Abstract
Objective
To develop a new geometrical index that combines height, waist circumference (WC), and hip circumference (HC) and relate this index to total and visceral body fat.
Design and Methods
Subject data were pooled from three databases that contained demographic, anthropometric, dual energy X-ray absorptiometry (DXA) measured fat mass, and magnetic resonance imaging measured visceral adipose tissue (VAT) volume. Two elliptical models of the human body were developed. Body roundness was calculated from the model using a well-established constant arising from the theory. Regression models based on eccentricity and other variables were used to predict % body fat and % VAT.
Results
A body roundness index (BRI) was derived to quantify the individual body shape in a height-independent manner. Body roundness slightly improved predictions of % body fat and % VAT compared to the traditional metrics of body mass index (BMI), WC, or HC. On this basis, healthy body roundness ranges were established. An automated graphical program simulating study results was placed at http://www.pbrc.edu/bodyroundness.
Conclusions
Body roundness index, a new shape measure, is a predictor of % body fat and % VAT and can be applied as a visual tool for health status evaluations.
INTRODUCTION
Due to its simplicity and established relationship with mortality (1, 2) and obesity related comorbidities (3, 4), the body mass index (BMI) has been a long-standing accepted proxy for adiposity. The underlying theory behind BMI relies on encapsulating adiposity (5) in a height independent manner with one numerical value.
Despite the ease of application, BMI has often been criticized for misclassifying individuals at risk for obesity related comorbidities. One reason why BMI can misclassify individuals is that it fails to distinguish between individual amounts of fat-free mass (FFM) and (FM). For example, two individuals could have the same height, weight, and BMI even though one individual is more muscular than the other. Since FFM is denser than FM, the individual with higher amounts of FM in this example has a larger body volume and thus a larger waist size. Also, greater adiposity is associated with more central than peripheral fat distribution. Therefore, one way to improve on BMI is to develop an index that quantifies body girth in relation to height.
Another critique of BMI is that it does not provide information about body fat distribution. A relatively large quantity of abdominal body fat was first identified as a predictor of obesity related comorbidities by Vague (6) in 1956. With the application of imaging technologies including computed tomography and magnetic resonance imaging (MRI) for the quantification of tissues in-vivo, it is now well-established that a higher deposition of visceral adipose tissue (VAT) within the abdominal cavity is related to higher risks of obesity related comorbidities (7–10). Hence, several new indices have been developed that use some aspect of waist size or body shape (11, 12) in an attempt to improve on one or both of these limitations of BMI. Measures such as waist circumference (WC) and hip circumference (HC) and their related ratios have been identified as potentially better measures of body shape and adiposity-related risks (13, 14), but the drawback of using WC or HC is that neither corrects for the fact that taller individuals have larger waist or hip circumferences. Advancing this idea, body indices have recently been developed that combine several of the traditional body measurements such as height, WC, HC, and/or weight by fitting a conjectured formula to anthropometric data (12, 15). The comparison of these indices to BMI as predictors of VAT and overall health risk is ongoing within the nutrition research community (16, 17).
This study brings together two major concepts in obesity phenotypes and risk assessment that have not been adequately addressed by BMI: predicting both total % body fat and % VAT using anthropometric body measurements. To do so, we modeled the human body shape as an ellipse or an oval, which captures body girth in relation to height (body roundness). First introduced in 1609 by the German astronomer Johannes Kepler to quantify the circularity of planetary orbits, the degree of roundness of an ellipse is characterized by a non-dimensional value referred to as eccentricity (18). We apply eccentricity to develop a simple numerical quantifier of body roundness; the body roundness index (BRI). We also applied eccentricity to predict % total body fat and % VAT. While the notion of body roundness improves quantification of body shape and provides a more accurate estimate of total % body fat and % VAT, the calculation of BRI sacrifices simplicity in comparison to BMI. To preserve simplicity and enhance clinical utility, we programmed the calculations presented here as a simple user interface based calculator on the following web site: http://www.pbrc.edu/bodyroundness.
