Abstract
The Epworth Sleepiness Scale (ESS) was initially developed to measure daytime sleep propensity in patients affected by a variety of sleep disorders. Obstetrical research has measured sleepiness in pregnant women with the ESS, although a psychometric analysis and dimensionality evaluations have never been conducted with this population.
Objective
to perform a psychometric evaluation of the ESS in an obstetric population.
Design
secondary data analysis of subjects enrolled in the Prenatal Exposures and Preeclampsia Prevention III (PEPP) study.
Setting
subjects who received prenatal care at Magee-Women’s Hospital UPMC in Pittsburgh, Pennsylvania.
Participants
337 pregnant women in their first trimester who completed the ESS.
Methods
principal components analysis and confirmatory factor analysis were performed using SPSS and M-Plus. Additionally, reliability was assessed and construct validity was measured using the Life Orientation Test (LOT). Lastly, a relationship between daytime sleepiness and snoring was investigated using Item 5e from the Pittsburgh Sleep Quality Index (PSQI).
Results
PCA with varimax rotation yielded two factors that explained approximately 50% of the variance. CFA results verified the two-factor solution. An overall Cronbach’s alpha (0.751) revealed moderate reliability (Factor 1α = .754 ; Factor 2α = .524 ). Both convergent and discriminant validity were established.
Conclusion
The ESS is appropriate for use in an obstetric population to measure daytime sleepiness. Future work should include additional evaluations of the ESS in a diverse group of pregnant women.
Keywords: Epworth Sleepiness Scale, pregnancy, psychometrics, sleepiness, sleep, Confirmatory Factor Analysis, Exploratory Factor Analysis
Poor sleep is associated with devastating conditions in the obstetric population, including: preterm labor [1], hypertensive disorders [2], and gestational diabetes mellitus [3]. When compared with the general population, pregnant women are at a higher risk of developing sleep-related problems [4], likely due to physical and hormonal changes through pregnancy. Sleep disturbances are common among pregnant women and worsen during the pregnancy course [4]. The mechanism of these changes remains unknown and an accurate measurement of daytime sleepiness is needed to evaluate this phenomenon. The Epworth Sleepiness Scale (ESS) is an 8-item Likert-based instrument that has adequately measured daytime sleepiness in diverse populations [5-7]. The scale’s ease of use, low expense, and minimal time to complete make it an attractive option to measure sleep in both clinical and research populations. Although the ESS has been utilized to measure daytime sleepiness in both obstetrical and other clinical populations, the psychometric properties have not been examined in a sample of pregnant women.
BACKGROUND
Development of the Epworth Sleepiness Scale
The ESS was developed to quickly and conveniently measure daytime sleep propensity in populations suffering from a variety of sleep disorders [8]. The sleep disorders experienced by subjects in the development of this tool include: primary snoring, obstructive sleep apnea syndrome (OSAS), narcolepsy, idiopathic hypersomnia, insomnia and periodic limb movement disorder. Johns (1991) admits that, although the ESS does not “distinguish the nature of long-term physiological or pathological processes that produce a particular level of sleep propensity” (p. 544), it is capable of distinguishing normal subjects from patients suffering from OSAS, narcolepsy and idiopathic hypersomnia [8].
Prior to the development of the ESS, the Multiple Sleep Latency Test (MSLT) and the Maintenance of Wakefulness Test (MWT) were frequently used as objective, physiologic measures of sleepiness [9,10]. Despite the MSLT’s high test-retest reliability over periods of months [11], this test is burdensome, time-consuming and requires a polysomnographer. The Maintenance of Wakefulness Test, though capable of differentiating daytime wake tendencies from impaired wake tendencies, is costly [10].
The purpose of the development of the ESS was to provide a convenient, standardized and cost-effective way to measure sleep propensity in patients who suffer from sleep disorders [8]. Additionally, variability in daily routines is accounted for in this instrument, as frequency is not assessed (for example, not everyone sits and reads every day; however, nearly everyone can assess their likelihood of dozing when in this situation). The development of the ESS has provided a cost-effective, unobtrusive instrument that quickly and accurately assesses daytime sleepiness.
Prior Psychometric Evaluations
Since its development in 1991, the ESS has been administered to a variety of populations to determine its reliability. Overall, when measured in a sleep disturbed population, the reliability of the scale has been established in foreign languages ( α = .81 to .88) [12-16], and English-based studies ( α = .78 to .88) [17-19, 5]. When administered to populations not recruited from a sleep clinic, the reliability of the ESS is more variable, with Myotonic Dystrophy patients exhibiting the lowest internal consistency ( α = .24) [20] and Parkinsons’ patients providing the highest reliability score ( α = .84) [7].
