Abstract
Background:
Recently, the use of one-piece implants (OPI) has become more popular. Since no reports specifically focus on OPIs inserted in molar areas, a retrospective study has been performed.
Materials and Methods:
A series of 36 OPIs (Diamond; BIOIMPLANT, Milan, Italy) were inserted into the molar area of patients admitted at the Dental Clinic, University of Chieti, Italy, for oral rehabilitation between January and December 2010.
Results:
In our series survival rate (SVR) and success rate (SCR) were 91.7% and 97%, respectively. Statistical analysis demonstrated that no studied variable has an impact on survival (i.e., lost implants) as well as on clinical success (i.e., crestal bone resorption).
Conclusion:
OPIs are reliable devices for oral rehabilitation in the molar areas.
Keywords: Bone, fixture, immediate loading, implant, one-piece, welding
INTRODUCTION
Two-piece implants inserted into molar areas are predicable tools for oral rehabilitation. In 2008 Fugazzotto[1] reported a series of implants placed at the time of maxillary molar extraction. A total of 391 were reviewed and followed for up to a mean of 40 months. The cumulative survival rate was 99.5%. In a subsequent study, the same author[1] reported the clinical outcome of 341 implants placed into the mandible at the time of molar extraction. Concomitant regenerative therapy was performed around 332 of the placed implants. One implant was mobile 3 weeks post insertion. A second implant was lost after 30 months in function. All other implants were stable at the time of uncover 3-7 months post insertion. A total of 339 implants have been in function for up to 6 years, with a mean time in function of 30 months, yielding a cumulative survival rate of 99.1%.
The ITI Study Group Italia[2] assessed the clinical and radiographic outcomes of immediate transmucosal implant placement into molar extraction sockets. A 12-month multicenter prospective cohort study was performed. Following molar extraction, implants were immediately placed into the sockets. Molars with evidence of acute peri-apical pathology were excluded. After implant placement and achievement of primary stability, flaps were repositioned and sutured allowing non-submerged, transmucosal healing. Peri-implant marginal defects were treated according to the principles of guided bone regeneration (GBR) by means of de-proteinized bovine bone mineral particles in conjunction with a bio-resorbable collagen membrane. Standardized radiographs were obtained at baseline and 12 months thereafter. Changes in depth and width of the distance from the implant shoulder and from the alveolar crest to the bottom of the defect were assessed. Eighty-two patients were enrolled and followed for 12 months. Extraction sites displayed sufficient residual bone volume to allow primary stability of all implants. Sixty-four percent of the implants were placed in the areas of 36 and 46. GBR was used in conjunction with the placement of all implants. No post-surgical complications were observed. All implants healed uneventfully yielding a survival rate of 100% and healthy soft tissue conditions after 12 months. The authors concluded that immediate transmucosal implant placement represented a predictable treatment option for replacement of mandibular and maxillary molars.
Matarasso, et al.[3] studied the dimensional ridge alterations following immediate implant placement in molar extraction sites. Twelve subjects received 12 immediate transmucosal implants in molar extraction sites. Peri-implant defects were treated according to the principles of GBR by means of a de-proteinized bone substitute and a bio-resorbable collagen membrane. Changes in vertical and horizontal distances of alveolar bony walls to the bottom of the defects and to the implant surfaces were compared between implant placement and surgical re-entry at 6 months. The implant survival rate at 6 months was 100%. Statistically significant differences were observed in the mean changes in vertical distances between baseline and re-entry. At re-entry, all peri-implant marginal defects assessed from the internal socket wall to the implant surface were healed. The authors concluded that the marginal defects around immediate implants placed in molar extraction sites were completely filled after 6 months of healing through de novo bone formation.
