Abstract
AIM
To compare the outcomes of laser in situ keratomileusis (LASIK) performed with a femtosecond laser (Femtec, Technolas Perfect Vision GmbH, Germany) versus a mechanical microkeratome (Hansatome, Bausch and Lomb, USA) for the correction of myopia and astigmatism.
METHODS
In this retrospective study, patients who had undergone LASIK using the 80-kHz Femtec femtosecond laser were compared to age- and refraction-matched patients in whom the Hansatome microkeratome was used. Refractive and visual results 1 month and 3 months postoperatively, and complication rates were compared between the two groups.
RESULTS
A total of 280 eyes were analyzed (140 in each group). At 3 months postoperatively in the Femtec vs Hansatome group, spherical equivalent refraction was within ±1.00D of emmetropia in 140 vs 138 eyes (P=0.498), the cylinder was within ±0.50D in 137 vs 139 eyes (P=0.622), and the UDVA was 20/20 or better in 136 vs 137 eyes (P=0.724), respectively. There was no statistically significant difference in the complication rates between the two groups (P=0.099).
CONCLUSION
LASIK performed both with Femtec femtosecond laser and Hansatome microkeratome achieved satisfactory refractive and visual results at 3 months postoperatively, without significant differences in efficacy, safety, and complication rates between the two procedures.
Keywords: laser in situ keratomileusis, femtosecond laser, Femtec, microkeratome, Hansatome
INTRODUCTION
LASIK flap creation can be performed either by a mechanical microkeratome or a femtosecond laser. Currently, five femtosecond (FS) lasers are FDA-licensed for LASIK: Intralase (Abbott Medical Optics), VisuMax (Carl Zeiss Meditec AG), Femtec (Technolas Perfect Vision), Femto LDV (Ziemer Ophthalmic Systems AG), and Wavelight FS200 (Alcon Surgical). All FS laser systems use ultra-short laser pulses, and the interaction process for cutting the corneal tissue is based on photodisruption. However, significantly different technical details and clinical experience are have to be considered[1].
The flap creation process is different between the Femtec femtosecond laser and most mechanical microkeratomes including Hansatome. With the latter, the eye is fixed with a suction ring and the cornea is not applanated before the cut is made. During the cutting process, the cornea bulges out of the ring and is compressed by the moving applanation surface. The corneal cut is made with a moving blade. In this case, biomechanical parameters (e.g., corneal rigidity, total corneal thickness) can influence the parallelism and thickness of the flap. In addition, the suction of the femtosecond laser head is less than with a mechanical microkeratome, which is more comfortable for the patient[2].
Although several studies have compared LASIK outcomes with different mechanical microkeratomes to those with femtosecond lasers to treat myopia, to our knowledge the visual and refractive results, and complications of Femtec femtosecond laser are not reported previously[3],[4]. This paper is the first to compare the clinical results and complication rates of LASIK by Femtec femtosecond laser to Hansatome.
SUBJECTS AND METHODS
Subjects
In this study, the medical records of patients who underwent LASIK using Femtec 80Hz femtosecond laser and Hansatome mechanical microkeratome at Acibadem Maslak Hospital Eye Clinic from January 1, 2010 to December 31, 2011 were evaluated retrospectively. Femto-LASIK was reserved for patients with thin corneas, steep or flat corneas (K≤40D or K≥46D), high refractive errors, or patients with a preference for it. All patients have given informed consent.
The inclusion criteria was myopia of up to -10.00D, astigmatism of up to 6.00D, and a central corneal thickness of at least 500µm. The exclusion criteria were unstable refraction, a predicted stromal bed thickness <250µm, previous ocular surgery, suspicion of keratoconus, any ocular disease, systemic diseases that could alter the wound-healing process such as diabetes and connective tissue disorders, pregnancy and breastfeeding.
