Abstract
AIM
To evaluate the visual function after bilateral implantation of aspheric diffractive multifocal Tecnis ZMA00, aspheric monofocal ZA9003 versus spherical monofocal Akreos Adapt intraocular lenses (IOLs).
METHODS
Tecnis ZMA00, Tecnis ZA9003 or Akreos Adapt IOLs were bilaterally implanted in 180 eyes from 90 patients. The following parameters were assessed 3 months postoperatively: monocular and binocular uncorrected visual acuity (UCVA) and distance-corrected visual acuity (DCVA) for distance, intermediate and near, spherical aberration (SA), contrast and glare sensitivity, near point refractive power, uncorrected and best-corrected near stereoscopic acuity (NSA). Patient satisfaction was assessed by a questionnaire.
RESULTS
Three months postoperatively, the monocular and binocular UCVA and DCVA at near of Tecnis ZMA00 were significantly better than other two groups. The mean SA for 5.0mm optical zone in Tecnis ZMA00 and Tecnis ZA9003 was significantly lower than that in Akreos Adapt. Mean contrast sensitivity and glare sensitivity were better for Tecnis ZA9003 group than for other two groups. Patients with Tecnis ZMA00 had higher monocular and binocular near point refractive power and uncorrected NSA than monofocal groups. The patients in Tecnis ZMA00 had higher mean values for halo compared with other two groups.
CONCLUSION
Tecnis ZMA00 provided better near VA and uncorrected NSA and higher near point refractive power than monofocal IOLs and patients were spectacle independent. The IOLs with Tecnis aspheric design improved contrast and glare sensitivity. Patients with Tecnis ZMA00 reported more disturbances on visual phenomena of halo.
Keywords: intraocular lens, aberration, visual acuity, multifocal
INTRODUCTION
Advances in intraocular lens (IOL) design and surgical techniques have significantly improved the visual outcomes of cataract surgery. Traditional monofocal IOLs provide excellent visual acuity (VA). However, they have a fixed focal distance and limited depth of focus. Patients with monofocal IOLs lose most of their accommodation and usually require glasses for near vision.
The multifocal IOL was first introduced in the early 1980s and designed to provide simultaneous vision at both distance and near. These lenses, based on refractive or diffractive optics, can produce two or more foci according to the lens design. However, the distribution of incoming light to more than one focus results in reduced image contrast and unwanted visual phenomena, including glare and halos [1], [2].
The Tecnis ZMA00 multifocal IOL is an acrylic diffractive 3-piece lens. This multifocal IOL has a posterior full diffractive multifocal surface and an anterior modified prolate surface with Tecnis aspheric design, which neutralizes the negative impact of spherical aberration (SA) on vision. The aim of this aspheric design is to improve contrast sensitivity and visual function[3]-[8]. To our knowledge, few reports have discussed the visual performance of this particular IOL[9].
The purpose of this prospective study was to assess the visual performance after bilateral implantation of diffractive aspheric multifocal Tecnis ZMA00 IOLs and aspheric monofocal Tecnis ZA9003 IOLs with standard spherical monofocal Akreos Adapt IOLs as controls.
SUBJECTS AND METHODS
Subjects
This prospective study was of consecutive 90 patients who had bilateral implantation of a Tecnis ZMA00 IOL (30 patients), or a Tecnis ZA9003 IOL (30 patients) or an Akreos Adapt IOL (30 patients) as control at Eye Center, Second Affiliated Hospital, College of Medicine, Zhejiang University. Informed consent was obtained from all patients after the nature and possible consequences of the study were explained. Institutional Review Board approval was obtained and all patients provided informed consents.
Inclusion criteria were healthy eyes (except for cataract) with a potential VA of 20/40 or better, uneventful surgery, IOL implantation in the capsular bag, surgery in both eyes within 1 week, availability for all postoperative control examinations. Exclusion criteria included more than 1.50 diopter (D) of corneal astigmatism, a history of glaucoma or retinal detachment, corneal disease, previous corneal or intraocular surgery, abnormal iris, pupil deformation, macular degeneration or retinopathy, neurophthalmic disease, and history of ocular inflammation.
Intraocular lens characteristics
The Tecnis ZMA00 multifocal IOL is an acrylic diffractive 3-piece lens. The lens is designed to provide both near and far vision and thereby reduce spectacle dependence. The light distribution between the distance and near focus is approximately 50/50. The labeled power of the lens is the distance power. The near power represents a +4.0D add in actual lens power (approximately +2.8D in the spectacle plane). It has a full diffractive multifocal surface on the posterior side of the lens and a Tecnis modified prolate aspheric surface on the anterior side. The Tecnis ZA9003 monofocal IOL is an acrylic 3-piece lens with prolate aspheric design on the anterior surface. The Akreos Adapt is an acrylic spherical monofocal IOL and used as control. The characteristics of the three IOLs are listed in Table 1.
Table 1. Characteristics of IOLs implanted in patients.
| Tecnis ZMA00 | Tecnis ZA9003 | Akreos Adapt | |
| Manufacturer | AMO | AMO | Bausch and Lomb |
| Optics | Symmetric diffractive multifocal, aspheric | Monofocal, aspheric | Monofocal, spherical |
| Light distribution | 50% far focus, 50% near focus | 100% far focus | 100% far focus |
| Near add spectacle plane | 2.8D | 0 | 0 |
| Pupil dependence | No | No | No |
| Material | Acrylic | Acrylic | Acrylic |
IOL: Intraocular lens.