The factor structure of the ESS has also been examined in a variety of populations. A Principal Components Analysis (PCA) of the ESS was included in Heaton’s (2007) evaluation of long-haul truck drivers [5]. PCA of the ESS was also performed using a sample of college students [21], patients with sleep disorders [18], and victims of Parkinson’s Disease [7]. Izci (2008), examined the dimensionality of a Turkish version of the ESS [16], and Johns (1992) and Johns (1994) performed factor analysis of the ESS in a group of patients with sleep disorders, but these studies did not describe the factor analytic method [19, 22]. Factor analyses of the ESS have yielded both one [14, 16, 19, 22] and two factors [21, 18, 7, 5]. Only one study, to our knowledge, has performed a Confirmatory Factor Analysis (CFA) with the ESS [17]. The examination of the ESS in OSAS patients resulted in a one-factor solution only when items 6 and 8 were deleted [17].
Use of ESS in Obstetric Population
Previous studies focusing on the obstetric population have utilized the ESS to measure daytime sleepiness. Mindell (2000) revealed that despite 67.2% of subjects reporting “moderate” to “very great” daytime sleepiness, no differences were found in ESS total scores throughout pregnancy [4]. Izci (2005) uncovered that among pregnant women who snore, ESS scores were higher, which indicated an increase in daytime sleepiness [23]. Despite the extensive use of the ESS in the obstetric population to examine quality of life [24] and risk of late stillbirth [25], the psychometric properties have not been explored using a sample of pregnant women.
PURPOSE
Psychometric evaluations of the ESS have been performed in a variety of populations with varied results. The wide variability among findings in clinical populations suggest that further exploration of the dimensionality of the ESS is needed to facilitate appropriate scoring. A psychometric evaluation of the ESS is necessary if pregnancy-related research aims to accurately measure sleep propensity in the obstetric population. This is especially vital since poor sleep is associated with pregnancy complications, including preterm labor [26] and gestational diabetes mellitus [27]. The purpose of this study was to assess the psychometric performance of the ESS in women who are in their first trimester of pregnancy (n=337).
METHODS
Sample and Parent Study (PEPP III)
This study was a secondary analysis of data collected through a larger project, Prenatal Exposures and Preeclampsia Prevention III (PEPP) study, which aims to better understand the role of obesity in the pathogenesis of preeclampsia, though subjects of all BMIs are invited to participate. The PEPP III study has recruited both longitudinal (before preeclampsia) and cross-sectional (preeclamptic or suspected preeclamptic) subjects, and remains an ongoing project through the Magee-Women’s Research Institute. Longitudinal subjects were recruited during the first trimester at a prenatal appointment at the WomanCare clinic at Magee-Womens Hospital. Subjects had a total of five study visits that occur during regularly scheduled appointments: 1) first trimester, 2) second trimester, 3) third trimester, 4) immediately postpartum and 5) 6-week postpartum clinic visit. PEPP III has been approved by the University of Pittsburgh’s Institutional Review Board (IRB), and all participating subjects signed an informed consent before any research procedures were performed. Additionally, approval to conduct this secondary analysis was obtained by the University of Pittsburgh’s IRB.
The sample for this analysis reflects only the longitudinal subjects who were recruited by the PEPP III study between January 2009 and September 2011 (n=337). Cross-sectional subjects with suspected preeclampsia were not included in this project, since these women delivered at different gestational ages and completion rates for the ESS were lower in this subgroup. Mindell (2000) reports no differences in the ESS scores throughout pregnancy [4]; thus, data from one time point during the first trimester was analyzed in this study. At this time point subjects completed, the ESS, Life Orientation Test (LOT) and Pittsburgh Sleep Quality Index (PSQI), among other questionnaires not included in this secondary analysis.
Instruments
Epworth Sleepiness Scale (ESS)
The ESS is a self-administered, eight-item questionnaire that takes 2-3 minutes to complete [22]. Items address daily lifestyle activities and the respondent is asked to rate their likelihood of dozing in each situation, from: “would never doze” (0) to “high chance of dozing” (3). The ESS provides a cumulative score between 0 and 24, with higher numbers indicating greater daytime sleepiness.