METHODS AND PROCEDURES
Elliptical Models
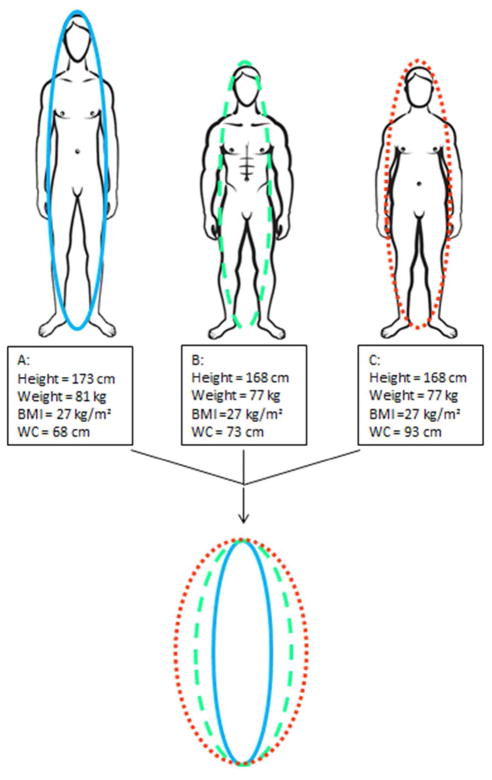
An ellipse is defined by two lengths referred to as the major axis and the minor axis. The major and minor axes can be thought of as the height and width of the ellipse, respectively. A person’s height determines the major axis. We assume that the minor axis can be represented as the girth around the waist or hip region, and so we calculate the diameter from WC and HC using the formula ½WC/π or ½HC/π, respectively. A simplification here is that the cross-section at the waist or the hip is taken to be circular. To use both WC and HC measurements, two separate models were developed; a waist-based ellipse and a hip-based ellipse (Figure 1). A more self-contained descriptive formula based explanation is provided in the Supplementary Information.
Figure 1.
Schematic diagram of the body outlining how body circumference can be equated to an ellipse. Panel A depicts an ellipse generated from height (H) in cm and WC (cm). Waist circumference represents the distance around an ellipse at waist level. The diameter of this ellipse (dw) is equal to waist circumference divided by 3.14. Similarly, Panel B depicts an ellipse arising from HC (cm).
Body Roundness Index
Eccentricity quantifies the degree of circularity of an ellipse, and its values range between 0 to 1, with 0 characterizing a perfect circle, and 1, a vertical line. Because of the challenge in distinguishing differences between values that are so small in magnitude, we mapped eccentricity to a range of 1 to 20 through the transformation:
This formula was derived solely to scale eccentricity values to a more accessible range of values. We note that the body roundness index (BRI) was never achieved a negative value across the NHANES database (lowest observed BRI was 1). Larger values of BRI are associated with rounder individuals and values closer to 1 are related to more narrowly shaped lean individuals. The maximum observed BRI value was 16.
Subjects
Three separate databases were used to develop prediction formulas. The third National Health and Nutrition Examination Survey (NHANES III) contained anthropometric measures including age, height, race, weight, sex, WC, and % body fat measured by dual energy X-ray absorptiometry (DXA). This database was used to develop models that predict total % body fat.
The second database consisted of data pooled from several studies conducted at St. Luke’s/Roosevelt Hospital New York Nutrition Obesity Research Center (NORC). The database is comprised of MRI measured VAT, age, height, race, sex, WC, and HC. This database was used to derive prediction models of %VAT (VAT mass/total body mass) that included both waist and hip-based body roundness as independent variables. For comparison to traditional metrics, the database was also used to derive formulas that tested the effectiveness of BMI, WC, and HC as predictor variables.
The third database consisted of MRI measured VAT in subjects pooled from several studies conducted at the Christian Albrecht’s University in Kiel, Germany. This database was used to determine the consistency of % VAT prediction models across studies and to validate the derived regression models used within the web based calculator.
NHANES
The NHANES III database included 3281 males and 3158 non-pregnant non-lactating females over the age of 18 years. Race groups were defined in NHANES III as non-Hispanic whites, non-Hispanic African Americans, Mexican Americans, and “other” (Aleut, Eskimo, American Indian, Asian, or Pacific Islander). Waist circumference was measured using the NHANES designated method as WC above the iliac crest (19). The database also included age, height, sex, and body composition measured by DXA. The NHANES III study did not report HC (20). The NHANES III study protocol had institutional review board approval and included written informed consent.
Kiel
The MRI methods have been previously described (19). Total adipose tissue and VAT volume were assessed by Magnetom Avanto 1.5-T scanner (Siemens Medical Systems) over the course of several different studies performed at Christian Albrecht’s University in Kiel, Germany since 2000. Briefly, the entire abdomen from the diaphragm (top of the liver or the base of the lungs, T10) to the femur heads was scanned using continuous axial images with an 8-mm slice thickness and 2-mm interslice gaps. Images were obtained using a T1 weighted gradient-echo sequence (TR 157 ms, TE 4 ms, flip angle 70°, voxel size 3.9 × 2 × 8 mm3), during which participants were required to hold their breath. All images were segmented manually using Slice-O-Matic, Tomovision 4.3 Software. In addition to MRI assessed VAT measurements, the Kiel database contained subject age, height, sex, WC, HC, and weight. Waist circumference was determined using the World Health Organization (WHO) designated method between the lower rib and above the iliac crest (19). The Institutional Review Board at Christian-Albrecht’s University approved the original studies, and subjects signed an informed consent form.
