Abstract
The congenital granular cell epulis (CGCE) is a rare tumor, which is apparent at birth. The histogenesis is still uncertain, but several theories, including origin from epithelial, undifferentiated mesenchymal cells, pericytes, fibroblasts, smooth muscle cells, and nerve-related cells have been proposed. This case report describes management of a 2-day-old baby girl having a large, round, soft, single 3 × 4 cm, pedunculated swelling, on the lower anterior ridge, which was causing difficulty in feeding. Clinical diagnosis of congenital epulis (CE) was made and lesion was excised under conscious sedation. A vessel running over the surface of the lesion was continuous on the alveolar ridge. To reduce intra-operative hemorrhage transfixion suture was passed around the vessel on the alveolar ridge. Then the lesion was excised from the base of peduncle with a scalpel. Histopathologically, the diagnosis of a congenital granular cell lesion of the jaw was given. Follow up of 3 months shows no signs of recurrence. CGCE may interfere with feeding, requiring a conservative excision as soon as the child is fit to undergo surgery. Tendency for recurrence and malignant transformation has not been documented.
Keywords: Congenital epulis, congenital granular cell lesion, epulis
INTRODUCTION
The word “Epulis” has previously been described for the lesion on gingiva. The term is derived from a Greek word meaning “on the gum” or gum boil. This gingival overgrowth was first described by Neumann in 1871.[1] To date, fewer than 200 cases have been described in the literature.[2] The exact nature of this entity is not clear. Fuhr and Krogh in an excellent centennial review of congenital epulis (CE) noted that tumor occurred 8 times more frequently in females than males and 3 times more often on the maxilla than the mandible.[3] The histogenesis is mostly uncertain, but several theories like origin from epithelial, undifferentiated mesenchymal cells, pericytes, fibroblasts, smooth muscle cells, and nerve-related cells have been proposed.[2]
The lesion clinically presents in the form of a pedunculated, non-ulcerated reddish pink mass of varying sizes. However, multiple lesions may also occur in the same or different alveolar ridges. Histologically it shows characteristically large cells with granular cytoplasm and spindle cells resembling fibroblasts. The lesion shows a benign behavior and no recurrence or metastasis has been reported.
We report here a unique case of congenital granular cell epulis (CGCE) in a newborn baby causing feeding problems. This was dealt by multidisciplinary approach.
CASE REPORT
This case report is unique due to the fact that the patient was referred to us within an hour of the delivery of a baby girl weighing 2.3 kg who was a product of normal full-term pregnancy having a single, large, oblong, lobulated swelling on the mandibular anterior alveolar ridge. Surface of the swelling was smooth, red colored and showed prominent blood vessels. The large size of the lesion was causing feeding problems. A clinical diagnosis of CE was made by the maxillofacial surgery team [Figure 1]. Further consultations with the treating gynecologist, pediatrician and an anesthesiologist were done and the patient was operated under conscious sedation within the next few hours. General anesthesia was placed in spare to manage intra-operative complications like blood asphyxiation and other airway related problems. Local infiltration was done with 2% lignocaine with 1:100,000 adrenaline. The feeder vessels were seen to be originating from the alveolar ridge. Hence a transfixion suture had to be placed slightly away from the lesion on the alveolar ridge so as to achieve pre-excision hemostasis and minimize the chances of intra-operative bleeding which could have endangered the airway. The lesion was completely excised from the base and was subjected to histopathological examination. The patient was kept on observation for the next 24 hours. No untoward complication was seen. The patient was recalled after 6 days for suture removal. The healing was satisfactory and the feeding habits were seen to be normalized.
Figure 1.

Clinically large protruding lesion in newborn
HISTOPATHOLOGY
H and E stained section shows lesional tissue comprising of large, rounded and polyhedral, histiocyte-like cells with small, dark oval eccentrically placed nuclei and abundant eosinophilic granular cytoplasm. Lesional cells are usually rounded but may be somewhat spindled. Numerous vascular spaces and extravasated RBCs are seen in between granular cells. Fibrous stroma is scanty. The tumor cells extend to the overlying epithelium, which is atrophic. Final diagnosis of CGCE was made based on clinical and histopathological features [Figures 2 and 3]. Further we did immunohistochemical staining of the section with vimentin to differentiate whether it is of mesenchymal origin or epithelial origin. Vimentin positive staining confirmed mesenchymal origin of these granular cells [Figure 4].
