Abstract
Emphysematous pyelonephritis is a rare, potentially lethal complication of polycystic kidney disease. Treatment mostly includes emergency nephrectomy of the affected kidney. We report a case of bilateral emphysematous pyelonephritis in a 57-year-old diabetic male with autosomal dominant polycystic kidney disease, who recovered with conservative treatment. Escherichia coli was cultured from the cyst aspirate. He was treated with percutaneous needle aspiration of infected cysts and intravenous antibiotics (meropenem and pazufloxacin) for 3 weeks.
Keywords: Emphysematous pyelonephritis, percutaneous aspiration, polycystic kidney disease
Introduction
Cyst infections account for 10% of hospitalizations in autosomal dominant polycystic kidney disease (ADPKD) patients with an estimated incidence of 0.01 episodes per patient per year.[1] Emphysematous pyelonephritis (EPN) is a severe necrotizing form of renal parenchymal infection caused by gas-forming organisms. EPN in polycystic kidneys is diagnosed by computed tomography (CT) images of air inside renal cysts. Bilateral EPN is a special situation where initial management with antibiotics, diabetes control, and percutaneous drainage must be attempted, so as to avoid bilateral nephrectomy. Overall, data on EPN in ADPKD are limited to case reports. We report a case of bilateral EPN in polycystic kidney disease and review the pertinent literature.
Case Report
A 57-year-old man with diabetes mellitus, systemic hypertension, and polycystic kidney disease presented with fever and left loin pain for 1 week. His medications included two oral anti-diabetic drugs (metformin and glimepiride) and two anti-hypertensive drugs. There was no history of dysuria or hematuria. Physical examination revealed pallor, bilateral pedal edema, pulse rate of 102/min, blood pressure of 160/100 mmHg, temperature of 39°C, and respiratory rate of 19/min. Abdomen examination revealed bilateral nodular enlarged kidneys with tenderness in the left renal angle. Respiratory system and cardiovascular system examinations were unremarkable. His hemoglobin (10.3 g/dL) was decreased and white blood cell count was increased to 13.8 × 109/L with neutrophils 84%, lymphocytes 12%, eosinophils 2%, and monocytes 2%. Platelet count was 364 × 109/L and 1.2% of reticulocyte count was normal. Blood sugar was 390 mg/dl, serum creatinine was 1.39 mg/dL, and the estimated four-variable MDRD GFR was 55 mL/min/1.73 m2. Blood gas analysis revealed high anion gap metabolic acidosis (pH, 7.26; pCO2, 25 mm Hg; HCO3, 19 meq/L; pO2, 128 mmHg; anion gap 16 meq/L; lactate, 1.5 meq/L; Na, 136 meq/L; K, 3.8 meq/L; and Cl 101 meq/L). Liver function tests, uric acid, calcium, inorganic phosphorus, and lipid profile were within normal limits. HBsAg, HIV, and anti-HCV antibody enzyme-linked immunosorbent assay were negative. Urine analysis showed 2+ ketone, 4+ glucose, and hematuria with 1+ proteinuria. Urine nitrite test was positive. There were 8–10 white blood cells per high-power field (hpf), 8–10 red blood cells per hpf, 12–15 pus cells per hpf, and no evidence of casts on microscopic examination of the urine sediment. Ultrasound revealed bilateral polycystic kidneys with features of thick wall and intracystic debris in one upper pole cyst of right kidney. Emergency non-contrast computerized tomogram of abdomen revealed features of bilateral emphysematous cyst infection [Figure 1] with features of pyelonephritis. A provisional diagnosis of EPN with diabetic ketoacidosis was made. His initial management included intravenous antibiotics (piperacillin + tazobactum 4.5 gm q8h and levofloxacin 500 mg q24h), IV fluids, insulin infusion (regular insulin titrated to maintain capillary blood glucose range of 100–150 mg/dl), and supportive measures. Percutaneous aspiration of both the cysts was done under real-time ultrasound guidance on day 2. About 250 ml of purulent fluid was aspirated. Gram stain revealed multiple gram-negative bacilli. Urine and blood cultures showed no growth. Chest X-ray did not reveal any abnormality. Culture of pus revealed Escherichia coli (non-ESBL) sensitive to meropenem and pazufloxacin. Antibiotics were changed to meropenem, pazufloxacin from day 4. Patient became afebrile on day 6. Antibiotics were continued for a period of 3 weeks. Repeat ultrasound done after 3 weeks showed significant resolution of cyst collection on both sides. Patient was discharged on day 22 with oral antibiotics (faropenem and levofloxacin). Twelve weeks after discharge, patient is asymptomatic, with a serum creatinine of 1.04 mg/dL. He is presently on levofloxacin prophylaxis.
Figure 1.
