Abstract
Objective
Co-occurring depression is common in patients seeking treatment for anxiety; however, the literature on the effects of depression on anxiety treatment outcomes is inconclusive. The current study evaluated prescriptive and prognostic effects of depression on anxiety treatment outcomes in a large primary care sample.
Method
Data were analyzed from a randomized controlled effectiveness trial that compared Coordinated Anxiety Learning and Management (CALM) to usual care (UC). The study enrolled 1,004 patients between June 2006 and April 2008. Patients were referred by their primary care provider and met DSM-IV criteria for generalized anxiety disorder, panic disorder, posttraumatic stress disorder, and/or social anxiety disorder. They were treated for 3 to 12 months with CALM (computer-assisted cognitive-behavioral therapy, medication management, or their combination) or UC. Outcomes were evaluated by blinded assessment at 6, 12, and 18 months. Effects of baseline major depressive disorder (MDD) on anxiety symptoms, anxiety-related disability, and response/remission rates were evaluated using statistical models accounting for baseline anxiety and patient demographics.
Results
MDD did not moderate the effects of CALM (relative to UC) on anxiety symptoms, anxiety-related disability, or response/remission rates. Greater improvements in anxiety symptoms and anxiety-related disability were observed in depressed patients, regardless of treatment assignment (p’s < .005). However, depressed patients also displayed higher absolute anxiety symptom and anxiety-related disability scores at baseline and all subsequent assessments (p’s < .001). Depressed patients also displayed lower remission rates at each follow-up (p’s < .001).
Conclusions
CALM had comparable advantages over UC for patients with and without MDD. Depressed patients displayed more severe anxiety symptoms and anxiety-related disability at baseline, but their clinical improvement was substantial and larger in magnitude than that observed in the non-depressed patients. Results support the use of empirically supported interventions for anxiety disorders in patients with co-occurring depression.
Keywords: anxiety, depression, randomized controlled trial, primary care, cognitive-behavioral therapy
Introduction
Epidemiological studies1, 2 report high comorbidity rates among anxiety and mood disorders in the general population, and co-occurrence of these disorders is even higher in treatment-seeking samples.3,4 Patients with principal anxiety disorders who also meet criteria for a mood disorder have more severe anxiety symptoms, impairment, and course.5 Understanding the effects of co-occurring depression on treatment for anxiety disorders is important, particularly if effects are discovered that have implications for treatment selection or implementation.
The available literature does not permit strong conclusions about the influence of depression on anxiety treatment outcomes. Most studies have considered depression as a potential predictor or prognostic indicator of outcome (i.e., a variable that demonstrates a relationship to outcome variables irrespective of treatment assignment). 6 Results of these studies have been mixed; some7–11 observed that co-occurring depression predicted reduced improvement of anxiety symptoms while others12–18 found no significant effects of depression on degree of clinical improvement. Lack of consistent findings may be attributable to a variety of factors from heterogeneous patient samples, study interventions, and assessment measures to statistical issues related to small sample sizes.
Randomized controlled trials of anxiety interventions have rarely evaluated depression as a potential moderator or prescriptive indicator of outcome (i.e., a variable that interacts with treatment assignment and affects outcome differentially across groups).19 Studies to date that have included this type of analysis reported no significant prescriptive effects of depression on anxiety outcomes.20,21 However, additional work (preferably with larger samples) is needed before conclusions about the prescriptive effects of depression can be drawn.
In the present investigation, we aimed to clarify the effects of depression on anxiety treatment outcomes by analyzing data from a large sample (N > 1000) of primary care patients with anxiety disorders who received treatment as part of the Coordinated Anxiety Learning and Management (CALM) study. The CALM intervention is superior to usual care (UC) in reducing anxiety symptoms and anxiety-related disability (and in producing clinical response and remission) during 18 months of follow-up.4, 22 However, it is unknown whether these effects are moderated by co-occurring depression.
Based on the available literature, we hypothesized that: (1) depressed patients would display more severe anxiety symptoms and anxiety-related disability at baseline, (2) depressed patients would display more severe anxiety symptoms and anxiety-related disability at follow-ups (prognostic effects); and (3) despite higher overall levels of anxiety symptoms and anxiety-related disability, the effectiveness of CALM (relative to UC) in improving anxiety outcomes would not vary based on depression status (i.e., co-occurring depression would not be a prescriptive indicator of outcome).
Method
Participants
Participants were patients enrolled in the CALM study, an RCT conducted in 17 primary care clinics located in Seattle, WA; Los Angeles, CA; San Diego, CA; and Little Rock, AR. Patients provided informed consent to participate and the study was approved by Institutional Review Boards at all study sites. Patients were referred to the study by their primary care providers; in some clinics, referral was facilitated by a 5-item anxiety screener. 23
Between June 2006 and April 2008, 1004 patients with DSM-IV anxiety disorders [panic disorder (PD), generalized anxiety disorder (GAD), posttraumatic stress disorder (PTSD), and/or social anxiety disorder (SAD)], aged 18 to 75 years, English- or Spanish-speaking, were enrolled in the study. Most co-occurring disorders, including MDD, were permitted; active suicidal intent or plan, psychosis, Bipolar I, and substance use disorders (except for alcohol and marijuana abuse) were cause for exclusion. Table 1 presents the demographic and diagnostic characteristics of the sample.
Table 1.
