Abstract
Purpose
To determine the prevalence and correlates of decisions made about life-sustaining treatments among residents in long-term care settings, including how often decisions were honored and characteristics associated with decisions not being followed.
Design and Methods
Retrospective interviews with one family caregiver and one facility staff member for each of 327 decedents who received end-of-life care in 27 nursing homes (NHs) and 85 residential care/assisted living (RC/AL) settings in four states were analyzed with respect to decedent demographics, facility characteristics, prevalence of decisions made about medical interventions, proportion of residents whose decisions were heeded, and characteristics associated with decisions not being heeded.
Results
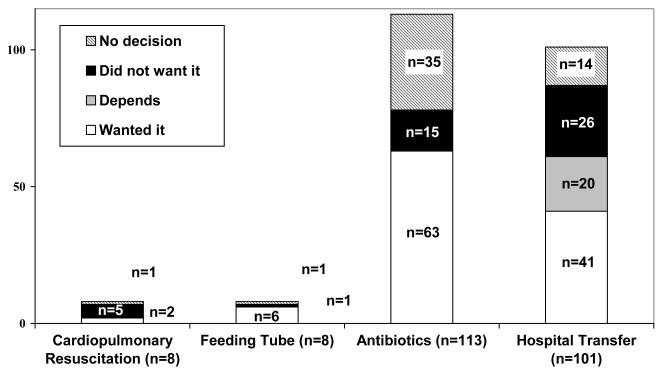
Most family caregivers reported making a decision with a physician about resuscitation (89.1%), inserting a feeding tube (82.1%), administering antibiotics (64.3%), and hospital transfer (83.7%). Reported care was inconsistent with decisions made in five of seven (71.4%) of resuscitations, one of seven feeding tube insertions (14.3%), 15 of 78 antibiotics courses (19.2%), and 26 of 87 hospital transfers (29.9%). Decedents who received antibiotics contrary to their wishes were older (mean age 92 versus 85, p= 0.014). More than half (53.8%) of decedents who had care discordant with their wishes about hospitalization lived in a NH compared to 32.8% of those whose decision were concordant (p=0.034).
Implications
Most respondents reported decision-making with a doctor about life-sustaining treatments, but those decisions were not consistently heeded. Being older and living in a NH were risk factors for decisions not being heeded.
Keywords: Advance directives, end-of-life care, nursing home, assisted living
INTRODUCTION
For dying long-term care (LTC) residents and their caregivers, making and then adhering to advance decisions about the use of life-sustaining treatments (LSTs) including cardiopulmonary resuscitation, insertion and use of a feeding tube, administration of antibiotics, or hospitalization can be ethically and medically complex. Such decisions are known to be affected by the perceived effectiveness of the treatment in question, its presumed effect on the patient’s quality of life, and the wishes, beliefs, and expectations of the patient and family (Gillick, 2000; National Institutes of Health Consensus Statement, Improving End-of-Life Care, 2004). However in LTC settings, where the individuals are not necessarily ill when decisions regarding LSTs are made, factors that influence decisions and subsequent care at end of life (EOL) may differ from those in other settings. Further, EOL care in LTC settings is influenced by residents, family members, and the setting itself to such an extent that one cannot effectively study EOL care without taking all of these characteristics into account.
For example, the demographics of nursing home (NH) residents are associated with whether LST decisions are made and followed. Residents who are older, female, white, and cognitively impaired, are more likely to have advance directives concerning LSTs than their younger, non-white, cognitively intact, male counterparts (Dobalian, 2004; Lamberg, Person, Kiely, & Mitchell, 2005; Levy, Fish, & Kramer, 2005; Messinger-Rapport & Kamel, 2005; Resnick, Schuur, Heineman, Stone, & Weissman, 2008). Further, older and female residents at the EOL are less likely to have their LST decisions honored than younger or male individuals in NH and hospital settings (Dobalian, 2004, Hamel et al, 1999). Also, NH residents with a Do Not Hospitalize (DNH) order who are more independently functional are more likely to be sent to the hospital during a crisis (despite having a DNH order) than those who are more dependent (Dobalian, 2004).
Family members play an important role in whether LST decisions are made or honored in LTC settings. In fact, doctors admit that when the patient no longer has decision-making capacity, family members’ wishes may have more influence on actual care provided than the patient’s wishes (Torke, Simmerling, Siegler, Kaya, & Alexander, 2008). Additionally, familiarity between family and physicians is important, as doctors are reticent to discuss LSTs in advance if they are not familiar with the family or are concerned that the family would perceive the discussion as inappropriate (Morrison, Morrison, & Glickman, 1994). Limited communication by physicians appears to be especially prevalent for patients who are not acutely ill, which would include most LTC residents (Culberson, Levy, & Lawhorne, 2005; Dobalian, 2004, 2006; Messinger-Rapport & Kamel, 2005; Teno, et al., 1997).
Facility factors also affect whether orders regarding LST are recognized or honored. In the 2004 National Nursing Home Survey, residents in nonprofit NHs were more likely to have orders regarding LSTs on their charts compared to those in larger facilities (>200 beds) (Resnick, et al., 2008). However, NH residents who had DNH orders on their charts were more likely to be hospitalized despite the DNH order if they were from nonprofit NHs or those that were not hospital-based.(Dobalian, 2004) Virtually all of the information regarding LST decisions and related care in LTC settings has been obtained in NHs; in contrast, very little is known about such decisions and care in residential care/assisted living (RC/AL) settings (i.e., those that provide room, board, assistance with activities of daily living and protective oversight) (Zimmerman et al., 2005). . Learning more about these issues in RC/AL is important because they house almost one million older adults and have become a frequent site of EOL care (Sloane, Zimmerman, Williams, & Hanson, 2008).