Life Orientation Test (LOT)
The Life Orientation Test measures general optimism versus pessimism with ten Likert-scaled items that range from “strongly disagree” (0) to “strongly agree” (4) [28]. This scale is designed to assess overall expectations for positive or negative outcomes [29] and is widely used in social and medical sciences, including obstetrics [30]. Reports of the scale’s reliability are mostly adequate but with large variability, ranging from α = .35 [31] to α = 0.85[32].
Pittsburgh Sleep Quality Index
Item five from the Pittsburgh Sleep Quality Index (PSQI) contains ten questions and measures nighttime sleep disturbances. Item 5e asks the subject to identify the frequency of trouble sleeping in the past month due to coughing or snoring (not during the past month, less than once a week, once or twice a week or three or more times a week). The PSQI has been shown to have high internal consistency ( α = .83) in clinical populations [33].
Statistical Analyses
Preliminary Analyses
Descriptive statistics were computed for the demographic variables and the percent of missing data was assessed. Distributions for each ESS item, PSQI (item 5e) and LOT score were examined with histograms and q-q plots. The Shapiro-Wilk test was used as a formal test for univariate normality for all items of each instrument used in the analysis. Potential multivariate outliers were assessed three ways: 1) scatterplots, 2) Mahalanobis Distance and 3) leverage values. The initial screening of data and Principal Components Analysis (PCA) were performed using Statistical Packages for the Social Sciences [34], while the confirmatory analyses were performed using MPLUS [35].
Principal Components Analysis
The inter-item correlation table was obtained to summarize the interrelationships among the eight items that comprise the ESS. The Keiser-Meyer-Olkin statistic (KMO) and Bartlett’s test of sphericity were obtained to ensure the suitability of factor analysis. KMO values of .6 indicated that a factor analysis was appropriate [35]. Communalities, the scree plot, total variance explained and eigenvalues were assessed along with factor loadings in order to determine factor structure. Factor loadings of greater than .32 were considered sufficient, while items with factor loadings of .32 or greater on more than one factor were considered cross-loading [37]. PCA was performed and both varimax and promax rotations were applied in one half of the sample (n=168). Varimax cross-loadings are reported, since this orthogonal rotation assumes uncorrelated factors and therefore provides a clearer picture of loadings [38]. Next, the emergent factor structure was tested using confirmatory techniques with the other half of the sample (n=169). In order to assess model fit, the Root Mean Square Error of Approximation (RMSEA) and Comparative Fit Index (CFI) were examined. RMSEA values of less than .05 and values higher than .90 for CFI were indicative of good model fit.
Reliability and Validity
The internal consistency of the ESS was assessed with Cronbach’s alpha to obtain: 1) an overall reliability, and 2) subscale reliabilities. Cronbach’s alpha levels of .80 or greater were considered acceptable since the ESS is an established instrument [39]. Data from a gold standard measure of daytime sleepiness were not available; therefore, a series of hypotheses were tested to further evaluate validity [40]:
The ESS subscale score(s) will be weakly and not significantly correlated with LOT scores, since these instruments measure different constructs. A weak r-value and nonsignificant p-value will reinforce that the LOT and ESS measure unrelated (discriminant) concepts. This hypothesis was tested using appropriate correlational techniques.
The ESS subscale score(s) will be positively correlated with Item 5e of the PSQI, which measures difficulty sleeping due to coughing or snoring. Previous studies have shown snoring is positively correlated with ESS scores in pregnant women [23]. Hypothesis 2 was tested by computing correlations between the ESS subscale(s) and item 5e of the PSQI.
RESULTS
There were no missing cases for the ESS data and missing data was less than 3% for the LOT questionnaire and Item 5e of the PSQI. The descriptives and analyses do not include data from eight subjects that were removed as influential multivariate outliers. Descriptives (Table 1) are reported for each analysis group. Sum ESS scores were similar between both groups and were consistent with previous findings that used the ESS in a pregnant population. The examination of the descriptives, box plots, histograms and q-q plots indicated that the items of the ESS, LOT and item 5e (PSQI) were non-normal.
Table 1.