Baseline Patient Characteristicsa
| All | No Major Depressive Disorder |
With Major Depressive Disorder |
|
|---|---|---|---|
| (N = 1004) | (n = 356) | (n = 648) | |
| Age, mean (SD), y | 43.47(13.44) | 42.25(13.67) | 44.15(13.28) |
| Women | 714(71.12) | 239(67.14) | 475(73.30) |
| Education | |||
| < High school | 55(5.49) | 9(2.53) | 46(7.12) |
| 12 y | 165(16.47) | 44(12.36) | 121(18.73) |
| > 12 y | 782(78.04) | 303(85.11) | 479(74.15) |
| Ethnicity | |||
| Hispanic | 196(19.52) | 63(17.70) | 133(20.53) |
| African American | 116(11.55) | 26(7.30) | 90(13.89) |
| White | 568(56.57) | 223(62.64) | 345(53.24) |
| Other | 124(12.35) | 44(12.36) | 80(12.35) |
| No. of chronic medical conditions | |||
| 0 | 202(20.14) | 88(24.72) | 114(17.62) |
| 1 | 219(21.83) | 92(25.84) | 127(19.63) |
| ≥ 2 | 582(58.03) | 176(49.44) | 406(62.75) |
| Anxiety disorderb | |||
| Panic | 475(47.31) | 169(47.47) | 306(47.22) |
| Generalized anxiety | 756(75.30) | 245(68.82) | 511(78.86) |
| Social phobia | 405(40.34) | 125(35.11) | 280(43.21) |
| Posttraumatic stress | 181(18.03) | 27(7.58) | 154(23.77) |
| Type of health insuranceb | |||
| Medicaid | 101(10.08) | 23(6.46) | 78(12.07) |
| Medicare | 124(12.38) | 34(9.55) | 90(13.93) |
| Other government insurancec | 35(3.49) | 12(3.37) | 23(3.56) |
| Private insurance | 749(74.75) | 289(81.18) | 460(71.21) |
| No insurance | 141(14.07) | 39(10.96) | 102(15.79) |
| Any Opiate Use | 86(8.57) | 13(3.65) | 73(11.27) |
| Any Pain | 441(43.92) | 93(26.12) | 348(53.70) |
| Interventiond | 503(50.10) | 173(48.60) | 330(50.93) |
Data are reported as No. (%) unless otherwise indicated.
Because patients could have more than one, ns may total more than 1004.
Includes Veterans’ Administration benefits, TRICARE, county programs, or other government insurance not otherwise specified.
Randomization to CALM intervention (versus usual care) was stratified by presence/absence of Major Depressive Disorder.
Design of the CALM Study
Prior reports4,24 provided detailed descriptions of the CALM study design. Briefly, eligible participants were randomly assigned to CALM or UC; randomization was stratified by clinic and presence/absence of MDD. Stratification therefore ensured equivalent assignment of participants with MDD to CALM and UC. Blinded telephone assessments were performed by the RAND Survey Research Group at baseline, 6, 12, and 18 months. Study retention was high and similar for the CALM and UC groups, with more than 80% of participants assessed at each follow-up.
Intervention
Patients assigned to UC received care as usual from their primary care physician, with no restrictions imposed (e.g., patients could receive pharmacotherapy, in-house counseling if available, or be referred out for specialty care). Patients assigned to CALM met with an Anxiety Clinical Specialist (ACS) and were given the choice of computer-assisted cognitive-behavioral therapy (CBT), medication management, or both. The majority of patients selected CBT, either as monotherapy or in combination with medication.4
The CALM algorithm allowed for multiple treatment steps (up to 4 steps over the course of 12 months), which could include either “stepping up” by adding more of the same modality (e.g., providing CBT sessions focused on a secondary anxiety disorder; adding a second antidepressant or a benzodiazepine to first-line pharmacotherapy) or “stepping over” by switching to or adding the other modality. Once patients had achieved criteria for remission 4 or improved to the degree where they did not want further treatment, they entered a relapse prevention phase where they received monthly phone calls to reinforce CBT skills, medication adherence, or both, until the 12-month treatment period had elapsed. Prior reports provide additional details of the CALM intervention 4, 24, 25 and ACS training.26
Measures
Depression
DSM-IV MDD and other diagnoses were established using the Mini International Neuropsychiatric Interview (MINI), version 5.0.27 Reliability and validity of MDD diagnoses established using the MINI is satisfactory.27 The MINI was conducted in-person by the ACS at the participant’s primary care clinic. Depressive symptoms also were measured during the baseline telephone assessment using items from the Patient Health Questionnaire-9 (PHQ-9), a reliable and valid measure of depressive symptoms.28
Anxiety Symptoms
The primary outcome of the CALM study was the sum of the Anxiety and Somatization subscales of the well-validated Brief Symptom Inventory.29 This subset of 12 items (BSI-12) captures psychic and somatic anxiety, which characterize all anxiety disorders.4
Anxiety-related Disability
Disability was measured using the well-validated Sheehan Disability Scale (SDS),30 which measures the degree to which symptoms disrupt work/school, social functioning, and family/home life. For the CALM study, the instructions that preceded each of the ratings were modified to target anxiety-related disability (e.g., “Anxiety, tension, and worry symptoms have disrupted your work/schoolwork…”).
Response and Remission
Following the main CALM outcome study, treatment response was defined as achieving a 50% or greater reduction in baseline BSI-12 score, or meeting the criteria for remission.4 Remission was defined as a BSI-12 score of 6 or less (i.e., a per-item average of 0.5 or the midpoint of “none” and “mild”).
