Abstract
Objectives
To use the Children’s Sleep Habits Questionnaire (CSHQ) to characterize sleep problems in a group of 5- to 6-year-old minority children living in urban communities and to compare our findings with data from 5- to 6-year-old children in the original CSHQ validation study.
Methods
A cross-sectional study design was used to collect sleep data from parents using the CSHQ.
Results
The CSHQ was completed by 160 parents; 150 (94%) scored ≥41, indicating a sleep problem. The prevalence of having sleep problems for our minority community sample was significantly higher than the original community sample (94% vs 23%, P < .001). The minority sample also had significantly higher mean total CSHQ scores (51.5 vs 37.9, P < .001) and higher scores across all 8 subscales of the CSHQ (P < .001 for all comparisons).
Conclusions
The results suggest that sleep problems may be more prevalent in urban, early-school-aged minority children than previously reported.
Keywords: child, African American, Latino, Hispanic, Children’s Sleep Habits Questionnaire
Introduction
Although studies have shown that children from minority populations take more daytime naps and have shorter nighttime sleep durations than their nonminority peers,1,2 few studies to date have focused on sleep patterns and sleep problems in early-school-aged Latino and African American children living in urban, economically disadvantaged communities.3 We studied this high-risk population because at 5 and 6 years of age, they are starting school. As a result, they may have less time available for sleep overnight because of school start times and less time for daytime naps, thereby reducing the amount of sleep at a time when the effect of shortened or disrupted sleep on learning, behavior,4 and health5 is critically important. The purpose of this study was to determine the extent of behavioral sleep problems and sleep disorders in a group of urban-dwelling, 5- to 6-year-old mostly Latino children. Additionally, our goal was to characterize the nature of the sleep problems reported by parents in this group of children.
We used the Children’s Sleep Habits Questionnaire (CSHQ), a validated, parent-report instrument commonly used to screen for childhood sleep problems,6 to identify and characterize sleep disturbances. To our knowledge, the CSHQ has not been used extensively in minority populations to examine sleep.7 Although studies have characterized the sleep habits and patterns of toddlers, preschool and elementary school-aged children using the CSHQ,2,6 the absence of substantial numbers of children from minority groups in these studies represents a major gap in our understanding of sleep in a vulnerable population known to have numerous risk factors for poor sleep. For these reasons, we sought to describe the sleep patterns and behaviors of this group of children using the CSHQ. Furthermore, we compared our results with those from the study of 5- to 6-year-old children in the original community sample used by Owens et al8 to validate the CSHQ. Our primary hypothesis was that low-income, urban minority children would have more frequent sleep problems than reported in a previous study of school-aged children by Owens et al.
Methods
Participants
Between September 2010 and April 2011, 160 parents were recruited from 4 clinical practice sites affiliated with Columbia University Medical Center (New York, NY). Parents were recruited in Family Practice, Obstetrics and Gynecology, Internal Medicine, and Pediatrics clinics while they waited to receive care for themselves or others. The communities where the practices are located serve predominantly Latino (primarily Dominican) populations. Eligibility criteria for parents were as follows: (1) legal guardian aged 18 years or older; (2) having a child 5 to 6 years of age; (3) child enrolled in school for a minimum of 5 hours per day; (4) living in permanent housing within the catchment communities for the study (not in a shelter or other temporary housing) with the child for the previous 12 months; and (5) speaking either English or Spanish. Families were excluded if a serious comorbid condition in the child was present that could affect sleep, such as (1) a clinician diagnosis of attention-deficit/hyperactivity disorder (ADHD), (2) seizures or other neurological or neuromuscular disorders, (3) autism or other types of developmental delay, or (4) psychiatric disorders. Additionally, children whose parents reported that they were taking medications for ADHD, depression, or anxiety were excluded.
Procedures
Enrollment
Enrollment procedures were completed by 3 trained, bilingual, research staff members. Parents underwent a brief screening interview to determine eligibility. They were asked if they had a 5- to 6-year-old child enrolled in school and if they were willing to participate in a study investigating children’s sleep that required the parent to complete a face-to-face interview while at the practice site. The child did not have to be present in the clinic at the time of enrollment.