Methods
Preoperative assesment
Preoperatively, all patients had a full ophthalmologic examination that included measurement of uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), undilated and cycloplegic autorefraction (KR 8800, Topcon, Japan), manifest refraction, slit-lamp biomicroscopy, airpuff tonometry (CT-80, Topcon, Japan); corneal pachymetry (Tomey pachymeter, SP-3000, USA; Pentacam, Oculus, Germany); corneal topography (Pentacam; Allegro Topolyzer, WaveLight, Inc., USA); mesopic pupil measurement (Colvard pupillometer, Oasis, USA); and funduscopy.
Surgical technique
Three surgeons (CBC, MM, ABS) performed all the procedures. After topical anesthesia with 0.5% proparacaine hydrochloride (Alcaine, Alcon-Couvreur, Belgium), 5% povidone-iodine solution was applied to the skin and the conjunctiva, and a sterile surgical drape and an eyelid speculum were positioned.
In the Hansatome group, the Hansatome microkeratome was used to create the flap. The cutting head (160µm) and the suction rings (8.5mm or 9.0mm) depending on the white-to-white corneal diameter were selected.
In the Femtec group, customed FLAP procedure was used to create the flap, using the following parameters: superior hinge position, a flap diameter of 8.5-9mm depending on the white-to-white corneal diameter, an attempted flap depth of 120µm, centripetal spiral pattern, a bed energy level of 1100nJ, a rim energy of 2700nJ, a spot separation of 7.0µm in the bed and 3/6µm in the rim, a 105-degree rim cut angle, and a hinge arc angle of 60 degrees.
In both groups, once the flap was created with either method, it was raised with a spatula, the stromal bed was dried with a sponge, and the ablation was performed using the 400Hz Allegretto wave Eye-Q excimer laser (Wavelight, Germany) using a conventional treatment algorithm. The stroma was then rinsed with balanced salt solution and the flap was gently put back in place with a cannula. One drop of an antibiotic drop (Vigamox; 0.5% moxifloxacin hydrochloride ophthalmic solution, Alcon Laboratories, USA) was applied at the end of the procedure.
Postoperative management
Postoperatively, all patients used preservative-free artificial tears as needed and were instructed to apply topical antibiotic drops (Vigamox; 0.5% moxifloxacin hydrochloride ophthalmic solution) 3 times daily for 5 days. Prednisolone acetate 1% (Pred Forte, Allergan Westport, Co., Ireland) were used 5 times daily and tapered in 5 days.
Patients were examined at postoperative-day 1, and -months 1 and 3; UDVA, CDVA, and subjective refraction were measured. All complications were recorded. Safety and efficacy of the procedure were assessed 1- and 3- months postoperatively. Safety was defined as the ratio of postoperative CDVA to preoperative CDVA. Efficacy was defined as the ratio of postoperative UDVA to preoperative CDVA.
Statistical Analysis
Refractive and visual results at 1- and 3- months postoperatively, and complication rates were compared between the Femtec and Hansatome groups. Statistical analysis was performed using the SPSS 16.0 (SPSS, Chicago, USA) software. Visual acuity was converted to logarithm of the minimal angle of resolution (logMAR) from the decimal notation for statistical analysis, using a visual acuity conversion chart. Continuous data were expressed as the arithmetical mean±standard error. Statistical comparisons were made with the unpaired 2-tailed Student's t test. P≤0.05 was considered statistically significant. Complication rates were compared with Chi-square test.
RESULTS
Two hundred and eighty eyes (140 eyes in each group) of 140 patients were included in the study. There were 42 females and 28 males in the Femtec group, and 38 females and 32 males in the Hansatome group (P=0.609). The mean age was 31.34±0.85 (range 19-54) in the Femtec group and 31.24±0.76 (range 20-46) in the Hansatome group (P=0.930) (Table 1).
Table 1. Preoperative data of eyes in the Femtec group and the Hansatome group.
| Femtec (n=140) | Hansatome (n=140) | P | |
| Age (a) | 31.34±0.85 (19-54) | 31.24±0.76 (20-46) | 0.930 |
| Female/Male | 42/28 | 38/32 | 0.609 |
| Preop sphere (D) | -3.48±0.17 (0.00 ∼ -8.00) | -3.47±0.14 (-0.50 ∼ -7.75) | 0.955 |
| Preoperative cylinder (D) | -0.89±0.07 (0 ∼ -4.50) | -0.75±0.07 (0 ∼ -5.00) | 0.168 |
| Preoperative SE (D) | -3.92±0.17 (-0.75 ∼ -8.50) | -3.82±0.14 (-1.00 ∼ -7.75) | 0.659 |
| Preop BSCVA (decimal) | 1.0 | 1.0 | 1.000 |
SE: Spherical equivalent; BSCVA: Best spectacle corrected visual acuity.
