Abstract
Background:
A review of literature revealed that, although the involvement of temporomandibular joint (TMJ) in rheumatoid arthritis (RA) patients is not uncommon, variation in presentation persist. Comparative studies of bony changes in the right and left TMJ with the right and left peripheral hand (Metacarpophalangeal-MCP)/wrist joints have not been done, to the best of our knowledge.
Materials and Methods:
In this cross-sectional study, the temporomandibular and hand (MCP) and wrist joints of fifteen rheumatoid arthritis patients were evaluated with questionnaires, clinical and lab assessment and radiographically using conventional radiographs and computed tomography. Students t-test was applied for the statistical analysis of the data obtained and a P value of 0.05 was considered as statistically significant.
Results:
Comparisons between the right TMJ with right MCP/wrist joint and left TMJ with left MCP/wrist joint did not reveal statistically significant results. Radiographically, flattening and erosions were the common manifestations. MCP joints were more affected than the wrist, but whenever the wrist was involved, it was more likely to be bilaterally affected.
Conclusions:
Although the TMJ showed osseous changes of a higher grade than the hand (MCP) and wrist joints radiographically, it was observed that patients were more aware of the peripheral joint discomfort. There were no significant differences between TMJ and peripheral joints on both right and left sides.
Keywords: Diagnostic imaging, hand joints, rheumatoid arthritis, temporomandibular joint
INTRODUCTION
The temporomandibular joints (TMJ) or the craniomandibular joints are one of the important joints in the body which may be subjected to disease processes like degeneration and inflammation.
The commonest of the inflammatory joint diseases is Rheumatoid Arthritis (RA) which is a chronic multisystem disease. The disease is characterized by a pathologic immune response that affects the synovial cells, cartilage and bone resulting in joint destruction and permanent disability.
It is not specific to any particular race or region, the prevalence being 1-2% of the population world wide. Females are three times more prone for affliction than males. Although, it can occur at any age, the peak incidence is during the fourth and sixth decades of life. RA often affects the peripheral small joints like the fingers and toes, eventually involving other joints like knee and shoulder.[1,2,3,4] Studies of the incidence of TMJ symptoms in RA have shown wide range of figures of involvement varying from 2-86%.[2,3,4,5]
The position and relative anatomy of TMJ and its surrounding structures requires a skillful and accurate technique of imaging for a detailed study. The first reported formal study of TMJ in RA was done by Cadenat and Blanc (1958) in fifteen patients, which revealed radiographic changes in the TMJ, as well as other joints. The frequency of radiologic findings in the TMJ has been reported to be between 19% and 84% in patients with RA.[6] Also, studies thus far have revealed an involvement of TMJ in RA with many patients having significant changes radiographically, but less clinical signs and symptoms when compared to the peripheral joints.
With this in mind, a study was undertaken to evaluate radiographically the extent of TMJ involvement as compared to hand (MCP)/wrist joints in RA patients by using conventional and modern imaging techniques. Also, an assessment of the TMJ's and peripheral joints on the right and left sides was done, to ascertain, if certain joints were more prone to disease processes, based on functional inequalities.
MATERIALS AND METHODS
This study was approved by the ethics committee of SDM College of Dental Sciences, Karnataka, India. Fifteen patients in the age group of 20-60 years (11 females and 4 males) were selected for this study, out of a referral pool of patients from the Oral Medicine, Rheumatology and Orthopaedics clinics. Informed consent was obtained from all the patients.
Inclusion criteria
Patients with a diagnosis of RA according to the American Rheumatism Association's Revised Criteria for Rheumatoid Arthritis.[7] Only patients over the age of 18 were included.
Exclusion criteria
Patients with joint involvement other than the TMJ/hand (MCP) and wrist joint were not included. Patients with myofascial pain, TMJ ankylosis, headache, patients with known history of previous trauma, cervical spondylosis and pregnant females were not included.
Detailed case history as per the questionnaire was taken. As the patients were known RA patients, the primary focus was to ascertain the onset, duration, site, type of symptoms like pain, limited/altered movement of the hands and jaw etc. Visual Analog scale was used. Patients were also questioned on psychosocial history and any prior treatments undertaken. Clinical assessment of TMJ for function and range (deviation/limitation) of movement, pain in the joint proper or while biting, audible or palpable clicking of joints were recorded. Examination of the mouth was carried out at the same time as the clinical examination of the joint. Any occlusal discrepancies were noted. Examination of hand/wrist joints for soft tissue swelling, pain, limitation of movement, tenderness to palpation, difficulty in performing simple functions like writing or picking up objects and deformities was done. In all cases, only abnormalities present at the time of examination were recorded.