Since Americans are increasingly likely to spend their final days in a LTC facility, understanding and honoring advanced decisions about the use of LSTs in these settings becomes ever more important (Brock & Foley, 1998). The proportion of deaths occurring in NHs is expected to double over the next 20 years (Brock & Foley, 1998), and annual mortality rates for residents of RC/AL communities already range from 16% to 22% (Zimmerman et al, 2005). Despite these statistics, the prevalence of LST discussions in varied LTC settings, the concordance of treatment decisions with actual clinical outcomes, and the characteristics associated with discordant treatment decisions and outcomes is not well understood (Cartwright, 2002). To address these issues, we analyzed data from after-death interviews with family members and care staff who reported on residents who were cared for and died in NHs and RC/AL settings. The study objectives were to: (1) estimate the prevalence of advance LST decisions made; (2) determine characteristics associated with LST decisions; and (3) determine characteristics that are associated with honoring advance decisions about LST.
DESIGN AND METHODS
Facility Sample
This study used data from the End of Life (EOL) in Residential Care and Nursing Homes study which is a project in the Collaborative Studies of Long-Term Care (CS-LTC). Established in 1997, the CS-LTC includes a stratified sample of licensed LTC facilities in four states (Florida, Maryland, North Carolina, and New Jersey) that includes NHs and three types of RC/AL communities: facilities with fewer than 16 beds; larger “new-model” facilities (tending to have nursing support available and private accommodations); and larger “traditional” facilities that do not meet the “new-model” definition established in prior work (Zimmerman et al., 2003). A detailed overview of the CS-LTC cohort is provided elsewhere (Zimmerman et al., 2001). Facility recruitment for the EOL study occurred from July 2002 to March 2003. The final sample included consenting facilities from the original CS-LTC sample (developed in 1996) plus additional facilities randomly selected from current stratified state registries to address the study’s goal of reflecting attrition of older facilities and opening of new facilities. Identification of deaths began in a facility as soon as it was recruited. A total of 230 facilities were enrolled in the EOL study: 31 NHs and 199 RC/AL settings.
To identify LTC residents who had recently died, a facility liaison was telephoned monthly during the enrollment period and asked about all deaths in the previous month. Given that the focus of this study was on the EOL care provided in LTC settings, residents who died more than 3 days after discharge from the facility, or who had not lived in the facility for at least 15 days during their last month of life, were ineligible.
Subject Sample and Measures
For each eligible LTC resident, an interview was conducted with a family caregiver, defined as the person most involved in care decisions for the deceased LTC resident during the last month of life and who visited the resident and/or spoke with staff on the LTC resident’s behalf at least once during the last month of life. An interview also was conducted with the staff member who knew the LTC resident best, as identified by the facility liaison. Overall, the study conducted a total of 451 family and 677 staff interviews for 792 decedents. Since these analyses required data from both sources, only the 327 decedents with complete data from both family and staff interviews were included.
Family caregivers were mailed a letter of condolence, introduction to the study, and consent form four weeks after the death. Within the next two weeks, research staff telephoned and requested an interview. Verbal consent was obtained at the beginning of each telephone interview. Staff respondents were contacted by telephone shortly after the death was reported to the research team. Nearly all (95%) family caregiver and staff interviews were completed within six months of the death. Also, each facility’s administrator provided information about the facility’s characteristics, policies, and procedures. Recruitment, consent, and data collection procedures were approved by the Committee for the Protection of the Rights of Human Subjects of the University of North Carolina at Chapel Hill.
The family caregiver interview included questions about the LTC resident (such as marital status, race, and ethnicity), as well as four items concerning LST decisions: “Was a decision ever made (not just during the last months of life) in discussions with the doctor about whether or not: a) to do CPR, by that I mean resuscitation, starting the heart if it has stopped?; b) to put in a feeding tube if [HE/SHE] could not eat?; c) to transfer [HIM/HER] to the hospital or emergency department if [HE/SHE] got worse during the last months of life?; and d) to give antibiotics in case of infection?” For each of these to which the family caregivers replied yes, a second question was asked: “What was that decision?” Family caregivers also answered questions about their level of involvement in the care of the resident, the number of days they visited in the last month of life, whether they had met the resident’s physician, the resident’s health in the last month of life, and whether they knew that the resident’s death was imminent (“In other words, did you know that HIS/HER death was days or weeks away?”).
Information concerning whether or not residents received specific LST during the last month of life was obtained from the staff person in the facility who had been most familiar with the resident’s care. Specifically, staff respondents reported on whether the resident: (1) was transferred to the hospital; or received (2) resuscitation attempts; (3) feeding tube insertion; or (4) antibiotics during the last month of life while in the facility. Decedent cognitive status (impaired/unimpaired) was determined by asking the staff respondent whether the resident had, “a diagnosis of Alzheimer’s disease or a related disease with significant problems with memory, confusion, and difficulty making decisions or communicating” or was unable to speak or write in a meaningful way in the last month of life. Facility data such as size (number of beds), type (NH or RC/AL), and proprietary status (for-profit or nonprofit) were obtained from the administrator. The facility liaison who informed study staff of the death of each resident also reported the resident’s length of stay in the facility, as well as whether there was a Do Not Resuscitate (DNR) or DNH order on the chart.
Data Analyses
Descriptive statistics were used to describe characteristics of the family caregivers, LTC residents, LTC facilities, decisions about LST reported by family caregivers (related to CPR, feeding tube or antibiotics in the facility, and hospital transfer), and the incidence of each of these interventions. Given how different these LSTs are in terms of their cultural and clinical implications we felt it important to examine them separately. For each LST, associations between resident, family and facility characteristics, and whether or not a decision was made about that intervention, were examined using logistic regression, employing Generalized Estimating Equations (GEE) to account for clustering of family respondents within facilities. Due to the small number of LSTs reported, only administration of antibiotics and hospitalization was further analyzed. For these two LSTs, in the subset having made a decision and who received the intervention, associations between characteristics of the resident, family, facility, and whether the decision was heeded were examined, again using GEE applied to logistic regression. Analyses were performed using SAS, version 9.1 (SAS Institute, Inc., Cary, NC).