Figure 2.
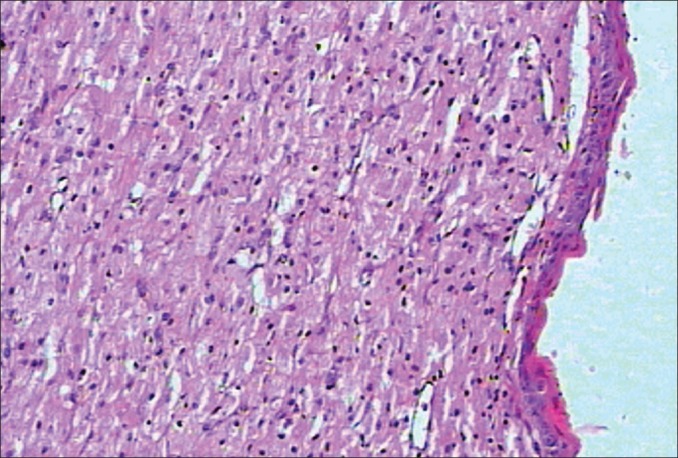
Lesional cells are compactly arranged with indistinct cytoplasmic outline (×10)
Figure 3.
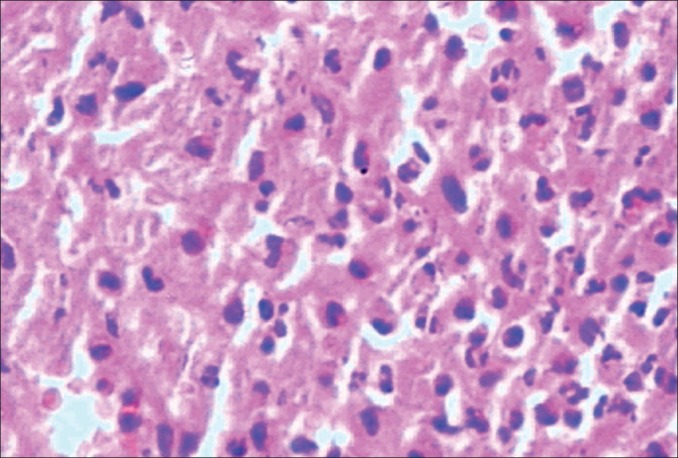
Lesional cells are large, rounded and polyhedral in shape with small, dark oval eccentrically placed nuclei and abundant eosinophilic granular cytoplasm (×40)
Figure 4.
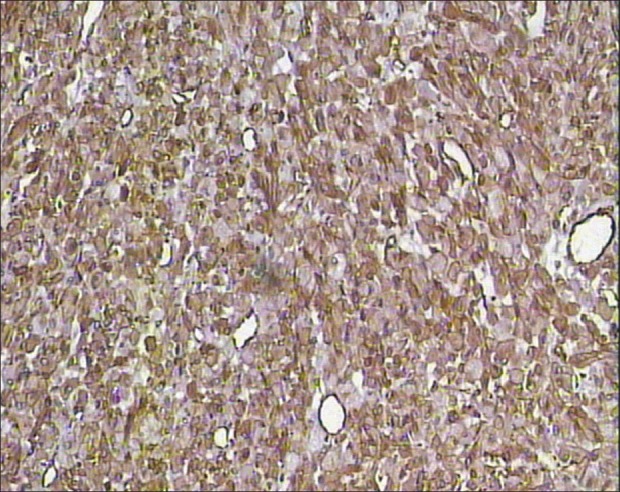
Vimentin positivity on immunohistochemical staining
DISCUSSION
CE is the term most commonly used and widely accepted. It is a rare, benign soft tissue tumor seen only in the newborn and is a different entity from other granular cell tumors as the lesion shows no propensity towards malignancy or recurrence.[4] It appears as a mass arising in the mouth and originates from the alveolar ridge. It is more common in the upper jaw and in girls. The tumor is usually solitary, but occasionally multiple tumors are found and they may interfere with respiration or feeding.[4] Antenatal ultrasonographic diagnoses of CE have been described in the literature. The earliest reported case was identified by ultrasound in a 31-week fetus.[5] There is no tenderness or surface change and the lesion does not increase in size after birth. In fact, many of the smaller lesions spontaneously regress after birth.[6,7]
The mucosal mass is comprised almost entirely of large, rounded and polyhedral, histiocyte-like cells with small, dark, oval nuclei and abundant eosinophilic granular cytoplasm. Lesional cells are usually rounded but may be somewhat spindled. There are vascular channels between granular cells, but fibrous stroma is minimally present and often appears to be completely lacking. The tumor cells extend to the overlying epithelium, which is atrophic and never demonstrates the pseudoepitheliomatous hyperplasia so commonly seen in the granular cell tumor of adults.[6,7,8]
The fact that CE arises in the newborn may lead to the hypothesis that maternal hormonal influence is an important factor in the growth of the lesion.
