Case History
In the year 2008, a 42 years old female presented to the medical outpatient with complaints of dyspepsia for 3 months with mild vague pain abdomen off and on. Her bowel and bladder habits were normal. She had no other associated comorbidity. She had no history of jaundice, malaena or haematemesis. There was no significant family history or past history. On clinical examination, she had moderate pallor and rest of the general and systemic examination was normal. Her routine blood investigations showed Hb% of 7.5 gm% and serum electrolyte, creatinine and LFT were within normal limits. She was advised ultrasound abdomen which was normal. Thereafter she was planned for Upper Gastrointestinal Endoscopy which was done and revealed a cauliflower like growth in the second part of the duodenum with stomach and esophagus being normal. Endoscopic biopsy was done which was reported as adenomatous polyp with no evidence of malignancy. CECT abdomen was done which showed duodenal growth with ? pancreatic head invasion and ampullary region was spared.
Patient was planned for exploratory laparotomy, frozen section and proceed. After two units of blood tansfusion for her anaemia, exploratory laparotomy was done and a growth was felt in second part of duodenum which was soft to firm in consistency. A dimpling was noted on the anterior wall of the second part of the duodenum and a small paraduodenal node found anterior to duodenum. Rest of the abdominal structures were normal.
Duodenotomy was done and excision of the duodenal polyp, which was about 5.5 × 5 × 2.5 cms, cauliflower like in appearance, was done. The ampulla was found to be normal. Frozen section was sent which was suggestive of adenomatous polyp with mild to moderate dysplastic changes and no evidence of malignancy and reactive lymphadenitis in the paraduodenal node hence, duodenoplasty performed and an abdominal drain kept in right subhepatic space and abdomen closed (Figs. 1 and 2).
Fig. 1.

Intraoperative view of the villous adenoma seen after duodenotomy
Fig. 2.

Scanner view showing stalk of the polyp with the overlying glands
Post-operative period was uneventful and the patient was discharged in good health on the tenth post-operative day. Final biopsy was of Villous adenoma of the duodenum. A repeat UGIE was done at 6 months and 1 year and then annually for 3 years and was found to be normal. In view of the high association of duodenal and colonic polyps, the patient was also advised colonoscopy, but did not agree. At present she is in follow-up and asymptomatic with good quality of life after 3 years follow-up (Figs. 3, 4 and 5).
Fig. 3.
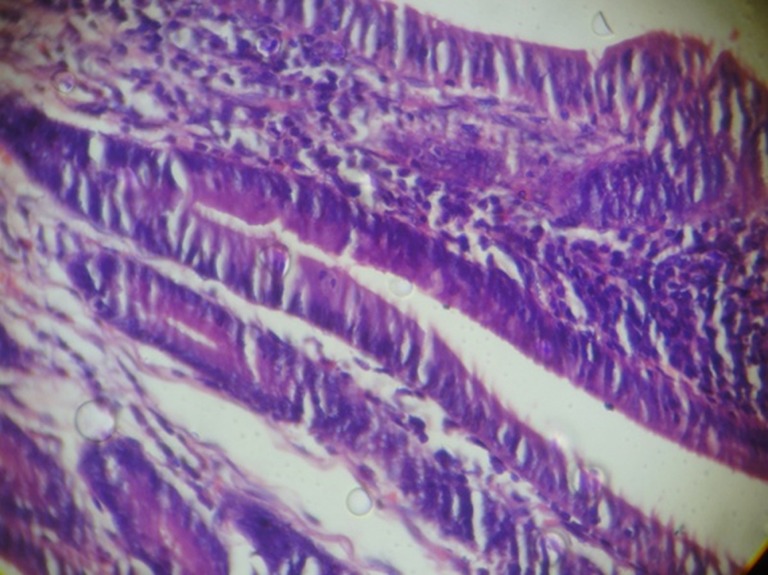
High power view showing glands with villous architecture with nuclear stratification and crowding in the glands without nuclear atypia or atypical mitosis
Fig. 4.
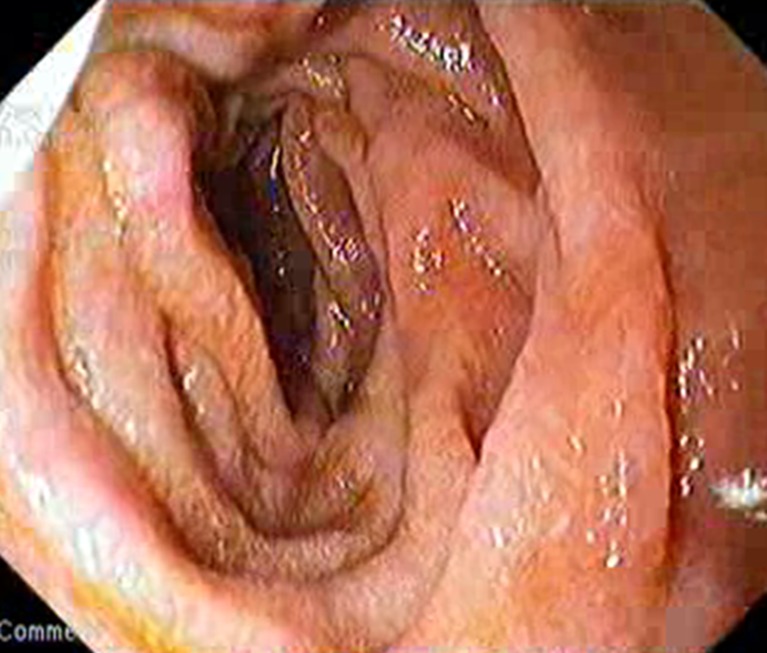
Endoscopic view of junction of first and second part of duodenum 2 years after surgery
Fig. 5.
