Abstract
Transhiatal herniation of the pancreas is an extremely rare condition. In the published literature we found only eleven cases reported in the period of 1958 to 2011. A coincidental hiatal herniation of the duodenum is described in two cases only. To our knowledge, we report the first case with a hiatal herniation of the complete duodenum and proximal pancreas presenting an intrathoracic major duodenal papilla with consecutive intrahepatic and extrahepatic cholestasis. A 72-year-old Caucasian woman was admitted to our department with a hiatal hernia grade IV for further evaluation. According to our recommendation of surgical hernia repair soon after the diagnosis of a transhiatal herniation of the proximal pancreas and entire duodenum, we had to respect the declared intention of the patient for a conservative procedure. So we were forced to wait for surgical repair within an emergency situation complicated by a myocardial infarction and reduced general condition. We discuss the therapeutic decision making process and a complete literature review of this rare entity.
Keywords: Hiatal hernia, Paraesophageal hernia, Intrathoracic pancreas, Intrathoracic duodenum, Diaphragmatic hernia
Core tip: Hiatal herniation of the pancreas is a rarity. In the world literature we identified 11 cases reported from 1958 to 2011. A 72-year-old Caucasian woman was admitted to the hospital with symptoms of mechanical cholestasis such as mild jaundice, pruritus, diarrhea and fatigue. Our case illustrates the serious sequelae of a hiatal hernia (HH) type IV that can occur when treated conservatively and therefore we recommend that all HH type IV should be repaired as soon as possible after the diagnosis. Despite of the fatal outcome we were encouraged to publish this case to improve future decision finding processes in similar cases.
INTRODUCTION
Hiatal herniation of the pancreas is a rarity. In the world literature we identified 11 cases reported from 1958 to 2011 (Table 1). All reported patients were symptomatic except one case reported by Katz et al[1]. Surgical repair of the hernia was performed in all patients except one recently reported case by Rozas et al[2].
Table 1.
Review of the literature: Transhiatal herniation of the pancreas
| Author | Age (yr) | Sex | Herniated part of pancreas | Other herniated organs | Cholest- asis | Pancreat- itis | Sympto- matic | Myocardial Infarction | Surgery |
| Moore et al[9], 1958 | 67 | F | Head | Pylorus, proximal duodenum | - | - | + | - | + |
| Coral et al[5], 1987 | 56 | M | Body-tail | - | - | - | + | - | + |
| Kafka et al[11], 1994 | 71 | F | Head-body | Stomach, duodenum | - | + | + | + | + |
| Chevallier et al[12], 2001 | 70 | M | Body-tail (transient) | - | - | + | + | - | + |
| Katz et al[1], 2002 | 74 | M | Body-tail | - | - | - | - | - | + |
| Skinner et al[17], 2003 | 52 | M | Body | Gastric fundus | - | - | + | - | + |
| Saxena et al[14], 2006 | 78 | F | Complete | - | - | + | + | - | + |
| Tagaya et al[15], 2007 | 75 | F | Body-tail | Jejunum, transverse colon | - | + | + | - | + |
| Maksoud et al[13], 2010 | 68 | M | Complete (transient) | Stomach, transverse colon | - | + | + | - | + |
| Rozas et al[2], 2010 | 78 | F | Head | Stomach | - | + | + | - | - |
| Coughlin et al[16], 2011 | 61 | F | Mid-body | Stomach | - | - | + | - | + |
F: Female; M: Male.
To the best of our knowledge, we describe the first case of a hiatal hernia (HH) type IV with herniation of the complete duodenum and proximal pancreas presenting an intrathoracic major duodenal papilla with consecutive intra- and extrahepatic cholestasis.
HH are categorized into four types. Type I or sliding HH accounting for 85%-95% is characterized by an intact, circumferential lax phrenoesophageal membrane and widening of the muscular hiatal tunnel[3]. Types II, IIIand IV (5%-15%) are subsumed as paraesophageal hernia (PEH). A type II hernia results from a localized defect in the phrenoesophageal membrane while the gastroesophageal junction remains fixed to the preaortic fascia and the median arcuate ligament[3]. A type III hernia has aspects of both types I and II. Typical for a type IV HH is a large defect in the phrenoesophageal membrane with herniation of other abdominal organs (colon, spleen, pancreas and small intestine).