Demographics
| PCA (n=168) | CFA (n=169) | |
|---|---|---|
| Mean age (years) | 23.92 | 24.7 |
| Race | ||
| African American (%) | 101 (60.1) | 96 (56.8) |
| Caucasian (%) | 61 (36.3) | 70 (41.4%) |
| Other (%) | 6 (3.5) | 3 (1.8) |
| Education | ||
| Less than H.S. (%) | 26 (15.5) | 25 (14.7) |
| H.S. Diploma/GED (%) | 60 (35.7) | 57 (33.7) |
| Some education after H.S. (%) | 50 (29.7) | 55 (32.5) |
| College/vocational degree/cert (%) | 26 (15.4) | 27 (15.9) |
| Graduate school/degree (%) | 4 (2.3) | 3 (1.8) |
| No answer (%) | 2 (1.2) | 2 (1.1) |
| Income | ||
| Less than $19,999 | 66 (39.3) | 70 (41.4) |
| $20,000 to $49,999 | 25 (14.9) | 39 (23) |
| $50,000 to $75,000 | 6 (3.6) | 7 (4.1) |
| Greater than $75,000 | 2 (0.6) | 7 (4.1) |
| Unsure/no answer | 56 (33.3) | 46 (27.2) |
| Mean ESS score | 7.17 | 7.24 |
Principal Components Analysis
Correlations from the inter-item correlation matrix ranged from r= 0.07 to r= 0.455. There were no correlations greater than 0.5, indicating no problems with multicollinearity [41]. The KMO of 0.788 indicated that the dataset was suitable for factor analysis. Additionally, Bartlett’s test of sphericity was significant (p<0.005); therefore it was appropriate to perform a factor analysis with this sample. Communalities, which quantify the amount of variance between items, ranged from 0.300 to 0.784.
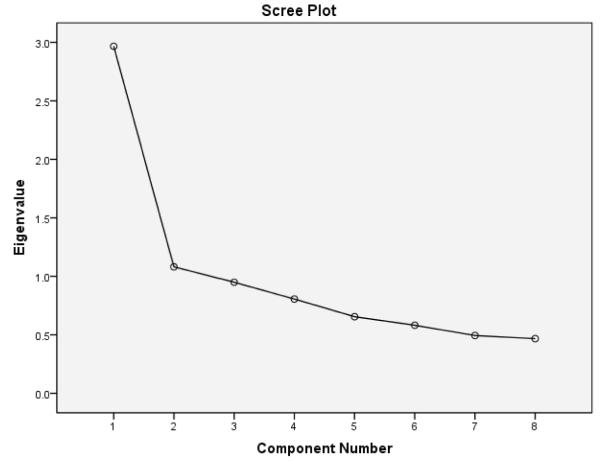
We uncovered a two-factor structure through the examination of the scree plot, eigenvalues, and factor loadings. These findings were similar to a previous factor analysis of the ESS [5]. An examination of the scree plot (Figure 1) revealed the possibility of two factors. Two factors had eigenvalues greater than one and explained 50.59% of the total variance (Table 2). Three items loaded onto factor one (items two, four and five) and two items loaded onto factor two (items six and eight). Items one and three, though technically cross-loading (greater than 0.32 on both factors), were most theoretically appropriate under factor one, for which the loading was higher (Table 2). Item seven (sitting quietly after lunch without alcohol) has nearly identical cross-loading values on both factors (0.492 and 0.497). Factor one is comprised of life situations in which dozing is socially acceptable, and factor two depicts life situations in which dozing is socially unacceptable.
Figure 1.
Scree plot
Table 2.
PCA Factor loadings and Total Variance Explained
| ESS Item | Factor 1 | Factor 2 |
|---|---|---|
| 1 – Sitting and reading | 0.576 | |
| 2 – Watching TV | 0.705 | |
| 3 – Sitting inactive in a public place | 0.497 | |
| 4 – As a passenger in a car for an hour without a break | 0.691 | |
| 5 – Lying down to rest in the afternoon | 0.747 | |
| 6 – Sitting and talking to someone | 0.886 | |
| 7 – Sitting quietly after lunch without alcohol | 0.492 | 0.447 |
| 8 – In a car, while stopped for a few minutes in traffic |
0.653 | |
| Total variance explained (%) = 50.592 | 37.078 | 13.514 |
Confirmatory Factor Analysis
In order to determine if the findings of the PCA were appropriate, we compared the two-factor model to a one-factor model of previous findings [14, 16, 19, 22] using confirmatory factor analysis. The indices of the two-factor model were compared to the indices of the one-factor solution. While both models yielded a good model fit, the two-factor solution produced a slightly better solution, with lower RMSEA and higher CFI indices (Table 3).
Table 3.