Endoscopic view of second part of duodenum 2 years after surgery
Discussion
Villous tumor of the duodenum was first described in 1893 as a broad based mass. In 1928 the first definitive case of villous adenoma of the duodenum was published. Duodenum is the most common site of villous tumours of the small intestine but accounts for only 1 % of all duodenal tumours [1]. Despite being relatively rare, villous tumors of the duodenum (VTD) remain the most common benign periampullary neoplasm [2, 3]. VTD appear to behave in a manner similar to villous adenomas of the colon and rectum [2], but association of mucorrhea and electrolyte loss, often described with villous lesions of colon and rectum, has been reported only once with duodenal villous tumours [4]. The VTD are prone to bleed and may cause small intestinal obstruction [5–7]; in second part of the duodenum near the ampulla, they may also cause extrahepatic biliary obstruction that mimics choledocholithiasis or periampullary carcinoma [5, 8–10].
VTD possesses a high risk of malignant development [11, 12]. Carcinomatous changes occur in 30 to 60 % of duodenal villous adenomas and much less in tubulovillous and tubular adenomas [13]. Kutin et al. reported that no duodenal villous tumour under 4 cm in size showed evidence of invasive malignancy [14] but Schulten et al., Galandiuk et al. and Charles et al. found size to be a poor predictor of malignancy [5, 15, 16].
Although most cases of villous duodenal tumour are sporadic, these tumours also occur in patients with Gardner syndrome or familial adenomatous polyposis [17]. In cases of duodenal adenoma, there is an increased incidence of associated colorectal malignancy [18] and 20 times higher risk of concomitant colonic adenoma [19] as found in the study by Murray and colleagues and Apel and associates respectively in their study of patients from 1990 to 2003. This suggests that patients who have duodenal adenomas should undergo colonoscopy to determine whether a synchronous colonic neoplasm is present.
There is controversy in the most appropriate treatment of VTD. The treatment options available are endoscopic snare or ablation, local submucosal excision (with or without sphincteroplasty and pancreatic duct septotomy in case of periampullary VTD), full thickness excision, pancreas sparing duodenectomy and pancreaticoduodenectomy [17]. Regardless of the type of procedure, complete excision is mandatory [2]. Accurate preoperative histologic diagnosis is a problem in VTD because of the frequently large size of the lesion and the small sample taken via endoscopic biopsy forceps. Also the histologic evaluation at time of frozen section is associated with a high false-negative rate [16]. Recurrence of benign villous tumours after local excision is common and may be malignant [20]. Galanduik et al. reported a recurrence rate of 46 % in patients undergoing local excision [15], and 24 % of all recurrences were found to be adenocarcinomas in a recent study from Mayo Clinic [2]. In view of the biological behavior of VTD, pancreaticoduodenectomy is the procedure of choice in VTD with proved carcinoma, carcinoma in situ, severe dysplasia or in selected benign villous tumours specially if located near papilla in all medically fit patients [17]. Endoscopic treatment in the form of snare or photodynamic therapy and argon plasma coagulation should be reserved for patients who are not candidates for surgery, but require close follow up [21]. The justification for local excision of villous tumours of the duodenum is based on the presumed similarity to colorectal villous tumours which do not metastasize to lymph nodes until there is invasion of the muscularis mucosae. But in small bowel, mucosa contains lymphatics that course through the normal villi extending near the luminal surface. So, theoretically intramucosal carcinoma in villous duodenal adenoma may metastasize before invading the muscularis mucosae. Data to support this is inconclusive [16]. Endosonography combines endoscopy and ultrasound and localizes the gastrointestinal tumour by direct endoscopic location and assesses the submucosal extent of the target lesion and its surrounding structures by ultrasonic imaging, which may aid in better planning of treatment of VTD [22].
In our case, as the tumour was far away from the ampulla and the final histopathological report was also in favour of benign adenoma, no further surgery was done. In cases of local excision, with the pathology report suggestive of malignancy, revision surgery in the form of pancreaticouodenectomy should be done.
Contributor Information
Arunima Verma, Email: vermaarunima@yahoo.co.in, Email: dr.arunima@tatasteel.com.
Sunil Kumar, Email: drsunilkumar@tatasteel.com.