Laboratory tests involving erythrocyte sedimentation rate (ESR-westergren's method) and RA test using the Rhelax Rf slide test kit (Tulip, India) was used in this study for the determination of rheumatoid factor.
Radiographic evaluation of the TMJ was carried out using the conventional projections, transcranial and OPG and advanced computed tomography (CT). Posteroanterior view (PA) of the hand and wrist joints was also taken.
Transcranial views of right and left TM joints of all patients were taken using Siemens Vertix 100 extraoral radiographic machine with a setting of 70-72 mAs and 74-82 KVp on an average.
Orthopantomographs were taken using the Villa rotograph machine with a machine setting of 70-75 KVp and 60 mAs.
Ten patients were subjected to CT scans using the Toshiba 2D CT scanner model- 300 S and with a machine setting of 150 KVp and 250 mAs on an average. Slices of 2 mm thickness were taken in both the coronal and axial sections. The remaining five patients were not willing for CT examinations.
PA views of the hand and wrist were made with the Siemens Vertix 100 extra oral radiographic machine with a setting of 55 KVp and 6-8 mAs on an average.
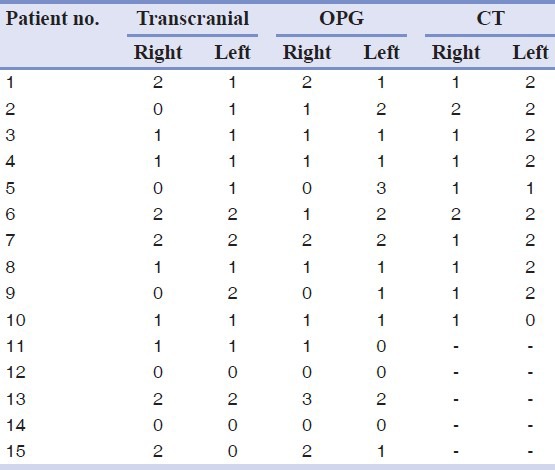
Detailed analysis of the hand and wrist radiographs was performed based on Larsen's gradings[8] [Table 1]. For the TMJ, the gradings were restricted to the condyle proper, as the glenoid fossa could not be clearly visualized in all the radiographs. Since the anatomy of the TMJ is different from that of the hand and foot joints, a modification of the grading system proposed by Larsen et al.[8] was made for the TMJ [Tables 2 and 3].[9] These radiographs were assessed individually by a medical and oral radiologist. During the process of deliberation the conclusion arrived at by the examiners were noted.
Table 1.
Radiographic interpretation (gradings) of hand and wrist joints from PA view
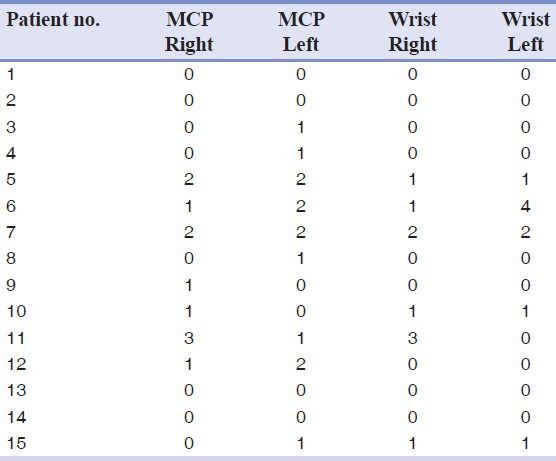
Table 2.
Modified grading system for evaluation of TMJ radiographs[9]
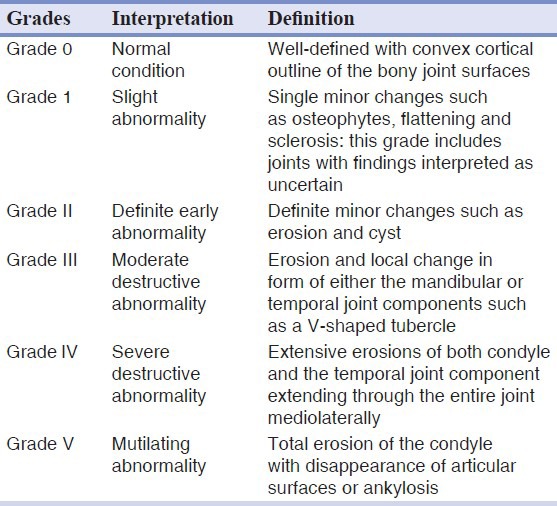
Table 3.