Acocella, et al.[4] evaluated the predictability a modified implant insertion at the time of maxillary molar extraction. Sixty-eight patients with a total of 68 teeth scheduled for tooth extraction and immediate implant placement into fresh sockets were included. Implants were positioned just after teeth removal and, in case of necessity, a regenerative therapy was performed at the same time. After a 3-month period of healing, implants were restored with single crown fixed prostheses. All implants restored with single crowns were monitored for 36 months; only three implants failed with a cumulative survival rate of 97.96%. The authors concluded that the combination of a traumatic extraction of maxillary molars, sufficient residual inter-radicular bone, and use of appropriate regenerative material at the time of implant insertion represents a predictable long-term treatment. Lauritano and co-workers[5,6,7] focused on possible consequences of a peri-implantitis disease caused by bacteria on the stability of the implant. Previously we reported the effectiveness on a new type of one-piece implants (OPI) (Diamond; BIOIMPLANT, Milan, Italy) for oral rehabilitation.[8,9,10,11,12,13,14] Moreover, we demonstrated that spiral family implants can be used successfully in low bone.[15]
Since OPIs became more and more popular and no reports specifically focus on their outcome in molar areas, a retrospective study is performed.
MATERIALS AND METHODS
Study design/sample
To address the research purpose, the investigators designed a retrospective cohort study. The study population was composed of patients admitted at the Dental Clinic, University of Chieti, Italy, for evaluation and implant treatment, between January and December 2010, as reported previously.[8,9,10,11,12,13,14]
Subjects were screened according to the following inclusion criteria: Controlled oral hygiene and absence of any lesions in the oral cavity; in addition, the patients had to agree to participate in a post-operative check-up program.
The exclusion criteria were as follows: Bruxists; smoking more than 20 cigarettes per day; consumption of alcohol more than 2 glasses of wine per day; localized radiation therapy of the oral cavity; antitumor chemotherapy; liver, blood, and kidney diseases; immunosuppression; patients on corticosteroids; pregnant women; and inflammatory and autoimmune diseases of the oral cavity.
Variables
Several variables are investigated: Demographic (age and gender), anatomic (tooth site, distance between implants), implant (length and diameter), and prosthetic (welding procedure) variables.
Primary and secondary predictors of clinical outcome were used. The primary predictor is the presence/absence of the implant at the end of the observation period. It is defined as survival rate (i.e., SVR) that is the total number of implants still in place at the end of the follow-up period.
The second predictor of outcome was the peri-implant bone resorption. It is defined as implant success rate (SCR) and it is evaluated according to the absence of persisting peri-implant bone resorption greater than 1.5 mm during the first year of loading and 0.2 mm per year during the following years.[16]
Data collection methods
Data were collected as reported previously.[8,9,10,11,12,13,14]
Surgical protocol
All patients underwent the same surgical protocol.[8,9,10,11,12,13,14]
Data analysis
Pearson χ2-test was used to detect if implant position has an impact both on failures (i.e., lost fixtures) and/or on success (i.e., crestal bone resorption around implants smaller than 1.5 mm).
RESULTS
Nineteen patients (10 females and 9 males) with a median age of 62 years (min.-max., 43-80 years) were enrolled. The mean follow-up was 7 months. A total of 176 OPIs (Diamond; BIOIMPLANT) were inserted [Figure 1]. Among them 36 fixtures were inserted into the molar area. A total of 1, 6, and 29 implants had a diameter narrower than, equal to, and wider than 4 mm, respectively. A total of 20, 7, and 9 fixtures were shorter than, equal to, and longer than 13 mm, respectively. Twenty implants were placed into the mandible and 16 into the maxilla; 17 in females and 19 in males; and 26 were welded. The mean observation period, patient’ age, inter-implant distance, and peri-implant bone resorption per implant were 8 ± 6 months (min.-max., 1-26 months), 65 ± 11 years (min.-max., 43-76 years), 3.7 ± 1.7 mm (min.-max., 1.1-8.3 mm), and 0.2 ± 0.7 (min.-max., −1.7-1.8 mm), respectively. Pearson χ2-test was used to detect if implant site had an impact both on failures (SVR, i.e., lost fixtures) and/or on success (SCR, i.e., crestal bone resorption around implants lower than 1.5 mm).