The uniqueness of our case is characterized by the transhiatal herniation of the duodeno-pancreatic unit (duodenal C, pancreatic head, major and minor duodenal papilla, common bile duct and pancreatic duct) with subsequent mechanical intra- and extrahepatic cholestasis. Cholestasis occurs due to tension and compression of the common bile duct by the diaphragmatic clamp resulting in dilated intra- and extrahepatic bile ducts with temporally elevated liver enzymes and cholestasis parameters. Clinical symptoms can vary from mild obstructive jaundice up to serious organic and systemic damage. A complete literature review and the decision finding process in the treatment of our patient are presented.
CASE REPORT
A 72-year-old Caucasian woman was admitted to the hospital with symptoms of mechanical cholestasis such as mild jaundice, pruritus, diarrhea and fatigue. Several months before, she had already suffered from mild epigastric pain, rated as three out of ten on the numeric rating scale. Her abdominal examination was unremarkable with audible bowel sounds, no epigastric tenderness and no palpable masses. A stool test for occult blood was negative. Laboratory studies revealed a complete blood count within normal limits and normal electrolytes except gamma-glutamyl transpeptidase (G-GT) of 382 U/L [normal adult female range (NAFR): 0-45 U/L, serum glutamic-pyruvic transaminase (GPT) of 96 U/L (NAFR: 0-48 U/L), alkaline phosphotase (AP) of 153 U/L (NAFR: 20-125 U/L) and amylase of 153 U/L (NAFR: < 110 U/L)]. Cholinesterase, bilirubin and lipase were within normal limits on admission.
Her medical history was significant for hypertension, three-vessel coronary artery disease and cholecystolithiasis. In 1995 she underwent definitive resection arthroplasty of the left hip because of an aseptic loosening followed by prosthetic joint infection. Her functional status was limited, with walking restricted to using a cane. In 2004 a total hysterectomy was performed. Neither a pulmonary disease nor a chest trauma was reported. Her current medication included Nifedipine, Amiloride, Hydrochlorothiazide, Acetylsalicylic acid and Simvastatin.
An upper gastrointestinal study (200 mL of soluble contrast) revealed an intrathoracic duodenum with delayed contrast passage. In the following esophagogastroduodenoscopy a prestenotic dilatation of the descending duodenum with no hemorrhage or mucosal damage was found. Microscopic examination of a biopsy specimen from the distal esophagus showed reflux esophagitis grade I without any evidence of fungal infection or Barrett’s metaplasia. Gastric specimen revealed Helicobacter pylori (H. pylori) associated gastritis. H. pylori eradication therapy was initiated.
Thoracic and abdominal computed tomography (CT) showed a HH type IV with displacement of the entire duodenum and proximal pancreas through the hiatal orifice into the posterior mediastinum (Figure 1A and B).
Figure 1.
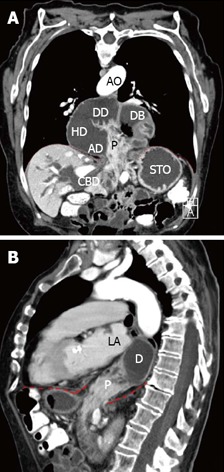
Computed tomographic scan obtained after oral administration of contrast. A: Frontal plane; B: Sagittal plane. The duodenum (D) lies dorsal to the atrial chambers. The descending duodenum is in immediate proximity to the left atrial (LA) chamber. The diaphragm is pointed out as the red dashed line. P: Head of pancreas; CBD: Common bile duct; STO: Stomach; DB: Duodenal bulb; DD: Descending duodenum; HD: Horizontal duodenum; AD: Ascending duodenum; AO: Aorta.
An intermittent mechanical intra- and extrahepatic cholestasis was present due to obstruction of the common bile duct caused by the compression of the right diaphragmatic pillar which served as a hypomochlion to the common bile duct (Figure 1A and B).
The endoscopic retrograde cholangiopancreatography revealed a stenosis about 3 cm proximal to the major duodenal papilla. An endoscopic papillotomy or the insertion of a stent was not necessary at this time because of normal bilirubin levels despite morphologic dilated intrahepatic bile ducts.
