Sir,
Lymph node metastases from adult soft tissue sarcomas (STS) are rare. They are frequently associated with certain histological subtypes which include angiosarcoma, embryonal rhabdomyosarcoma and epithelioid sarcomas. Therapeutic lymphadenectomy is considered appropriate treatment for isolated regional lymph nodes metastasis (RLNM) from STS and can potentially improve long-term survival [1]. The role of surgery in the presence of non regional lymph node metastasis is not clearly defined in literature.
A 19-year-old girl presented to us with a recurrent painless swelling in the right supraclavicular region for 4 months duration. She supposedly underwent a surgical excision for a similar swelling a year prior, elsewhere. Clinical examination confirmed the presence of a well circumscribed, multi-nodular swelling measuring 4 × 3cm in the right supraclavicular fossa, with involvement of the overlying skin; which had healed by secondary intention following the first surgery (Fig. 1). There were multiple significant discrete lymph nodes in bilateral cervical and right axillary regions. (Along levels II, III and IV on the right side and levels III and IV on the left side) Histopathology of the trucut biopsy from the supraclavicular swelling with immunohistochemistry correlation suggested a diagnosis of high grade malignant peripheral nerve sheath tumor (MPNST) (Figs. 2 and 3a–d). A PET-CT scan done for staging, showed metabolically active uptakes in the recurrent tumor in the supraclavicular fossa and in the multiple bilateral cervical and right axillary lymph nodes (Fig. 4).
Fig. 1.
Clinical photograph at presentation
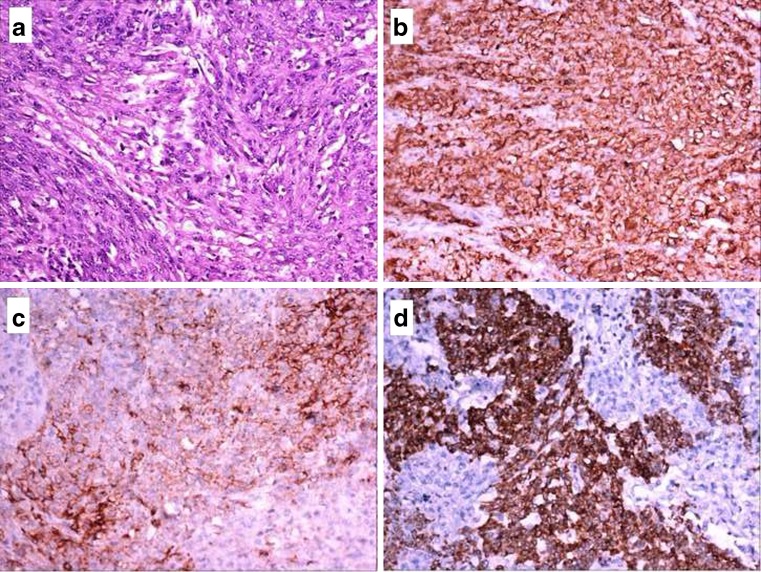
Fig. 2.
a. H&Ex20—Showing tumor arranged in sheets and vague fascicles composed of round, oval to spindle shaped cells having pleomorphic vesicular nuclei and prominent nucleoli, with peritheliomatous arrangement at certain areas. b IHCX20—Tumor cells showing immumopositivity to CD 57. c IHCX20—Tumor cells showing immumopositivity to CD 99. d IHCX20—Tumor cells showing immumopositivity to Bcl-2
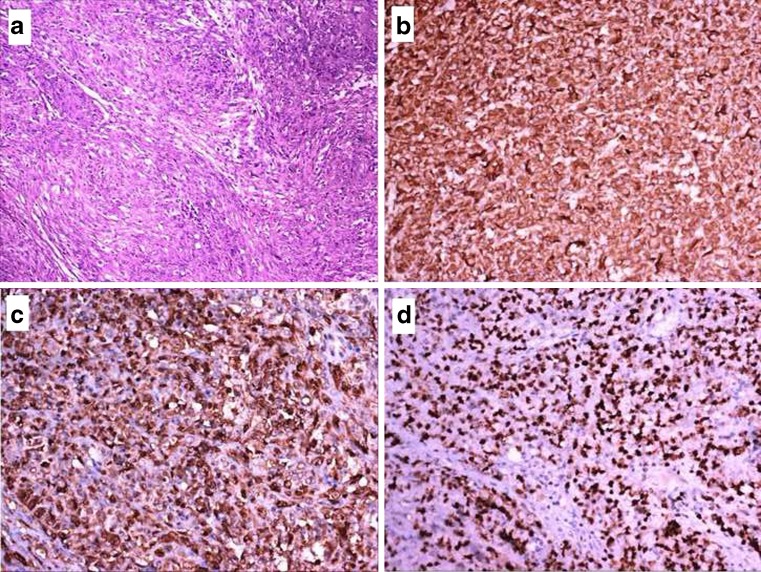
Fig. 3.