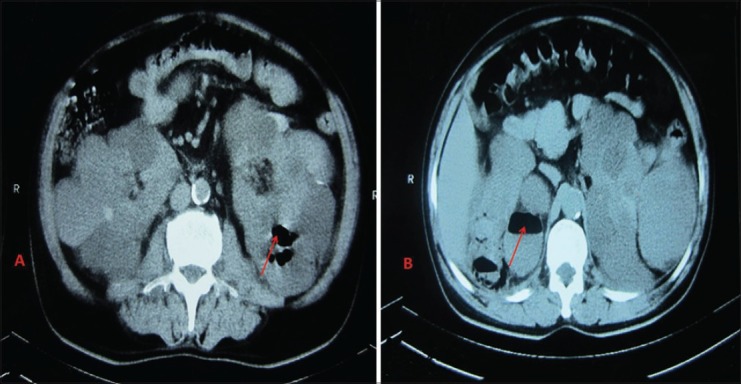
Non-contrast computerised tomogram of abdomen showing bilaterally enlarged kidneys with multiple cysts. Both kidneys showed cyst with air pockets (arrows)
Discussion
Current guidelines of emphysematous pyelonephritis recommend conservative management with antibiotics and percutaneous drainage as the preferred first line of treatment.[2] In patient with polycystic kidney disease, presence of air in cysts with perinephric stranding indicates infection by gas-forming organisms. The terms emphysematous pyelonephritis and emphysematous cyst infection are used interchangeably to describe this condition.[3] This is only the fifth case report of bilateral EPN in polycystic kidneys. Interestingly, three of the five cases have been successfully managed with conservative treatment [Table 1].
Table 1.
Summary of case reports of bilateral emphysematous pyelonephritis in polycystic kidney disease
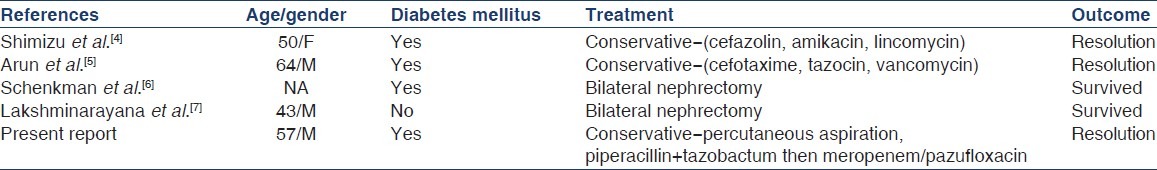
Unilateral EPN is often managed by emergency nephrectomy. However, bilateral EPN is a special situation where bilateral nephrectomy involves high morbidity and mortality and is a major dilemma when patients present with normal baseline renal functions. The decision for bilateral nephrectomy in such situations must be reserved for exceptional cases where conservative approach including percutaneous drainage fails.
Our case highlights the diagnostic value of computerized tomogram and percutaneous aspiration in EPN. CT is useful in diagnosis and staging of EPN. Though E. coli is the most common cause of EPN, it is important to isolate the microbe, so as to administer appropriate antibiotics. Interestingly, in our case, E. coli could not be isolated from blood or urine, and the culture of the aspirate alone yielded the right diagnosis. Percutaneous needle aspiration is a simple bedside procedure which can be done in the emergency department and the aspirate can be combined with other primary culture fluids sent from the emergency department.
On literature review, all five cases reported so far have been caused by E. coli. Two of the five patients required bilateral nephrectomy following failure of conservative measures. We observe that aggressive conservative management with appropriate antibiotics and percutaneous methods can avoid bilateral nephrectomy in most instances.[7]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sallée M, Rafat C, Zahar JR, Paulmier B, Grünfeld JP, Knebelmann B, et al. Cyst infections in patients with autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2009;4:1183–9. doi: 10.2215/CJN.01870309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pontin AR, Barnes RD. Current management of emphysematous pyelonephritis. Nat Rev Urol. 2009;6:272–9. doi: 10.1038/nrurol.2009.51. [DOI] [PubMed] [Google Scholar]
- 3.Sooraj YS, Nainan GK, Joseph F, Thara P. Emphysematous polycystic renal infection. Indian J Nephrol. 2010;20:205–6. doi: 10.4103/0971-4065.73457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shimizu H, Hariu K, Kamiyama Y, Tomomasa H, Iizumi T, Yazaki T, et al. Bilateral emphysematous pyelonephritis with autosomal-dominant polycystic kidney disease successfully treated by conservative method. Urol Int. 1999;63:252–4. doi: 10.1159/000030462. [DOI] [PubMed] [Google Scholar]
- 5.Arun N, Hussain A, Kapoor MM, Abul F. Bilateral emphysematous pyelonephritis and emphysematous cystitis with autosomal-dominant polycystic kidney disease: Is conservative management justified? Med Princ Pract. 2007;16:155–7. doi: 10.1159/000098371. [DOI] [PubMed] [Google Scholar]
- 6.Schenkman E, Auriemma P. Bilateral emphysematous pyelonephritis with autosomal dominant polycystic kidney disease. J Urol. 1998;159:1633–4. doi: 10.1097/00005392-199805000-00060. [DOI] [PubMed] [Google Scholar]
- 7.Lakshminarayana G, Mathew A, Rajesh R, Kurien G, Unni VN. Bilateral emphysematous pyelonephritis in autosomal dominant polycystic kidney disease. Indian J Nephrol. 2012;22:136–8. doi: 10.4103/0971-4065.97138. [DOI] [PMC free article] [PubMed] [Google Scholar]