CFA Indices
| Structure | Chi Square | RMSEA | CFI |
|---|---|---|---|
| One factor | .055 | .975 | |
| Two factors | .049 | .981 |
Reliability
The overall Cronbach’s alpha of the ESS was very close to the recommended value for acceptable reliability of an established instrument [39], ( α = .751) . The reliability of factor one was also acceptable ( α = .743) , while the reliability of factor two was well below the acceptable level ( α = .524 ). As previously discussed, rotated factor loadings for item seven were similar for both factors. To determine the appropriate factor for this item, reliability was examined with and without item seven on the overall scale and on each factor. The resulting Cronbach’s alpha for the overall score without item seven ( α = .708 ) was less than when it was included in the overall score ( α = .751) . Additionally, the reliability of factor one was lower without item seven ( α = .706) . The reliability of factor two with item seven was lower than when item seven was omitted from factor two ( α = .488 and α = .524 , respectively). The results of the reliability analysis provided evidence that item seven should remain on factor one.
Validity
Hypotheses 1
As expected, the correlations between the emergent ESS subscales and the LOT scores were very low and nonsignificant. The correlation between Factor one (sleepiness in appropriate situations) and the overall LOT score was very weak (r =.094, p=.088), while the correlation between Factor two (sleepiness in inappropriate situations) and the overall LOT score was even lower (r= .075, p = .169). Additionally, the magnitude of the relationship between the overall score of the ESS and the overall LOT score was diminutive (r = .095, p = .084). Hypothesis 2: A significant and positive correlation was revealed between Factor two of the ESS (items six and eight) and item 5e (PSQI) (rs=.119, p=.031). The positive direction indicated that as trouble sleeping due to coughing or snoring increased, sleepiness in socially inappropriate situations increased.
DISCUSSION
There have been several previous psychometric evaluations of the ESS in various populations, but to our knowledge, none have assessed the validity or reliability in a sample of pregnant women. A previous evaluation of the ESS has revealed a potential gender bias, as women who report unrest are less likely than men to have an elevated ESS score >10 [42]. However, another study uncovered similar ESS scores between men and women [43]. This represents a dearth of information related to the performance of the ESS in specific clinical populations, including pregnant women. According to the Standards of the American Educational Research Association (1999) [40], it is the responsibility of the user of an instrument to justify its use, either by synthesizing prior evidence or by providing new supporting evidence. This study provided an overview of prior psychometric studies, and supplied new evidence obtained with a sample of obstetric patients.
Due to the conflicting results of prior factor analytic studies, it was our goal to determine the appropriate dimensional structure of the ESS when used in samples of pregnant women. Previous studies have reported both one and two factor structures. In order to score the ESS appropriately, the researcher must be familiar with the dimensionality of the instrument. Using an overall (unidimensional) score of a multidimensional instrument may result in a loss of information that could reflect an important characteristic of the population, and it could lead to incorrect inferences with consequential outcomes. Performing a PCA allowed us to uncover a preliminary structure that reflected two factors: sleepiness in appropriate situations and sleepiness in inappropriate situations. In order to justify and substantiate this finding, we performed a CFA and found this structure to be appropriate. These findings imply that future researchers should score the ESS in two parts. High scores on sleepiness in inappropriate situations could be an indication of further complication during pregnancy. Previous work has shown that sleepiness in pregnant women can be related to preterm labor [26] and gestational diabetes mellitus [27]; however, the relationships between these clinical characteristics and the factors of the ESS have yet to be explored.
Once the two-factor structure was confirmed, we continued to substantiate psychometric evidence by examining the reliability of the emergent subscales. The internal consistency of factor 1 was adequate; however, the internal consistency of factor 2 was below standard. The low Cronbach’s alpha of factor 2 ( α = .524) could be due to the limited number of items (n=2). The two items of factor two are related to situations in which sleeping is socially unacceptable. We recommend that more content relevant items representative of sleepiness in socially unacceptable situations be added to factor two.
Item seven (sitting quietly after lunch without alcohol) may be unclear to a population to which this scenario may not apply, and its inclusion illustrates the justification for psychometric testing of the ESS in an obstetric population. The wordage of this item within an obstetric population deserves further explanation, since only one out of eight pregnant women report alcohol consumption [44], a rate that is markedly lower than that of the general population. The inclusion of item seven does increase the reliability of factor one; therefore, we recommend when using the ESS with an obstetric population, item seven could be reworded to: “sitting quietly after lunch”. This wordage continues to measure postprandial doziness, yet considers the life experience common to this population.