RESULTS
Study Sample
The final sample consisted of 327 LTC residents, about half from NHs (n=154, 47.1%) and half from RC/AL settings (n=173, 52.9%). The residents were from 27 different NHs and 85 different RC/AL communities. Table 1 displays characteristics of the decedent residents, family caregivers, and LTC facilities. Residents were mostly white, non-Hispanic (91.7%) and female (71.6%), with an average age of 86.6 years (range 39-107). The majority of the residents were cognitively impaired (77.4%). Most of the family members classified the resident’s illness in the last months of life as a “steady, slow decline” (66.5%), and about half (51.4%) reported expecting the death imminently. The majority of family caregivers reported their involvement in the resident’s care at the EOL as high (25.1%) or very high (54.8%), and the average number of days reported visiting in the last month of life was 15.2 (range 0-31). Most residents died in their LTC facility (86.9%), while the rest died in a hospital, a hospice facility, or died in transit. Many residents had DNR (78.0%, n=255) and/or DNH (21.1%, n=69) orders in their chart.
Table 1.
Characteristics of the 327 decedents, their families and facilities
| N* (%) or Mean (SD; range) |
|
|---|---|
| Decedent Characteristics | |
| Age (yrs) | 86.6 (9.9; 39-107) |
| Gender: Female | 234 (71.6) |
| Race/Ethnicity | |
| White, non-Hispanic | 300 (91.7) |
| White, Hispanic | 7 (2.1) |
| Black | 17 (5.2) |
| Other | 3 (0.9) |
| Marital status | |
| Never married | 29 (9.0) |
| Married | 50 (15.5) |
| Widowed | 216 (67.1) |
| Divorced/separated | 27 (8.4) |
| Cognitively impaired | 253 (77.4) |
| Health in last months | |
| Stable health | 37 (11.4) |
| Steady, slow decline | 216 (66.5) |
| Series of ups and downs | 72 (22.2) |
| Location of death | |
| Facility | 284 (86.9) |
| Hospital | 40 (12.2) |
| Other | 3 (0.9) |
| Length of stay (yrs) | 2.4 (2.8; 0-22) |
| Medicaid is primary payer | 122 (38.2) |
| Family Member Characteristics | |
| Family relationship | |
| Spouse | 24 (7.3) |
| Daughter, daughter-in-law | 156 (47.7) |
| Son, son-in-law | 63 (19.3) |
| Sibling, other relative | 62 (19.0) |
| Other | 22 (6.7) |
| Family education | |
| High school or less | 72 (22.2) |
| Tech/trade school or some college | 101 (31.2) |
| College graduate | 151 (46.6) |
| Family’s involvement in care | |
| Low/very low | 22 (6.8) |
| Moderate | 43 (13.3) |
| High | 81 (25.1) |
| Very high | 177 (54.8) |
| Days family visited in last month | 15.2 (10.2; 0-31) |
| Family ever met face-to-face with MD | 232 (70.9) |
| Death was expected | 168 (51.4) |
| Facility Characteristics | |
| Facility Type | |
| RC/AL | 173 (52.9) |
| Nursing home | 154 (47.1) |
| Number of beds | 79.1 (46.1; 5-180) |
| For-profit facility | 236 (72.2) |
Missing data as follows: marital status (n=5); Medicaid (8); health in last months (2); family involvement in care (4); provision of MD/PA visits (21); ≥75% residents have same MD (39)
Cardiopulmonary Resuscitation
A decision was recorded about CPR for most (N=290; 89.0%) subjects, almost all of whom (N=277, 95.5%) desired not to be resuscitated. Family caregivers who were more likely to have made a decision with a doctor about CPR were more likely to be college educated (compared to those with a high school education or less; p=.033), report a very high level of involvement (p<.001), and to have visited more often during the last month (15.7 vs. 11.0 days, p<.032) compared to those who reported that a decision had not been made (Table 2). A total of 8 residents received CPR in the facility in the last month of life, and of these, only one had no reported decision regarding CPR. Of the other seven, five were reported not to have wanted resuscitation according to the family caregiver, and three actually had a DNR order on their medical charts.
Table 2.