Methods
Surgical technique
One experienced surgeon (Prof. Yao K) performed sutureless phacoemulsification in all cases. After local or topical anesthesia was administered, a 3.0mm clear corneal incision was made. After complete hydrodissection, a continuous curvilinear capsulorhexis 5.0mm-5.5mm was created. The lens was removed and the posterior lens capsule polished. The capsular bag was refilled with the ophthalmic viscosurgical device (OVD) and the IOL was injected into the bag with a 3.0 injector. The IOL was centered in the capsular bag. The OVD was aspirated from the anterior chamber and capsular bag and from behind the IOL. IOL centration and haptic configuration were rechecked, and the anterior chamber was refilled with a balanced salt solution.
Standard examinations
Patients were scheduled for clinical evaluation preoperatively and postoperatively at 1 day, 1 week, 1 month and 3 months. A standard ophthalmologic examination was performed at all visits and included manifest refraction, slitlamp biomicroscopy and binocular indirect ophthalmoscopy.
Visual performance measurements
Visual performance was assessed 3 months postoperatively by the same ophthalmic technician. VA under photopic conditions (80 candelas [cd]/m2) was measured using decimal charts and then converted to logMAR units. Monocular and binocular uncorrected visual acuity (UCVA) and distance-corrected visual acuity (DCVA) were assessed using International visual testing chart at 30cm and 5m and using Colebrander mixed contrast visual testing chart at 63cm. Stereoscopic acuity was assessed with the Titmus stereo ring test.
Near point refractive power with the push-up test was measured monocularly and binocularly with the distance correction in place using the rule. Patients viewed the Slataper icon on the attached test chart with a +2.5D correction added to the test eye. The test chart was put on 40cm distance and moved toward the patient at approximately 2cm per second. The patient was instructed to keep the print clear for as long as possible and then indicate the point at which the print became blurred. The distance on the rule was noted. The near point refractive power (D) was calculated as the inverse of the near point (m) (minus +2.5D if near correction used). The near point was measured 3 times, and the 3 measurements were averaged [10].
Optical quality measures
Contrast sensitivity testing was assessed using a contrast glare tester (CGT-1000 Takagi Seiko). The CGT-1000 measures 12-step contrast thresholds using concentric ring-shaped visual targets that are equivalent to visual angles of 6.3, 4.0, 2.5, 1.6, 1.0, and 0.7 degrees at 0.35m. Contrast sensitivity is calculated as a logarithm of the inverse value of the contrast threshold. SA was measured for 3.0mm and 5.0mm optical zone using OPD Scan II Wavefront Aberrometer (Nidek, Japan).
Patient Questionnaire
A written 23-question survey assessing the lifestyle impact of IOL implantation was administered 3 months postoperatively. The content of this questionnaire has been used to assess functional visual outcomes after cataract surgery. The survey included questions about the visual difficulty of performing everyday tasks such as reading newspaper, using computer, cooking, watching television, shopping and so on. Patient satisfaction was based on questions about distance, intermediate, near and night vision. Patients rated satisfaction with their vision on a scale from 1 to 10 (absolutely dissatisfaction to absolutely satisfaction). Patients rated the incidence of visual disturbances (eg., halos, glare) on the following scale: 0=none; 1=a little; 2=moderate; 3=extreme. Patients also rated quality of vision on the following scale: 0=no difficulty; 1=a little difficulty; 2=moderate difficulty; 3=extreme difficulty; 4=I wear glasses to perform this activity.
Statistical Analysis
Comparisons were performed using the Student t-test for numerical variables and the Pearson chi-square test for categorical variables. Differences were considered to be statistically significant when the P value was less than 0.05. All tests were 2-sided with confidence level set at 95%. Data analysis was performed using SPSS for Windows software (version 12.0, SPSS, Inc.).
RESULTS
Ninety patients (180 eyes) ranging from 43 to 86 years were enrolled in this study. Table 2 shows the patients' demographics. There were no intraoperative complications. No eye had posterior lens capsule breakage or outward vitreous flow intraoperatively. One eye had mild cystoid macular edema 2 weeks after surgery, but the edema resolved at 1 month. No other complication was found within 3 months after surgery. All eyes had good IOL centration and no IOL tilt.
Table 2. Patients' demographics.
| Characteristic | Tecnis ZMA00 | Tecnis ZA9003 | Akreos adapt | P |
| Patients (n) | 30 | 30 | 30 | |
| Eyes (n) | 60 | 60 | 60 | |
| Sex (male/female) | 14/16 | 15/15 | 15/15 | NS |
| Mean age (a)±SD | 68.53±9.08 | 70.80±8.61 | 71.67±7.24 | NS |
Visual acuity
Table 3 shows the postoperative VA outcomes. No statistically significant differences were observed between these groups in either monocular or binocular VA at distance or intermediate. However, the patients with Tecnis ZMA00 had significant advantage in monocular UCVA and DCVA at near (mean logMAR 0.29±0.13, 0.27±0.11) than the patients with Tecnis ZA9003 (0.56±0.16, 0.59±0.16) and Akreos Adapt (0.58±0.13, 0.63±0.11) (P=0.000). The statistically significance also existed in binocular VA (P=0.000).