Radiographic interpretation (gradings) of TMJ from transcranial, OPG and CT
Student's t-test was applied for the statistical analysis of the data obtained.
RESULTS
The study was carried out in the proposed manner and the data was statistically analyzed.
Of the 15 patients taken randomly, 11 (73.3%) were females and 4 (26.6%) were males. Ten patients (67%) were seropositive for rheumatoid factor. Values higher than 20 mm for ESR have been taken as abnormal i.e. 13 patients (87%), thereby showed abnormal values.
Comparison of the TMJ with the hand (MCP) and wrist on the right and left side did not reveal any statistically significant results. The results were not significant when the individual joints were compared on the right and left sides [Tables 4 and 5].
Table 4.
Comparison of right TMJ (Transcranial and OPG) with right hand (MCP) and wrist and comparison of left TMJ (Transcranial and OPG) with left hand (MCP) and wrist
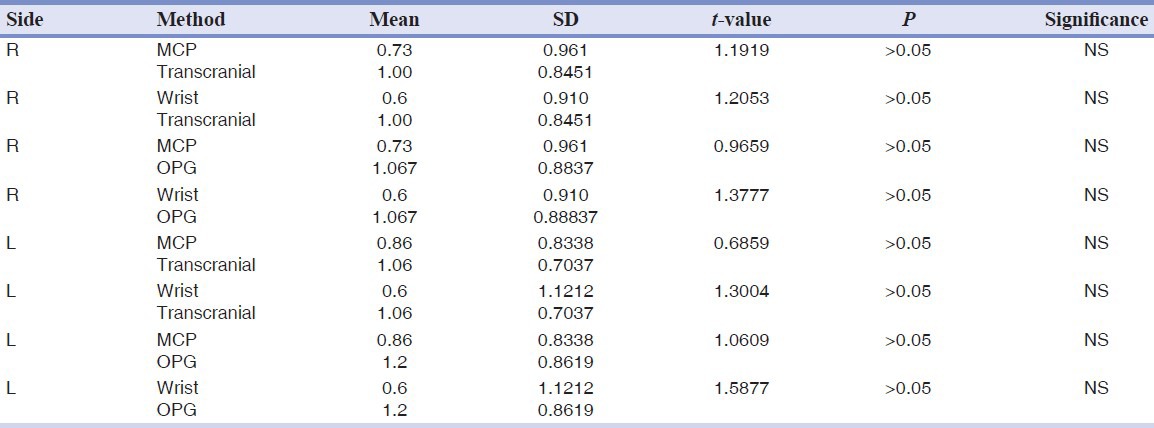
Table 5.
Comparison between right and left sides of hand and wrist joints and TMJ
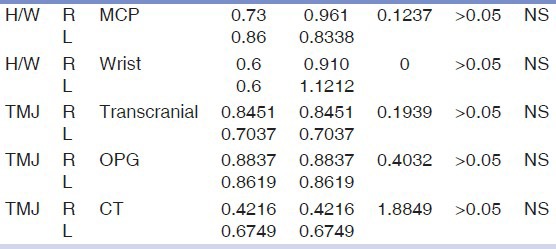
It was however noticed that hand (MCP) joints were more frequently affected when compared to wrist joints and when the wrist was involved, it was bilaterally involved [Figure 1].
Figure 1.
No of patients with unilateral/bilateral/normal joint involvement of the hand- MCP and Wrist and TMJ- as visualised from Transcranial (trans), OPG and CT
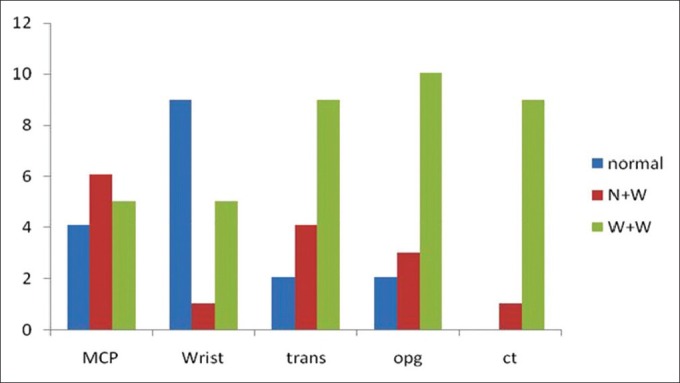
Comparison of the mean gradings of the TMJ and MCP and wrist joints on the right and left side indicated a higher grade on left side [Figure 2].