Characteristics associated with report of having made a decision about CPR, feeding tube, antibiotics, or hospitalization
| CPR (N=326) | Feeding Tube (N=324) | Antibiotics (N=314) | Hospitalization (N=314) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| N (%) or Mean (SD) making a decision |
p-value a | N (%) or Mean (SD) making a decision |
p-value a | N (%) or Mean (SD) making a decision |
p-value a | N (%) or Mean (SD) making a decision |
p-value a | |||||
|
| ||||||||||||
| Overall | 290 | (89.0) | 267 | (82.4) | 203 | (64.6) | 271 | (86.3) | ||||
| Decedent Characteristics | ||||||||||||
| Age (yrs)b | 86.9 | (8.6) | 0.210 | 86.5 | (8.2) | 0.646 | 86.6 | (8.1) | 0.635 | 86.7 | (8.2) | 0.439 |
| Gender | ||||||||||||
| Male | 79 | (85.9) | 0.237 | 74 | (81.3) | 0.712 | 52 | (58.4) | 0.177 | 76 | (82.6) | 0.772 |
| Female | 211 | (90.2) | 193 | (82.8) | 151 | (67.1) | 195 | (84.1) | ||||
| Race/Ethnicity | ||||||||||||
| White, non-Hispanic | 265 | (88.6) | 0.540 (vs. all) |
244 | (82.2) | 0.687 (vs. all) |
183 | (63.5) | 0.142 (vs. all) |
248 | (83.5) | 0.816 (vs. all) |
| White, Hispanic | 7 | (100. 0) |
6 | (85.7) | 7 | (100.0) | 7 | (100. 0) |
||||
| Black | 16 | (94.1) | 15 | (88.2) | 12 | (75.0) | 14 | (82.4) | ||||
| Other | 2 | (66.7) | 2 | (66.7) | 1 | (33.3) | 2 | (66.7) | ||||
| Marital status | ||||||||||||
| Never married | 19 | (67.9) | <0.001 | 18 | (64.3) | 0.019 | 19 | (67.9) | 24 | (82.8) | ||
| Married | 41 | (82.0) | 0.022 | 42 | (84.0) | 0.876 | 26 | (53.1) | 39 | (78.0) | ||
| Widowed | 201 | (93.1) | -- ref0.003 | 178 | (83.2) | -- ref0.071 | 135 | (65.5) | -- ref0.741 | 180 | (84.5) | -- ref0.297 |
| Divorced/separated | 24 | (88.9) | 0.462 | 24 | (88.9) | 0.464 | 18 | (69.2) | 23 | (85.2) | ||
| Cognitive Status | ||||||||||||
| Cognitively impaired | 227 | (89.7) | 0.415 | 211 | (84.1) | 0.114 | 157 | (64.3) | 0.841 | 210 | (84.0) | 0.740 |
| Cognitively intact | 63 | (86.3) | 56 | (76.7) | 46 | (65.7) | 61 | (82.4) | ||||
| Health in last months | ||||||||||||
| Stable health | 29 | (78.4) | 0.056 | 26 | (72.2) | 0.047 | 22 | (61.1) | 27 | (75.0) | ||
| Steady, slow decline | 194 | (89.8) | 0.666C | 177 | (82.3) | 0.384C | 132 | (64.4) | 180 | (84.1) | ||
| Series of ups and downs | 65 | (91.5) | --ref0.063 | 62 | (87.3) | --ref0.099 | 47 | (66.2) | --ref0.852 | 63 | (87.5) | --ref0.329 |
| Location of death | ||||||||||||
| Facility | 249 | (88.0) | 0.157 | 230 | (81.9) | 0.478 | 176 | (64.9) | 0.790 | 234 | (83.3) | 0.642 |
| Hospital/Other | 41 | (95.3) | 37 | (86.0) | 27 | (62.8) | 37 | (86.0) | ||||
| Length of stay (yrs) | 2.3 | (2.) | 0.105 | 2.3 | (2.4) | 0.176 | 2.3 | (2.6) | 0.314 | 2.4 | (2.6) | 0.552 |
| Medicaid is primary payerb | 37.0 | (30.6) | 0.121 | 37.5 | (30.5) | 0.741 | 42.4 | (30.6) | 0.023 | 38.6 | (30.6) | 0.462 |
| Family Member Characteristics | ||||||||||||
| Family education | ||||||||||||
| High school or less | 59 | (81.9) | 0.033 | 56 | (77.8) | 45 | (66.2) | 0.719 | 58 | (80.6) | ||
| Tech/trade school or Some college |
90 | (89.1) | 0.444 | 82 | (82.0) | 56 | (57.7) | 0.076 | 82 | (82.8) | ||
| College graduate | 138 | (92.0) | -- ref0.102 | 126 | (84.6) | --ref0.408 | 100 | (68.5) | --ref0.200** | 128 | (85.3) | --ref0.656 |
| Family relationship | ||||||||||||
| Spouse | 21 | (87.5) | --ref0.546 | 23 | (95.8) | --ref0.179* | 12 | (50.0) | --ref0.357 | 19 | (79.2) | --ref0.648 |
| Daughter, daughter-in-law | 142 | (91.0) | 132 | (85.2) | 103 | (66.9) | 128 | (83.1) | ||||
| Son, son-in-law | 57 | (90.5) | 49 | (77.8) | 40 | (69.0) | 51 | (81.0) | ||||
| Sibling, Other relative | 50 | (82.0) | 45 | (73.8) | 38 | (65.5) | 53 | (86.9) | ||||
| Other | 20 | (90.9) | 18 | (85.7) | 10 | (50.0) | 20 | (90.9) | ||||
| Family involvement very high | ||||||||||||
| No | 119 | (82.1) | <0.001 | 109 | (75.2) | 0.003 | 85 | (60.3) | 0.175 | 120 | (82.8) | 0.765 |
| Yes | 167 | (94.4) | 154 | (88.0) | 115 | (68.0) | 147 | (84.0) | ||||
| Days visited in last monthb | 15.7 | (10.3) | 0.032 | 16.2 | (10.3) | <0.001 | 16.2 | (10.5) | 0.037 | 15.6 | (10.4) | 0.078 |
| Family expected death | ||||||||||||
| No | 139 | (88.0) | 0.530 | 130 | (83.3) | 0.651 | 93 | (60.4) | 0.080 | 135 | (86.5) | 0.126 |
| Yes | 151 | (89.9) | 137 | (81.5) | 110 | (68.8) | 136 | (81.0) | ||||
| Family ever met face-to-face with MD |
||||||||||||
| No | 79 | (84.0) | 0.117 | 72 | (77.4) | 0.150 | 55 | (59.1) | 0.203 | 74 | (78.7) | 0.146 |
| Yes | 211 | (90.9) | 195 | (84.4) | 148 | (67.0) | ||||||
| Facility Characteristics | ||||||||||||
| Facility type | ||||||||||||
| RC/AL | 153 | (89.0) | 0.998 | 139 | (81.8) | 0.781 | 90 | (55.6) | 0.002 | 138 | (81.2) | 0.274 |
| Nursing home | 137 | (89.0) | 128 | (83.1) | 113 | (74.3) | 133 | (86.4) | ||||
| Number of bedsb | 79.4 | (46.0) | 0.760 | 78.5 | (45.6) | 0.489 | 84.4 | (44.6) | 0.025 | 80.8 | (45.4) | 0.354 |
| Proprietary status | ||||||||||||
| For-profit | 207 | (88.1) | 0.378 | 193 | (82.8) | 0.757 | 142 | (62.8) | 195 | (83.3) | 0.840 | |
| Not-for-profit | 83 | (91.2) | 74 | (81.3) | 61 | (69.3) | 76 | (84.4) | ||||
Based on unadjusted GEE logistic regression models (with whether or not decision was made as the dependent variable and the characteristic shown as the single independent variable), specifying independent working correlation matrix for facility; p-values based on empirical (robust) standard errors. Note that for multi-category variables, pairwise comparisons shown only if overall (k-1 df) p-value (shown as superscript by reference category) is p<0.200.