Statistical Analysis/Design of the Current Study
To estimate the effect of baseline MDD over time, we jointly modeled the outcomes (BSI-12 and SDS scores) at the four assessment points by Treatment Assignment (CALM vs. UC), Time (baseline, 6, 12, and 18 months), MDD (presence vs. absence of MDD at baseline)*, and the interaction of Treatment Assignment, Time, and MDD. Study site, education level, gender, race/ethnicity, and age were included in all models as covariates. In models where the 3-way (Treatment Assignment × Time × MDD) interaction was non-significant, we refit the model including 2-way interactions of Treatment Assignment × Time and MDD × Time, dropping the 3-way interactions. Time was treated as a categorical variable. To avoid restrictive assumptions, the covariance of the outcomes at the four assessment points was left unstructured.
We fitted the proposed model using a restricted maximum likelihood approach, which produces valid estimates under the missing-at-random assumption.31 This approach correctly handles the additional uncertainty arising from missing data and uses all available data to obtain unbiased estimates for model parameters.32 This is an efficient way to conduct intent-to-treat analyses as it includes all participants with a baseline assessment.
For cross-sectional analyses involving response and remission rates, we used attrition weights to correctly account for participants who missed one or more follow-ups.33
The statistical software used was SAS version 9 (SAS Institute Inc., Cary, NC). All p values were two-tailed and a conservative significance level of p < .01 was adopted to account for multiple comparisons.
Results
Demographic and Diagnostic Differences Related to MDD
Table 1 summarizes the demographic and diagnostic characteristics of participants with and without MDD. Nearly two-thirds (64.5%) of the sample met criteria for MDD at baseline. The group with MDD had higher proportions of Hispanic and African American participants, and a lower proportion of White participants (p = .005). Those with MDD also reported lower educational levels (p < .001) and more chronic medical conditions (p < .001), pain (p < .001), and opiate use (p < .001). They were more likely to have Medicaid (p = .005) and less likely to have private insurance (p = .001). Greater proportions of participants with MDD met criteria for GAD (p < .001) and PTSD (p < .001).
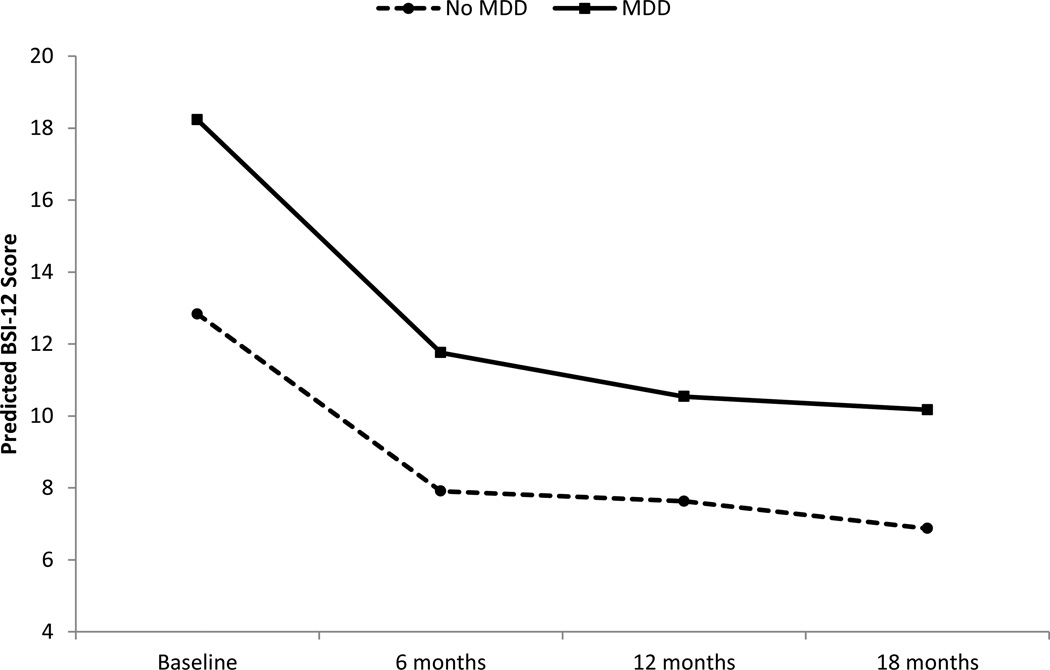
Effects of MDD on Anxiety Symptoms
The Treatment Assignment × Time × MDD effect on BSI-12 scores was non-significant (p = .555), indicating that baseline MDD did not moderate the effects of CALM on anxiety symptoms. Two-way interactions were then examined, revealing a significant MDD × Time effect on BSI-12 scores [F(3,991) = 5.08, p = .002]. Depressed participants displayed larger decreases in anxiety symptoms, regardless of Treatment Assignment (see Figure 1). While the group difference was not significant at p < .01 at 6 months [mean difference, −1.40, SE = 0.60; t(991) = −2.35, p = .019], a significant difference was observed at 12 months [mean difference, −2.34, SE = 0.62; t(991) = −3.79, p < .001], and 18 months [mean difference, −1.96, SE = 0.63; t(991) = −3.11, p = .002]. A main effect of MDD also was observed whereby BSI-12 scores were higher for patients with baseline MDD, regardless of Time or Treatment Assignment [mean difference, 5.25, SE = 0.57; t(991) = 9.22, p < .001; see Figure 1].