The mean sphere, cylinder, and spherical equivalent preoperatively in the Femtec and Hansatome group are shown in Table 1. Preoperatively, there was no statistically significant difference between the Femtec group and the Hansatome group in the mean sphere, cylinder and spherical equivalent, respectively (P=0.955, P=0.168, and P=0.659).
The mean sphere, cylinder, and spherical equivalent at postoperative month 1 in the Femtec and Hansatome group are shown in Table 2. At 1 month postoperatively, there was no statistically significant difference between the Femtec group and the Hansatome group in the mean sphere, cylinder and spherical equivalent, respectively (P=0.677, P=0.761, and P=0.919).
Table 2. Visual and refractive results 1 month after LASIK in the Femtec group and the Hansatome group.
| Femtec (n=140) | Hansatome (n=140) | P | |
| Postop sphere (D) | -0.02±0.01 (-0.50 ∼ 0.25) | 0.02±0.01 (-0.75 ∼ 0.50) | 0.677 |
| Postop cylinder (D) | -0.04±0.01 (-0.75 ∼ 0) | -0.05±0.01 (-0.50 ∼ 0.00) | 0.761 |
| Postop SE (D) | -0.04±0.01 (-0.50 ∼ 0.25) | -0.04±0.01 (-0.75 ∼ 0.25) | 0.919 |
| Eyes within ±0.50D SE | 137 | 136 | 0.724 |
| Eyes within ±1.0D SE | 140 | 138 | 0.498 |
| Eyes within ±0.50D cylinder | 137 | 139 | 0.622 |
| Eyes with UDVA ≥20/20 | 137 | 135 | 0.502 |
| Eyes with UDVA ≥20/25 | 140 | 138 | 0.498 |
| Safety | 1.00±0.00 (1.00 ∼ 1.00) | 1.00±0.00 (1.00 ∼ 1.00) | 1.000 |
| Efficacy | 0.998±0.001 (0.9 ∼ 1.0) | 0.995±0.001 (0.8 ∼ 1.0) | 0.280 |