Figure 2.
Bar graph showing the radiographic mean gradings across TMJ's and peripheral joints
DISCUSSION
Rheumatoid arthritis is a chronic destructive inflammatory disease process known to commonly affect the peripheral joints. This results in joint effusion, swelling, pain, limitation in movement and deformities. The TMJ like the peripheral hand and wrist joints can be a site for chronic synovial inflammation. TMJ involvement in RA results in clinical symptoms like pain, swelling, crepitation, stiffness and limitation in jaw movement.[10]
Radiography is a frequently used diagnostic aid to detect and assess disease severity and response to treatment. The radiographic findings ascribed to RA in the TMJ are erosion and flattening of the condylar head, limitation of movement, marginal proliferations and sclerosis.
In this study, the temporomandibular joints of 15 patients (30 joints) with definite RA were compared with their hand (MCP) and wrist joints to assess the degree of involvement in each case using the transcranial radiograph, OPG and CT scans. Of the 15 patients, 11 (73%) were females and 4 (23%) were males, in the ratio of 2.7:1. This incidence rate indicates that RA affects women approximately three times more than men and is consistent with the well documented findings of other authors.[11,12,13,14]
The mean age of incidence of rheumatoid arthritis in this study is 34.5 years. This finding is comparable with that of the age of patients (35) in the study conducted by Mc Carthy[11] but not in agreement with that of 55 years of Ogus[12] and 56.4 years of Syrjanen.[3] This disparity could be because of the difference in sample size, the higher age group and also the racial differences in other studies.
It was observed that although all the patients presented with complaints of either swelling, morning stiffness or limitation of movement of the MCP and wrist joints, the TMJs were symptomatic in five patients only (33%). TMJ symptoms were less noticed by the patient who has more stiffness and pain with visible inflammatory signs in other joints. Also, patients often attributed TMJ symptoms to tooth related problems. In this study, other symptoms of TMJ involvement like restriction in mouth opening was not observed which is consistent with previous reports.[5,12]
Most studies indicate that TMJ lesions found radiographically vary in frequency from 50% to 80% in RA.[15] In this study, conventional methods revealed that 13 RA patients (87%) had radiographic evidence of TMJ abnormalities (from slight to marked) in one or both TM joints, which is in consonance with the previous studies.[12,16] However, bilateral presentation was observed in 9 (60%) and 10 (67%) patients with the transcranial and OPG, respectively. Symmetric involvement of both right and left joints have been reported in previous studies as well.[12,13]
CT scans were performed to assess whether any additional radiographic changes could be observed in the TMJ and to confirm the accuracy of the findings obtained with transcranial and OPG. It was found that all the patients exhibited radiographic abnormalities, with 9 (90%) patients showing bilateral presentation.
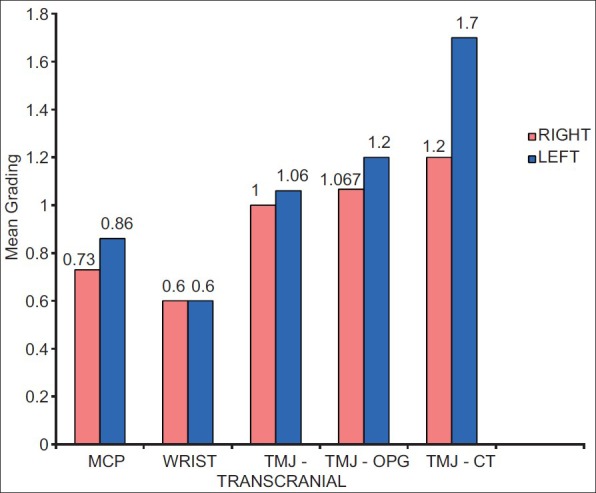
The present study shows that flattening [Figure 3] and bone erosion of the condyle was the most common radiographic manifestations. Of the 15 patients i.e. 30 joints evaluated, transcranial view revealed involvement of 9 TM joints (30%) as erosions and 16 joints (44%) as flattening. This was followed by osteophytes/marginal proliferations seen in 3 joints (10%) and subcortical cyst in 1 joint (3%). Sclerosis and ankylosis could not be visualized from this technique.