Figure 1.
Predicted Mean BSI-12 Score at baseline, 6 months, 12 months, and 18 months by MDD status. BSI-12 = 12-item version of the Brief Symptom Inventory (Anxiety + Somatization Subscales). MDD = Major Depressive Disorder.
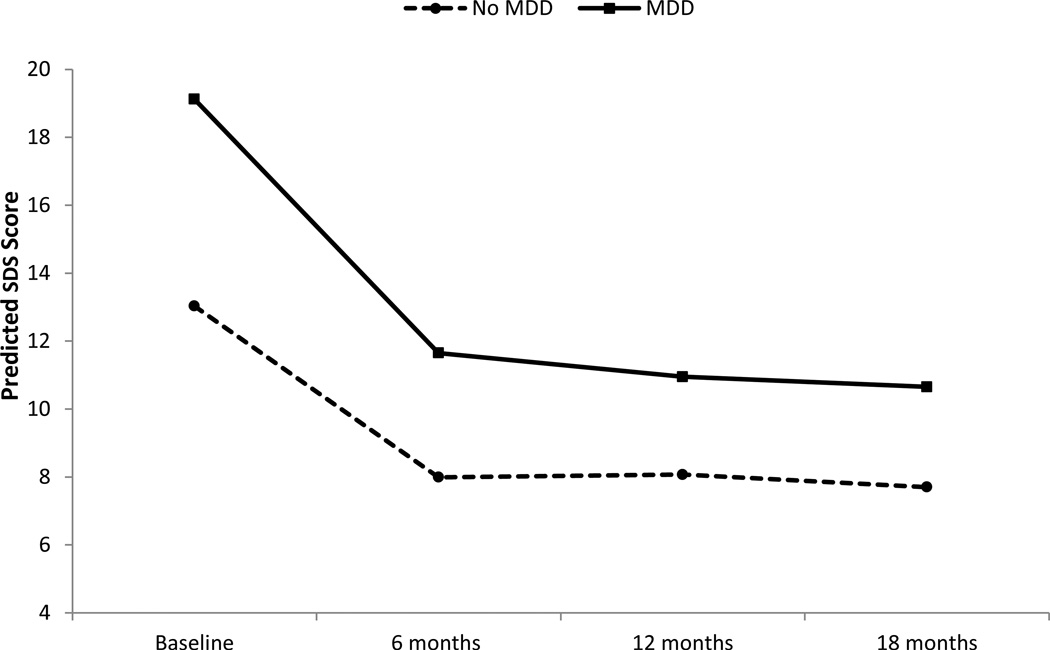
Effects of MDD on Anxiety-Related Disability
The Treatment Assignment × Time × MDD effect on SDS scores was non-significant (p = .524), indicating that baseline MDD did not moderate the effects of CALM on anxiety-related disability. Two-way interactions were then examined, revealing a significant MDD × Time interaction [F(3,991) = 10.99, p < .001]. Depressed participants displayed larger decreases in anxiety-related disability, regardless of Treatment Assignment (see Figure 2). This was observed at 6 months [mean difference, −2.26, SE = 0.56; t(991) = −4.02, p < .001], 12 months [mean difference, −3.03, SE = 0.56; t(991) = −5.39, p < .001], and 18 months [mean difference, −2.96, SE = 0.60; t(991) = −4.93, p < .001]. A main effect of MDD also was observed whereby disability was higher for participants with baseline MDD, regardless of Time or Treatment Assignment [mean difference, 5.91, SE = 0.45; t(991) = 13.25, p < .001; see Figure 2].
Figure 2.
Predicted Mean SDS Score at baseline, 6 months, 12 months, and 18 months by MDD status. SDS = Sheehan Disability Scale (modified to capture disability related to anxiety); MDD = Major Depressive Disorder.
Effects of MDD on Response and Remission
There were no significant Treatment Assignment × MDD interaction effects on response rates at 6, 12, or 18 months (p’s >.14; see Table 2). A main effect of MDD was observed at 6 months (p = .009), in which participants with MDD displayed a lower response rate (44%; CI = 39–48%) than those without MDD (53%; CI = 47–59%). However, between-groups differences did not meet the threshold for significance at 12 months (p = .144) or 18 months (p = .025; see Table 2).
Table 2.
Proportion Achieving Response and Remission From Baseline BSI-12 Scorea
| MDD at Baseline | No MDD at Baseline | |||||
|---|---|---|---|---|---|---|
| CALM | Usual Care | CALM | Usual Care | |||
| Proportion (95% CI) | Proportion (95% CI) | p value | Proportion (95% CI) | Proportion (95% CI) | p value | |
| Response b | ||||||
| 6 mo | 0.56(0.50 to 0.61) | 0.32(0.26 to 0.38) | <.001 | 0.62(0.54 to 0.69) | 0.44(0.37 to 0.52) | 0.002 |
| 12 mo | 0.63(0.57 to 0.69) | 0.41(0.35 to 0.47) | <.001 | 0.66(0.57 to 0.73) | 0.50(0.42 to 0.58) | 0.009 |
| 18 mo | 0.64(0.58 to 0.70) | 0.46(0.40 to 0.52) | <.001 | 0.67(0.59 to 0.75) | 0.60(0.52 to 0.68) | 0.236 |
| Remission c | ||||||
| 6 mo | 0.41(0.35 to 0.47) | 0.20(0.15 to 0.25) | <.001 | 0.48(0.41 to 0.56) | 0.39(0.31 to 0.47) | 0.087 |
| 12 mo | 0.50(0.44 to 0.56) | 0.26(0.21 to 0.32) | <.001 | 0.55(0.47 to 0.63) | 0.43(0.35 to 0.51) | 0.040 |
| 18 mo | 0.50(0.43 to 0.56) | 0.28(0.22 to 0.34) | <.001 | 0.55(0.46 to 0.63) | 0.50(0.42 to 0.58) | 0.421 |
Abbreviations: BSI-12 = 12-item version of Brief Symptom Inventory (Anxiety + Somatization Subscales). MDD = Major Depressive Disorder. CI = confidence interval.