SE: Spherical equivalent; UDVA: Uncorrected distance visual acuity.
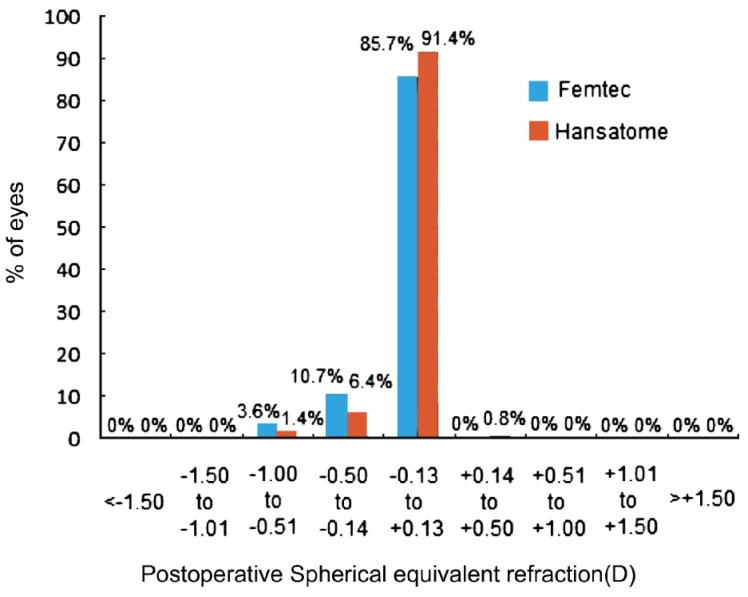
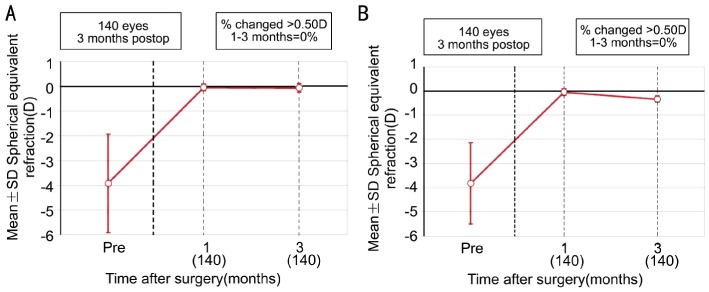
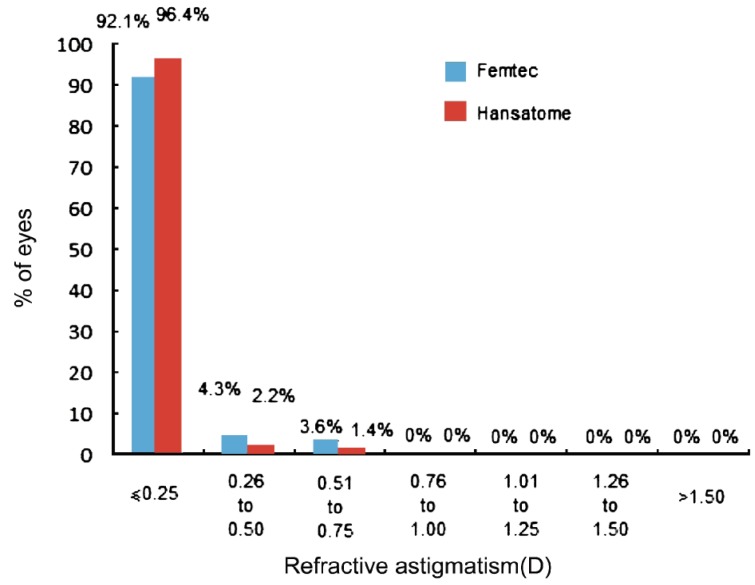
The mean sphere, cylinder, and spherical equivalent at postoperative month 3 in the Femtec and Hansatome group are shown in Table 3. At 3 months postoperatively, there was no statistically significant difference between the Femtec group and the Hansatome group in the mean sphere, cylinder and spherical equivalent, respectively (P=0.102, P=0.760, and P=0.129) (Figures 1–3).
Table 3. Visual and refractive results 3 months after LASIK in the Femtec group and the Hansatome group.
| Femtec (n=140) | Hansatome (n=140) | P | |
| Postop sphere (D) | -0.03±0.01 (-0.50 ∼ 0.25) | -0.01±0.01 (-0.75 ∼ 0.50) | 0.102 |
| Postop cylinder (D) | -0.05±0.01 (-0.50 ∼ 0) | -0.04±0.01 (-0.50 ∼ 0.00) | 0.760 |
| Postop SE (D) | -0.06±0.01 (-0.50 ∼ 0.00) | -0.03±0.01 (-0.75 ∼ 0.25) | 0.129 |
| Eyes within ±0.50D SE | 136 | 137 | 0.724 |
| Eyes within ±1.0D SE | 140 | 138 | 0.498 |
| Eyes within ±0.50D cylinder | 137 | 139 | 0.622 |
| Eyes with UDVA ≥20/20 | 137 | 135 | 0.502 |
| Eyes with UDVA ≥20/25 | 140 | 138 | 0.498 |
| Safety | 1.00±0.00 (1.00 ∼ 1.00) | 1.00±0.00 (1.00 ∼ 1.00) | 1.000 |
| Efficacy | 0.998±0.001 (0.9 ∼ 1.0) | 0.995±0.001 (0.8 ∼ 1.0) | 0.280 |
SE: Spherical equivalent, UDVA: Uncorrected distance visual acuity.
Figure 1. Spherical equivalent refractive accuracy at 3 months postoperatively in the Femtec grop and the Hansatome group.