Our recommended elective surgical repair of the hernia was refused by the patient due to lack of symptoms. Therefore she was discharged from hospital with periodic aftercare in three month intervals.
The following laboratory tests revealed continuously increasing liver and pancreatic enzymes (GPT: 235 U/L, G-GT: 600 U/L, AP: 241 U/L, lipase: 61 U/L, amylase: 167 U/L). Bilirubin counts were within normal limits. On physical examination she denied any clinical symptoms.
One year later the patient was treated as an inpatient at our facility because of a dislocated distal, left-sided radius multifragment fracture. On the second day of hospitalization, she complained of sudden chest pain without radiation. Additional symptoms were mild dyspnoea, indigestion and nausea. The patient denied palpitations, sweating or anxiety. Our initial concern was that of the presentation of symptoms related to the HH. A cardiac workup based on her clinical symptoms and the history of a three-vessel coronary artery disease revealed a non-ST elevation myocardial infarction (NSTEMI) based on electrocardiogram changes and elevation of CK-MB to 85 [normal level (NL) < 25 U/L], CK of 999 (NL < 170 U/L) and troponin of 1.23 (NL < 0.03 mg/mL).
A percutaneous coronary intervention was performed and a left anterior descending artery stent placed. Thrombocyte aggregation inhibitor therapy was initiated. The distal radius fracture was treated conservatively with a forearm cast for six weeks. The patient had an uneventful recovery and was discharged for rehabilitation care. She still denied any significant abdominal symptoms.
One year after the diagnosis of a HH type IV and an eventful course, the patient was still opposing an elective surgical repair. Meanwhile G-GT level climaxed 2327 U/L. She still remained symptom-free.
Three months after the NSTEMI, the patient was admitted to the emergency room with a six day history of constant severe epigastric pain, vomiting, weight loss (
7 kg/mo) and jaundice. Within our diagnostic investigation a mechanical ileus and again a NSTEMI was diagnosed.
After passing a nasogastric tube with release of 1500 mL of bile stained fluid and infusion therapy to equate water and electrolyte balance the patient was prepared for surgery.
As expected the HH type IV was identified and found to contain the entire duodenum, pancreatic head and the common bile duct (Figure 2). The esophageal hiatus was dilated (10 cm in diameter) with no evidence of previous mechanical disruption.
Figure 2.
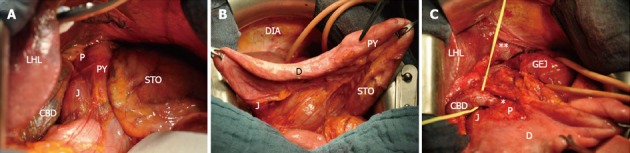
Intraoperative findings. A: After midline laparotomy; B: After reposition of the hiatal content; C: After closure with non-absorbable mesh. Asterisk indicates constriction of the common bile duct; Asterisks indicate closure of the esophageal hiatus with mesh and non-absorbable sutures. STO: Stomach; PY: Pylorus; J: Jejunum; CBD: Enlarged common bile duct; LHL: Left hepatic lobe; P: Pancreas; D: Duodenum; DIA: Diaphragm; GEJ: Gastroesophageal junction.
Manual reposition of the herniated content, excision of the thickened hernia sack and a cholecystectomy were performed without complications. The defect was augmented with interrupted non-absorbable sutures and mesh. The enlarged common bile duct was identified and released from adhesions and constrictions (Figure 2C).
After two days of an uneventful postoperative course with monitoring at the intensive care unit, the patient suffered disseminated intravascular coagulopathy with ischemia of the terminal ileum so that a re-laparotomy with right hemicolectomy and an ileotransversostomy became necessary. Extubation was possible after stabilization of the critical hemodynamic condition. Deterioration of general condition occurred shortly after on the intensive care unit with increased demand on catecholamine and the need for re-intubation. On day 20 after repair of the HH the patient developed increasing cardiac complaints with myocardial ischemia and cardiogenic shock, culminating in ventricular fibrillation and death.