Data presented as proportion weighted for non-response at each follow-up.
Response defined as ≥ 50% reduction on the BSI-12, with all those in remission considered to have responded; 95% CI in parentheses.
Remission defined as a per item BSI-12 score of <0.5 (total score <6); 95% CI in parentheses.
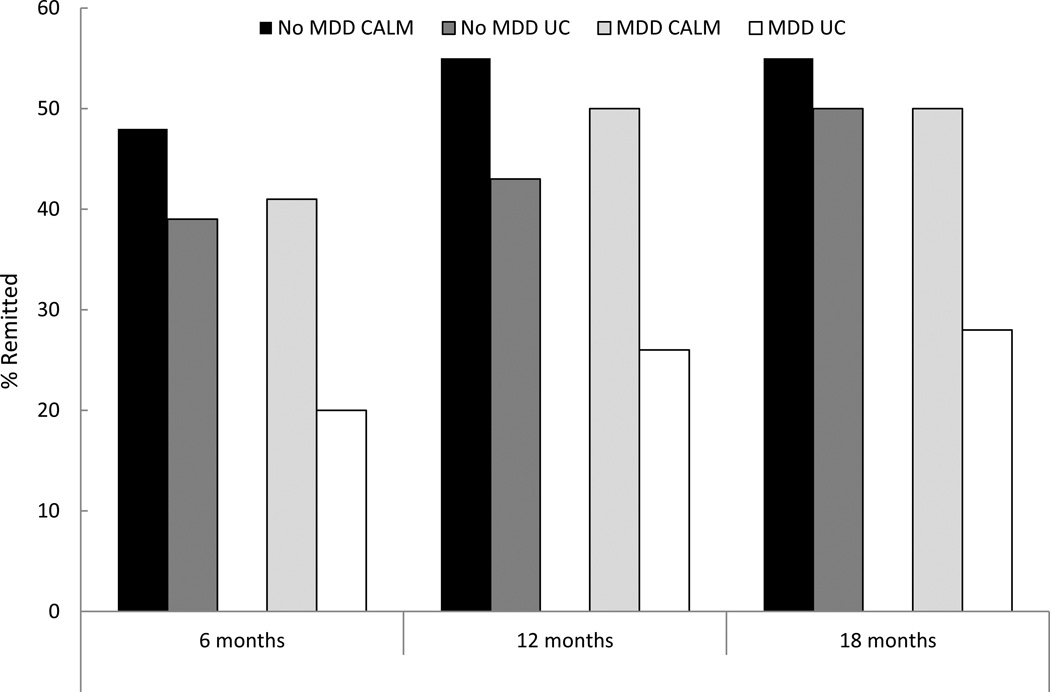
MDD × Treatment Assignment interaction effects also were non-significant for remission at 6 months (p = .038), 12 months (p = .094), and 18 months (p = .015). Although not significant at p < .01, it is noteworthy that at 6 months, twice the percentage of depressed patients receiving CALM (41%) achieved remission compared to those receiving UC (20% remission, or a 21% advantage for CALM; see Table 2 and Figure 3). The difference in 6-month remission rates for CALM versus UC was less pronounced for the non-depressed group (48% vs. 39%, or a 9% advantage for CALM). This pattern also was apparent at 12 and 18 months (see Table 2 and Figure 3). Main effects of MDD on remission rates were observed at all 3 assessment points (ps < .003), with remission rates being lower for participants with MDD (see Table 2).
Figure 3.
Proportion remitted at 6, 12, and 18 months by Baseline MDD Status and Treatment Assignment. MDD = Major Depressive Disorder. CALM = Coordinated Anxiety Learning and Management. UC = Usual Care.
Discussion
Co-occurring depression was common in this sample of primary care patients with anxiety disorders, with nearly two-thirds of patients meeting criteria for MDD at baseline. This comorbidity rate is consistent with the extensive literature showing a strong association between anxiety and mood disorders, particularly in clinical samples.5 Depressed participants had higher rates of GAD, PTSD, and medical comorbidity than non-depressed participants and endorsed more severe anxiety symptoms and anxiety-related disability at baseline. Socio-demographically, participants with co-occurring MDD were more likely to identify as Hispanic and African-American, to endorse a low educational level, and to qualify for Medicaid. These baseline findings suggest that primary care patients with co-occurring anxiety disorders and MDD often present with additional clinical complexities (e.g., co-occurring medical problems, social challenges related to lower education/financial resources) that may play a role in their anxiety and mood symptoms.