Figure 3. Stability of spherical equivalent refraction after LASIK.
A: Femtec group; B: Hansatome group.
Figure 2. Refractive astigmatism at 3 months postoperatively in the Femtec group and the Hansatome group.
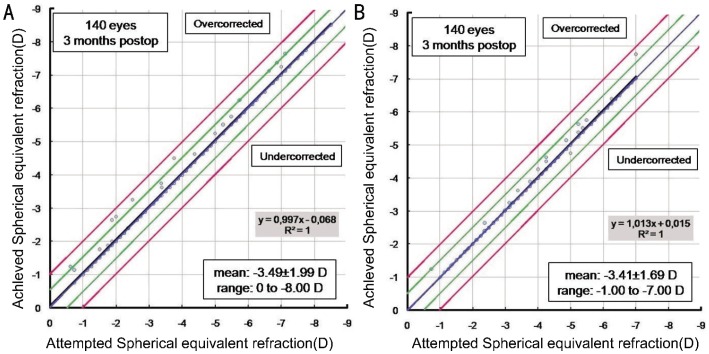
At 1 month postoperatively in the Femtec vs Hansatome group, spherical equivalent refraction was within ±0.50D of emmetropia in 137 vs 136 eyes (P=0.724), within ±1.00D of emmetropia in 140 vs 138 eyes (P=0.498), and the cylinder was within ±0.50D in 137 vs 139 eyes (P=0.622) (Table 2). At 3 months postoperatively in the Femtec vs Hansatome group, spherical equivalent refraction was within ±0.50D of emmetropia in 136 vs 137 eyes (P=0.724), within ±1.00D of emmetropia in 140 vs 138 eyes (P=0.498), and the cylinder was within ±0.50D in 137 vs 139 eyes (P=0.622) (Table 3). The relationship between acchieved and attempted correction in 2 groups at 3 months postoperatively in Figure 4.
Figure 4. Spherical Equivalent Attempted vs Acchieved at 3 months postoperatively.
A: Femtec group; B: Hansatome group.
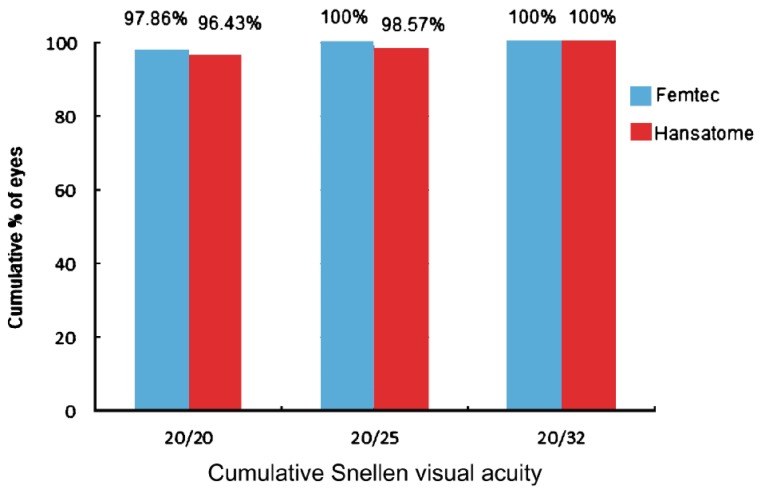
At 1 month postoperatively, the UDVA in the Femtec group vs Hansatome group were 20/20 or better in 137 of eyes vs 135 of eyes (P=0.502), and were 20/25 or better in 140 vs 138 eyes (P=0.498), respectively (Table 2). At 3 months postoperatively, the UDVA in the Femtec group vs Hansatome group were 20/20 or better in 137 vs 135 eyes (P=0.502), and were 20/25 or better in 140 vs 138 eyes (P=0.498), respectively (Table 3, Figure 5).
Figure 5. Uncorrected distance visual acuity at 3 months postoperatively in the Femtec group and the Hansatome group.