Written informed consent was provided by each parent. The study protocol was approved by the Columbia University Medical Center Institutional Review Board.
Data collection
Parents who met the eligibility requirements completed an interview that included the CSHQ. The responses on the CSHQ were based on the child’s sleep behaviors during the previous week if that was a “typical” week and if not, the most recent typical week. We avoided interviewing parents during school holidays. Research staff also collected demographic and general health information about the child. The CSHQ was automatically scored on microcomputer tablets used for the study. A score of ≥41 on the CSHQ indicated the presence of a sleep problem.6
Measures
The Children’s Sleep Habits Questionnaire
Parents completed a 52-item sleep screening instrument designed to classify children with and without sleep problems.6 The CSHQ comprises 8 subscales that allow delineation of the types of sleep problems common to our group of 5- to 6-year-olds. The 8 subscales of the CSHQ include the following: (1) bedtime behavior; (2) delay in sleep onset; (3) sleep duration; (4) sleep anxiety; (5) night waking; (6) sleep-disordered breathing; (7) parasomnias; and (8) daytime sleepiness. Parental responses related to the child’s sleep behaviors occurring over a typical week were rated on a 3-point Likert scale (usually = 5–7 nights/wk, sometimes = 2–4 nights/wk, and rarely = 0–1 night/wk). The CSHQ has an internal consistency for both community samples (α = .68) and clinical samples (α = .78). Test-retest reliability is in the range of 0.62 to 0.79. A cutoff CSHQ score of 41 or higher yields a sensitivity of 0.80 and specificity of 0.72 for sleep problems.6 A higher score on the questionnaire indicates more disturbed sleep.6,8 In addition to answering “usually,” “sometimes,” or “rarely” to each item (which represented a sleep behavior) on the CSHQ, parents were asked if they thought a particular sleep behavior as represented by each item in the questionnaire was a problem or not a problem for them or their child. For example, the parent was asked, “Does your child fall asleep in his/her parent’s or sibling’s bed” and they responded either “usually,” “sometimes,” or “rarely.” The parent was then asked if this behavior is a problem for them or the child.
The CSHQ was originally validated by Owens et al6,8 using the responses of parents from 2 groups of children aged 4 to 10 years (a school-based community sample; n = 469) and a clinical sample of children referred to a pediatric sleep disorders center for evaluation of sleep problems; n = 154). Both samples were composed of residents of a predominantly white, middle-income, English-speaking suburban school district in southeastern New England in the United States. Although both samples did include some children from ethnic and racial minority groups, they were not present in large numbers. We used the data from only the 5- to 6-year-old children in Owens’s community sample for the purposes of comparison with our minority community sample. Additionally, we analyzed the data using the same items that were included on the validation survey in Owens’s community sample, so that the scores would be comparable.
Statistical Analyses
Descriptive statistics were generated for participant characteristics as well as the CSHQ total and subscale scores. To assess our primary hypothesis, we compared the prevalence of sleep problems for our minority community sample with the 5- to 6-year-olds in Owens’s community sample using the χ2 test. In addition, we performed t tests to examine the differences between the 2 groups on CSHQ total and subscale scores. To assess whether parents felt the sleep behaviors identified by the questionnaire were a problem for themselves and their child, we compared the mean subscale scores for parents who answered “yes” or “no” to whether a sleep behavior was really a problem, using the t test. Children whose parents stated that a sleep behavior on the CSHQ was a problem were identified as problem sleepers and those whose parents did not identify sleep behaviors as problems were termed nonproblem sleepers. The Holm step-down procedure was used to adjust for multiple comparisons to control the overall type I error rate. All statistical analyses were conducted with SPSS version 19.0.