Despite the more severe and complex baseline presentation of depressed participants, co-occurring MDD did not significantly moderate the effects of the CALM intervention (relative to UC) on anxiety symptoms, anxiety-related disability, or treatment response and remission rates. This finding converges with results of prior studies with smaller samples showing no prescriptive effects of depression on treatment outcomes following behavioral treatment for anxiety disorders.7,8
In contrast, co-occurring MDD was prognostic of outcomes over the 18 months of follow-up, predicting both magnitude of improvement and absolute levels of anxiety symptoms and anxiety-related disability at each assessment point. Irrespective of treatment assignment, depressed participants improved more yet still appeared worse than non-depressed participants at all follow-up assessments. The higher absolute levels of symptoms and disability (and hence lower remission rates) in the depressed group appeared to be a byproduct of their baseline elevations, which were not fully compensated for by their larger improvements on the anxiety outcome measures.
The analyses of remission rates merit comment, as the results were striking yet not significant at the a priori threshold of p < .01. For depressed patients, the 6-month remission rate in CALM was twice that of UC (41% versus 20%). The corresponding difference in the non-depressed group was less dramatic (48% versus 39%). This pattern persisted at subsequent follow-ups, and it is noteworthy that at the final assessment (18 months), depressed patients who received UC displayed particularly low remission rates (28%) compared to all other patients (50%–55%; see Table 2 and Figure 3). These data suggest that UC may have particularly low efficacy for patients with co-occurring depression; whereas higher-intensity interventions such as CALM may improve likelihood of remission in this subgroup.
Clinical Implications
As noted in previous reports,4, 22 the CALM intervention is superior to UC in reducing anxiety symptoms and anxiety-related disability in primary care patients with anxiety disorders. The current findings support the use of CALM and similar empirically supported interventions for anxiety disorders in patients with co-occurring depression. The lack of moderation of the CALM intervention effect by MDD suggests that, contrary to some clinical opinion, the potency of empirically supported treatments for anxiety is not generally compromised by co-occurring depression. On the contrary, improvements in anxiety symptoms and anxiety-related disability associated with CALM and UC were larger for the depressed versus the non-depressed participants. These improvements were not only statistically but clinically significant; collapsing across CALM and UC, the average anxiety symptom score for depressed participants was in the “mild” range at all follow-up assessments.
Factors Contributing to the Effect of Depression on Degree of Clinical Improvement
To our knowledge, co-occurring depression has not been associated with larger improvements in previous studies examining prognostic effects of depression on anxiety treatment outcomes. Prior studies found either less clinical improvement10–14 or equivalent degrees of change15–21 in depressed patients relative to comparison groups. We therefore consider potential factors that may have contributed to this discrepant finding.
First, the more naturalistic design of CALM (compared to efficacy trials) may partly explain the larger improvements observed in the depressed participants. Rather than prescribing a set number of sessions, the CALM intervention allowed clinicians and patients to work flexibly toward a goal of clinical remission. Primary care providers and any specialist clinicians who treated patients assigned to UC were presumably working toward a similar goal. Within this context, it is not entirely surprising that depressed participants displayed greater clinical change; because they started with more severe symptoms, larger decreases would be required for them to approach the goal of remission. Study clinicians had a range of options available for targeting the symptoms of patients with more complicated presentations, including “stepping up” by adding more of the initial treatment modality or “stepping over” to the alternative treatment modality.
To investigate this further, we conducted post-hoc analyses to explore whether the more severe initial presentations of depressed participants prompted clinicians to deliver treatment differently. For patients assigned to CALM, data were available from the study’s web-based tracking system (see Supplementary Table). We found that depressed and non-depressed patients assigned to CALM did not differ significantly in terms of proportions who received CBT only, medication management only, and combination treatment. There also were no significant between-groups differences in the number of contacts with study clinicians, regardless of the type of contact (in-person vs. phone; medication management vs. CBT; active treatment vs. relapse prevention). The only difference that approached statistical significance was in the direction of non-depressed patients receiving more CBT contacts; on average they received approximately one more CBT contact than depressed patients (p = .013; all other differences were non-significant at p > .10).
For the full sample, data were limited to patients’ self-reports of treatment from the baseline, 6, 12, and 18 month assessments. Rates of depressed and non-depressed patients who reported receiving key elements of CBT during treatment sessions did not differ significantly at any of the follow-ups. Not surprisingly, depressed participants were more likely to report using antidepressant or antianxiety medication of adequate type, length, and dose (see34 for the study’s operational definitions of adequate pharmacotherapy); however, the advantage that depressed patients had on this indicator of treatment quality was greater at baseline (33.0% vs. 23.7%) than at the study follow-ups . While clear implications cannot be deduced from this pattern, it is possible that the difference in rate of adequate pharmacotherapy or other aspects of medication treatment (e.g., more aggressive regimens) could have contributed to the larger improvements observed in the depressed group.
In addition to differences in treatment delivery, patient factors influencing outcome should also be considered as a potential explanation for the larger improvements in depressed patients. It is possible that participants who were more impaired at baseline (as the depressed participants were) may have been more motivated to comply with treatment recommendations than those whose symptoms were less disabling. Again, this type of effect could be more apparent in an effectiveness study conducted in a “real-world” setting than in an efficacy trial conducted in a research setting (where there may be less variability in treatment adherence due to more stringent controls in subject selection and treatment delivery).
Finally and importantly, it may have been more difficult to demonstrate change in the non-depressed participants because they endorsed relatively low anxiety symptom and anxiety-related disability scores at baseline. Conversely, the more severe baseline symptoms and disability of the depressed patients may have allowed more room for improvement on the outcome measures. This basic measurement issue could have contributed to the different magnitudes of improvement observed in the depressed and non-depressed groups.