For those not making a decision, the mean (SD) for CPR, feeding tube, antibiotic, and hospitalization are, respectively: for age, 84.7 (11.3), 87.2 (11.8), 86.1 (10.6), 85.6 (12.1); for days visited, 11.0 (10.9), 10.2 (10.1), 13.7 (10.6), 13.0 (10.9); for facility size, 76.9 (50.3), 83.7 (50.0), 71.0 (48.6), 73.3 (50.3); for percent Medicaid, 45.4 (30.3), 39.3 (32.0), 32.2 (29.4), 34.7 (31.0); for length of stay (years), 3.1 (3.8), 2.8 (4.2), 2.6 (3.0), 2.6 (3.4)
For decision about CPR, the p-value for stable health vs. slow, steady decline is 0.027; for decision about feeding tube, the p-value for stable health vs. slow, steady decline is 0.099.
Feeding Tube
Most residents (N=267; 82.4%) had reportedly made a decision about feeding tubes and the majority of those (N=248; 92.9%) had decided against this type of LST. As with CPR, family caregivers were more likely to have made a decision if they reported very high care involvement (p<.003), or more visits during the last month (16.2 vs. 10.2 days; p<.001). Also, residents for whom decisions had been made were more likely to be experiencing a series of ups and downs in their clinical course compared to those in more stable condition (p<.05). Of the 8 residents reported to have received a feeding tube in the facility, seven reported having had discussions with a doctor about it previously and in one case the decision had been against a feeding tube.
Antibiotics
Only about two-thirds of family caregivers reported having a discussion with a physician about the use of antibiotics (N=203; 64.6%); and most respondents (N=161; 79.1%) were in favor of using antibiotics when indicated. Those reporting a decision concerning use of antibiotics spent more days visiting in the last month of life (16.2 vs. 13.7; p=.037). Family caregivers of residents from NHs were more likely to have reported a decision (74.3%) about antibiotics than caregivers from RC/AL settings (55.6%, p=.002). Related to this finding, those with a decision about antibiotics were more likely to have been on Medicaid (42.4% vs. 32.2%; p=.023) and to live in larger facilities (84.4 vs. 71.0 beds; p=.025). Of the 113 residents reported to have received antibiotics in the last months of life, more than two-thirds (N=78; 69.0%) had made a prior decision regarding their use according to their family caregiver, and fifteen residents who received antibiotics had reports of prior decisions to not use them. The mean age of those whose decisions were not heeded was 91.7 compared to 85.0 for those who decisions were heeded (p=.014; see Table 3).
Table 3.
Among those who made a decision about and then received antibiotics (n=78), or were hospitalized (n=87), correlates of family’s decision
| Among those receiving antibiotics (N=78) |
Among those receiving hospitalization (N=87) |
|||||
|---|---|---|---|---|---|---|
|
|
||||||
| Family decision on Antibiotics |
Family decision on Hospitalization |
|||||
| Yes, do it (N=63) |
No, don’t do it (N=15) |
Yes, do it/Varied (N=61) |
No, don’t do it (N=26) |
|||
|
|
|
|||||
| N ( column %) or Mean (SD) | p-valuea | N ( column %) or Mean (SD) | p-valuea | |||
| Decedent Characteristics | ||||||
| Age (yrs) | 85.0 (10.3) | 91.7 (6.7) | 0.014 | 86.9 (7.7) | 84.0 (9.5) | 0.103 |
| Female | 43 (68.3) | 11 (73.3) | 0.663 | 42 (68.9) | 22 (84.6) | 0.116 |
| White, non-Hispanic | 59 (93.7) | 15 (100.0) | 0.835 | 54 (88.5) | 22 (84.6) | 0.669 |
| Married | 10 (16.1) | 0 (0.0) | 0.196 | 8 (13.1) | 2 (9.1) | 0.632 |
| Cognitively impaired | 46 (73.0) | 14 (93.3) | 0.134 | 41 (67.2) | 17 (65.4) | 0.873 |
| Health last months, steady slow decline | 39 (62.9) | 8 (53.3) | 0.748 | 29 (47.5) | 17 (65.4) | 0.110 |
| Length of stay (yrs) | 2.4 (2.5) | 2.9 (2.8) | 0.542 | 2.2 (2.3) | 2.8 (2.8) | 0.219 |
| Medicaid is primary payer | 28 (45.9) | 7 (46.7) | 0.953 | 16 (27.1) | 10 (38.5) | 0.272 |
| Family Member Characteristics | ||||||
| Family education | ||||||
| High school or less | 3 (20.0) | 20 (32.8) | 0.669 | 8 (30.8) | 11 (18.6) | 0.418 |
| Tech/trade school or some college | 7 (46.7) | 17 (27.9) | 0.289 | 7 (26.9) | 24 (40.7) | 0.473 |
| College graduate | 5 (33.3) | 24 (39.3) | - ref | 11 (42.3) | 24 (40.7) | - ref |
| Family’s involvement very high | 34 (55.7) | 7 (50.0) | 0.672 | 34 (55.7) | 14 (56.0) | 0.983 |
| Days family visited in last month | 16.7 (9.9) | 13.7 (10.0) | 0.296 | 14.8 (10.0) | 15.4 (8.4) | 0.778 |
| Family expected death | 36 (57.1) | 7 (46.7) | 0.465 | 20 (32.8) | 14 (53.8) | 0.086 |
| Family ever met face-to-face with MD | 43 (68.3) | 12 (80.0) | 0.305 | 43 (70.5) | 20 (76.9) | 0.483 |
| Facility Characteristics | ||||||
| Nursing home (vs. RC/AL) | 41 (65.1) | 9 (60.0) | 0.685 | 20 (32.8) | 14 (53.8) | 0.034 |
| Number of beds | 88.5 (44.8) | 76.1 (42.1) | 0.289 | 73.0 (45.2) | 72.1 (45.3) | 0.913 |
| For-profit facility | 41 (65.1) | 12 (80.0) | 0.184 | 48 (78.7) | 20 (76.9) | 0.850 |
Based on GEE applied to logistic regression, specifying independent working correlation matrix for facility.