St. Luke’s-Roosevelt Hospital
The total volume of adipose tissue and VAT were measured using a 1.5 T MRI system and collected from a series of studies conducted at the New York Obesity Nutrition Research Center at St. Luke’s/Roosevelt Hospital as previously reported (21). All subjects were scanned with a T1-weighted, spin-echo sequence, with a 300 ms repetition time and an 11 ms echo time. A field of view 48 cm and a 256 × 256 matrix was used. The protocol involved acquisition of ~40 axial images of 10 mm thickness and at 40 mm intervals from fingers to toes with the subject in a supine position. The L4–L5 intervertebral disc was used as the point of origin. Following acquisition, subcutaneous adipose tissue and VAT were segmented by trained, quality-controlled technicians using image analysis software (SliceOmatic; Tomovision, Montreal, Quebec, Canada) at the Image Reading Center of the New York Nutrition Obesity Research Center. Subjects included healthy men and women over the age of 18 including White, Hispanic, Asian, and African American participants (Table 1). The database contained demographic information on race, height, sex, and weight along with % body fat measured by DXA. In addition, WC was measured on a horizontal plane around the abdomen at the top of the iliac crest (22) and HC was measured on all subjects around the widest portion of the buttocks (23). The pooled database includes athletes, normal active, overweight, and obese subjects. The original studies were reviewed and approved by the Institutional Review Board of St. Luke’s-Roosevelt Hospital.
Table 1.
Subject characteristics including age, BMI, WC, HC, % body fat (fat mass/body weight) and % VAT (VAT mass/body mass).
| Study | Age (yrs) | BMI (kg/m2) | Waist (cm) | Hip (cm) | % Fat | % VAT |
|---|---|---|---|---|---|---|
|
| ||||||
| NHANES† | ||||||
| M (N=3281) | 46± 20 | 27.41±5.36 | 97.46±15.06 | --------- | 27.37±6.76 | --------- |
| F (N=3158) | 48± 20 | 28.17±6.83 | 92.89±15.79 | --------- | 39.68±7.21 | |
|
| ||||||
| St. Luke’s | ||||||
| M (N=167) | 39±15 | 25.70±3.78 | 87.58±10.74 | 99.68±7.47 | 20.53±7.99 | 2.61±1.95 |
| F (N=203) | 45±17 | 25.82± 5.53 | 79.80±13.16 | 101.10±11.95 | 33.48±10.10 | 2.06±1.42 |
|
| ||||||
| Kiel†† | ||||||
| M (N=174) | 42±14 | 27.14±4.39 | 96.01±12.91 | 101.49±8.72 | 24.05±8.44 | 4.02±2.37 |
| F (N= 246) | 38±13 | 28.60±6.90 | 92.93±16.32 | 108.57±15.33 | 38.26±10.29 | 2.32±1.64 |
NHANES III: % body fat was measured by DXA.
Calculations and Statistical Methods
VAT volumes were converted to VAT mass by multiplying by the density constant 1.09 kg/L (24).
Calculation of healthy ranges of body roundness
Healthy body roundness ranges were determined by regressing a formula through the NHANES database to predict roundness as a function of age, sex, height, and % body fat. We substituted the lower bound and upper bound for published healthy body fat ranges (25) into the formula for the %body fat variable to determine an upper and lower bound for a range of healthy roundness. The %body fat ranges were based on a range of age and height and were gender specific. Thus the generated healthy roundness ranges are also dependent on age and height. We point out that the %body fat ranges were originally determined using BMI cutoffs. The healthy ranges of roundness were included as a shaded zone in the web-based calculator as a reference for individual user roundness output.
Calculation of ellipses normalized by height
In order to visually compare individual roundness to a healthy roundness range, we normalized each individual’s ellipse by constructing an ellipse of equal eccentricity but with the same length for the major axis. This is equivalent to considering an individual’s body girth after adjusting for height, allowing comparison of body roundness at the population level while correcting for differences in height.
Comparison of total percent body fat and total visceral adipose tissue volume predictors
A series of regression models that relate a single covariate to % body fat or % VAT were developed to determine how much variance is explained by each of the variables; waist eccentricity, hip eccentricity, combined waist and hip eccentricity, WC, HC, combined waist and hip circumferences, and BMI. The analysis tested for significance of each covariate and their powers (for example BMI, BMI2, BMI3, …) to capture potential nonlinear relationships.
The NHANES III database was utilized to determine the relationships between waist eccentricity, waist circumference, and BMI measurements with % body fat. Because the NHANES database did not contain hip related measurements, other models were developed using the St. Luke’s and Kiel database. Due to potential differences in MRI assessments of VAT collected at different sites, along with the difficulty in comparing waist-related predictions using the NHANES versus WHO designated WC measurements (19), the St. Luke’s and Kiel databases were not pooled in this analysis.