Results
Participant Characteristics
A total of 180 parents of 5- to 6-year-old children in 4 practice sites completed a brief screening interview: 20 were ineligible, leaving a final study sample of 160 (89%) who completed the CSHQ. Of the 20 who were ineligible, 7 (4%) had a diagnosis of ADHD, 4 (2%) had developmental delay, 3 (1.6%) did not live with the parent, 3 (1.6%) lived outside the catchment communities for the study, 1 (0.6%) of the respondents was not the parent or legal guardian, and 1 (0.6%) of the children was not enrolled in school a minimum of 5 hours a day. Of the 160 eligible participants, 96% of the respondents were the biological or adoptive mothers of the children, and their mean age was 31.2 years (standard deviation [SD] = 7; range = 22–61; Table 1). The racial/ethnic composition of the children was 90% Latino (predominantly Dominican American) and 10% African American. Race and ethnicity were based on parental identification of the child’s racial and ethnic groups (Table 1). Although none of the children had a clinically diagnosed sleep problem at the time of enrollment, 4 parents (2.5%) reported speaking with the child’s pediatrician about the child’s sleep in the previous 12 months.
Table 1.
Participant Characteristics (n = 160)
| n | Percentage | |
|---|---|---|
| Parent characteristics | ||
| Mother | 154 | 96 |
| Father | 5 | 3 |
| Grandmother | 1 | 1 |
| Age, mean (SD), range (years) | 31.2 (7), 22–61 | |
| Marital status | ||
| Single | 90 | 56 |
| Married | 56 | 35 |
| Separated, divorced, other | 14 | 9 |
| Highest level of education completed | ||
| Did not complete high school | 43 | 27 |
| High school graduate | 45 | 28 |
| Education beyond high school | 48 | 30 |
| College graduate | 24 | 15 |
| Employment status | ||
| Employed, full-time | 101 | 63 |
| Employed, part-time | 22 | 14 |
| Unemployed | 16 | 10 |
| Full-time student | 11 | 7 |
| Disabled | 2 | 1 |
| Other | 8 | 5 |
| Child characteristics | ||
| Latino | 144 | 90 |
| African American | 16 | 10 |
| Female | 93 | 58 |
| Insured by Medicaid | 130 | 81 |
Abbreviation: SD, standard deviation.
Prevalence of Sleep Problems Identified in the Minority Community Sample Using the CSHQ
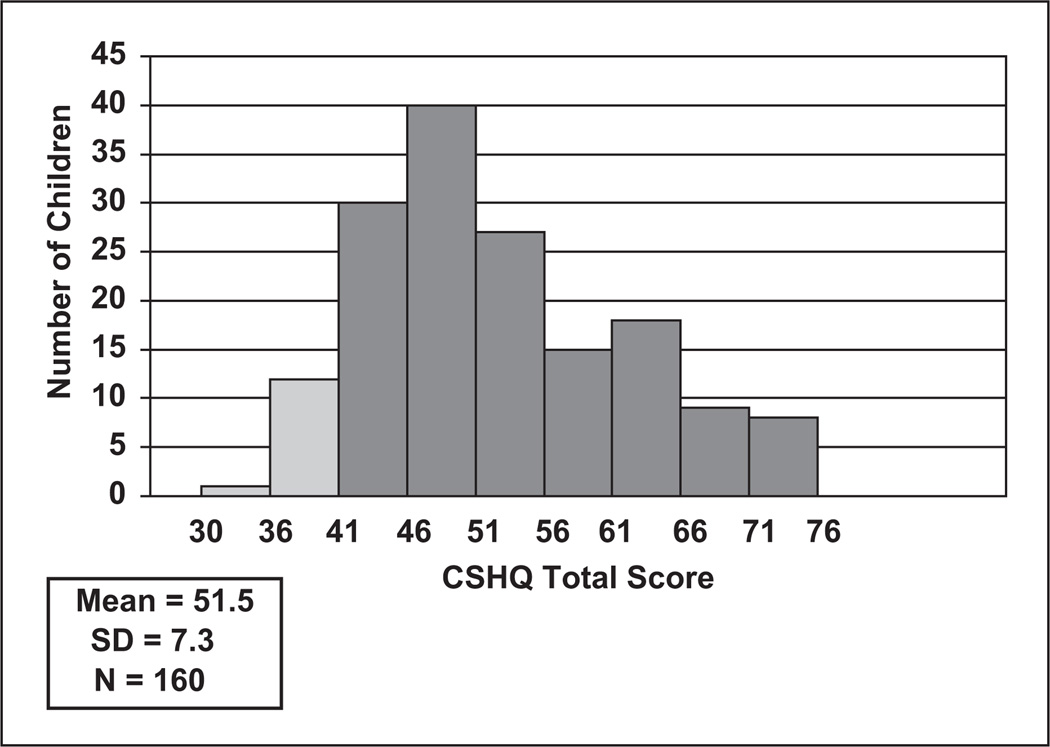
Of the 160 participants who completed the CSHQ, 150 (94%) scored ≥41, indicating the presence of a sleep problem. The mean total CSHQ score for all participants was 51.5 (SD = 7.3; range = 34–74) and was not significantly different from that of children who had a CSHQ score above the cutoff (mean = 52.4; SD = 6.6; range = 41–74). The distribution of CSHQ total scores is shown in Figure 1. There was no difference in mean total CSHQ scores between male and female participants in the sample.