The absence of data obtained from a gold-standard measure of daytime sleepiness led us to test a series of hypotheses in order to further establish the validity of the two subscales obtained from the ESS. The emergent subscales of the PCA were assessed in order to further substantiate the use of the two-factor structure. The LOT questionnaire and ESS subscales were very weakly correlated and non-significant, which supported hypotheses (1A) and (1B), respectively. The LOT questionnaire, which measures orientation to life situations as positive (optimistic) or negative (pessimistic), is not expected to be related to sleep propensity; therefore, this implies that both subscales of the ESS are measuring a different construct than the LOT. The significant relationship between factor two of the ESS and item 5e of the PSQI supports hypothesis (2). Izci (2005) reported a significant positive relationship between snoring and ESS scores among pregnant women in the third trimester [23]. Our findings support this relationship and suggest that this pattern may also exist in the first trimester. The significant correlation with only factor two during the first trimester supports a two-factor structure rather than a unidimensional scale, as dozing during socially unacceptable scenarios may be more common among sleepier subjects.
While these findings seem to support the use of a two-factor structure when using the ESS in a sample of pregnant women, some limitations to the current investigation should be addressed. A large proportion of our sample was African American (58.9%), which could skew the findings. Previous work has shown that African Americans score higher on the ESS and generally experience more sleepiness than Caucasians [45]. The relationship between ESS scores and race should be further investigated, as the larger sample of African Americans in our sample could have led to the emergence of factor two.
Other limitations of this study include the unavailability of parity status, as children in the home may impact sleep cycles and subsequent daytime sleep propensity; however, previous work has revealed that children at home did not significantly impact sleepiness [4] or sleep duration [46]. Additionally, depression symptoms, including fatigue, low energy, and lack of vigor may confound ESS scores [16], and employment status, which influence sleep patterns [47], were not investigated in this secondary analysis. Additionally, item 5e (PSQI) includes both snoring and coughing; however, only snoring has been associated with ESS scores [23], sleep disturbances [4] and pregnancy complications [23]. We were not able to delineate between the coughing and snoring effects to accurately conclude which is most related to daytime sleepiness in socially appropriate and inappropriate situations.
Conclusions
This is the first time the psychometric properties of the ESS have been examined in an obstetric sample. The performance of this instrument is generally consistent with previous evaluations of the ESS [5]. The findings of this investigation supply additional reliability and validity evidence for the ESS and provide evidence of a multidimensional, two-factor structure of the ESS when it is used as a measure of daytime sleep propensity in pregnant women. Further evaluation of this instrument is needed to investigate the relationships between the two factor structure with relevant demographic and clinical characteristics. Also, the structure should be confirmed in pregnant women at various stages of pregnancy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor’s list: Kelley Baumgartel, BSN Predoctoral fellow, Targeted Research and Academic Training Program for Nurses in Genomics, University of Pittsburgh, Pittsburgh, PA
Lauren Terhorst, PhD Assistant Professor and Statistician, University of Pittsburgh, Pittsburgh, PA
Yvette P. Conley, PhD Associate Professor of Nursing and Human Genetics, University of Pittsburgh, Pittsburgh, PA
James M. Roberts, MD Investigator, Magee-Women’s Research Institute and Professor of Obstetrics, Gynecology, Reproductive Sciences, Epidemiology, and Clinical and Translational Research, University of Pittsburgh, Pittsburgh, PA
References
- 1.Micheli K, Komninos I, Bagkeris E, et al. Sleep patterns in late pregnancy and risk of preterm birth and fetal growth restriction. Epidemiology. 2011;22(5):738–744. doi: 10.1097/EDE.0b013e31822546fd. [DOI] [PubMed] [Google Scholar]