Table 3. Visual acuity (logMAR) in patients implanted with Tecnis ZMA00, Tecnis ZA9003 and Akreos Adapt IOLs bilaterally.
| Tecnis ZMA00 | Tecnis ZA9003 | Akreos adapt | P | |
| Monocular distance | ||||
| UCVA | 0.12±0.08 | 0.10±0.08 | 0.11±0.08 | NS |
| BCVA | 0.04±0.04 | 0.04±0.05 | 0.03±0.05 | NS |
| Monocular intermediate | ||||
| UCVA | 0.25±0.12 | 0.21±0.09 | 0.23±0.11 | NS |
| DCVA | 0.24±0.11 | 0.20±0.09 | 0.22±0.09 | NS |
| Monocular at near | ||||
| UCVA | 0.29±0.13 | 0.56±0.16 | 0.58±0.13 | 0.000 ZMA00 vs other groups |
| DCVA | 0.27±0.11 | 0.59±0.16 | 0.63±0.11 | 0.000 ZMA00 vs other groups |
| Binocular distance | ||||
| UCVA | 0.11±0.08 | 0.08±0.06 | 0.09±0.06 | NS |
| BCVA | 0.02±0.06 | 0.01±0.03 | 0.02±0.04 | NS |
| Binocular intermediate | ||||
| UCVA | 0.22±0.13 | 0.21±0.09 | 0.22±0.11 | NS |
| DCVA | 0.22±0.12 | 0.19±0.07 | 0.22±0.09 | NS |
| Binocular at near | ||||
| UCVA | 0.26±0.11 | 0.55±0.12 | 0.56±0.13 | 0.000 ZMA00 vs other groups |
| DCVA | 0.25±0.11 | 0.58±0.14 | 0.61±0.11 | 0.000 ZMA00 vs other groups |
IOL: Intraocular lens, UCVA: Uncorrected visual acuity, BCVA: Best-corrected visual acuity, DCVA: Distance-corrected visual acuity. Monocular, n=60; Binocular, n=30.
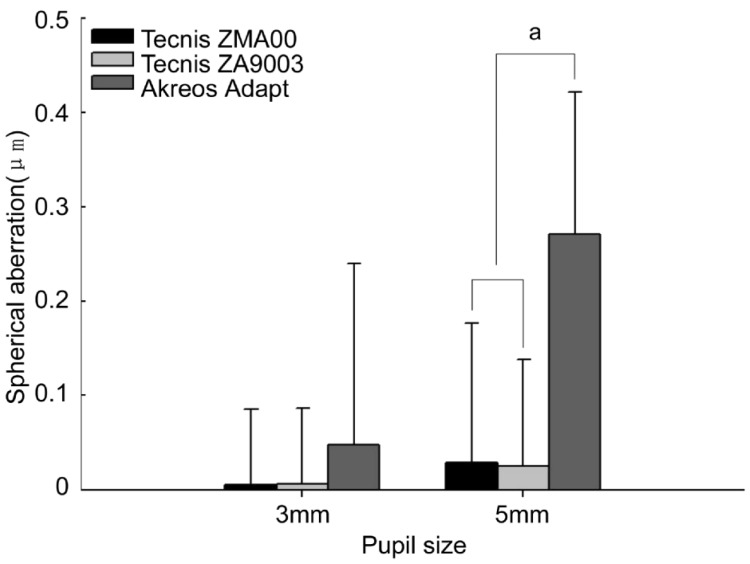
Spherical aberration
The mean overall ocular SA coefficient [Z(4,0)] was measured for 3.0mm and 5.0mm aperture diameter, approximating the pupil diameter under photopic and mesopic/scotopic conditions (Figure 1). The mean SA coefficient was (0.005±0.080)µm, (0.006±0.081)µm and (0.048±0.192)µm for 3.0mm optical and (0.029±0.148)µm, (0.025±0.114)µm and (0.271±0.151)µm for 5.0mm optical zone in Tecnis ZMA00, Tecnis ZA9003 and Akreos Adapt respectively. The SA in Tecnis ZMA00 and Tecnis ZA9003 was significantly different from Akreos Adapt (P=0.000) for 5.0mm optical zone.
Figure 1. Spherical aberration (SA) for 3.0mm and 5.0mm aperture diameter.
aP <0.05, n=60.