Figure 1.
Distribution of CSHQ total scores for the minority community sample
Abbreviation: CSHQ, Children’s Sleep Habits Questionnaire.
Comparison of Prevalence of Sleep Problems in the Minority Community Sample With the Community Validation Sample, Using the CSHQ
We compared the prevalence of sleep problems from our sample with Owens’s community sample.6 Using a total CSHQ cutoff score of ≥41, 23% of children in Owens’s community sample of 5- to 6-year-olds were identified as having sleep problems, whereas 94% of our minority community sample had scores of 41 or greater. The difference in the prevalence of sleep problems was statistically significant (P < .001).
Comparison of Total and Subscale CSHQ Scores With Published Data
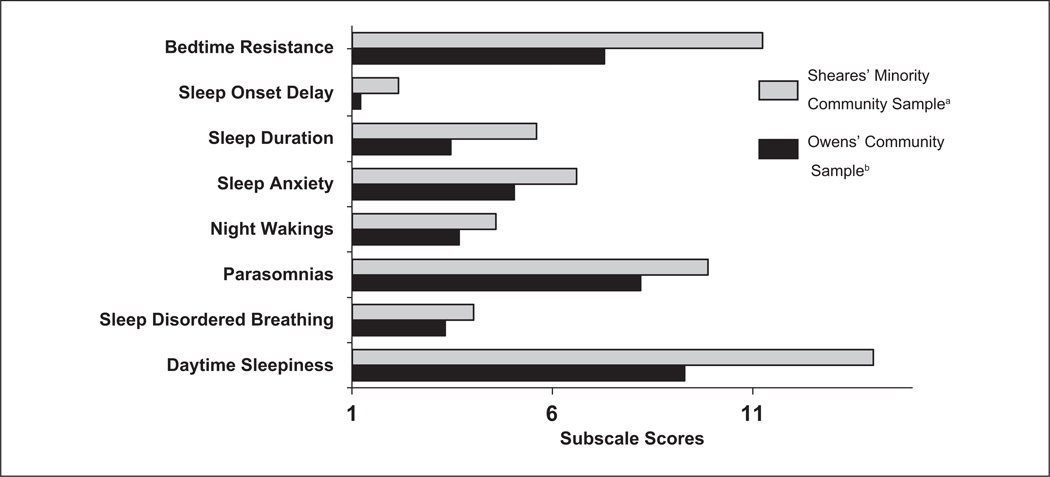
The mean total CSHQ score for our minority community sample (51.5, SD = 7.3) was significantly greater than that for the reference community sample (37.9, SD = 5.2; P < .001).8 Our findings also suggested that the sample of minority children showed significantly higher subscale scores than the reference community sample across all 8 subscales (Holm-adjusted P < .001 for all subscales; Figure 2).
Figure 2.
