. [DOI] [PubMed] [Google Scholar]
- 4.Kyhse-Andersen J, Schmidt C, Nordin G, Andersson B, Nilsson-Ehle P, Lindström V, et al. Serum cystatin C, determined by a rapid, automated particle-enhanced turbidimetric method, is a better marker than serum creatinine for glomerular filtration rate. Clin Chem. 1994;40:1921–6. [PubMed] [Google Scholar]
- 5.Jung K, Jung M. Cystatin C: A promising marker of glomerular filtration rate to replace creatinine. Nephron. 1995;70:370–1. doi: 10.1159/000188621. [DOI] [PubMed] [Google Scholar]
- 6.Kim KE, Onesti G, Ramirez O, Brest AN. Creatinine clearance in renal disease. A reappraisal. Br Med J. 1969;4:11. doi: 10.1136/bmj.4.5674.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Randers E, Erlandsen EJ, Pedersen OL, Hasling C, Danielsen H. Serum cystatin C as an endogenous parameter of the renal function in patients with normal to moderately impaired kidney function. Clin Nephrol. 2000;54:203–9. [PubMed] [Google Scholar]
- 8.Randers E, Kristensen JH, Erlandsen EJ, Danielsen H. Serum cystatin C as a marker of the renal function. Scand J Clin Lab Invest. 1998;58:585–92. doi: 10.1080/00365519850186210. [DOI] [PubMed] [Google Scholar]
- 9.Newman DJ, Thakkar H, Edwards RG, Wilkie M, White T, Grubb AO, et al. Serum cystatin C measured by automated immunoassay: A more sensitive marker of changes in GFR than serum creatinine. Kidney Int. 1995;47:312–8. doi: 10.1038/ki.1995.40. [DOI] [PubMed] [Google Scholar]
- 10.Knight EL, Verhave JC, Spiegelman D, Hillege HL, de Zeeuw D, Curhan GC, et al. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int. 2004;65:1416–21. doi: 10.1111/j.1523-1755.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- 11.Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to serum creatinine as a marker of kidney function: A meta-analysis. Am J Kidney Dis. 2002;40:221–6. doi: 10.1053/ajkd.2002.34487. [DOI] [PubMed] [Google Scholar]
- 12.Ahlström A, Tallgren M, Peltonen S, Pettilä V. Evolution and predictive power of serum cystatin C in acute renal failure. Clin Nephrol. 2004;62:344–50. doi: 10.5414/cnp62344. [DOI] [PubMed] [Google Scholar]
- 13.Hoek FJ, Kemperman FA, Krediet RT. A comparison between cystatin C, plasma creatinine and the Cockcroft and Gault formula for the estimation of glomerular filtration rate. Nephrol Dial Transplant. 2003;18:2024–31. doi: 10.1093/ndt/gfg349. [DOI] [PubMed] [Google Scholar]
- 14.Peralta CA, Shlipak MG, Judd S, Cushman M, McClellan W, Zakai NA, et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA. 2011;305:1545–52. doi: 10.1001/jama.2011.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coll E, Botey A, Alvarez L, Poch E, Quintó L, Saurina A, et al. Serum cystatin C as a new marker for noninvasive estimation of glomerular filtration rate and as a marker for early renal impairment. Am J Kidney Dis. 2000;36:29–34. doi: 10.1053/ajkd.2000.8237. [DOI] [PubMed] [Google Scholar]