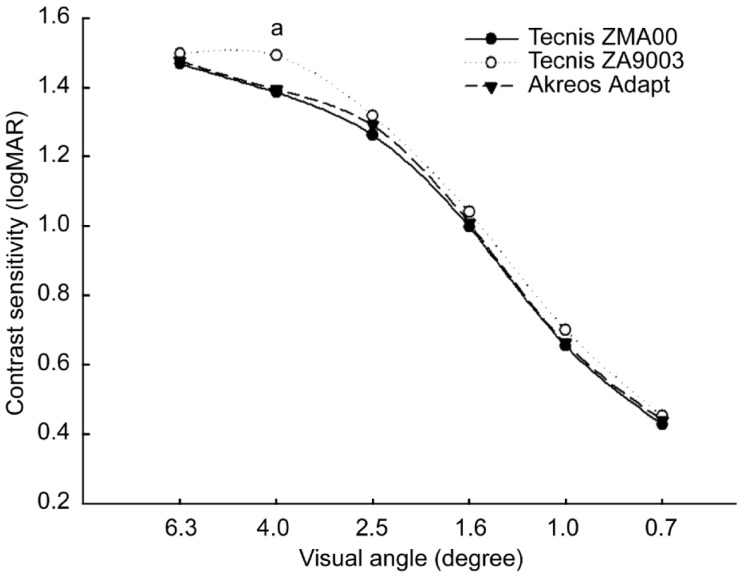
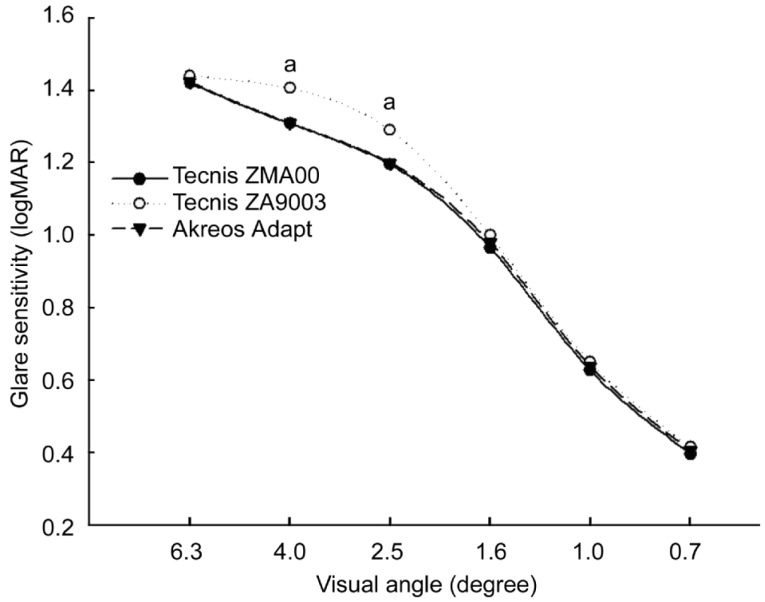
Contrast sensitivity and glare sensitivity
The results of contrast sensitivity testing at all visual angles are shown in Figures 2 and 3. On average, patients implanted with Tecnis ZA9003 showed better contrast sensitivity and glare sensitivity than those implanted with Tecnis ZMA00 and Akreos Adapt. Statistically significant differences were detected for contrast sensitivity on 4.0 degree (P=0.022, Tecnis ZA9003 vs Tecnis ZMA00; P=0.034, Tecnis ZA9003 vs Akreos Adapt) and glare sensitivity on 4.0 degree (P=0.033, Tecnis ZA9003 vs Tecnis ZMA00; P=0.035, Tecnis ZA9003 vs Akreos Adapt) and 2.5 degree (P=0.039, Tecnis ZA9003 vs Tecnis ZMA00; P=0.049, Tecnis ZA9003 vs Akreos Adapt). Few significant differences of contrast sensitivity and glare sensitivity were observed between Tecnis ZMA00 and Akreos Adapt.
Figure 2. LogMAR values of contrast sensitivity.
Patients with Tecnis ZA9003 showed better contrast sensitivity on 4.0 degree than those with Tecnis ZMA00 and Akreos Adapt. aP <0.05,n=60.
Figure 3. LogMAR values of glare sensitivity.
Patients with Tecnis ZA9003 showed better glare sensitivity on 4.0 and 2.5 degrees than those with Tecnis ZMA00 and Akreos Adapt. aP < 0.05,n=60.
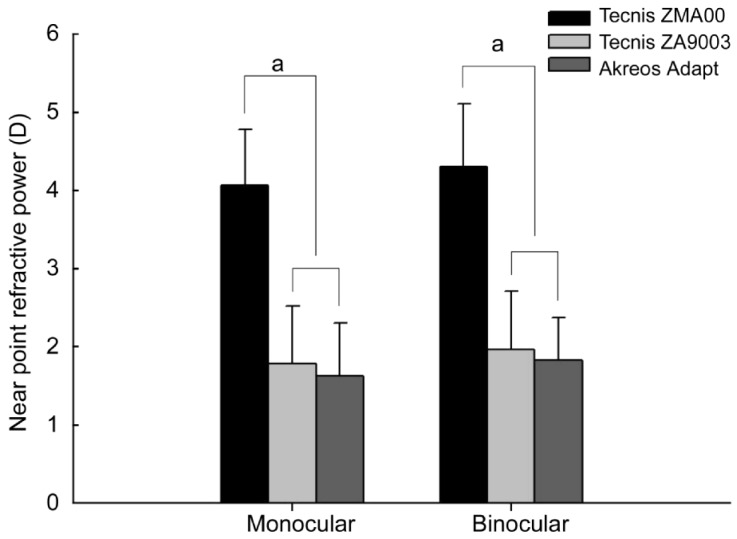
Near point refractive power
Figure 4 shows the monocular and binocular near point refractive powers with push-up methods in each group. The monocular near point refractive power was (4.07±0.71)D in Tecnis ZMA00, (1.79±0.74)D in Tecnis ZA9003 and (1.63±0.68)D in Akreos Adapt. There were significant differences between multifocal IOL and monofocal IOL (P=0.000, Tecnis ZMA00 vs Tecnis ZA9003 and Akreos Adapt). The binocular near point refractive power also showed the same significant difference between multifocal IOL and monofocal IOL.