Prediction models of total percent fat and total percent VAT
There were two objectives for developing prediction models: comparing the models without any covariates; and comparing the models with inclusion of covariates. This analysis is similar to the comparison of body adiposity index (BAI) with BMI and WC (17). Finally all significant covariates (age, height, sex, weight, and race) along with interaction terms and nonlinearities were included with both waist eccentricity and hip eccentricity for application in the web-based calculator.
We applied waist and hip eccentricity as opposed to BRI in these formulas since the purpose of the BRI is to generate a visibly simple numerical value that has a wider range than eccentricity values. To develop the statistical models, we revert back to the original directly computed eccentricity.
The % body fat and % VAT prediction models that rely on waist eccentricity and hip eccentricity were derived from the NHANES and St. Luke’s datasets and validated against the Kiel dataset.
RESULTS
Comparison Models
Regression models were developed to test for accuracy of predictive models comparing combined waist eccentricity, hip eccentricity, WC, HC, BMI, and body weight to predict % body fat and % VAT. Most of the developed models contained significant nonlinear terms of quadratic or cubic powers. The resulting adjusted R2 values are listed in Table 2. With no additional covariates, the combination of waist eccentricity and hip eccentricity outperformed predictions of % body fat for men and women that relied solely on BMI, WC combined with HC, WC, and HC. We note that this improvement over WC and HC is only slightly better. However, taken together, the best single predictor of both % body fat and % VAT is the combined waist and hip eccentricity. With the inclusion of covariates as age and height, eccentricity based models of % VAT were comparable to the existing best predictors. These predictors varied by sex but most often the best traditional predictor of % VAT was WC.
Table 2.
Adjusted R2 for various models comparing combined waist eccentricity, hip eccentricity, WC, HC, BMI, and body weight to predict % body fat mass and %VAT. A. Results including NHANES III and St. Luke’s for % body fat. B. Results including St. Luke’s and Kiel for % VAT.
| A. | ||||||
|---|---|---|---|---|---|---|
| %BF (Fat Mass/Body Mass) NHANES | ||||||
| Eccentricities | Circumferences | |||||
| Model co-variates | Waist | Waist | BMI (kg/m2) | |||
| M | F | M | F | M | F | |
| None | 0.78 | 0.65 | 0.74 | 0.63 | 0.60 | 0.67 |
| Age | 0.78 | 0.66 | 0.75 | 0.64 | 0.68 | 0.71 |
| Age Height | 0.78 | 0.66 | 0.78 | 0.66 | 0.68 | 0.71 |
| %BF (Fat Mass/Body Mass) St. Luke’s | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eccentricities | Circumferences (cm) | |||||||||||||
| Model co-variates | Waist & Hip | Waist | Hip | Waist & Hip | Waist | Hip | BMI (kg/m2) | |||||||
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| None | 0.65 | 0.80 | 0.63 | 0.71 | 0.58 | 0.77 | 0.65 | 0.73 | 0.63 | 0.73 | 0.54 | 0.72 | 0.48 | 0.78 |
| Age | 0.66 | 0.80 | 0.63 | 0.71 | 0.61 | 0.77 | 0.64 | 0.73 | 0.63 | 0.73 | 0.57 | 0.74 | 0.53 | 0.78 |
| Age Height | 0.67 | 0.82 | 0.65 | 0.73 | 0.63 | 0.78 | 0.68 | 0.73 | 0.68 | 0.73 | 0.63 | 0.78 | 0.53 | 0.78 |
| B. | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| %VAT (VAT mass/Body Mass) St. Luke’s | ||||||||||||||
| Eccentricities | Circumferences (cm) | |||||||||||||
| Model co-variates | Waist & Hip | Waist | Hip | Waist & Hip | Waist | Hip | BMI (kg/m2) | |||||||
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| None | 0.64 | 0.46 | 0.56 | 0.44 | 0.26 | 0.25 | 0.61 | 0.43 | 0.51 | 0.40 | 0.19 | 0.17 | 0.34 | 0.31 |
| Age | 0.67 | 0.55 | 0.63 | 0.54 | 0.48 | 0.43 | 0.64 | 0.54 | 0.58 | 0.53 | 0.42 | 0.41 | 0.47 | 0.47 |
| Age Height | 0.67 | 0.55 | 0.63 | 0.54 | 0.48 | 0.43 | 0.66 | 0.54 | 0.61 | 0.54 | 0.48 | 0.43 | 0.48 | 0.47 |
| %VAT (kg) (VAT mass/Body Mass) Kiel | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eccentricities | Circumferences (cm) | |||||||||||||
| Model co-variates | Waist & Hip | Waist | Hip | Waist & Hip | Waist | Hip | BMI (kg/m2) | |||||||
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| None | 0.42 | 0.30 | 0.38 | 0.23 | 0.23 | 0.14 | 0.37 | 0.29 | 0.31 | 022 | 0.22 | 0.11 | 0.24 | 0.14 |
| Age | 0.49 | 0.39 | 0.48 | 0.36 | 0.42 | 0.29 | 0.49 | 0.39 | 0.47 | 0.36 | 0.40 | 0.29 | 0.43 | 0.32 |
| Age Height | 0.49 | 0.39 | 0.48 | 0.36 | 0.42 | 0.29 | 0.49 | 0.39 | 0.47 | 0.36 | 0.41 | 0.29 | 0.43 | 0.32 |
Prediction Models
Prediction formulas were developed to generate personalized output in the web-based calculator. Three specific models were developed. The first applied the NHANES III database and waist eccentricity to predict % body fat while considering all covariates; age, height, sex, race, and weight. Significant interaction terms and powers of the covariates were also included. The second model applied the St. Luke’s database to predict total %VAT from combined waist and hip eccentricity. Similar to the first model, this model included all covariates, their significant interaction terms, and significant powers. The third model applied the St. Luke’s database to develop a model that did not rely on hip eccentricity to provide predictions of %VAT for users who did not have HC.