- 2.Williams MA, Millers RS, Qiu C, Cripe SM, Gelaye B, Enquobahrie D. Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. Sleep. 2010;33(10):1363–1371. doi: 10.1093/sleep/33.10.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qiu C, Enguobahrie D, Frederick IO, Abetew D, Williams MA. Glucose intolerance and gestational diabetes risk in relation to sleep duration and snoring during pregnancy: a pilot study. BMC Womens Health. 2010;10:17. doi: 10.1186/1472-6874-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mindell J, Jacobson B. Sleep disturbances during pregnancy. JOGNN. 2000;29(6):590–597. doi: 10.1111/j.1552-6909.2000.tb02072.x. [DOI] [PubMed] [Google Scholar]
- 5.Heaton K, Anderson D. A psychometric analysis of the Epworth Sleepiness Scale. Journal of Nursing Measurement. 2007;15(3):177–188. doi: 10.1891/106137407783095748. [DOI] [PubMed] [Google Scholar]
- 6.Pahwa P, Karunanayake CP, Hagel L, et al. Prevalence of high Epworth Sleepiness Scale scores in a rural population. Can Respir J. 2012;19(2):e10–14. doi: 10.1155/2012/287309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagell P, Broman J. Measurement properties and hierarchical item structure of the Epworth Sleepiness Scale in Parkinson’s disease. J Sleep Res. 2007;16(1):102–109. doi: 10.1111/j.1365-2869.2007.00570.x. [DOI] [PubMed] [Google Scholar]
- 8.Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 9.Carskadon MA, Dement WC, Mitler MM, et al. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep. 1986;9(4):519–524. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 10.Doghramji K, Mitler MM, Sangal RB, et al. A normative study of the maintenance of wakefulness test (MWT) Electroencephalogr Clin Neurophysiol. 1997;103(5):554–562. doi: 10.1016/s0013-4694(97)00010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zwyghuizen-Doorenbos A, Roehers T, Schaeffer M, Roth T. Test-retest reliability of the MSLT. Sleep. 1988;11:562–565. doi: 10.1093/sleep/11.6.562. [DOI] [PubMed] [Google Scholar]
- 12.Bertolazi AN, Fagondes SC, Hoff LS, et al. Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J Bras Pneumol. 2009;35(9):877–883. doi: 10.1590/s1806-37132009000900009. [DOI] [PubMed] [Google Scholar]
- 13.Beiske KK, Kjelsberg FN, Ruud EA, Stavem K. Relability and validity of a Norweigian version of the Epworth Sleepiness Scale. Sleep Breath. 2009;13(1):65–72. doi: 10.1007/s11325-008-0202-x. [DOI] [PubMed] [Google Scholar]
- 14.Chen N, Johns M, Li H, et al. Validation of a Chinese version of the Epworth Sleepiness Scale. Quality of Life Research. 2002;11:817–821. doi: 10.1023/a:1020818417949. [DOI] [PubMed] [Google Scholar]
- 15.Kaminska M, Jobin V, Mayer P, et al. The Epworth Sleepiness Scale: self-administration versus administration by the physician, and validation of a French version. Can Respir J. 2010;17(2):e27–34. doi: 10.1155/2010/438676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Izci B, Ardic S, Firat H, et al. Reliability and validity studies of the Turkish version of the Epworth Sleepiness Scale. Sleep Breath. 2008;12(2):161–168. doi: 10.1007/s11325-007-0145-7. [DOI] [PubMed] [Google Scholar]
- 17.Smith SS, Oei TP, Douglas JA, Brown I, Jorgensen G, Andrews J. Confirmatory factor analysis of the Epworth Sleepiness Scale in patients with obstructive sleep apnoea. Sleep Med. 2008;9(7):739–744. doi: 10.1016/j.sleep.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 18.Violani C, Lucidi F, Robusto E, Devoto A, Zucconi M, Ferini-Strambi L. The assessment of daytime sleep propensity: a comparison between the Epworth Sleepiness Scale and a newly developed Resistance to Sleepiness Scale. Clinical Neurophysiology. 2003;114:1027–1033. doi: 10.1016/s1388-2457(03)00061-0. [DOI] [PubMed] [Google Scholar]
- 19.Johns M. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–381. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 20.Laberge L, Gagnon C, Jean S, Mathieu J. Fatigue and daytime sleepiness rating scales in myotonic dystrophy: a study of reliability. J Neurol Neurosurg Psychiatry. 2005;76(10):1403–1405. doi: 10.1136/jnnp.2004.043455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pilcher JJ, Pury CL, Muth ER. Assessing subjective daytime sleepiness: an internal state versus behavior approach. Behav Med. 2003;29(20):60–67. doi: 10.1080/08964280309596058. [DOI] [PubMed] [Google Scholar]