Figure 1.
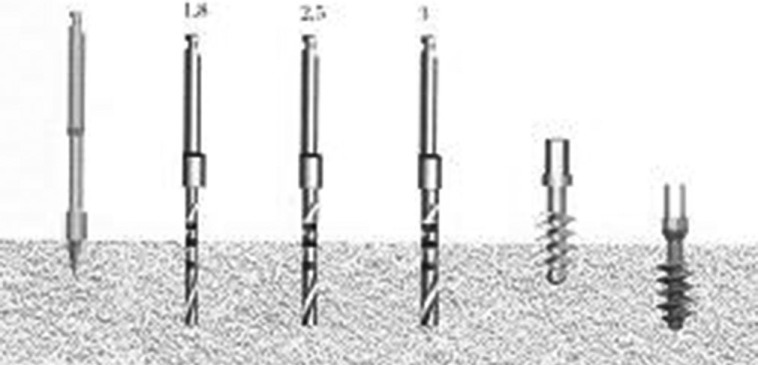
Different diameters of drill
Three implants were lost in the post-operative period (within 3 months) and one had a peri-implant bone resorption area wider than 1.5 mm; thus SVR and SCR were 91.7% and 97%, respectively. Statistical analysis demonstrated that no studied variable had an impact on survival (i.e., lost implants) as well as on clinical success (i.e., crestal bone resorption).
DISCUSSION
Few articles focus on implants inserted in molar sites[17,18,19,20,21] and none on OPIs. In addition to previously reported articles,[17,18,19,20,21] Annibali, et al.[22] reported a series of patients treated consecutively for first molar replacement according to unconventional (immediate = Group 1, early = Group 2) or conventional (late = Group 3) surgical protocols. Peri-apical radiographs obtained upon delivery of the definitive crown and 1 year later were digitized and assessed to evaluate marginal bone loss (MBL). Clinical photographs were evaluated to determine soft tissue health. Forty-seven patients were treated, with a total of 53 immediate, early, or late single implants. The implant survival rate was 100% for all groups. The success rate was 91.7% for early implants, 95.0% for immediate post-extraction implants, and 100% for implants placed in healed sites. MBL and soft tissue parameters did not differ significantly among the three groups at definitive restoration delivery or 1 year later; a thin gingival biotype, irrespective of treatment timing, was the only covariate that was able to slightly affect the outcome variables. The authors concluded that short-term implant survival and success rates, as well as MBL values for immediate, early, and conventional implants, appear similar for maxillary and mandibular first molar sites. Freitas-Junior, et al.[23] tested the reliability and failure modes of molar crowns supported by three different implant-supported designs.
There were the following groups: Group 1, one standard-diameter implant (3.75 mm); Group 2, one narrow-diameter implant (3 mm); and Group 3, two narrow-diameter implants (3 mm). Loads were applied as mouth-motion cycles using a step-stress accelerated life-testing method. Abutment screw failure was the chief failure mode. Strength and reliability were significantly higher for Groups 1 and 3 compared with Group 2.
Urban, et al.[24] identified risk factors for early failure of immediately placed implants in molar regions associated with three bone regenerative techniques. Ninety-two patients in need of a single implant crown to replace a molar were included. After placing the implant, patients were randomized to one of three treatment groups for bone reconstruction of remaining peri-implant defects: Autologous bone (AB) chips, ossix membrane (OM), or a combination of AB chips and OM. The implant was submerged, and after 4 months of healing a re-entry surgery was made to connect a healing abutment. Implants with a dehiscence on ≥ 2 sites (mesial/distal/oral/buccal), together with ≥ 50% visible threads, were judged as failures. A series of simple logistic regression analyses was performed to identify risk factors for failure among the following independent variables: Sex, jaw, smoking status, plaque, bleeding on probing, fistula, extraction reason, mean initial peri-implant defect size, treatment group, implant length, buccal bone dehiscence (BBD), soft-tissue dehiscence, and infection. Fifteen implants failed before abutment operation (13 explantations and 2 non-osseo-integrated). Treatment group had no impact on failure. Risk factors for failure were smoking >10 cigarettes per day, BBD, and infection. There was no difference in failure rate between three bone reconstructive techniques.