a H&Ex20—Showing tumor with epithelioid and spindle cell areas. b IHCX20—Tumor cells showing immumopositivity to vimentin. c IHCX20—Tumor cells showing immumopositivity to S-100p. d IHCX20—70 % of the tumor cells showing nuclear positivity to Ki-67
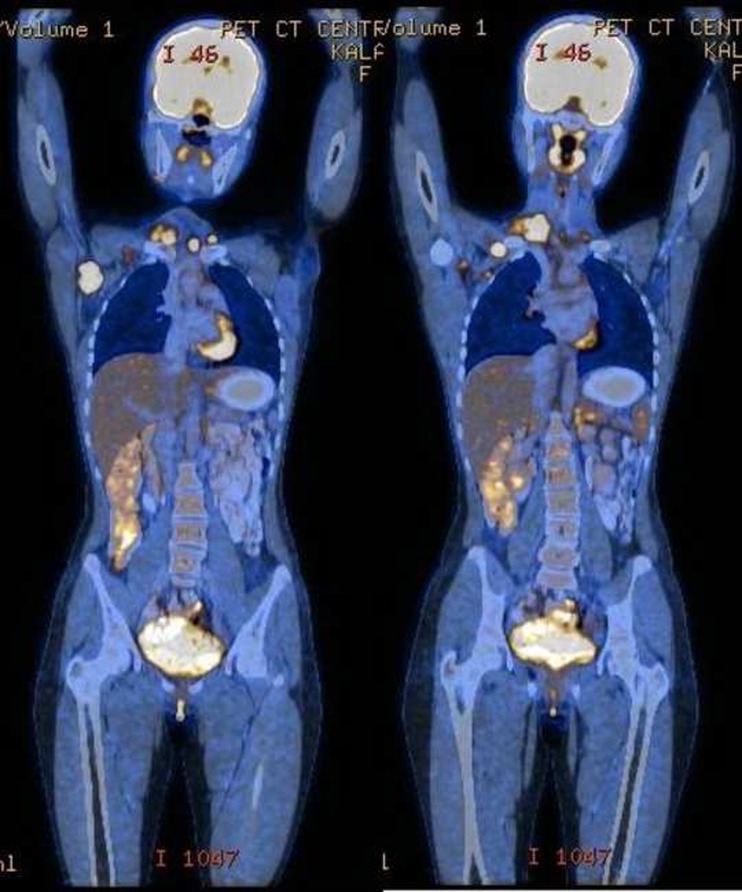
Fig. 4.
PET-CT scan showing metabolically active uptakes in the recurrent tumor in the supraclavicular fossa and in the multiple bilateral cervical and right axillary lymph nodes
The patient was taken up for a radical surgery; en-bloc excision of the recurrent tumor along with the overlying skin was done, safeguarding the truck of the brachial plexus. A bilateral selective neck dissection involving levels II to V and a complete right axillary clearance was done. The resultant skin and soft tissue defect in the right supraclavicular region was reconstructed using a right latissimus dorsi myocutaneous flap (Fig. 5a, b). The final histopathology confirmed the preoperative diagnosis of MPNST. 6 out of the 14 right sided cervical lymph nodes, 4 out of the 12 left sided cervical lymph nodes and 9 out of the 15 right sided axillary lymph nodes showed metastatic tumor deposits. The patient completed 60 Grey of adjuvant external beam radiotherapy to the tumor bed and is disease free for the past one and half years following surgery.