Comparison of CSHQ subscale scores between the minority community sample and reference community sample; Sheares’ minority community samplea had significantly higher scores than the reference community sampleb for all 8 subscales (Holm-adjusted P < .001 for all subscales)
Abbreviation: CSHQ, Children’s Sleep Habits Questionnaire.
Problem Sleepers Versus Nonproblem Sleepers
To further explore differences among our group of children with positive CSHQ (≥41) scores, we divided our sample based on whether or not parents identified a particular sleep behavior as a problem. Children identified as problem sleepers by their parents were found to have significantly higher mean subscale scores compared with nonproblem sleepers (Holm-adjusted P < .04 for all subscales; Table 2).
Table 2.
Comparisons of Mean CSHQ Subscale Scores Between Problem Sleepers and Nonproblem Sleepers for the Minority Community Sample
| Subscale | Problem Sleepers, n = 114, Mean (SD) |
Nonproblem Sleepers, n = 36, Mean (SD) |
Holm-Adjusted P Values |
|---|---|---|---|
| Bedtime resistance | 10.77 (2.99) | 8.95 (2.54) | .004 |
| Sleep onset delay | 1.76 (0.81) | 1.39 (0.68) | .026 |
| Sleep duration | 4.83 (2.04) | 3.37 (0.85) | <.001 |
| Sleep anxiety | 7.12 (2.17) | 5.42 (1.57) | <.001 |
| Night wakings | 4.59 (1.66) | 3.97 (1.31) | .038 |
| Parasomnias | 10.05 (2.44) | 8.21 (1.63) | <.001 |
| Sleep disordered breathing | 4.37 (1.71) | 3.37 (0.75) | <.001 |
| Daytime sleepiness | 14.93 (3.86) | 12.97 (3.39) | .018 |
Abbreviations: CSHQ, Children’s Sleep Habits Questionnaire; SD, standard deviation.
In all, 76% of parents reported at least 1 sleep behavior in their child as a problem. The prevalence of individual sleep problem subscales ranged from 11% to 51%. Our results indicated that among children described as problem sleepers, parents identified parasomnias (51%), bedtime resistance (51%), and sleep duration (51%) as the most common sleep problems. Sleep anxiety (49%) and daytime sleepiness (47%) were the next most commonly reported problems. Nearly one-third of parents (32%) reported problems in the night wakings subscale, whereas 27% identified problems in sleep onset delay. Sleep disordered breathing was the least common problem reported, with 11% of parents reporting it as a problem.
Discussion
The primary finding of our study is that among a minority community sample of 160 predominantly Latino 5- to 6-year-old children, 94% had parent-reported sleep problems identified by the CSHQ. Our results suggest that sleep problems are more prevalent in urban, minority, early-school-aged children compared with the reference group of 5- to 6-year-old children studied using the CSHQ.8 This finding is striking, and the prevalence exceeds published estimates that 20% to 43% of healthy children have sleep problems.4 Moreover, the prevalence of sleep problems in our minority community sample was higher than that reported in several clinical samples of children with known sleep problems.6,9,10 Among children with pervasive developmental disorders, including autism, the prevalence of sleep problems ranges from 40% to 80%9,10—less than that in our minority community sample.
Because the CSHQ has not been extensively used with urban minority populations, our findings highlight the need to better understand and delineate the family, sociocultural, biological, and economic dynamics that affect sleep. We believe that our finding of a high prevalence of sleep problems can be explained in part by the many risk factors for poor sleep that are exaggerated in low-income, urban environments.
There is an extensive literature documenting risk factors for poor sleep at both the community and family levels.11,12 It has been shown that minority children nap more frequently, take longer naps, and continue napping at much older ages compared with their Caucasian counterparts.1 Children 2 to 8 years of age from minority populations have significantly later bedtimes (P ≤ .001) and either similar or earlier wake times, resulting in shorter nocturnal sleep durations compared with their nonminority peers.13–15 Shorter sleep duration among African American children was confirmed by actigraphy in a cross-sectional study of 7- to 11-year-olds (P < .01).16 African American children (8–11 years old) had 4.8 times the odds of going to bed after 11 PM.15 Studies show that children who sleep less at night, despite taking naps, have significantly more externalizing daytime behavior problems (aggressive, acting out) even if they are getting the same amount of sleep as their nonnapping peers in a 24-hour period.15 Insufficient and disrupted sleep in school-aged children has also been correlated with learning and behavioral problems that may last through childhood.5 These factors may have contributed to the sleep behaviors and disorders that parents in our study reported.