References
- 1.Herbsman H, Wetstein L, Rosen Y, et al. Tumours of small intestine. Curr Probl Surg. 1980;17:121–182. doi: 10.1016/S0011-3840(80)80018-9. [DOI] [PubMed] [Google Scholar]
- 2.Sakorafas GH, Friess H, Dervenis CG. Villous tumors of the duodenum: biologic characters and clinical implications. Scan J Gastroenterol. 2000;35:337–344. doi: 10.1080/003655200750023877. [DOI] [PubMed] [Google Scholar]
- 3.Witzigmann H, Möbius C, Uhlmann D, et al. Treatment concept of adenomas of Vater’s ampulla. Chirurg. 2000;71:196–201. doi: 10.1007/s001040050033. [DOI] [PubMed] [Google Scholar]
- 4.Weiss JB, Semerdijian GG. Recurrent villous adenoma of the duodenum. Gastroenterology. 1986;90:440–442. doi: 10.1016/0016-5085(86)90945-5. [DOI] [PubMed] [Google Scholar]
- 5.Schulten MF, Jr, Oyasu R, Beal JM. Villous adenoma of the duodenum. A case report and review of the literature. Am J Surg. 1976;132:90–96. doi: 10.1016/0002-9610(76)90297-X. [DOI] [PubMed] [Google Scholar]
- 6.Bremer EH, Battaile W, Bulle PH. Villous tumours of the upper gastrointestinal tract. Am J Gastroenterol. 1968;50:135–143. [PubMed] [Google Scholar]
- 7.Cohen A, McNeill D, Terz JJ, et al. Neoplasms of small intestine. Am J Dig Dis. 1971;16:815–824. doi: 10.1007/BF02239311. [DOI] [PubMed] [Google Scholar]
- 8.Mir-Madjlessi SH, Farmer RG, Hawk WA. Villous tumours of the duodenum and jejunum: report of four cases and review of literature. Am J Dig Dis. 1973;18:467–476. doi: 10.1007/BF01076597. [DOI] [PubMed] [Google Scholar]
- 9.Sobol S, Cooperman AM. Villous adenoma of the ampulla of Vater: an unusual cause of biliary colic and obstructive jaundice. Gastroenterology. 1978;75:107–109. [PubMed] [Google Scholar]
- 10.Griffen WO, Jr, Schaefer JW, Schindler S, et al. Ampullary obstruction by benign duodenal polyps. Arch Surg. 1968;97:444–449. doi: 10.1001/archsurg.1968.01340030104009. [DOI] [PubMed] [Google Scholar]
- 11.Hoyuela C, Cugat E, Veloso E, et al. Treatment options for villous adenoma of the ampulla of Vater. HPB Surg. 2000;11:325–331. doi: 10.1155/2000/86476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doi K, Iida M, Kohrogi N, et al. Villous adenoma of the duodenum in a patient with familial adenomatosis coli. Surg Endosc. 1995;9:512–4. doi: 10.1007/BF00206838. [DOI] [PubMed] [Google Scholar]
- 13.Adedeji OA, Trescoli-Serrano C, Garcia-Zarco M. Primary duodenal carcinoma. Postgrad Med J. 1995;71:354–358. doi: 10.1136/pgmj.71.836.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kutin ND, Ranson JHC, Gouge TH, Localio SA. Villous tumours of the duodenum. Ann Surg. 1975;181:164–168. doi: 10.1097/00000658-197502000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galandiuk S, Hermann RE, Jagelman DG, Fazio VW, Sivak MV. Villous tumours of the duodenum. Ann Surg. 1988;207:234–239. doi: 10.1097/00000658-198803000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chappius CW, Divincenti FC, Cohn I., Jr Villous tumours of the duodenum. Ann Surg. 1989;209:593–598. doi: 10.1097/00000658-198905000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aslan S, Cetin B, Markoc F, et al. A duodenal villous adenoma associated with in situ carcinoma: a case report. Turk J Cancer. 2001;31:162–167. [Google Scholar]
- 18.Murray MA, Zimmerman MJ, Ee HC. Sporadic duodenal adenoma is associated with colorectal neoplasia. Gut. 2004;53(2):261–265. doi: 10.1136/gut.2003.025320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Apel D, Jakobs R, Weickert U, et al. High frequency of colorectal adenoma in patients with duodenal adenoma but without familial adenomatous polyposis. Gastrointest Endosc. 2004;60(3):397–399. doi: 10.1016/S0016-5107(04)01712-2. [DOI] [PubMed] [Google Scholar]
- 20.Farnell MB, Sakorafas GH, Sarr MG, et al. Villous tumours of the duodenum: reappraisal of local vs extended resection. J Gastrointest Surg. 2000;4:13–21. doi: 10.1016/S1091-255X(00)80028-1. [DOI] [PubMed] [Google Scholar]
- 21.Saleem A, Wang KK, Baron TH. Successful endoscopic treatment of intraductal extension of a villous adenoma with high grade dysplasia, with 3-year follow-up. Gastrointest Endosc. 2011;74(3):714–716. doi: 10.1016/j.gie.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 22.Tio TL, Sie LH, Verbeek PCM, De Wit LT, Tytgat GNJ. Endosonography in diagnosing and staging duodenal villous adenoma. Gut. 1992;33:567–568. doi: 10.1136/gut.33.4.567. [DOI] [PMC free article] [PubMed] [Google Scholar]