- 22.Johns M. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994;17:703–710. doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- 23.Izci B, Martin SD, Dundas KC, Wang LA, Calder AA, Douglas N. Sleep complaints: snoring and daytime sleepiness in pregnant and pre-eclamptic women. Sleep Med. 2005;6:163–169. doi: 10.1016/j.sleep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 24.Amador-Licona N, Gulzar-Mendoza JM. Daytime sleepiness and quality of life: are they associated in obese pregnant women? Arch Gynecol Obstet. 2012;295(1):105–109. doi: 10.1007/s00404-011-1879-9. [DOI] [PubMed] [Google Scholar]
- 25.Stacey T, Thompson JM, Mitchell EA, Ekeroma AJ, Zuccollo JM, McCowan LM. Association between maternal sleep practices and risk of late stillbirth: a case-control study. BMJ. 2011;342:d3403. doi: 10.1136/bmj.d3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okun ML, Schetter CD, Glynn LM. Poor sleep quality is associated with preterm birth. Sleep. 2011;34(11):1493–1498. doi: 10.5665/sleep.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reutrakul S, Zaidi N, Wroblewski K, et al. Sleep disturbances and their relationship to glucose tolerance in pregnancy. Diabetes Care. 2011;34(11):2454–2457. doi: 10.2337/dc11-0780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scheier MF, Carver CS. Optimism, coping and health: Assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 29.Vassar M, Bradley G. A reliability generalization study of coefficient alpha for the life orientation test. J Pers Assess. 2010;92(4):362–370. doi: 10.1080/00223891.2010.482016. [DOI] [PubMed] [Google Scholar]
- 30.Moyer C, Ekpo G, Calhoun C, et al. Quality of life, optimism/pessimism, and knowledge and attitutes toward HIV screening among pregnant women in Ghana. Womens Health Issues. 2008;18(4):301–309. doi: 10.1016/j.whi.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graci G. Optimism, health locus of control, and quality of life women with recurrent breast cancer. 1998. Available from ProQuest Dissertation and Theses database (UMI No. 1392755)
- 32.Eid J, Matthews MD, Meland NT, Johnsen BH. Dispositional optimism and self-assessed situation awareness in a Norweigian military training exercise. Perceptual and Motor Skills. 2005;100:649–658. doi: 10.2466/pms.100.3.649-658. [DOI] [PubMed] [Google Scholar]
- 33.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:129–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 34.IBM SPSS Statistics. Version 19.0.0. Copyright 2010.
- 35.Muthén LK, Muthén BO. Mplus User’s Guide. Sixth Edition Muthén & Muthén; Los Angeles, CA: 1998-2011. [Google Scholar]
- 36.Kaiser H. An index of factorial simplicity. Psychometrika. 1974;39:32–36. [Google Scholar]
- 37.Costello A, Osborne J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Practical Assessment, Research and Evaluation. 2005;10(7) [Google Scholar]
- 38.Cureton EE, Mulaik SA. The weighted varimax rotation and promax rotation. Psychometrika. 1975;40(2):183–195. [Google Scholar]
- 39.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed McGraw Hill; New York: 1994. [Google Scholar]
- 40.American Educational Research Association . Standards for educational and psychological testing. American Educational Research Association; Washington, D.C.: 1999. [Google Scholar]
- 41.Pett M. Making Sense of Factor Analysis: the Use of Factor Analysis of Instrument Development in Health Care Research. Sage Publications; Thousand Oaks: 2003. [Google Scholar]
- 42.Baldwin CM, Kapur VK, Holberg CJ, et al. Associations between gender and measures of daytime somnolence in the Sleep Heart Health Study. Sleep. 2004;27(2):305–311. doi: 10.1093/sleep/27.2.305. [DOI] [PubMed] [Google Scholar]
- 43.Mohsenin V. Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest. 2001;120(5):1442–1447. doi: 10.1378/chest.120.5.1442. [DOI] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention [Accessibility verified May 14, 2012];Alcohol use among women of childbearing age – United States, 1991-2005. Available at: http://www.cdc.gov/ncbddd/fasd/data.html.
- 45.Hayes A, Spilsbury J, Patel S. The Epworth score in African American populations. J Clin Sleep Med. 2009;5(4):344–348. [PMC free article] [PubMed] [Google Scholar]
- 46.Hedman C, Pohjasvaara T, Tolonen U, Suhonen-Malm AS, Myllyla VV. Effects of pregnancy on mother’s sleep. Sleep Med. 2002;3:37–42. doi: 10.1016/s1389-9457(01)00130-7. [DOI] [PubMed] [Google Scholar]
- 47.Akerstedt T, Nordin M, Alfredsson L, Westerholm P, Kecklund G. Predicting changes in sleep complaints from baseline values and changes in work demands, work control, and work preoccupation – the WOLF-project. Sleep Med. 2012;13(1):73–80. doi: 10.1016/j.sleep.2011.04.015. [DOI] [PubMed] [Google Scholar]