The adjusted R2 for the NHANES derived % body fat model was 0.88. The races, Mexican-American, White, and African American had significant coefficients, and the overall model contained up to cubic nonlinearities.
The adjusted R2 for the St. Luke’s derived %VAT model that included both hip and waist eccentricity was 0.71. Both African American and Asian races were determined significant with African Americans having less and Asians having more % VAT in comparison than Whites of equal BMI. These results are consistent with previous observations (27–29). The final model which predicted % VAT from solely waist eccentricity resulted in an R2 of 0.69. Similar race effects were found as in the model which included both waist and hip eccentricity.
Similar to the observations of Flegal et al (26), we observed consistently lower correlations between circumference related measurements and % body fat and %VAT in women across studies. A closer examination of the relationship between % VAT and VAT mass in women revealed higher variation in the larger amounts of VAT (Figure 5 in Supplemental Information). This variation was also reflected in the Bland Altman analysis of the % VAT model validation (Supplementary Information) which identified increasing bias with higher levels of % VAT.
The values for model coefficients for the three models and a validation across studies are included in the Supplementary Information.
Relationship of BRI to BMI
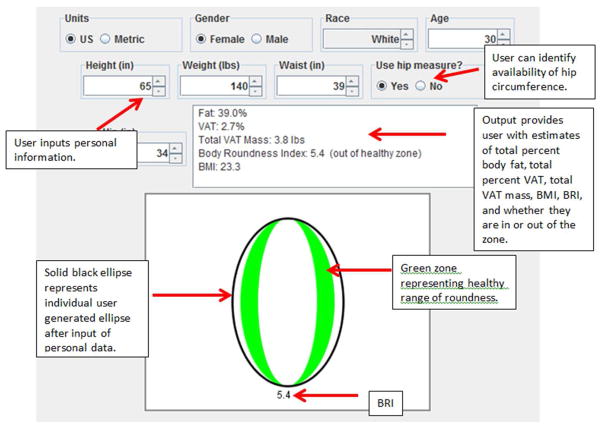
To test the relationship of BRI vs. BMI, BRI values were calculated in each range of BMI classification from the NHANES database. Mean roundness values increased with increasing BMI (Table 3). The average BRI decreased with BMI classification, as expected. However, while the endpoints of the ranges also decreased with BMI classifications, there was overlap in BRI value ranges, indicating that BRI classification differs from BMI. An example of how BRI differentiates between various body types of the same BMI is depicted in Figure 2.
Table 3.
Average and range of BRI in the BMI groupings of individuals classified as underweight, normal weight, overweight, obese, and extremely obese in the NHANES database.