Studies also consistently show that minority children are more likely to sleep in overcrowded, noisy spaces that are difficult to modify.17,18 Parental work schedules, inability to control one’s sleep environment, and shared sleeping space may have contributed to our results. It is important to note that although overcrowded sleeping environments can adversely affect children’s sleep, cosleeping is a common behavior among minority families and may not be as disruptive as other risk factors.19,20 Investigators have found that African American children are significantly more likely than Latino or Caucasian children to sleep in a room with a sibling, and Latino children are significantly more likely than African American or Caucasian children to sleep in a room with parents.20 These behaviors may occur even when there is adequate sleeping space.21 We found elevated mean bedtime resistance subscale scores which include questions regarding bed sharing. Our mean scores were higher than those of the validated community sample and may reflect the culture of cosleeping in our population.
In addition to poor sleep environments, minority children living in low-income, urban communities are at risk for increased behavioral sleep problems, sleep disturbances, and decreased sleep duration as a result of poorly controlled asthma,22 exposure to environmental tobacco smoke,22 community violence,17,23 and maternal depression, with concomitant insecure emotional maternal attachment.24 Further study is needed to determine the extent to which these problems contribute to the sleep behaviors reported. Despite all these factors, it has been demonstrated that among African American children living in less advantageous physical home environments, consistent bedtime vigilance by parents, compared with parents who were more permissive, resulted in significantly fewer sleep problems and improved sleep duration.18
We have shown that among our sample of children with sleep problems, there is variability in the types of sleep problems they exhibit and that are recognized by parents. We demonstrated that almost every child in our sample has some type of sleep problem, and more than 70% of parents reported that their child’s sleep behavior was a problem either for them or their child. However, despite this finding, only 4 parents reported speaking with their pediatrician in the previous 12 months about their child’s sleep. Studies suggest that parents are more likely to discuss their concerns regarding their child’s sleep when children are younger25 because infancy and toddlerhood are periods of time when clinicians routinely inquire about children’s sleep and when parents are most aware of the child’s sleep patterns. However, as children get older, studies show that clinicians are less likely to ask about sleep, and parents are less likely to raise sleep issues with the clinician.26 Parents may not view problem sleep as a medical issue; therefore, they do not discuss the subject with their pediatrician or other health professionals. Our results suggest that there may be a large population of children with significant sleep problems who have not been brought to the attention of their health care providers and, as a result, are not receiving the care needed to improve sleep.
This is particularly disturbing because studies show that sleep problems and sleep disorders can adversely affect behavior, cognitive performance, school functioning, and academic achievement and that minority children may be particularly vulnerable to the adverse effects of poor sleep.16 We chose to focus on Latino and African American 5- to 6-year-old children because this group has received little attention in sleep research to date. Additionally, because this age group is starting school, their sleep may be shortened by earlier wake times (school starting time), and there may be less time for naps. Parents in our study reported more daytime sleepiness compared with the validated community and clinical samples, which could be related to both these factors.
It is notable that although sleep disordered breathing was the least prevalent sleep problem in our group, 11% had behaviors suggestive of this sleep disorder. This finding needs to be confirmed because studies have demonstrated that minority status is a risk factor for sleep disordered breathing, and sleep disordered breathing is associated with poorer neurocognitive performance on a broad range of tests,27 behavioral problems,28 and increased risk for cardiovascular disease and metabolic syndrome.29
There are several limitations that should be noted when interpreting the results of this study. Because parents were recruited in clinical sites while they were waiting to receive care for themselves or others, they may not be representative of the community at large. Second, this was a relatively homogeneous sample of participants living within a relatively small catchment area, with a predominantly Dominican sample. This may limit our ability to generalize our conclusions to Latino and African American children in this age group as a whole. However, we believe that a strength of the study is its homogeneity. Our study is one of very few studies of sleep behaviors that include predominantly Latino children. Additionally, we were able to show that even in communities of concentrated social disadvantage and very high prevalence of sleep problems in children, there are considerable differences among families with regard to the types of problems they report. An additional limitation is that the validated instrument, the CSHQ, is based on parental reports of sleep problems that are not independently validated. Regardless of this limitation, we believe that our findings are important and support the need for further study of this high-risk population of children.