DISCUSSION
The mechanisms and sources for diaphragmatic herniation of the pancreas remain unclear. Traumatic or iatrogenic diaphragmatic hernia (DH) are rare entities accounting for less than 1% of all DH[4].
Possible explanations are associated with congenital structural anomalies of the diaphragm or abdominal and thoracic organs like a persistent pneumoenteric defect, a failure of closure of the pleuroperitoneal canal like in Bochdalek’s hernia or a traction of a vascular pedicle by other organs as in PEH[1,5]. Congenital diaphragmatic hernia (CDH) occur with a prevalence between 1.7 and 5.7 per 10000 births and are classified in hiatal, posterolateral (Bochdalek), retrosternal (Morgagni) and transverse septum defect hernia[4]. Bochdalek´s hernia is the most common CDH type (95%). The remaining three types occur with an incidence of about 2% each.
Mullin et al[6] reviewed 13138 abdominal CT reports for incidental Bochdalek’s hernia in adults and identified 22 cases. Only one of the 13138 patients showed dislocation of the pancreas. Further cases of reported herniation of the pancreas as a Bochdalek’s hernia are described by Cuschieri et al[7] and Oliver et al[8]. One case reported by Moore et al[9] describes a herniated pancreas through the left-sided ventrolateral part of the diaphragm.
A hiatal herniation of the pancreas is a rarity. Our review of the literature yielded 11 reported cases with herniation of the pancreas or parts of it through the esophageal hiatus (Table 1). To the best of our knowledge we present the first case of a HH type IV containing the entire duodenum, head of pancreas and an intrathoracic duodenal papilla associated with intra- and extra-hepatic cholestasis.
Possible complications of a HH may result in hemorrhage, incarceration, obstruction, strangulation and perforation. Extrahepatic biliary obstruction as a complication of a HH with intrathoracic gastric volvulus is described by Llaneza et al[10]. In only one case the association of a myocardial infarction in patient’s history and a pancreatic HH is reported by Kafka et al[11]. Another interesting aspect is described by Chevallier et al[12] and Maksoud et al[13] pointing out that a hiatal herniation of the pancreas may remain reversible. Further cases in the published literature are described in Table 1[14-17]. Whether the patients were symptomatic or not, all described cases (Table 1) underwent surgical repair except one actual case reported by Rozas et al[2].
Historically, surgical repair was advocated for the treatment of patients with PEH (types II, III and IV HH) regardless of whether they had related symptoms. This approach stem from retrospective reports showing 30%-45% incidence of complications and mortality rates up to 50% among patients left untreated[18,19]. More recently, however, several authors have questioned the need for repair in truly asymptomatic patients[20]. Although our patient was asymptomatic, there were clear-cut signs (compression of the common bile duct) that warranted a surgical repair. Despite our recommendation of surgical hernia repair soon after the diagnosis, we had to respect the declared intention of the patient for a conservative procedure. The uniqueness of this case also supported this dilemma. So we were forced to wait for surgical repair within an emergency situation complicated by a myocardial infarction and reduced general condition.
Our case illustrates the serious sequelae of a HH type IV that can occur when treated conservatively and therefore we recommend that all HH type IV should be repaired as soon as possible after the diagnosis. Despite of the fatal outcome we were encouraged to publish this case to improve future decision finding processes in similar cases.
ACKNOWLEDGMENTS
We thank Professor Kai Matthes (Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, United States) for editorial assistance.