In our series SVR and SCR were 91.7% and 97%, respectively. Statistical analysis demonstrated that no studied variable had an impact on survival (i.e., lost implants) as well as on clinical success (i.e., crestal bone resorption).
CONCLUSION
OPIs are reliable devices for oral rehabilitation in molar areas.
ACKNOWLEDGEMENTS
This work was supported by the University of Ferrara (F.C.), Ferrara, Italy and by PRIN 2008 (20089MANHH_004).
Footnotes
Source of Support: This work was supported by the University of Ferrara (F.C.), Ferrara, Italy and by PRIN 2008 (20089MANHH_004)
Conflict of Interest: None declared
REFERENCES
- 1.Fugazzotto PA. Implant placement at the time of maxillary molar extraction: Treatment protocols and report of results. J Periodontol. 2008;79:216–23. doi: 10.1902/jop.2008.070338. [DOI] [PubMed] [Google Scholar]
- 2.Cafiero C, Annibali S, Gherlone E, Grassi FR, Gualini F, Magliano A, et al. Immediate transmucosal implant placement in molar extraction sites: A 12-month prospective multicenter cohort study. Clin Oral Implants Res. 2008;19:476–82. doi: 10.1111/j.1600-0501.2008.01541.x. [DOI] [PubMed] [Google Scholar]
- 3.Matarasso S, Salvi GE, Iorio Siciliano V, Cafiero C, Blasi A, Lang NP. Dimensional ridge alterations following immediate implant placement in molar extraction sites: A six-month prospective cohort study with surgical re-entry. Clin Oral Implants Res. 2009;20:1092–8. doi: 10.1111/j.1600-0501.2009.01803.x. [DOI] [PubMed] [Google Scholar]
- 4.Acocella A, Bertolai R, Sacco R. Modified insertion technique for immediate implant placement into fresh extraction socket in the first maxillary molar sites: A 3-year prospective study. Implant Dent. 2010;19:220–8. doi: 10.1097/ID.0b013e3181dbe2fe. [DOI] [PubMed] [Google Scholar]
- 5.Brunelli G, Carinci F, Zollino I, Candotto V, Scarano A, Lauritano D. Peri-implantitis: A case report and literature review. Eur J Inflamm. 2012;10:1–6. [Google Scholar]
- 6.Brunelli G, Carinci F, Zollino I, Candotto V, Scarano A, Lauritano D. SEM evaluation of 10 infected implants retrieved from man. Eur J Inflamm. 2012;10:7–12. [Google Scholar]
- 7.Scarano A, Murmura G, Carinci F, Lauritano D. Immediately loaded small diameter dental implants: Evaluation of retention, stability and comfort for the edentulous patient. Eur J Inflamm. 2012;10:19–24. [Google Scholar]
- 8.Fanali S, Carinci F, Zollino I, Brugnati C, Lauritano D. One-piece implants installed in restored mandible: A retrospective study. Eur J Inflamm. 2012;10:37–41. [Google Scholar]
- 9.Fanali S, Carinci F, Zollino I, Brugnati C, Lauritano D. A retrospective study on 83 one-piece implants installed in resorbed maxilla. Eur J Inflamm. 2012;10:55–8. [Google Scholar]
- 10.Fanali S, Carinci F, Zollino I, Brunelli G, Minguzzi R. Effect of distance between one piece implants on crestal bone resorption. Eur J Inflamm. 2011;9:1–6. [Google Scholar]
- 11.Fanali S, Carinci F, Zollino I, Brunelli G, Minguzzi R. Effect of one-piece implant diameter on clinical outcome. Eur J Inflamm. 2011;9:7–12. [Google Scholar]