| BMI Range | BRI range mean±SD |
%FM range mean±SD |
||
|---|---|---|---|---|
| M | F | M | F | |
| 40≤BMI | [6.80, 18.09] 10.00±2.00 |
[5.80, 14.84] 9.87±0.01 |
[30.7,46.5] 39.2±3.3 |
[41.0,58.1] 49.5±3.6 |
| 30≤BMI<40 | [3.15, 10.74] 6.47±1.18 |
[3.83 12.29] 6.86±0.01 |
[20.1,44] 33.3±4.1 |
[32.1,54.4] 45.1±3.6 |
| 25≤BMI<30 | [2.03, 7.33] 4.66±0.91 |
[2.34 11.53] 4.96±1.06 |
[13.4,41.3] 28.4±4.2 |
[25.3,53.3] 40.8±3.9 |
| 18.5≤BMI<25 | [1.23, 6.62] 3.07±0.88 |
[1.57 6.85] 3.28±0.88 |
[11.6,38.8] 22.4±5.2 |
[18.6,51.1] 34.7±5.0 |
| BMI<18.5 | [1.00, 3.36] 1.76±0.50 |
[1.27 4.05] 1.95±0.50 |
[10.1,27.9] 16.8±4.0 |
[16.6,36.0] 26.3±4.1 |
| Total | [1.00, 18.09] 4.64 ±1.88 |
[1.27 14.84] 5.16 ±2.24 |
[10.1,46.5] 27.6±6.5 |
[16.6,58.1] 40.1±6.7 |
Figure 2.
BMI as a measure of adiposity fails to distinguish individuals with similar BMI but different degrees of body fat. The three depicted individuals vary in body type but share identical BMI. A: subject is tall and lean, B: subject is muscular, C: subject has highest percent body fat. Although their BMIs are identical, their corresponding BRI values differentiate their body types. After normalizing for height, the three generated ellipses can be visually compared for differences in body roundness, which can be converted into estimates of percent body fat. Images used with permission from http://www.shutterstock.com.
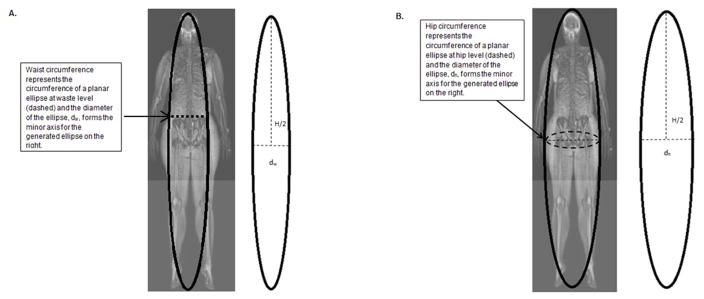
Web-based Calculator
The web-based calculator predicts % body fat, % VAT, and total VAT mass from age, height, sex, WC, HC, and race (Figure 3). The option to supply WC measurements in the absence of HC was programmed to allow for analysis in the absence of HC measurements. The web-based calculator provides an output for BRI and a graph of the individual user generated ellipse in relation to a healthy roundness zone (green).
Figure 3.
Screen shot of Body Roundness Calculator. After the user enters personal information for age, height, weight, sex, race, waist and hip circumferences, the program outputs total percent body fat, amount and percent of VAT, the body roundness index, and whether the individual is within the determined healthy range of body roundness. A graph depicting the resulting individual ellipse (African American curve) and healthy range (green shaded area) provide the user a visual representation of their body roundness relative to the healthy range.
DISCUSSION
Existing adiposity related indices attempt to identify external human body shape with body fat and body fat distribution through one numerical value. Here we derive the first purely geometrical model of body shape using the theory of ellipses. The derived elliptical model induces a 400-year old index which determines body roundness. We show here that our geometrically derived measure of body roundness consistently provides predictions of both % body fat and total % VAT comparable in accuracy to the best existing predictors of WC, HC, and BMI.
Our approach advances several attempts to combine circumference measurements with height to identify body shape by fitting a pre-designated formula to data (11, 12). These existing approaches require conjecture of formula type and a restriction to a few variables that may be important. Additionally, development of these indices requires determination of the height power values, which is an important continually investigated question. Our approach utilizes a well-established non-dimensional index that is solely derived from geometry. This geometrical derivation not only serves as a proxy for % body fat and % VAT, but also provides a method to visually compare individual body types and identify the body type location relative to a reference range of healthy body roundness (Figure 3).
There are several limitations of the current study. The first important limitation involves the size and inclusion of covariate measurements in existing databases. The higher adjusted R2 for combined HE and WE for prediction of total % FM in females in the St. Luke’s and Kiel database suggests that HC is a critical covariate for FM especially in females. Our results indicate the importance for HC to be included in future NHANES measurements. While the diversity of the St. Luke’s database with inclusion of different races and range of BMI allow one to examine the effect of different covariates on %VAT predictions, the small size of the database yield poorer predictions than the more homogeneous Kiel database. The combined St. Luke’s and Kiel studies currently represent one of the largest MRI measured total VAT mass databases. With increased use of MRI in obesity related body composition research, we expect to improve not only our understanding of the relationships between geometric properties of body shape and VAT but also the predictions of individual VAT from essential covariates.