Figure 4. Monocular and binocular near point refractive powers.
aP < 0.05. Monocular, n=60; Binocular, n=30.
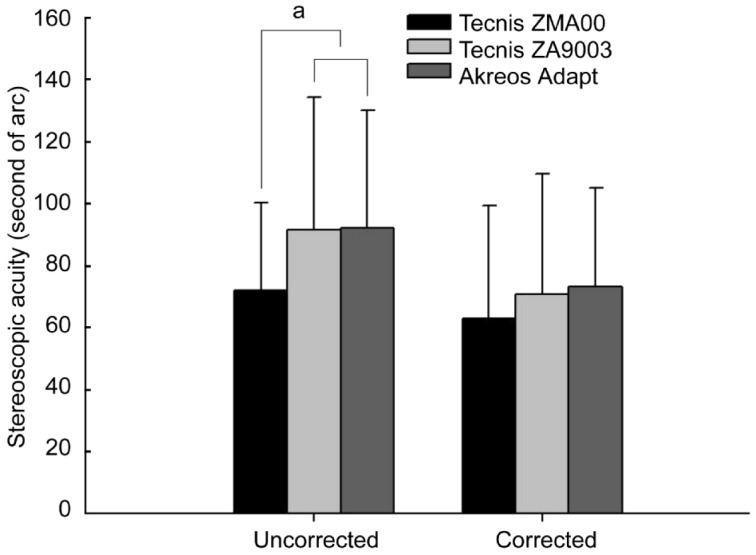
Stereopic acuity
Figure 5 shows the stereopsis results. The patients with Tecnis ZMA00 showed significantly better uncorrected near stereopic acuity (mean 72.0±28.3 seconds of arc) than the patients with Tecnis ZA9003 (mean 91.5±42.9 seconds of arc) and Akreos Adapt (mean 92.3±37.8 seconds of arc) (P=0.044, Tecnis ZMA00 vs Tecnis ZA9003; P=0.036, Tecnis ZMA00 vs Akreos Adapt). However, the beast-corrected near stereopic acuity had no significant difference between the three groups.
Figure 5. Uncorrected and best-corrected near stereopic acuity.
aP < 0.05, n=30.
Patient satisfaction and visual phenomena questionnaire
The patient satisfaction questionnaire (Table 4) shows that patients were satisfied with their vision (mean score 8.43±1.07 of Tecnis ZMA00; 7.97±1.47 of Tenics ZA9003; 7.87±1.53 of Akreos Adapt). Eighty percent of patients in the Tecnis ZMA00 group did not require glasses for near vision compared with 56.7% in the Tecnis ZA9003 group and 53.3% in the Akreos Adapt group. The patients with Tecnis ZMA00 reported good performance in terms of distance, near and intermediate visual tasks, with little to no difficulties performing any specific task. Compared with patients with Tecnis ZA9003 and Akreos Adapt, the patients with Tecnis ZMA00 did better in reading small prints, newspaper, doing fine handwork, filling in a form and shopping. All patients rated halos and glare as none to moderate and the patients with Tecnis ZMA00 had higher mean values for halo compared with the other two groups. Only 17.8% of patients surveyed were drivers, and driving at daytime did not seem to be a problem. Driving at night and in rainy or foggy day was rated as none to moderate difficulty. The data referring to performing sports and driving was not large enough and lacked statistical significance. No patients reported severe visual phenomena.
Table 4. Results of patient satisfaction and visual phenomena questionnaire administered 3 months postoperatively.