Using exact logistic regression because of 0 cell; does not adjust for clustering within facility
Hospitalization
A decision about hospitalization was reported for the majority (N=271; 86.3%) of decedents. Of these, 86 (31.7%) preferred hospitalization if indicated, 63 (23.2%) said the decision depended on the situation, and 122 (45.0%) preferred no hospitalizations. No resident, family caregiver, or facility factors were associated with having made a decision whether or not to hospitalize.
Of the 101 residents who were hospitalized in the last month of life, 87 had reportedly made prior decisions regarding whether hospitalization would be desired. Of those, 26 (25.7%) had indicated that the resident should not be hospitalized, and four had a DNH order found on their chart. More than half (53.8%) of those whose decision was not heeded lived in a NH compared to 32.8% of those whose decision was heeded (p=.034; see Table 3).
DISCUSSION
This study is the first to examine LST decisions in both NHs and RC/AL settings and also to examine the characteristics associated with non-adherence with decisions. Although previous studies have evaluated associations between LTC resident characteristics and documentation of LSTs, ours is the first to study family reports of LST decisions, to include RC/AL settings, and to consider characteristics of family caregivers who may be involved in decisions about LSTs in LTC (Dobalian, 2006; Levy et al., 2005; Messinger-Rapport & Kamel, 2005; Resnick et al., 2008).
Most family members reported that a decision was made with a physician about the four LSTs we studied; rates of reported decision-making ranged from 64.6% for antibiotics to 82.4-89.0% for tube feeding, hospitalization, and CPR. These prevalences of “reported decisions made” about LSTs are much higher than recent reports of LST orders on charts. Large national studies of NHs in 1991, 1996, and 2004 find DNR rates increasing from 32% to 39% to 60% and DNH rates increasing from 2% to 3% to 4% (Dobalian, 2006; Levy et al., 2005; Resnick et al., 2008). In our study 81% of the group that reported a decision had been made to resuscitate actually had a DNR on the resident’s chart. More concerning was that only 28% of those who reported a decision had been made not to hospitalize had a DNH order on the chart. It is notable that prior research has shown that the presence of written advance directives in the medical record did not improve the already high incidence of providing EOL care concordant with previously expressed wishes (Danis et al., 1991). However, these discrepancies between reported decisions and charted orders highlight the issue that physicians, even when we have conversations about the use of LSTs, may not be documenting the conversation or writing the orders in the chart. It may also be that the family caregiver or resident took part in the discussion, but did not desire a medical order to be written. Past research indicates that patient and families have a difficult time committing to advance directives for EOL care. (Cherlin et al., 2005; Golin et al., 2000; Happ et al., 2002)
In our sample few characteristics of the residents themselves were significantly associated with having made LST decisions and having those decisions honored. Those residents who had never married were least likely to have family report a decision had been made about CPR (67.9% as compared to 82.0 to 93.1% for other marital statuses) and use of a feeding tube (64.3% compared to 84.0 to 88.9% for others), which may be because these residents did not have surviving family members who felt authorized to make these decisions. There was also a trend for residents reported to have more stable health to be less likely to have made decisions about LSTs, likely because these residents and their families did not anticipate the need for EOL discussions in light of their stable health.
We did find that characteristics of family members of LTC residents were associated with differences in reported decisions and care. Family members who were more involved in care were significantly more likely to report having made a decision about CPR, feeding tube, or antibiotic use. . These findings are consistent with previous research showing that family members are more likely engage in decision-making about LSTs after being educated generally about EOL care (Braun, Karel, & Zir, 2006) Opportunities for physicians to have discussions with family members of LTC residents who are not acutely ill may be limited, so perhaps physicians should take any face-to-face opportunity they have to ensure these conversations take place, are documented, and appropriate orders are in the chart. At the very least, facilities and physicians should work towards educating family members of LTC residents about end-of-life care.
The majority of care provided was in concordance with treatment preferences, except for CPR. Reported care was inconsistent with decisions made in only one of seven feeding tube insertions (14.3%), 15 of 78 residents who received antibiotics (19.2%), and 26 of 87 hospital transfers (29.9%), but in five of seven resuscitations (71.4%). It is not clear whether the care providers were aware of the LST decisions that had been made at the time the LST was performed, or whether the patient or family member overrode the previous decision at the time the LST was clinically indicated. The factors that were associated with having made a decision and having that decision honored varied by LST, a finding that is consistent with reports by other investigators (Dobalian, 2004; Hamel et al., 2000; Messinger-Rapport & Kamel, 2005; Monturo & Strumpf, 2007).
Where there was discordance between preferences and practice there was precedence for some, but not all, of what we found. Older residents were more likely to receive antibiotics when there had been a decision against this, and those in NHs were more likely to be hospitalized when there had been a decision against this. The first finding is surprising, as previous investigators have found (in hospital settings) that older age is associated with a higher rate of withholding LSTs, even if the patient preferred to receive them (Hamel et al., 1999). Perhaps older NH residents are more likely to have surrogate decision makers who fail to honor the resident’s care preferences, even after discussions about them, as has been found in prior studies (Fagerlin, Ditto, Danks, Houts, & Smucker, 2001; Shalowitz, Garrett-Mayer, & Wendler, 2006). Age and frailty may also promote surrogate decision-making among physicians, other care providers, and family members for the oldest old NH residents. Such a hypothesis is consistent with a systematic review of patient and surrogate responses about LSTs at the EOL which found that surrogates would incorrectly direct treatment at least one third of the time (Shalowitz et al., 2006).