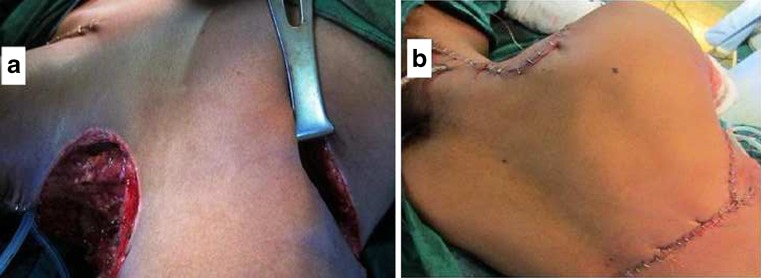
Fig. 5.
a Intra-operative photograph following the en-bloc resection of the tumor and the therapeutic cervical and axillary lymph node dissections. b Immediate post operative photograph following latissimus dorsi flap reconstruction
MPNST is currently the recommended term for all malignancies that arise from the peripheral nervous system or that show nerve sheath differentiation [2]. It is the sixth most common type and accounts for about 3–10 % of all STS [3]. Roughly half of all MPNSTs are sporadic; the remaining tumors are found in patients who are diagnosed with Neurofibromatosis Type I. These tumors commonly arise in the buttocks, thigh, brachial plexus, upper arm and para-spinal regions.
Clinically, these tumors are aggressive, locally invasive, and highly metastatic. The most common site of distant metastasis is the lung, followed by bone and pleura. RLNM are uncommon, occurring in <10 % of patients, and are mainly seen in conjunction with widespread metastasis. There is currently no standardized treatment for MPNST other than radical surgery even in the presence of RLNM [4]. Patients who present with isolated RLNM have an improved survival compared with patients who present with regional and distant metastasis at diagnosis.
Although routine use of FDG PET imaging as part of the initial staging of soft-tissue sarcomas is not recommended [5], it is reported to be useful in certain special circumstances as in our patient wherein the likelihood of distant metastasis was high. The absence of distant metastasis in the PET-CT prompted us to undertake a potentially curative surgery in our patient despite the presence of non regional lymph node metastasis; this case thus expands our knowledge on the biology of MPNST.
Acknowledgments
Competing interests
None declared
Funding
None
Ethical approval
Not required
References
- 1.Al-Refaie WB, Andtbacka RH, Ensor J, Pisters PW, Ellis TL, Shrout A, Hunt KK, Cormier JN, Pollock RE, Feig BW. Lymphadenectomy for isolated lymph node metastasis from extremity soft-tissue sarcomas. Cancer. 2008;112:1821–1826. doi: 10.1002/cncr.23363. [DOI] [PubMed] [Google Scholar]
- 2.Kolberg M, Høland M, Agesen TH, Brekke HR, Liestøl K, Hall KS, Mertens F, Picci P, Smeland S, Lothe RA. Survival meta-analyses for >1800 malignant peripheral nerve sheath tumor patients with and without neurofibromatosis type 1. Neuro Oncol. 2013;15:135–147. doi: 10.1093/neuonc/nos287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferner RE, Gutmann DH. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis. Cancer Res. 2002;62:1573–1577. [PubMed] [Google Scholar]
- 4.Godfrey GJ, Farghaly H. Lymph node metastasis of malignant peripheral nerve sheath tumor in the absence of widespread disease five years after diagnosis: a rare finding. Int J Clin Exp Pathol. 2010;3:812–814. [PMC free article] [PubMed] [Google Scholar]
- 5.Roberge D, Vakilian S, Alabed YZ, Turcotte RE, Freeman CR, Hickeson M. FDG PET/CT in initial staging of adult soft-tissue sarcoma. Sarcoma. 2012;2012:960194. doi: 10.1155/2012/960194. [DOI] [PMC free article] [PubMed] [Google Scholar]