Limitations
The current study elucidates the effects of depression on treatment for anxiety in a mixed anxiety disorder sample. Due to statistical power considerations, the study was not designed to evaluate further interactions involving specific anxiety disorder diagnoses (i.e., 4-way interactions among Principal Anxiety Diagnosis, MDD, Treatment Assignment, and Time). The results reported here cannot be assumed to apply uniformly to each individual anxiety disorder.
In addition, the CALM study evaluated a multifaceted intervention involving CBT, medication management, or their combination. Our results pertain specifically to the effects of depression on the CALM package compared to UC. Design considerations preclude us from drawing conclusions regarding the influence of depression on the effectiveness of specific components of CALM. While participants were randomly assigned to CALM or UC, the components of CALM they received (CBT, medication management) were not randomly assigned but dictated by patient and provider choice. Future investigations should evaluate potential prescriptive effects of depression on the specific modalities of CBT and pharmacotherapy, as this could aid in selection of an optimal empirically supported intervention for anxiety.
Conclusions and Future Directions
Co-occurring depression did not moderate the effects of CALM on anxiety symptoms, anxiety-related disability, or response/remission rates. Improvements in anxiety symptoms and anxiety-related disability were clearly demonstrated for depressed participants. These results support the use of interventions such as CALM for patients with co-occurring depression, especially when considered in conjunction with findings that depressive symptoms often improve with effective treatment of anxiety disorders.4, 35 Clinicians implementing such interventions in primary care settings can expect higher absolute levels of anxiety-related symptoms and disability (as well as additional complexities such as medical comorbidity and challenges related to social conditions) in depressed patients relative to non-depressed patients referred for similar interventions. However, the magnitude of improvement also may be greater for the depressed patients. Some noteworthy findings that did not meet the a priori threshold for statistical significance suggested the possibility of a stronger advantage of CALM over UC in producing remission of anxiety symptoms in the depressed participants. Future research should continue to explore the issue of whether higher-intensity interventions such as CALM are even more strongly indicated in anxiety patients with more complicated initial presentations involving co-occurring depression.
Supplementary Material
Clinical Points.
Depression is common in patients seeking treatment for anxiety disorders, and depressed patients often present with more severe anxiety symptoms and other clinical complexities.
Depression does not, however, compromise the effectiveness of standard treatments for anxiety disorders; on the contrary, substantial reductions in anxiety symptoms and disability are observed in depressed patients receiving treatment for anxiety disorders.
Empirically supported treatments for anxiety (cognitive-behavioral therapy, medication management, or their combination) should typically be offered to patients with co-occurring depression.
Acknowledgments
This work was supported by grants U01 MH057858 (Dr. Roy-Byrne), U01 MH058915 (Dr. Craske), U01 MH 070022 (Dr. Sullivan), U01 MH070018 (Dr. Sherbourne), U01 MH057835 and K24 MH64122 (Dr. Stein), and K01 MH072952 (Dr. Chavira) from the National Institute of Mental Health, Bethesda, MD, USA.
Footnotes
Disclosures: Dr. Roy-Byrne is a consultant to Valant Medical Solutions (EMR Company), and is Editor-in-Chief of Journal Watch Psychiatry, Depression and Anxiety, and UpToDate Psychiatry. Dr. Stein is paid for his editorial work on the journal Depression and Anxiety and the evidence-based medical information provider, UpToDate Psychiatry. The other authors have no disclosures.
Analyses were repeated using baseline scores on the items from the PHQ-9 in place of MDD diagnostic status. The same pattern of results was obtained, suggesting that the effects of depression reported here are robust to differences in construct definition (categorical vs. dimensional) and mode of assessment (clinician-administered versus self-report). Results of the analyses using the PHQ-9 items are available upon request.
References
- 1.Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch General Psychiatry. 2005 Oct;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 3.Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110(4):585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- 4.Roy-Byrne P, Craske MG, Sullivan G, et al. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huppert JD. Anxiety disorders and depression comorbidity. In: Antony MMS, Stein MB, editors. Oxford Handbook of Anxiety and Related Disorders. New York, NY: Oxford University Press; 2009. pp. 576–586. [Google Scholar]
- 6.Kraemer HC, Wilson GT, Fairburn CG, et al. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 7.Chambless DL, Tran GQ, Glass CR. Predictors of response to cognitive-behavioral group therapy for social phobia. J Anxiety Disord. 1997;11(3):221–240. doi: 10.1016/s0887-6185(97)00008-x. [DOI] [PubMed] [Google Scholar]
- 8.Abramowitz JS. Treatment of obsessive-compulsive disorder in patients who have comorbid depression. J Clin Psychol. 1994;60:1133–1141. doi: 10.1002/jclp.20078. [DOI] [PubMed] [Google Scholar]