The resident’s cognitive status did not rise to the level of statistical significance as a correlate to families reporting having made a decision about LSTs, or to having these decisions honored. However the numbers of cognitively impaired residents receiving LSTs were small. For instance, 15 of the 78 LTC residents who received antibiotics had made a prior decision not to use them, and 14 of those 15 were cognitively impaired (p=.134). Because cognitively impaired residents frequently have surrogate decision makers, the aforementioned issues of surrogates could be driving inconsistencies in desires and care. However, we found that family presence and involvement with care in the last month of life were not associated with adherence to decisions. Further research with larger numbers of residents who received LSTs after a decision has been discussed and documented is needed to investigate these issues more fully.
While we believe that this is the largest study to report on after-death interviews of staff and families who cared for LTC residents at the EOL in diverse NH and RC/AL settings, it does have several limitations. The sample was limited to those who died in, or within 3 days of leaving, a LTC facility and so excluded residents who died at a later point in time. However, the questions under study relate to care in a LTC facility, so our methods should have captured the appropriate sample to address this. The data represent reporting of discussions and decision-making and do not reflect all that happened at the bedside of the residents who appear to have received unwanted medical interventions. As noted earlier, it is possible that the patient and/or family caregivers could have changed their minds in the last days or hours of life, resulting in care that was contrary to prior decisions about LSTs. Also, it is not possible from these data to determine the concordance of care and preferences in those who did not have medical interventions performed, as it is not possible to know when the interventions might have been indicated and desired, but not carried out. In addition, the retrospective nature of the study needs to be acknowledged, as reports weeks to months after death could be different from those that would have been obtained in a prospective study. Finally, small numbers made several desirable analyses impossible, including those related to racial diversity (92% of the sample was White, non-Hispanic) and to correlates of undesired LSTs.
For physicians and other providers who participate in EOL care, 100% perfect concordance between advance care planning and the actual care provided at the EOL may not be an achievable or even desirable goal. After all, compliance with written advance directives does not necessarily translate into improved comfort at the EOL (Happ, et al., 2002). However, a greater understanding of characteristics that can affect EOL decisions, better education of patients and family caregivers about quality EOL care, and improved physician communication and documentation should result in better EOL care in LTC settings. Physicians and caregivers in a number of states are moving forward with efforts to encourage conversations about LSTs, using concise and recognizable forms to document these decisions and translate them into physicians orders (“POLST in your state,” 2007). Although such tools will help direct discussion and documentation of LSTs, further work concerning residents and family members’ expectations and wishes is needed to optimize EOL care in the LTC setting.
Figure 1.
Prior decision status of residents who received a life-sustaining treatment
ACKNOWLEDGEMENTS
The authors thank the family caregivers, residents, and staff members who participate in the Collaborative Studies of Long-Term Care for their time and commitment to learning more about and improving the quality of life and death in long-term care communities.
This work was supported by grants R01 AG18967, K02 AG00970 and K23 AG001030 from the National Institute on Aging. Dr. Biola’s time was supported by a National Research Service Award Primary Care Research grant (T32 HP-14001-19) from the Health Resources and Services Administration as well as the Duke University Geriatrics Fellowship program. The authors have no other relevant financial disclosures to report. Drs. Zimmerman and Sloane developed the initial study design, including acquisition of subjects and data collection. Dr. Christianna Williams assisted with study design and performed data management, analyses and interpretation and assisted with preparation of the manuscript. Drs. Biola, Williams, Sloane, Daaleman, and Zimmerman participated in the design of these analyses, data interpretation and preparation of the manuscript. The sponsors approved the research proposal to collect the data used in these analyses, but were not involved in the analysis or preparation of this paper.