- 12.Fanali S, Carinci F, Zollino I, Brunelli G, Minguzzi R. Impact of one-piece implant length on clinical outcome. Eur J Inflamm. 2011;9:13–8. [Google Scholar]
- 13.Fanali S, Carinci F, Zollino I, Brunelli G, Minguzzi R. Welding improves the success rate of one-piece implants. Eur J Inflamm. 2011;9:19–24. [Google Scholar]
- 14.Fanali S, Carinci F, Zollino I, Brunelli G, Minguzzi R. Bio-grip and machined titanium stimulate dental pulp stem cells towards osteoblast differentiation. Eur J Inflamm. 2011;9:25–30. [Google Scholar]
- 15.Danza M, Palmieri A, Farinella F, Brunelli G, Carinci F, Spinelli S. Three dimensional finite element analysis to detect stress distribution in spiral implants and surrounding bone. Dent Res J. 2009;6:59–64. [PMC free article] [PubMed] [Google Scholar]
- 16.Albrektsson T, Zarb GA. Determinants of correct clinical reporting. Int J Prosthodont. 1998;11:517–21. [PubMed] [Google Scholar]
- 17.Holst S, Hegenbarth EA, Schlegel KA, Holst AI. Restoration of a nonrestorable central incisor using forced orthodontic eruption, immediate implant placement, and an all-ceramic restoration: A clinical report. J Prosthet Dent. 2007;98:251–5. doi: 10.1016/S0022-3913(07)00266-1. [DOI] [PubMed] [Google Scholar]
- 18.Chu FC, Deng FL, Siu AS, Chow TW. The use of immediate implant placement for the replacement of a periodontally involved malaligned lateral incisor: A clinical report. J Prosthet Dent. 2007;98:423–8. doi: 10.1016/S0022-3913(07)00300-9. [DOI] [PubMed] [Google Scholar]
- 19.Paolantonio M, Pedrazzoli V, di Murro C, di Placido G, Picciani C, Catamo G, et al. Clinical significance of Actinobacillus actinomycetemcomitans in young individuals during orthodontic treatment. A 3-year longitudinal study. J Clin Periodontol. 1997;24:610–7. doi: 10.1111/j.1600-051x.1997.tb00237.x. [DOI] [PubMed] [Google Scholar]
- 20.Penarrocha M, Lamas J, Penarrocha M, Garcia B. Immediate maxillary lateral incisor implants with nonocclusal loading provisional crowns. J Prosthodont. 2008;17:55–9. doi: 10.1111/j.1532-849X.2007.00242.x. [DOI] [PubMed] [Google Scholar]
- 21.Degidi M, Nardi D, Piattelli A. Immediate rehabilitation of the edentulous mandible with a definitive prosthesis supported by an intraorally welded titanium bar. Int J Oral Maxillofac Implants. 2009;24:342–7. [PubMed] [Google Scholar]
- 22.Annibali S, Bignozzi I, Iacovazzi L, La Monaca G, Cristalli MP. Immediate, early, and late implant placement in first-molar sites: A retrospective case series. Int J Oral Maxillofac Implants. 2011;26:1108–22. [PubMed] [Google Scholar]
- 23.Freitas-Junior AC, Bonfante EA, Martins LM, Silva NR, Marotta L, Coelho PG. Effect of implant diameter on reliability and failure modes of molar crowns. Int J Prosthodont. 2011;24:557–61. [PubMed] [Google Scholar]
- 24.Urban T, Kostopoulos L, Wenzel A. Immediate implant placement in molar regions: Risk factors for early failure. Clin Oral Implants Res. 2012;23:220–7. doi: 10.1111/j.1600-0501.2011.02167.x. [DOI] [PubMed] [Google Scholar]