Finally, the high scores on the CSHQ need further study. Because the questionnaire has not been widely used in minority populations, a CSHQ total score cutoff of 41 may be too conservative for this group of children. Additionally, there may be different factors that affect children’s sleep today compared with a decade ago when the original validation studies were completed. Despite this, we demonstrated that the CSHQ was sensitive enough to discriminate between different behavioral sleep problems in this risk group. Future research should focus on the home and community environments that may contribute to poor sleep resulting in the high proportion of parents reporting sleep problems in their children. Moreover, objective measures of sleep may be useful in confirming the extent of sleep problems in this group of children. Given the consequences of poor sleep on health, behavior, and neurocognitive development,4,5,30 interventions should be developed specifically to address the sleep needs of children living in poor urban environments.
Conclusion
This is one of a few studies, to our knowledge, to examine sleep behaviors of a group of Latino and African American early-school-aged children using the CSHQ as a screening tool. The results of this study suggest that sleep problems are more common in urban, early-school-aged minority children than previously recognized. These sleep problems are underreported by parents, and as a result, health care providers may be unaware of the frequency with which these sleep problems occur. Our study identifies a group of children who may be at particularly high risk. Given the consequences of poor sleep, an important next step will be to develop effective interventions specifically to address the sleep needs of children living in poor urban environments.
Acknowledgments
We thank Judith Owens, MD, MPH, and Christopher Gables for generously providing us access to the original CSHQ data set. We also thank Robert Mellins, MD, for providing a critical review of this manuscript and Sara Lopez-Pintado, PhD, for providing early statistical support to the study.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Heart, Lung, and Blood Institute (Grant Number R01HL092856). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. The study sponsor had no role in (1) the design of the study; (2) data collection, analysis, or interpretation; (3) the production of this manuscript; or (4) the decision to submit the manuscript for publication. Beverley J. Sheares, MD, MS, is the principal investigator of the aforementioned grant and wrote the first draft of the manuscript.
Footnotes
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115(1, suppl):225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children’s Sleep Habits Questionnaire in toddlers and preschool children. J Dev Behav Pediatr. 2008;29:82–88. doi: 10.1097/dbp.0b013e318163c39a. [DOI] [PubMed] [Google Scholar]
- 3.Daniel LC, Grant M, Kothare SV, Dampier C, Barakat LP. Sleep patterns in an urban-dwelling minority pediatric population. Vulnerable Child Youth Stud. 2010;5:322–329. [Google Scholar]
- 4.Fricke-Oerkermann L, Pluck J, Schredl M, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007;30:1371–1377. doi: 10.1093/sleep/30.10.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:E60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 6.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–1051. [PubMed] [Google Scholar]
- 7.Daniel LC, Grant M, Kothare SV, Dampier C, Barakat LP. Sleep patterns in pediatric sickle cell disease. Pediatr Blood Cancer. 2010;55:501–507. doi: 10.1002/pbc.22564. [DOI] [PubMed] [Google Scholar]
- 8.Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Honomichl RD, Goodlin-Jones BL, Burnham M, Gaylor E, Anders TF. Sleep patterns of children with pervasive developmental disorders. J Autism Dev Disord. 2002;32:553–561. doi: 10.1023/a:1021254914276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malow BA, Crowe C, Henderson L, et al. A sleep habits questionnaire for children with autism spectrum disorders. J Child Neurol. 2009;24:19–24. doi: 10.1177/0883073808321044. [DOI] [PubMed] [Google Scholar]