| Question | Tecnis ZMA00 | Tecnis ZA9003 | Akreos adapt | P |
| How satisfied are you with your vision? | 8.43±1.07 | 7.97±1.47 | 7.87±1.53 | NS |
| Have you taken off your glasses? | 0.20±0.41 | 0.43±0.50 | 0.47±0.51 | 0.052 ZMA00 vs ZA9003 |
| (n/30) | (24/30) | (17/30) | (16/30) | 0.028 ZMA00 vs Akreos |
| How much difficulty do you have with… | ||||
| Night vision? | 0.40±0.50 | 0.37±0.49 | 0.33±0.48 | NS |
| Halo? | 0.73±0.78 | 0.30±0.60 | 0.30±0.53 | 0.011 ZMA00 vs other groups |
| Glare? | 0.50±0.78 | 0.27±0.45 | 0.30±0.60 | NS |
| Reading small prints? | 0.67±1.09 | 1.82±1.49 | 1.86±1.51 | 0.002 ZMA00 vs ZA9003 |
| 0.001 ZMA00 vs Akreos | ||||
| Reading newspaper? | 0.33±0.55 | 1.41±1.50 | 1.44±1.55 | 0.002 ZMA00 vs ZA9003 |
| 0.001 ZMA00 vs Akreos | ||||
| Reading posters? | 0.07±0.37 | 0±0 | 0.04±0.19 | NS |
| Identifying people? | 0±0 | 0.13±0.43 | 0.13±0.43 | NS |
| using a computer? | 0.29±0.47 | 0.55±0.93 | 0.50±1.24 | NS |
| Identifying streets and traffic signs? | 0.10±0.31 | 0.17±0.46 | 0.20±0.48 | NS |
| Seeing fence and stair? | 0.17±0.38 | 0.10±0.31 | 0.13±0.35 | NS |
| Seeing menu under mesopic condition? | 0.54±0.65 | 0.86±0.79 | 0.90±0.77 | NS |
| Fine handwork? | 0.41±0.59 | 1.17±1.15 | 1.06±1.14 | 0.017 ZMA00 vs ZA9003 |
| 0.043 ZMA00 vs Akreos | ||||
| Filling in a form? | 0.15±0.37 | 0.95±1.31 | 1.00±1.33 | 0.014 ZMA00 vs ZA9003 |
| 0.009 ZMA00 vs Akreos | ||||
| Performing leisure activities? | 0±0 | 0.26±0.93 | 0.32±0.95 | NS |
| Performing sports? | 0±0 | 0.50±0.58 | 0.40±0.55 | |
| Cooking? | 0.04±0.19 | 0.12±0.33 | 0.16±0.37 | NS |
| Watching TV? | 0.28±0.45 | 0.30±0.53 | 0.33±0.55 | NS |
| Shopping? | 0.07±0.25 | 0.38±0.56 | 0.48±0.63 | 0.020 ZMA00 vs ZA9003 |
| 0.002 ZMA00 vs Akreos | ||||
| Driving at daytime? | 0±0 | 0±0 | 0±0 | |
| Driving at night? | 0.86±0.69 | 0.83±0.75 | 0.75±0.50 | |
| Driving in rainy/foggy days? | 0.63±0.52 | 0.67±0.82 | 0.75±0.50 |
Scale for satisfaction with vision ranged from 1 to 10 (1=incapacitating; 10=excellent). Scale for taking off glasses was 0=yes; 1=no. Scale for halo and glare was 0=none; 1=a little; 2=moderate; 3=extreme. Scale for all other questions was 0=none; 1=a little; 2=moderate; 3=extreme; 4=I wear glasses. “Blank” of P value indicates the data was not large enough to be measured. n=30.
DISCUSSION
Multifocal IOLs alleviate the symptoms of presbyopia by providing functional near vision and increasing the depth of field of the eye. Depending on the diffractive or refractive design of multifocal IOLs, different visual outcomes are achieved at far and near distances. However, because of light distribution, many patients reported reduced contrast sensitivity and photic phenomena. The development of the prolate aspheric Tecnis IOL was a major step toward the reduction of ocular SA, resulting in improved visual function, particularly contrast vision. Tecnis multifocal IOL (AMO) is a second-generation diffractive multifocal IOL incorporating the aspheric IOL platform to counteract the negative impact of multifocal IOL design on contrast vision. Tecnis ZM900 is designed with silicone material and Tecnis ZMA00 is secondly designed with hydrophobic acrylic material. Previous studies have reported the visual quality of patients with its former design, Tecnis ZM900 [5]-[8],[11]. In this study, we evaluated the visual function of patients implanted with aspheric multifocal Tecnis ZMA00, compared with aspheric monofocal Tecnis ZA9003 and spherical monofocal Akreos Adapt.
In our prospective study, distance UCVA and DCVA were both good in all patients. However, regarding the results of UCVA and DCVA at near, the multifocal group had the best acuities monocularly and binocularly. The binocular UCVA and DCVA at near in the Tecnis ZMA00 group were logMAR 0.26±0.11 and logMAR 0.25±0.11, while the binocular UCVA and DCVA at near in the Akreos Adapt group were logMAR 0.56±0.13 and logMAR 0.61±0.11. The multifocal IOL had improved the near vision significantly without compromising distance vision. The importance of intermediate vision is growing because it encompasses most daily activities [12],[13]. Although the scores of monocular UCVA and DCVA at intermediate in the Tecnis ZMA00 group were a little lower than the other two monofocal IOL groups, there were no statistically differences between the three groups.