Figure 3.
OPG showing flattening of the temporomandibular joint on the left side with normal right TMJ
In OPG, 9 joints (30%) revealed bone erosions, flattening in 14 joints (46%), osteophytes in 2 joints (6%) and cyst in 1 joint (3%). No other radiographic abnormalities could be detected. The low frequency of erosions in the present study is comparable with the finding of less involvement of 24% of the joints in the study by Syrjanen, 1985.
CT scans of all the ten patients showed either mild or moderate involvement of the temporomandibular joint. The higher incidence of positive findings like erosions and joint space narrowing observed in this study is comparable with other studies [Figures 4 and 5].[17,18]
Figure 4.
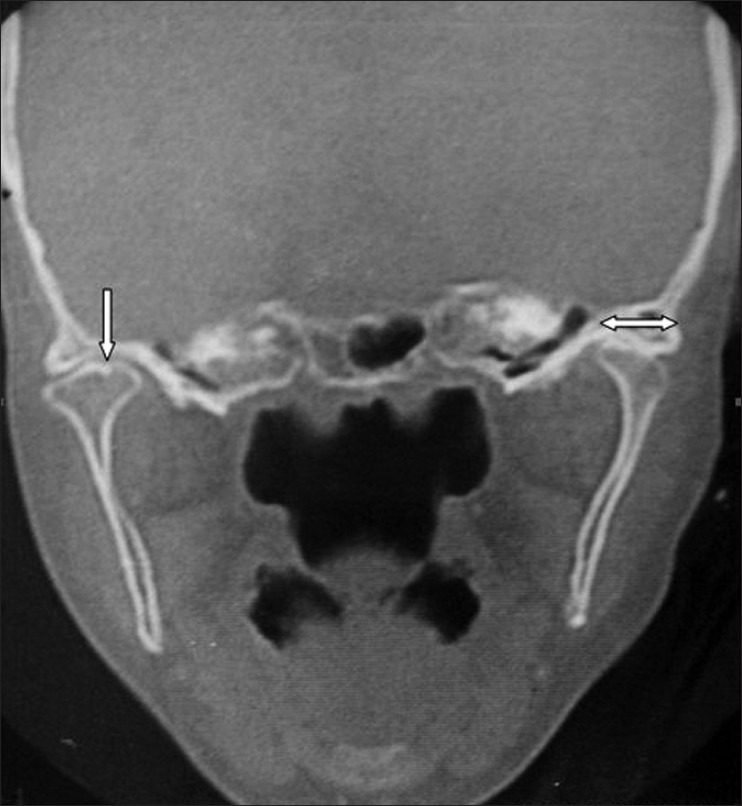
Coronal CT showing erosive changes and decreased joint space of right and left TMJ's
Figure 5.

Axial CT shows subchondral cyst in the left TMJ
The analysis of the data revealed possibility of a relationship between TMJ abnormalities and the duration and severity of disease. It was observed that in long standing cases, there was a corresponding increase in degree of structural changes as evidenced in radiographs. In this study, 4 of the 5 patients with TMJ symptoms had duration of disease exceeding 3 years. This may be attributed to the fact that as the disease progresses the chronic inflammatory process results in increased joint destruction. The most common radiographic findings are erosion and flattening of the head of the mandible and articular fossa and reduction of the joint spaces, usually noticed 5 to 10 years after the onset of symptoms.[19,20]
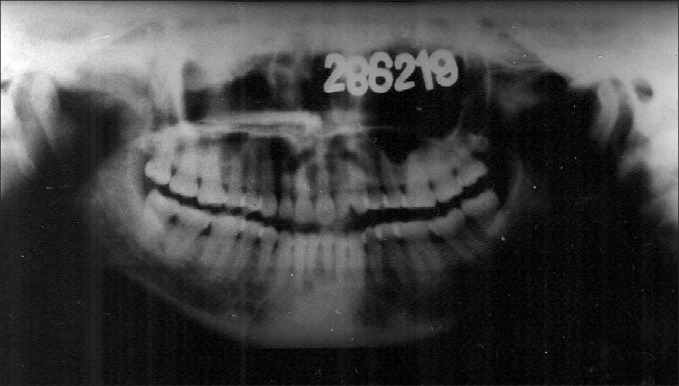
The hand (MCP) and wrist joints of all the patients exhibited radiographic abnormalities on both right and left sides [Figure 6]. Interestingly, it was noted that MCP joints were more affected than the wrist, but whenever wrist was involved, it was more likely to be bilaterally affected and showed a greater grade on radiographs. The most common findings were erosions, flattening and decreased joint space. However, one patient presented with ankylosis of the wrist joints on the left side. This patient aged 60 years had suffered from the disease for more than 10 years.