REFERENCES
- Braun KL, Karel H, Zir A. Family Response to End-of-Life Education: Differences by Ethnicity and Stage of Caregiving. American Journal of Hospice and Palliative Medicine. 2006;23:269–276. doi: 10.1177/1049909106290243. [DOI] [PubMed] [Google Scholar]
- Brock DB, Foley DJ. Demography and epidemiology of dying in the U.S. with emphasis on deaths of older persons. Hospice Journal. 1998;13(1-2):49–60. doi: 10.1080/0742-969x.1998.11882887. [DOI] [PubMed] [Google Scholar]
- Cartwright JC. Nursing homes and assisted living facilities as places for dying. Annual Review of Nursing Research. 2002;20:231–264. [PubMed] [Google Scholar]
- Cherlin E, Fried T, Prigerson HG, Schulman-Green D, Johnson-Hurzeler R, Bradley EH. Communication between physicians and family caregivers about care at the end of life: when do discussions occur and what is said? Journal of Palliative Medicine. 2005;8(6):1176–1185. doi: 10.1089/jpm.2005.8.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culberson J, Levy C, Lawhorne L. Do not hospitalize orders in nursing homes: A pilot study. Journal of the American Medical Directors Association. 2005;6(1):22–26. doi: 10.1016/j.jamda.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Danis M, Southerland LI, Garrett JM, Smith JL, Hielema F, Pickard CG, et al. A prospective study of advance directives for life-sustaining care. New England Journal of Medicine. 1991;324(13):882–888. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- Dobalian A. Nursing facility compliance with do-not-hospitalize orders. Gerontologist. 2004;44(2):159–165. doi: 10.1093/geront/44.2.159. [DOI] [PubMed] [Google Scholar]
- Dobalian A. Advance care planning documents in nursing facilities: Results from a nationally representative survey. Archives of Gerontology and Geriatrics. 2006;43(2):193–212. doi: 10.1016/j.archger.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Ditto PH, Danks JH, Houts R, Smucker WD. Projection in surrogate decisions about life-sustaining medical treatment. Health Psychology. 2001;20:166–175. [PubMed] [Google Scholar]
- Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. New England Journal of Medicine. 2000;342(3):206–210. doi: 10.1056/NEJM200001203420312. [DOI] [PubMed] [Google Scholar]
- Golin CE, Wenger NS, Liu H, Dawson NV, Teno JM, Desbiens NA, et al. A prospective study of patient-physician communication about resuscitation. Journal of the American Geriatrics Society. 2000;48(5 Suppl):S52–60. doi: 10.1111/j.1532-5415.2000.tb03141.x. [DOI] [PubMed] [Google Scholar]
- Hamel MB, Lynn J, Teno JM, Covinsky KE, Wu AW, Galanos A, et al. Age-related differences in care preferences, treatment decisions, and clinical outcomes of seriously ill hospitalized adults: lessons from SUPPORT. Journal of the American Geriatrics Society. 2000;48(5 Suppl):S176–182. doi: 10.1111/j.1532-5415.2000.tb03129.x. [DOI] [PubMed] [Google Scholar]
- Hamel MB, Teno JM, Goldman L, Lynn J, Davis RB, Galanos AN, et al. Patient age and decisions to withhold life-sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Annals of Internal Medicine. 1999;130(2):116–125. doi: 10.7326/0003-4819-130-2-199901190-00005. [DOI] [PubMed] [Google Scholar]
- Happ MB, Capezuti E, Strumpf NE, Wagner L, Cunningham S, Evans L, et al. Advance care planning and end-of-life care for hospitalized nursing home residents. Journal of the American Geriatrics Society. 2002;50(5):829–835. doi: 10.1046/j.1532-5415.2002.50207.x. [DOI] [PubMed] [Google Scholar]
- Lamberg JL, Person CJ, Kiely DK, Mitchell SL. Decisions to hospitalize nursing home residents dying with advanced dementia. Journal of the American Geriatrics Society. 2005;53(8):1396–1401. doi: 10.1111/j.1532-5415.2005.53426.x. [DOI] [PubMed] [Google Scholar]
- Levy CR, Fish R, Kramer A. Do-not-resuscitate and do-not-hospitalize directives of persons admitted to skilled nursing facilities under the Medicare benefit. Journal of the American Geriatrics Society. 2005;53(12):2060–2068. doi: 10.1111/j.1532-5415.2005.00523.x. [DOI] [PubMed] [Google Scholar]
- Messinger-Rapport BJ, Kamel HK. Predictors of do not resuscitate orders in the nursing home. Journal of the American Medical Directors Association. 2005;6(1):18–21. doi: 10.1016/j.jamda.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Monturo CA, Strumpf NE. Advance Directives at End-of-Life: Nursing Home Resident Preferences for Artificial Nutrition. Journal of the American Medical Directors Association. 2007;8(4):224–228. doi: 10.1016/j.jamda.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Morrison RS, Morrison EW, Glickman DF. Physician reluctance to discuss advance directives. An empiric investigation of potential barriers. Archives of Internal Medicine. 1994;154(20):2311–2318. [PubMed] [Google Scholar]
- National Institutes of Health Consensus Statement, Improving End-of-Life Care. 2004 from http://consensus.nih.gov/2004/2004EndOfLifeCareSOS024PDF.pdf.
- [Retrieved December 20, 2007];POLST in your state. 2007 Aug; 2007. from www.POLST.org.
- Resnick HE, Schuur JD, Heineman J, Stone R, Weissman JS. Advance Directives in Nursing Home Residents Aged >= 65 Years: United States 2004. American Journal of Hospice and Palliative Care. 2008;25(6):476–482. doi: 10.1177/1049909108322295. [DOI] [PubMed] [Google Scholar]
- Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Archives of Internal Medicine. 2006;166(5):493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- Sloane PD, Zimmerman S, Williams CS, Hanson L. Dying with dementia in long-term care. Gerontologist. 2008;48(6):741–751. doi: 10.1093/geront/48.6.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teno JM, Branco KJ, Mor V, Phillips CD, Hawes C, Morris J, et al. Changes in advance care planning in nursing homes before and after the patient Self-Determination Act: report of a 10-state survey. Journal of the American Geriatrics Society. 1997;45(8):939–944. doi: 10.1111/j.1532-5415.1997.tb02963.x. [DOI] [PubMed] [Google Scholar]
- Torke AM, Simmerling M, Siegler M, Kaya D, Alexander GC. Rethinking the ethical framework for surrogate decision making: a qualitative study of physicians. Journal of Clinical Ethics. 2008;19(2):110–119. [PubMed] [Google Scholar]
- Zimmerman S, Gruber-Baldini AL, Sloane PD, Eckert JK, Hebel JR, Morgan LA, et al. Assisted living and nursing homes: apples and oranges? Gerontologist. 2003;43(Spec No 2):107–117. doi: 10.1093/geront/43.suppl_2.107. [DOI] [PubMed] [Google Scholar]
- Zimmerman S, Sloane P, Eckert J, Buie V, Walsh J, Hebel J, et al. Overview of the collaborative studies of long-term care. In: Zimmerman S, Sloane P, Eckert J, editors. Assisted Living: Needs, Practices and Policies in Residential Care for the Elderly. Johns Hopkins University Press; Baltimore: 2001. [Google Scholar]
- Zimmerman S, Sloane PD, Eckert JK, Gruber-Baldini AL, Morgan LA, Hebel JR, et al. How good is assisted living? Findings and implications from an outcomes study. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60:S195–S204. doi: 10.1093/geronb/60.4.s195. [DOI] [PubMed] [Google Scholar]