Footnotes
P- Reviewers Feo CV, Tseng YL S- Editor Gou SX L- Editor A E- Editor Lu YJ
References
- 1.Katz M, Atar E, Herskovitz P. Asymptomatic diaphragmatic hiatal herniation of the pancreas. J Comput Assist Tomogr. 2002;26:524–525. doi: 10.1097/00004728-200207000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Rozas MG, González MM. A rare complication of hiatal hernia. Gastroenterology. 2010;139:e1–e2. doi: 10.1053/j.gastro.2009.12.069. [DOI] [PubMed] [Google Scholar]
- 3.Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–616. doi: 10.1016/j.bpg.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eren S, Ciriş F. Diaphragmatic hernia: diagnostic approaches with review of the literature. Eur J Radiol. 2005;54:448–459. doi: 10.1016/j.ejrad.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Coral A, Jones SN, Lees WR. Dorsal pancreas presenting as a mass in the chest. AJR Am J Roentgenol. 1987;149:718–720. doi: 10.2214/ajr.149.4.718. [DOI] [PubMed] [Google Scholar]
- 6.Mullins ME, Stein J, Saini SS, Mueller PR. Prevalence of incidental Bochdalek’s hernia in a large adult population. AJR Am J Roentgenol. 2001;177:363–366. doi: 10.2214/ajr.177.2.1770363. [DOI] [PubMed] [Google Scholar]
- 7.Cuschieri RJ, Wilson WA. Incarcerated Bochdalek hernia presenting as acute pancreatitis. Br J Surg. 1981;68:669. doi: 10.1002/bjs.1800680922. [DOI] [PubMed] [Google Scholar]
- 8.Oliver MJ, Wilson AR, Kapila L. Acute pancreatitis and gastric volvulus occurring in a congenital diaphragmatic hernia. J Pediatr Surg. 1990;25:1240–1241. doi: 10.1016/0022-3468(90)90516-c. [DOI] [PubMed] [Google Scholar]
- 9.Moore TC. Esophageal hiatus hernia with obstructive incarceration of pylorus, pancreas, and duodenum. AMA Arch Surg. 1958;77:997–999. doi: 10.1001/archsurg.1958.01290050167031. [DOI] [PubMed] [Google Scholar]
- 10.Llaneza PP, Salt WB, Partyka EK. Extrahepatic biliary obstruction complicating a diaphragmatic hiatal hernia with intrathoracic gastric volvulus. Am J Gastroenterol. 1986;81:292–294. [PubMed] [Google Scholar]
- 11.Kafka NJ, Leitman IM, Tromba J. Acute pancreatitis secondary to incarcerated paraesophageal hernia. Surgery. 1994;115:653–655. [PubMed] [Google Scholar]
- 12.Chevallier P, Peten E, Pellegrino C, Souci J, Motamedi JP, Padovani B. Hiatal hernia with pancreatic volvulus: a rare cause of acute pancreatitis. AJR Am J Roentgenol. 2001;177:373–374. doi: 10.2214/ajr.177.2.1770373. [DOI] [PubMed] [Google Scholar]
- 13.Maksoud C, Shah AM, DePasquale J, Baddoura W, Spira R. Transient pancreatic hiatal herniation causing acute pancreatitis--a literature review. Hepatogastroenterology. 2010;57:165–166. [PubMed] [Google Scholar]
- 14.Saxena P, Konstantinov IE, Koniuszko MD, Ghosh S, Low VH, Newman MA. Hiatal herniation of the pancreas: diagnosis and surgical management. J Thorac Cardiovasc Surg. 2006;131:1204–1205. doi: 10.1016/j.jtcvs.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Tagaya N, Tachibana M, Kijima H, Kakihara Y, Hamada K, Sawada T, Kubota K. Laparoscopic treatment of paraesophageal hiatal hernia with incarceration of the pancreas and jejunum. Surg Laparosc Endosc Percutan Tech. 2007;17:313–316. doi: 10.1097/SLE.0b013e318059bf50. [DOI] [PubMed] [Google Scholar]
- 16.Coughlin M, Fanous M, Velanovich V. Herniated pancreatic body within a paraesophageal hernia. World J Gastrointest Surg. 2011;3:29–30. doi: 10.4240/wjgs.v3.i2.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967;53:33–54. [PubMed] [Google Scholar]
- 18.Hill LD, Tobias JA. Paraesophageal hernia. Arch Surg. 1968;96:735–744. doi: 10.1001/archsurg.1968.01330230043007. [DOI] [PubMed] [Google Scholar]
- 19.Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: operation or observation? Ann Surg. 2002;236:492–500; discussion 500-501. doi: 10.1097/00000658-200210000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gremmels JM, Broome DR, Fisher KL. Pancreatic herniation through the gastroesophageal hiatus: magnetic resonance imaging, magnetic resonance cholangiopancreatography, and computed tomography evaluation. J Comput Assist Tomogr. 2003;27:616–618. doi: 10.1097/00004728-200307000-00029. [DOI] [PubMed] [Google Scholar]