Figure 6.
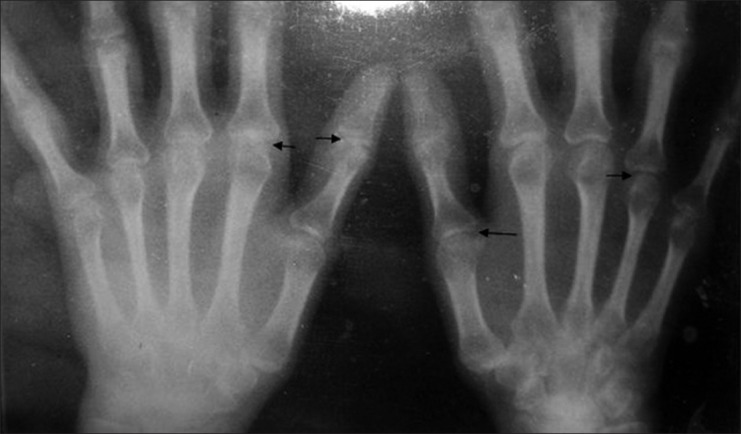
PA view of the hands shows erosive changes in the MCP and wrist joints of both hands
Upon evaluation of the data obtained from this study, it was found that the TMJ and the hand (MCP) and wrist joints of patients with rheumatoid arthritis exhibited similar radiographic abnormalities on both right and left sides. This finding is consistent with the findings of Akerman et al., in 1991[21] where they found no significant differences between the changes in TMJ and hand (MCP) and wrist joints.
Functional inequalities, if any, owing to the use of the right side over the left in the peripheral joints does not seem to have any significance with regard to the extent of disease progression. In the TMJ, functional movements like chewing on the right or left side more than the other also does not cause a corresponding increase in disease activity as evidenced by radiographic findings.
CONCLUSION
The results of the present study showed similar changes in the TMJ and MCP and wrist joints of patients with RA. Flattening and erosions were the common manifestations seen on radiographs. Though, 87% of patients had definite radiographic changes in the TMJ, only 33% of them had clinical symptoms such as pain on biting followed by tenderness to palpation.
Few studies have compared radiographically the bony changes in right and left TMJ's with the right and left hand (MCP) and wrist joints in Rheumatoid Arthritis patients. Although, statistically insignificant results and sample size limits this study, it is worthwhile to note that most RA patients exhibit similar TMJ bony changes along with peripheral joints.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Carlsson GE, Kopp S, Oberg T. Temporomandibular Joint Function and Dysfunction. Copenhagen: Munksgaard; 1979. Arthritis and Allied Diseases of the Temporomandibular joint; pp. 269–320. [Google Scholar]
- 2.Ericson S, Lundberg M. Alterations in the temporomandibular joint at various stages of rheumatoid arthritis. Acta Rheumatol Scand. 1967;13:257–74. doi: 10.3109/rhe1.1967.13.issue-1-4.22. [DOI] [PubMed] [Google Scholar]
- 3.Syrjanen SM. The temporomandibular joint in rheumatoid arthritis. Acta Radiol Diagn (Stockh) 1985;26:235–43. doi: 10.1177/028418518502600302. [DOI] [PubMed] [Google Scholar]
- 4.Tegelberg A, Kopp S. Subjective symptoms from the stomatognathic system in individuals with rheumatoid arthritis and osteoarthrosis. Swed Dent J. 1987;11:11–22. [PubMed] [Google Scholar]
- 5.Franks AS. Temporomandibular joint in adult rheumatoid arthritis. A comparative evaluation of 100 cases. Ann Rheum Dis. 1969;28:139–45. doi: 10.1136/ard.28.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goupille P, Fouquet B, Cotty P, Goga D, Mateu J, Valat JP. The temporomandibular joint in rheumatoid arthritis. Correlations between clinical and computed tomography features. J Rheumatol. 1990;17:1285–91. [PubMed] [Google Scholar]