It is not yet clear if CE of the newborn represents a neoplastic or reactive lesion. The absence of local recurrence even after incomplete excision, the possibility of a spontaneous regression, and the lack of a malignant counterpart all favor a non-neoplastic origin.
Ultrastructural studies have suggested that CE originates from primitive mesenchymal cells with myofibroblastic differentiation.[9,10]
In the present case vimentin positivity confirms mesenchymal origin of these granular cells. This is exclusively absent in granular cell tumor which shows positivity for S-100 protein, neuronal-specific enolase, and carcinoembryonic antigen (CEA).[2]
Recommended management for epulis is surgical excision, although some opt to wait for spontaneous regression if the mass is small and is not interfering with respiration or feeding. In addition to simple excision, undermining and advancing gingivo-periosteal flaps, and suturing them over the bony defect, thus extrapolating the techniques used by Millard and Latham for cleft alveolar management have also been reported.[6]
CONCLUSION
CGCE is a simple yet uncommon entity that manifests as an aberration in an otherwise healthy child. It leads to concern or even cause hysteria in the parents who often require proper counseling. The management of this lesion is a team effort by the maxillofacial surgeon, gynecologist, pediatrician and anesthesiologist.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Neumann E. Ein von congenital epulis. Arch Heilkd. 1871;12:189–90. [Google Scholar]
- 2.Leocata P, Bifaretti G, Saltarelli S, Corbacelli A, Ventura L. Congenital (granular cell) epulis of the newborn: A case report with immunohistochemical study on the histogenesis. Ann Saudi Med. 1999;19:527–9. doi: 10.5144/0256-4947.1999.527. [DOI] [PubMed] [Google Scholar]
- 3.Fuhr AH, Krogh PH. Congenital epulis of the newborn: Centennial review of the literature and a report of case. J Oral Surg. 1972;30:30–5. [PubMed] [Google Scholar]
- 4.Lapid O, Shaco-Levy R, Krieger Y, Kachko L, Sagi A. Congenital epulis. Pediatrics. 2001;107:E22. doi: 10.1542/peds.107.2.e22. [DOI] [PubMed] [Google Scholar]
- 5.Kim YD, Kim HJ, Lee NK, Ha WH, Lee CH, Park SE. Congenital epulis: Prenatal ultrasonographic and postnatal MR features with pathologic correlation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:743–8. doi: 10.1016/j.tripleo.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 6.Narasimhan K, Arneja JS, Rabah R. Treatment of congenital epulis (granular cell tumour) with excision and gingivoperiosteoplasty. Can J Plast Surg. 2007;15:215–8. doi: 10.1177/229255030701500411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dash JK, Sahoo PK, Das SN. Congenital granular cell lesion “congenital epulis”–report of a case. J Indian Soc Pedod Prev Dent. 2004;22:63–7. [PubMed] [Google Scholar]
- 8.Kaiserling E, Ruck P, Xiao JC. Congenital epulis and granular cell tumor: A histologic and immunohistochemical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:687–97. doi: 10.1016/s1079-2104(05)80253-7. [DOI] [PubMed] [Google Scholar]
- 9.Bosanquet D, Roblin G. Congenital epulis: A case report and estimation of incidence. Int J Otolaryngol. 2009;2009:508780. doi: 10.1155/2009/508780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lifshitz MS, Flotte TJ, Greco MA. Congenital granular cell epulis. Immunohistochemical and ultrastructural observations. Cancer. 1984;53:1845–8. doi: 10.1002/1097-0142(19840501)53:9<1845::aid-cncr2820530908>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]