- 9.van Balkom AJLM, van Boeijen CA, Boeke AJP, et al. Comorbid depression, but not comorbid anxiety disorders, predicts poor outcome in anxiety disorders. Depress Anx. 2008;25:408–415. doi: 10.1002/da.20386. [DOI] [PubMed] [Google Scholar]
- 10.Keijsers GPJ, Hoogduin CAL, Schaap CPDR. Prognostic factors in the behavioural treatment of panic disorder with and without agoraphobia. Behav Ther. 1994;25:689–708. [Google Scholar]
- 11.Keijsers GPJ, Hoogduin CAL, Schaap CPDR. Predictors of treatment outcome in the behavioural treatment of obsessive-compulsive disorder. Br J Psychiatry. 1994;165:781–786. doi: 10.1192/bjp.165.6.781. [DOI] [PubMed] [Google Scholar]
- 12.Chavira DA, Stein MB, Golinelli D, et al. Predictors of clinical improvement in a randomized effectiveness trial for primary care patients with panic disorder. J Nerv Ment Dis. 2009;197(10):715–721. doi: 10.1097/NMD.0b013e3181b97d4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLean PD, Woody S, Taylor S, et al. Comorbid panic disorder and major depression: implications for cognitive-behavioral therapy. J Consult Clin Psychol. 1998;66(2):240–247. doi: 10.1037//0022-006x.66.2.240. [DOI] [PubMed] [Google Scholar]
- 14.Steketee G, Siev J, Fama JM, et al. Predictors of treatment outcome in modular cognitive therapy for obsessive-compulsive disorder. Depress Anx. 2011;28(4):333–341. doi: 10.1002/da.20785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown TA, Antony MM, Barlow DH. Diagnostic comorbidity in panic disorder: effect on treatment outcome and course of comorbid diagnoses following treatment. J Consult Clin Psychol. 1995;63(3):408–418. doi: 10.1037//0022-006x.63.3.408. [DOI] [PubMed] [Google Scholar]
- 16.Aaronson CJ, Shear MK, Goetz RR, et al. Predictors and time course of response among panic disorder patients treated with cognitive-behavioral therapy. J Clin Psychiatry. 2008;69(3):418–424. doi: 10.4088/jcp.v69n0312. [DOI] [PubMed] [Google Scholar]
- 17.Allen LB, White KS, Barlow DH, et al. Cognitive-behavior therapy (CBT) for panic disorder: Relationship of anxiety and depression comorbidity with treatment outcome. J Psychopathol Behav Assess. 2010;32(2):185–192. doi: 10.1007/s10862-009-9151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erwin BA, Heimberg RG, Juster H, et al. Comorbid anxiety and mood disorders among persons with social anxiety disorder. Behav Res Ther. 2002;40(1):19–35. doi: 10.1016/s0005-7967(00)00114-5. [DOI] [PubMed] [Google Scholar]
- 19.Whisman MA. Mediators and moderators of change in cognitive therapy of depression. Psychol Bull. 1993;114(2):248–265. doi: 10.1037/0033-2909.114.2.248. [DOI] [PubMed] [Google Scholar]
- 20.Amir N, Taylor CT, Donohue MC. Predictors of response to an attention modification program in generalized social phobia. J Consult Clin Psychol. 2011;79(4):533–541. doi: 10.1037/a0023808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dow MG, Kenardy JA, Johnston DW, et al. Prognostic indices with brief and standard CBT for panic disorder: II. Moderators of outcome. Psychol Med. 2007;37(10):1503–1509. doi: 10.1017/S0033291707000682. [DOI] [PubMed] [Google Scholar]
- 22.Craske MG, Stein MB, Sullivan G, et al. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Arch Gen Psychiatry. 2011;68(4):378–388. doi: 10.1001/archgenpsychiatry.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Means-Christensen AJ, Sherbourne CD, Roy-Byrne PP, et al. Using five questions to screen for five common mental disorders in primary care: Diagnostic accuracy of the Anxiety and Depression Detector. Gen Hosp Psychiatry. 2006;28(2):108–118. doi: 10.1016/j.genhosppsych.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan G, Craske MG, Sherbourne C, et al. Design of the Coordinated Anxiety Learning and Management (CALM) study: Innovations in collaborative care for anxiety disorders. Gen Hosp Psychiatry. 2007;29(5):379–387. doi: 10.1016/j.genhosppsych.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Craske MG, Rose RD, Lang A, et al. Computer-assisted delivery of cognitive behavioral therapy for anxiety disorders in primary-care settings. Depress Anxiety. 2009;26(3):235–242. doi: 10.1002/da.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rose RD, Lang AJ, Welch SS, et al. Training primary care staff to deliver a computer-assisted cognitive-behavioral therapy program for anxiety disorders. Gen Hosp Psychiatry. 2011;33(4):336–342. doi: 10.1016/j.genhosppsych.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Int Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Derogatis L. BSI-18: Brief Symptom Inventory 18 Administration, Scoring, and Procedures Manual. Minneapolis, MN: NCS Pearson, Inc.; 2001. [Google Scholar]
- 30.Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int Clin Psychopharmacol. 1996;11(Suppl 3):89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- 31.Littell RC, Milliken GA, Stroup WW, et al. SAS System for Mixed Models. Cary, NC: SAS Institute, Inc.; 1996. [Google Scholar]
- 32.Little R, Rubin D. Statistical Analysis with Missing Data. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 33.Brick JM, Kalton G. Handling missing data in survey research. Stat Methods Med Res. 1996;5(3):215–238. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- 34.Stein MB, Roy-Byrne PP, Craske MG, et al. Quality of and patient satisfaction with primary health care for anxiety disorders. J Clin Psychiatry. 2011;72:970–976. doi: 10.4088/JCP.09m05626blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsao JC, Mystkowski JL, Zucker BG, et al. Impact of cognitive-behavioral therapy for panic disorder on comorbidity: a controlled investigation. Behav Res Ther. 2005;43(7):959–970. doi: 10.1016/j.brat.2004.11.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.