In the Femtec and Hansatome groups, at 1 month and 3 months postoperatively, no eyes lost any lines of Best spectacle corrected visual acuity (BSCVA). The safety of the procedure was 1.00±0.00 (range 1.00-1.00) at 1 month postoperatively and 1.00±0.00 (range 1.00-1.00) at 3 months postoperatively in both groups. The efficacy of the procedure in the Femtec group vs Hansatome groups was: 0.998±0.001 (range 0.9-1.0) vs 0.995±0.001 (range 0.8-1.0) at 1 month postoperatively and 0.998±0.001 (range 0.9-1.0) vs 0.995±0.001 (range 0.8-1.0) at 3 months postoperatively (P=0.280, P=0.280) (Tables 2, 3).
Minor flap adhesions occurred in 4 eyes (2.8%) in the Femtec group. Subconjunctival hemorrhages occured in 8 eyes (5.6%) in the Femtec group and 12 eyes (8.5%) in the Hansatome group. Peripheral, mild diffuse lamellar keratitis (DLK) occurred in 2 eyes (1.4%) in the Femtec group. Microstriae were noted in 1 eye (0.7%) on the first day after surgery in the Hansatome group; the microstriae had no further clinical implications and did not result in a loss of CDVA. A smoothing procedure was not performed. There was no statistically significant difference in the complication rates between the two groups (P=0.099) (Table 4).
Table 4. Complications in the Femtec and the Hansatome group.
| Femtec (n=140) | Hansatome (n=140) | P | |
| Minor flap adhesions | 4(2.8%) | 0 | 0.099 |
| Subconjunctival hemorrhages | 8(5.6%) | 12(8.5%) | |
| Mild DLK | 2(1.4%) | 0 | |
| Microstriae | 0 | 1(0.7%) |
DLK: Diffuse lamellar keratitis.
DISCUSSION
The femtosecond ophthalmic lasers are photodisruptive lasers with a pulse duration in the femtosecond (10–15) range. Photodisruption begins with laser-induced optical breakdown, when a strongly focused and short-duration laser pulse generates a high-intensity electrical field, thereby causing the formation of a mixture of free electrons and ions that constitutes the plasma state. The optically generated hot plasma expands with supersonic velocity and displaces surrounding material. As the plasma's expansion slows, the initial supersonic displacement propagates through the surrounding tissue as a shock wave. The rapid expansion of the generated plasma quickly decreases its temperature, and the vaporized tissue forms a cavitation gas bubble in the focal volume of the laser beam. The cavitation bubble consists mainly of CO2, N2, and H2O, which can diffuse out from the tissue through normal mechanisms. The ablation was found to be non-thermal due to the extremely short interaction time[5],[6]. In our study, we used Femtec femtosecond laser system with a wavelength of 1 040nm, pulse with of >500-fs, spot size of >1 micron, repetetion rate of 40 or 80kHz and a pulse energy of <1 microjoule.
There are many advantages of flap creation with a femtosecond laser. The incidence of complications like button-hole, epithelial abrasion, short flap, free cap, blade marks, and irregular cut are reduced with femtosecond lasers. There are greater options in flap diameter, flap thickness, side cut angle, hinge position and hinge length. There are no moving parts as in a microkeratome. The flap safety and flap thickness predictability are increased. The femtosecond lasers have the capability to cut thinner flaps. They cut planar flaps, in contrast with the meniscus-shaped flaps obtained with a mechanical microkeratome. Stromal hydration at the time of surgery has been shown to be lower after femtosecond flaps and that might influence refractive results[7],[8]. Additional advantages include stronger flap adherence and therefore less influence by trauma, fewer induced higher order aberrations, better contrast sensitivity, lesser need for retreatment, lesser rate of epithelial ingrowth, and lesser incidence of dry eye[9]-[13]. However, there are also some disadvantages of FS laser flap creation such as increased cost, larger physical size and lack of portability[2].