As noted in the results, there is a wider range of variance for higher degrees of VAT (See Figure S5 in the Supplementary Information). Because this observation was consistent across study sites, technical reasons are unlikely to explain these phenomena. One possible reason for this difference may be due to higher variability in measurements of WC and HC in standing individuals with higher amounts of body fat. The observed differences may additionally reflect the variability in fat distribution in individuals with high VAT. For example, some subjects with high VAT have large amounts of subcutaneous adipose tissue while others have not. Since we do not have a good understanding of what factors predict fat distribution, further investigation is required (30). However, our analysis here suggests that we may have reached the limits of maximal accuracy of predictions of VAT and % body fat that rely solely on the circumference measurements (waist and hip), age, height, sex, race, and weight. Further individual measurements collected at additional circumference sites or leg height may be required to improve upon these predictions.
Finally, BMI is the most accessible adiposity index due to its simplicity and requirement for two easily obtained measurements, body weight and height. Other models that rely on geometry (31) or statistically generated nonlinear models (32) improve upon predictive accuracy but are not as simple to apply in clinical settings in comparison to BMI. While BRI improves upon predictions of VAT over BMI, predictions of total %FM yielded a higher adjusted R2 than the predictions of total %VAT which has been observed as more dangerous to individual health. Thus, it remains to be shown how the newly developed index, BRI, relates to mortality and other markers of health (such as cardiovascular and development of type 2 diabetes) and whether any improvement over BMI outweighs the complexity of the model.
With the advancement of technology and web-based programs, however, more complex models that improve accuracy and relay more on body and health related information can be developed and accessed through a web-based calculator as designed in this study.
In conclusion, current practice utilizes BMI to inform and develop target recommendations to improve patient health. The proposed model and developed tool advances these existing models by including circumference measurements through well-established geometrical methodology and delivering these measurements in a easily usable software platform that can better inform and guide treatment to improve obesity related health.
Supplementary Material
Acknowledgments
Diana M. Thomas is supported by NIH grants R15 DK090739, U01 DK094418. Courtney Peterson is supported by NIH grant T32 DK064584. Eric Ravussin is supported by a NORC Center Grant # 2P30DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by NIDDK
Footnotes
The supplementary information contains a detailed description of model development, the coefficients for the models used in the web-based calculator, a validation of the web-based calculator models across studies, and an analysis of variance in the higher levels of VAT.
DISCLOSURE STATEMENT
Diana M. Thomas is a consultant for Jenny Craig.
References
- 1.Cai L, Lubitz J, Flegal KM, Pamuk ER. The predicted effects of chronic obesity in middle age on medicare costs and mortality. Med Care. 2010;48(6):510–7. doi: 10.1097/MLR.0b013e3181dbdb20. [DOI] [PubMed] [Google Scholar]
- 2.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–93. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 3.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29(6):1263–8. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 4.Li Z, Bowerman S, Heber D. Health ramifications of the obesity epidemic. Surg Clin North Am. 2005;85(4):681–701. v. doi: 10.1016/j.suc.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Heymsfield SB, Martin-Nguyen A, Fong TM, Gallagher D, Pietrobelli A. Body circumferences: clinical implications emerging from a new geometric model. Nutr Metab (Lond) 2008;5:24. doi: 10.1186/1743-7075-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vague J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr. 1956;4(1):20–34. doi: 10.1093/ajcn/4.1.20. [DOI] [PubMed] [Google Scholar]
- 7.Brochu M, Poehlman ET, Ades PA. Obesity, body fat distribution, and coronary artery disease. J Cardiopulm Rehabil. 2000;20(2):96–108. doi: 10.1097/00008483-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Despres JP, Nadeau A, Tremblay A, Ferland M, Moorjani S, Lupien PJ, et al. Role of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese women. Diabetes. 1989;38(3):304–9. doi: 10.2337/diab.38.3.304. [DOI] [PubMed] [Google Scholar]
- 9.Kaess BM, Pedley A, Massaro JM, Murabito J, Hoffmann U, Fox CS. The ratio of visceral to subcutaneous fat, a metric of body fat distribution, is a unique correlate of cardiometabolic risk. Diabetologia. 2012 doi: 10.1007/s00125-012-2639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sironi AM, Petz R, De Marchi D, Buzzigoli E, Ciociaro D, Positano V, et al. Impact of increased visceral and cardiac fat on cardiometabolic risk and disease. Diabet Med. 2012;29(5):622–7. doi: 10.1111/j.1464-5491.2011.03503.x. [DOI] [PubMed] [Google Scholar]