Several studies have reported that contrast sensitivity with a multifocal IOL is worse than with a monofocal IOL [1],[2],[14],[15]. The decreased contrast sensitivity with multifocal IOLs is explained by the multifocal IOL's division of the available light energy in the image between 2 or more foci. However, the loss of contrast sensitivity is somewhat different, maybe due to the effects of different technology (refractive or diffractive) and optical design and other types of ocular aberration. Traditional spherical IOLs have positive SA, resulting in a significant amount of SA in the pseudophakic eye following cataract surgery. The Tecnis aspheric IOLs are designed to produce negative SA, similar to that of the young crystalline lens. Our result of SA for the entire optical system was 0.005-0.006µm for 3.0mm pupil diameter and 0.025-0.029µm for 5.0mm pupil diameter in Tecnis aspheric IOLs, lower than spherical IOL. The Tecnis series of IOLs have aspheric, modified, prolate anterior surface, which neutralize the negative impact of SA on functional vision. Our previous study has confirmed that the contrast and glare sensitivity of patients with Tecnis ZA9000 IOLs were higher than those with conventional spherical IOLs [16]. In this study, it shows that the patients in the Tecnis ZA9003 group showed better contrast sensitivity and glare sensitivity at low and moderate spatial frequencies than those implanted with Tecnis ZMA00 and Akreos Adapt and no significant differences of contrast sensitivity and glare sensitivity were observed between Tecnis ZMA00 and Akreos Adapt. The results demonstrated the aspheric design of Tecnis somewhat improved the contrast and glare sensitivity, especially in multifocal IOLs.
It is well recognized the majority of patients after phacoemulsification with monofocal IOLs implantation have lost most of their accommodation, but some pseudophakic patients with monofocal IOLs still have good near VA with distance correction. This phenomenon is called pseudoaccommodation or apparent accommodation. Studies have reported about 0.8-1.0D of pseudoaccommodation existed in pseudophakic patients and it does not meet the requirements for near vision [17]. Compensating for this lack of accommodation is an important challenge. Multifocal and accommodating IOLs have been implanted to restore near vision. There are many methods of assessing the apparent accommodation in pseudophakic eyes. Subjective tests can be calculated from the push-up test or from defocus curves [18]. Multifocal diffractive IOLs have diffractive rings that equal different focus points. In this study, we used push-up test to assess the near point refractive power for clinical significance though it was not genuine accommodation by definition. The near point refractive power in the Tecnis ZMA00 group was 4.07D monocularly and 4.31D binocularly, higher than monofocal IOLs and accommodative IOLs (2.50-2.79D with push up test) as reported [19].
Binocular vision is an important and meaningful aspect of visual function. Multifocal IOLs provide a broad range of vision from far to near foci, which help to increase binocular vision [20],[21]. Stereopsis, the highest form of binocular vision, is the relative ordering of visual objects in depth in response to disparate stimulation of retinal elements. The results of the Titmus test in our study indicated that patients with Tecnis ZMA00 IOLs were more likely to perceive the stereopgrams positively than those with monofocal IOLs. Due to the +4 add power in the Tecnis ZMA00 IOL, the uncorrected near stereopic acuity of patients in Tecnis ZMA00 group was 72.0 seconds of arc, lower than macula stereopsis.
The Tecnis ZMA00 group had significantly better near vision than the other two groups, as it was particularly apparent from the visual phenomena questionnaire. On the questionnaire, 80% of patients with Tecnis ZMA00 reported total spectacle independence versus 56.7% with Tecnis ZA9003 and 53.3% with Akreos Adapt. Benefiting from good near vision, the patients with Tecnis ZMA00 performed better performance in near work than the patients in monofocal IOLs. The most frequent photic phenomenon reported by our patients was halos, which were caused by dispersed light energy. The patients with Tecnis ZMA00 rated the halos as none to moderate with a score of 0.73±0.78, significantly higher than the scores in the Tecnis ZA9003 group and Akreos Adapt group. Similarly, Mester et al[7] reported that 9 out of 23 patients with Tecnis ZM900 IOL implantation noticed halos that were not present before surgery. It seems to be inherent in multifocal IOLs as a result of the multiple images [2]. In fact, most patients with Tecnis ZMA00 were not disturbed and rated their night vision as no statistically significant difference with monofocal IOLs. Overall, patients were satisfied with their visual outcomes and Tecnis ZMA00 had the highest score of satisfaction.
The Tecnis platform IOLs had lower SA than Akreos Adapt. Tecnis ZA9003 showed the best contrast and glare sensitivity. The patients with Tecnis ZMA00 had better near VA and uncorrected near stereopic acuity and higher near point refractive power than monofocal IOLs and were spectacle independent. However, these patients had more complaints of visual disturbance, especially halo.