To our knowledge, this is the first paper comparing visual results, refraction, and complications of Femtec and a mechanical microkeratome in LASIK surgery, Pubmed revealed no references to it. In a comprehensive literature search and meta-analysis of Intralase femtosecond laser vs mechanical microkeratomes for myopia by Chen et al, fifteen articles describing a total of 3679 eyes were identified. No significant differences were identified between the two groups in regards to a loss of ≥2 lines of CDVA, patients achieving UDVA 20/20 or better, final UDVA, final mean refractive spherical equivalent, final astigmatism, or changes in high order aberrations. The IntraLase group had more patients who were within ±0.50D of target refraction compared to the microkeratome group, and flap thickness was more predictable in the Intralase group[3]. In our study, mean residual sphere, spherical equivalent, cylinder, UCVA and CDVA at 3 months postoperatively were not statistically different between the Femtec and Hansatome groups, so are the safety and efficacy.
There are some complications specific to femtosecond lasers. Cavitation gas bubbles are one of these complications. These bubbles confound the ability of the surgeon and the excimer laser eye tracker to locate the pupil. These bubbles can be moved away from the center by pushing with a cannula. Today, the bubble layer is decreased by the use of raster or centripetal spiral patterns, peripheral gutters evacuating the bubbles away from the center, and less energy level with faster firing rates[2]. Transient Light Sensitivity Syndrome (TLSS) is another femtosecond laser specific complication seen days/weeks after LASIK procedure. The visual acuity is good but there's increased ligt sensitivity. There's no positive finding in the clinical examination. It resolves in weeks with topical corticosteroids. The exact mechanism is unknown. However, it is believed to be due to biochemical response of the keratocytes to near-infrared laser energy or inflammatory response of the adjacent tissues to gas bubbles[14]. Rainbow glare is an optical side effect due to the light scattering from posterior surface of the interface is observed in 19% of Femto-LASIK patients. Visual acuity is not effected in most patients. The incidence of this complication has been decreased by the improvements in the focusing optics[15]. In our study, TLSS or rainbow glare were not observed.
Diffuse Lamellar Keratitis (DLK) was relatively common after initial FS laser surgeries. However, with the advent of faster firing systems, DLK incidence decreased. Today, DLK limited to the peripheral cornea, because of increased energy use for side cuts, is still encountered. This lamellar inflammation which is different from microkeratome related-DLK is believed to be the microscopic tissue damage aggrevated by ocular surface inflammatory mediators[16]. In Chen's systematic review and metaanalysis, the microkeratome group had more epithelial defects, whereas the IntraLase group had more cases of diffuse lamellar keratitis[3]. In our study, DLK was seen in 2 patients in the Femtec group and no epithelial defect was seen in both groups. Loss of vacuum by femtosecond laser is not as serious a problem as with the mechanical microkeratome. The vacuum ring can be reinserted and the flap could be recut. If loss of vacuum occurs during side cut, a smaller new cut is performed. Premature vacuum loss causes less change in the corneal shape with curved applanation systems[2]. We did not observe loss of vacuum in our patients. Minor flap adhesions by Femtec (2.8%) in our study might be due to the centripetal spiral pattern and/or high pulse energy used on Femtec.
In our study, Femto-LASIK was reserved for patients with thin corneas, steep or flat corneas, high refractive errors, or patients with a preference for it. So that, most complex cases were taken care by Femtec, which is beyond the ability of Hansatome. However, it is still fair to compare the two procedures in terms of refractive and visual results since these are the indications for femtosecond LASIK flap creation. Also, all studies in the literature comparing femtosecond lasers to mechanical microkeratomes have such patient selection criteria.
Since the follow up period in our study is short as 3 months, our patients are being followed up for refractive stability and any incidence of ectasia. In conclusion, LASIK performed both with Femtec femtosecond laser and Hansatome microkeratome achieved satisfactory refractive and visual results at 3 months postoperatively, without significant differences in efficacy, safety, and complication rates between the two procedures.