- 11.Bergman RN. A better index of body adiposity. Obesity (Silver Spring) 2012;20(6):1135. doi: 10.1038/oby.2012.99. [DOI] [PubMed] [Google Scholar]
- 12.Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012;7(7):e39504. doi: 10.1371/journal.pone.0039504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gomez-Ambrosi J, Silva C, Galofre JC, Escalada J, Santos S, Millan D, et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes (Lond) 2012;36(2):286–94. doi: 10.1038/ijo.2011.100. [DOI] [PubMed] [Google Scholar]
- 14.Berkova M, Berka Z. Obesity, body mass index, waist circumference and mortality. Vnitr Lek. 2011;57(1):85–91. [PubMed] [Google Scholar]
- 15.Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity (Silver Spring) 2011;19(5):1083–9. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Snijder MB, Nicolaou M, van Valkengoed IG, Brewster LM, Stronks K. Newly Proposed Body Adiposity Index (BAI) by Bergman et al. Is Not Strongly Related to Cardiovascular Health Risk. Obesity (Silver Spring) 2012;20(6):1138–9. doi: 10.1038/oby.2011.338. [DOI] [PubMed] [Google Scholar]
- 17.Freedman DS, Thornton J, Pi-Sunyer FX, Heymsfield SB, Wang J, Pierson RN, Jr, et al. The body adiposity index (hip circumference/height(1.5)) is not a more accurate measure of adiposity than is BMI, waist circumference, or hip circumference. Obesity (Silver Spring) 2012 doi: 10.1038/oby.2012.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kepler J. Astronomia nova (Pragae) p. 1609. [Google Scholar]
- 19.Bosy-Westphal A, Booke CA, Blocker T, Kossel E, Goele K, Later W, et al. Measurement site for waist circumference affects its accuracy as an index of visceral and abdominal subcutaneous fat in a Caucasian population. J Nutr. 2010;140(5):954–61. doi: 10.3945/jn.109.118737. [DOI] [PubMed] [Google Scholar]
- 20.Sun Q, van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB. Comparison of dual-energy x-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am J Epidemiol. 2010;172(12):1442–54. doi: 10.1093/aje/kwq306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shen W, Chen J, Gantz M, Velasquez G, Punyanitya M, Heymsfield SB. A Single mri Slice Does Not Accurately Predict Visceral and Subcutaneous Adipose Tissue Changes During Weight Loss. Obesity (Silver Spring) 2012 doi: 10.1038/oby.2012.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Heart Lung and Blood Institute, North American Association for the Study of Obesity. The practical guide identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, Md: The Institute; 2000. Available from: http://purl.access.gpo.gov/GPO/LPS16589. [Google Scholar]
- 23.World Health Organization. Expert Report, Waist Circumference and Waist-to-Hip Ratio. WHO Document Production Services; 2008. [Google Scholar]
- 24.Gallagher D, Belmonte D, Deurenberg P, Wang Z, Krasnow N, Pi-Sunyer FX, et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol. 1998;275(2 Pt 1):E249–58. doi: 10.1152/ajpendo.1998.275.2.E249. [DOI] [PubMed] [Google Scholar]
- 25.Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72(3):694–701. doi: 10.1093/ajcn/72.3.694. [DOI] [PubMed] [Google Scholar]
- 26.Flegal KM, Shepherd JA, Looker AC, Graubard BI, Borrud LG, Ogden CL, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89(2):500–8. doi: 10.3945/ajcn.2008.26847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conway JM, Yanovski SZ, Avila NA, Hubbard VS. Visceral adipose tissue differences in black and white women. Am J Clin Nutr. 1995;61(4):765–71. doi: 10.1093/ajcn/61.4.765. [DOI] [PubMed] [Google Scholar]
- 28.Hoffman DJ, Wang Z, Gallagher D, Heymsfield SB. Comparison of visceral adipose tissue mass in adult African Americans and whites. Obes Res. 2005;13(1):66–74. doi: 10.1038/oby.2005.9. [DOI] [PubMed] [Google Scholar]
- 29.Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT) Am J Clin Nutr. 2007;86(2):353–9. doi: 10.1093/ajcn/86.2.353. [DOI] [PubMed] [Google Scholar]
- 30.Hayes L, Pearce MS, Firbank MJ, Walker M, Taylor R, Unwin NC. Do obese but metabolically normal women differ in intra-abdominal fat and physical activity levels from those with the expected metabolic abnormalities? A cross-sectional study. BMC Public Health. 2010;10:723. doi: 10.1186/1471-2458-10-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fontaine KR, Gadbury G, Heymsfield SB, Kral J, Albu JB, Allison D. Quantitative prediction of body diameter in severely obese individuals. Ergonomics. 2002;45(1):49–60. doi: 10.1080/00140130110112627. [DOI] [PubMed] [Google Scholar]
- 32.Lim U, Turner SD, Franke AA, Cooney RV, Wilkens LR, Ernst T, et al. Predicting total, abdominal, visceral and hepatic adiposity with circulating biomarkers in caucasian and Japanese american women. PLoS One. 2012;7(8):e43502. doi: 10.1371/journal.pone.0043502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.