Footnotes
Foundation items: Zhejiang Key Innovation Team Project (No. 2009R50039); Doctoral Fund of Ministry of Education of China (No: 20100101120135); Key Lab Fund of Zhejiang Province, China (No. 2011E10006)
REFERENCES
- 1.Montés-Micó R, Alió JL. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg. 2003;29(4):703–711. doi: 10.1016/s0886-3350(02)01648-6. [DOI] [PubMed] [Google Scholar]
- 2.de Vries NE, Webers CA, Touwslager WR, Bauer NJ, de Brabander J, Berendschot TT, Nuijts RM. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi: 10.1016/j.jcrs.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Bellucci R, Scialdone A, Buratto L, Morselli S, Chierego C, Criscuoli A, Moretti G, Piers P. Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60AT intraocular lenses: A multicenter randomized study. J Cataract Refract Surg. 2005;31(4):712–717. doi: 10.1016/j.jcrs.2004.08.049. [DOI] [PubMed] [Google Scholar]
- 4.Maxwell WA, Lane SS, Zhou F. Performance of presbyopia-correcting intraocular lenses in distance optical bench tests. J Cataract Refract Surg. 2009;35(1):166–171. doi: 10.1016/j.jcrs.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 5.Cillino S, Casuccio A, Di Pace F, Morreale R, Pillitteri F, Cillino G, Lodato G. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology. 2008;115(9):1508–1516. doi: 10.1016/j.ophtha.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Martínez Palmer A, Gómez Faiña P, España Albelda A, Comas Serrano M, Nahra Saad D, Castilla Céspedes M. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: a prospective, randomized, controlled clinical trial. J Refract Surg. 2008;24(3):257–264. doi: 10.3928/1081597X-20080301-07. [DOI] [PubMed] [Google Scholar]
- 7.Mester U, Hunold W, Wesendahl T, Kaymak H. Functional outcomes after implantation of Tecnis ZM900 and Array SA40 multifocal intraocular lenses. J Cataract Refract Surg. 2007;33(6):1033–1040. doi: 10.1016/j.jcrs.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 8.Ye P, Yao K, Li X, Wu W, Huang X, Yu Y. Binocular clinical comparison study of Tecnis multifocal aspheric and monofocal spherical intraocular lenses. Zhonghua Yan Ke Za Zhi. 2010;46(7):625–630. [PubMed] [Google Scholar]
- 9.Hütz WW, Jäckel R, Hoffman PC. Comparison of visual performance of silicone and acrylic multifocal IOLs utilizing the same diffractive design. Acta Ophthalmol. 2012;90(6):530–533. doi: 10.1111/j.1755-3768.2010.01984.x. [DOI] [PubMed] [Google Scholar]
- 10.Yang Y, Yao K, Jiang J. Accommodation in pseudophakic eyes with monofocal posterior chamber intraocular lens. Zhonghua YanKe Zazhi. 1996;32(2):98–100. [PubMed] [Google Scholar]
- 11.Packer M, Chu YR, Waltz KL, Donnenfeld ED, Wallace RB, 3rd, Featherstone K, Smith P, Bentow SS, Tarantino N. Evaluation of the aspheric tecnis multifocal intraocular lens: one-year results from the first cohort of the food and drug administration clinical trial. Am J Ophthalmol. 2010;149(4):577–584. doi: 10.1016/j.ajo.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Blaylock JF, Si Z, Prescott C, Aitchison S. Intermediate optimization of vision with bilateral nonaspheric multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35(3):303–311. doi: 10.1016/j.jcrs.2008.10.042. [DOI] [PubMed] [Google Scholar]
- 13.Hütz WW, Eckhardt HB, Röhrig B, Grolmus R. Intermediate vision and reading speed with array, Tecnis, and ReSTOR intraocular lenses. J Refract Surg. 2008;24(3):251–256. doi: 10.3928/1081597X-20080301-06. [DOI] [PubMed] [Google Scholar]
- 14.Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: AcrySof ReSTOR apodized diffractive versus AcrySof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007;33(7):1244–1247. doi: 10.1016/j.jcrs.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 15.Ferrer-Blasco T, Montés-Micó R, Cerviño A, Alfonso JF, Fernández-Vega L. Contrast sensitivity after refractive lens exchange with diffractive multifocal intraocular lens implantation in hyperopic eyes. J Cataract Refract Surg. 2008;34(12):2043–2048. doi: 10.1016/j.jcrs.2008.06.046. [DOI] [PubMed] [Google Scholar]
- 16.Shentu X, Tang X, Yao K. Spherical aberration, visual performance and pseudoaccommodation of eyes implanted with different aspheric intraocular lens. Clin Experiment Ophthalmol. 2008;36(7):620–624. doi: 10.1111/j.1442-9071.2008.01856.x. [DOI] [PubMed] [Google Scholar]
- 17.Tsorbatzoglou A, Németh G, Máth J, Berta A. Pseudophakic accommodation and pseudoaccommodation under physiological conditions measured with partial coherence interferometry. J Cataract Refract Surg. 2006;32(8):1345–1350. doi: 10.1016/j.jcrs.2006.02.069. [DOI] [PubMed] [Google Scholar]
- 18.Wold JE, Hu A, Chen S, Glasser A. Subjective and objective measurement of human accommodative amplitude. J Cataract Refract Surg. 2003;29(10):1878–1888. doi: 10.1016/s0886-3350(03)00667-9. [DOI] [PubMed] [Google Scholar]
- 19.Cleary G, Spalton DJ, Marshall J. Pilot study of new focus-shift accommodating intraocular lens. J Cataract Refract Surg. 2010;36(5):762–770. doi: 10.1016/j.jcrs.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 20.Häring G, Gronemeyer A, Hedderich J, de Decker W. Stereoacuity and aniseikonia after unilateral and bilateral implantation of the Array refractive multifocal intraocular lens. J Cataract Refract Surg. 1999;25(8):1151–1156. doi: 10.1016/s0886-3350(99)00136-4. [DOI] [PubMed] [Google Scholar]
- 21.Mesci C, Erbil HH, Olgun A, Yaylali SA. Visual performances with monofocal, accommodating, and multifocal intraocular lenses in patients with unilateral cataract. Am J Ophthalmol. 2010;150(5):609–618. doi: 10.1016/j.ajo.2010.05.023. [DOI] [PubMed] [Google Scholar]