References
- 1.Lubatschowski H. Overview of commercially available femtosecond lasers in refractive surgery. J Refract Surg. 2008;24(1):102–107. doi: 10.3928/1081597X-20080101-18. [DOI] [PubMed] [Google Scholar]
- 2.Soong HK, Malta JB. Femtosecond lasers in ophthalmology. Am J Ophthalmol. 2009;147(2):189–197. doi: 10.1016/j.ajo.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 3.Chen S, Feng Y, Stojanovic A, Jankov MR, 2nd, Wang Q. Intralase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: a systematic review and meta-analyis. J Refract Surg. 2012;28(1):15–24. doi: 10.3928/1081597X-20111228-02. [DOI] [PubMed] [Google Scholar]
- 4.Zhang ZH, Jin HY, Suo Y, Patel SV, Montes-Mico R, Manche EE, Xu X. Femtosecond laser versus mechanical microkeratome laser in situ keratomileusis for myopia: Metaanalysis of randomized controlled trials. J Cataract Refract Surg. 2011;37(12):2151–2159. doi: 10.1016/j.jcrs.2011.05.043. [DOI] [PubMed] [Google Scholar]
- 5.Cosar CB, Sener AB. The FEMTEC laser in LASIK flap creation. CRS Today. 2004;2:27–29. [Google Scholar]
- 6.Cosar CB. LASIK flap creation with Femtec. In: Garg A, Alio JL, editors. Femtosecond Laser Techniques and Technology. New Delhi: Jaypee Brothers Medical Publishers Ltd; 2012. pp. 69–71. [Google Scholar]
- 7.Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical microkeratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(4):804–811. doi: 10.1016/j.jcrs.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 8.Durrie S, Kezirian GM. Femtosecond laser versus mechanical microkeratome flaps in wavefront-guided laser in situ keratomileusis: prospective contralateral eye study. J Cataract Refract Surg. 2005;31(1):120–126. doi: 10.1016/j.jcrs.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 9.Stahl JE, Durrie DS, Schwendeman FJ, Boghossian AJ. Anterior segment OCT analysis of thin IntraLase femtosecond flaps. J Refract Surg. 2007;23(6):555–558. doi: 10.3928/1081-597X-20070601-03. [DOI] [PubMed] [Google Scholar]
- 10.Kim JY, Kim MJ, Kim TI, Choi HJ, Pak JH, Tchah H. A femtosecond laser creates a stronger flap than a mechanical microkeratome. Invest Ophthalmol Vis Sci. 2006;47(2):599–604. doi: 10.1167/iovs.05-0458. [DOI] [PubMed] [Google Scholar]
- 11.Medeiros FW, Stapleton WM, Hammel J, Krueger RR, Netto MV, Wilson SE. Wavefront analysis comparison of LASIK outcomes with the femtosecond laser and mechanical microkeratomes. J Refract Surg. 2007;23(9):880--887. doi: 10.3928/1081-597X-20071101-03. [DOI] [PubMed] [Google Scholar]
- 12.Salomão MQ, Ambrósio R, Jr, Wilson SE. Dry eye associated with laser in situ keratomileusis: mechanical microkeratome versus femtosecond laser. J Cataract Refract Surg. 2009;35(10):1756–1760. doi: 10.1016/j.jcrs.2009.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Netto MV, Mohan RR, Medeiros FW, Dupps WJ, Jr, Sinha S, Krueger RR, Stapleton WM, Rayborn M, Suto C, Wilson SE. Femtosecond laser and microkeratome corneal flaps: comparison of stromal wound healing and inflammation. J Refract Surg. 2007;23(7):667–676. doi: 10.3928/1081-597x-20070901-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stonecipher KG, Dishler JG, Ignacio TS, Binder PS. Transient light sensitivity after femtosecond laser flap creation: Clinical findings and management. J Cataract Refract Surg. 2006;32(1):91–94. doi: 10.1016/j.jcrs.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Krueger RR, Thornton IL, Xu M, Bor Z, van den Berg TJ. Rainbow glare as an optical side effect of IntraLASIK. Ophthalmology. 2008;115(7):1187–1195. doi: 10.1016/j.ophtha.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Gil-Cazorla R, Teus MA, de Benito-Llopis L, Fuentes I. Incidence of diffuse lamellar keratitis after laser in situ keratomileusis associated with the IntraLase 15 kHz femtosecond laser and Moria M2 microkeratome. J Cataract Refract Surg. 2008;34(1):28–31. doi: 10.1016/j.jcrs.2007.08.025. [DOI] [PubMed] [Google Scholar]