- 7.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 8.Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 1977;18:481–91. doi: 10.1177/028418517701800415. [DOI] [PubMed] [Google Scholar]
- 9.Rohlin M, Petersson A. Rheumatoid arthritis of the temporomandibular joint: Radiologic evaluation based on standard reference films. Oral Surg Oral Med Oral Pathol. 1989;67:594–99. doi: 10.1016/0030-4220(89)90279-x. [DOI] [PubMed] [Google Scholar]
- 10.Bessa-Nogueira RV, Vasconcelos BC, Duarte AP, Bezerra TP, Góes PS. Targeted assessment of the temporomandibular joint in patients with rheumatoid arthritis. J Oral Maxillofac Surg. 2008;66:1804–11. doi: 10.1016/j.joms.2007.08.037. [DOI] [PubMed] [Google Scholar]
- 11.Mc Carthy. 3rd ed. Philadelphia: W.B. Saunders; 1972. A textbook of medical problems in dentistry. [Google Scholar]
- 12.Ogus H. Rheumatoid arthritis of the temporomandibular joint. Br J Oral Surg. 1975;12:275–84. doi: 10.1016/0007-117x(75)90058-x. [DOI] [PubMed] [Google Scholar]
- 13.Zide MF, Carlton DM, Kent JN. Rheumatoid disease and related arthropathies. Oral Surg Oral Med Oral Pathol. 1986;61:119–25. doi: 10.1016/0030-4220(86)90170-2. [DOI] [PubMed] [Google Scholar]
- 14.Klasser GD, Balasubramaniam R, Epstein J. Topical review-connective tissue diseases: Orofacial manifestations including pain. J Orofac Pain. 2007;2:171–84. [PubMed] [Google Scholar]
- 15.Larheim TA, Tveito L, Dale K, Ruud AF. Temporomandibular joint abnormalities in rheumatoid arthritis: Comparison of different radiographic methods. Acta Radiol Diagn (Stockh) 1981;22:703–7. doi: 10.1177/028418518102200615. [DOI] [PubMed] [Google Scholar]
- 16.Chalmers IM, Blair GS. Rheumatoid arthritis of the temporomandibular joint. A clinical and radiological study using circular tomography. Q J Med. 1973;42:369–86. [PubMed] [Google Scholar]
- 17.Goupille P, Fouquet B, Cotty P, Goga D, Valat JP. Direct coronal computed tomography of the temporomandibular joint in patients with rheumatoid arthritis. Br J Radiol. 1992;65:955–60. doi: 10.1259/0007-1285-65-779-955. [DOI] [PubMed] [Google Scholar]
- 18.Ardic F, Gokharman D, Atsu S, Guner S, Yilmaz M, Yorgancioglu R. The comprehensive evaluation of temporomandibular disorders seen in rheumatoid arthritis. Aust Dent J. 2006;51:23–8. doi: 10.1111/j.1834-7819.2006.tb00396.x. [DOI] [PubMed] [Google Scholar]
- 19.Yoshida A, Higuchi Y, Kondo M, Tabata O, Ohishi M. Range of motion of the temporomandibular joint in rheumatoid arthritis: Relationship to the severity of disease. Cranio. 1998;16:162–7. doi: 10.1080/08869634.1998.11746054. [DOI] [PubMed] [Google Scholar]
- 20.Celiker R, Gokce-Kutsal Y, Eryilmaz M. Temporomandibular joint involvement in rheumatoid arthritis: Relationship with disease activity. Scand J Rheumatol. 1995;24:22–5. doi: 10.3109/03009749509095149. [DOI] [PubMed] [Google Scholar]
- 21.Akerman S, Jonsson K, Kopp S, Petersson A, Rohlin M. Radiologic changes in temporomandibular, hand and foot joints of patients with rheumatoid arthritis. Oral Surg Oral Med Oral Pathol. 1991;72:245–50. doi: 10.1016/0030-4220(91)90171-8. [DOI] [PubMed] [Google Scholar]