- 11.El-Sheikh M, Buckhalt JA, Keller PS, Cummings EM, Acebo C. Child emotional insecurity and academic achievement: the role of sleep disruptions. J Fam Psychol. 2007;21:29–38. doi: 10.1037/0893-3200.21.1.29. [DOI] [PubMed] [Google Scholar]
- 12.Yoo JP, Slack KS, Holl JL. Material hardship and the physical health of school-aged children in low-income households. Am J Public Health. 2009;99:829–836. doi: 10.2105/AJPH.2007.119776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lavigne JV, Arend R, Rosenbaum D, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr. 1999;20:164–169. doi: 10.1097/00004703-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 14.McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O’Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6:319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Spilsbury JC, Storfer-Isser A, Drotar D, et al. Sleep behavior in an urban US sample of school-aged children [see comment] Arch Pediatr Adolesc Med. 2004;158:988–994. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- 16.Buckhalt JA, El-Sheikh M, Keller P. Children’s sleep and cognitive functioning: race and socioeconomic status as moderators of effects. Child Dev. 2007;78:213–231. doi: 10.1111/j.1467-8624.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- 17.Groves BM, Zuckerman B, Marans S, Cohen DJ. Silent victims: children who witness violence. JAMA. 1993;269:262–264. [PubMed] [Google Scholar]
- 18.Spilsbury JC, Storfer-Isser A, Kirchner HL, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea.[see comment] J Pediatr. 2006;149:342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 19.Lozoff B, Askew GL, Wolf AW. Cosleeping and early childhood sleep problems: effects of ethnicity and socioeconomic status. J Dev Behav Pediatr. 1996;17:9–15. doi: 10.1097/00004703-199602000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Milan S, Snow S, Belay S. The context of preschool children’s sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21:20–28. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- 21.Lozoff B, Wolf AW, Davis NS. Cosleeping in urban families with young children in the United States. Pediatrics. 1984;74:171–182. [PubMed] [Google Scholar]
- 22.Fagnano M, Bayer AL, Isensee CA, Hernandez T, Halterman JS. Nocturnal asthma symptoms and poor sleep quality among urban school children with asthma. Acad Pediatr. 2011;11:493–499. doi: 10.1016/j.acap.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadeh A. Stress, trauma, and sleep in children. Child Adolesc Psychiatr Clin N Am. 1996;5:685–700. [Google Scholar]
- 24.Benoit D, Zeanah CH, Boucher C, Minde KK. Sleep disorders in early childhood: association with insecure maternal attachment. J Am Acad Child Adolesc Psychiatry. 1992;31:86–93. doi: 10.1097/00004583-199201000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep. 2005;28:1568–1577. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- 26.Blunden S, Lushington K, Lorenzen B, Ooi T, Fung F, Kennedy D. Are sleep problems under-recognised in general practice? Arch Dis Child. 2004;89:708–712. doi: 10.1136/adc.2003.027011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gottlieb DJ, Chase C, Vezina RM, et al. Sleep-disordered breathing symptoms are associated with poorer cognitive function in 5-year-old children.[see comment] J Pediatr. 2004;145:458–464. doi: 10.1016/j.jpeds.2004.05.039. [DOI] [PubMed] [Google Scholar]
- 28.Chervin RD, Ruzicka DL, Giordani BJ, et al. Sleep-disordered breathing, behavior, and cognition in children before and after adenotonsillectomy. Pediatrics. 2006;117:e769–e778. doi: 10.1542/peds.2005-1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gozal D, Capdevila OS, Kheirandish-Gozal L. Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am J Respir Crit Care Med. 2008;177:1142–1149. doi: 10.1164/rccm.200711-1670OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fagnano M, van Wijngaarden E, Connolly HV, Carno MA, Forbes-Jones E, Halterman JS. Sleep-disordered breathing and behaviors of inner-city children with asthma. Pediatrics. 2009;124:218–225. doi: 10.1542/peds.2008-2525. [DOI] [PMC free article] [PubMed] [Google Scholar]