Abstract
We report the case of a 27-year-old female with intraparenchymal leiomyoma of the breast. This case is interesting not only because intraparenchymal leiomyoma of the breast is a rare benign non-epithelial tumor, but also because it is never found in women at such an early age. We explain all the aspects of this case in this report with its radiologic, histopathologic and immunohistochemical findings.
Keywords: Leiomyoma, Breast neoplasm, Intraparenchymal leiomyoma
Introduction
Intraparenchymal leiomyoma of the breast is one of the rarest benign non-epithelial tumors [1]. This benign smooth muscle neoplasm of the breast has been reported only in 22 cases, in women between their fifth and seventh decades of their lives [2], after Strong et al. initially described it in their book Leiomyoma of the Breast in 1913 [3]. Leiomyoma of the breast is commonly found in subareolar region due to the presence of abundant smooth muscle cells.
Case Report
A 27-year-old woman presented with the complaint of the growth of a painless lump in her left breast for the past 1 year. There was no evidence of nipple discharge, and there were no changes observed in the nipple and the areola. Furthermore, she was non-lactating and was not on hormone therapy. She also did not have any family history of breast cancer.
Physical examination revealed a well-defined mobile mass, 2 × 2 cm thick, in the upper medial quadrant (UMQ) of her left breast, 8 cm from the nipple. This mass was firm and non-tender with a smooth surface. It was also free from overlying skin, and there were no signs of inflammation. Axillary or supraclavicular lymph node was not palpable either, while the other breast and axilla were normal. The results of the fine needle aspiration cytology were inconclusive.
Imaging Findings
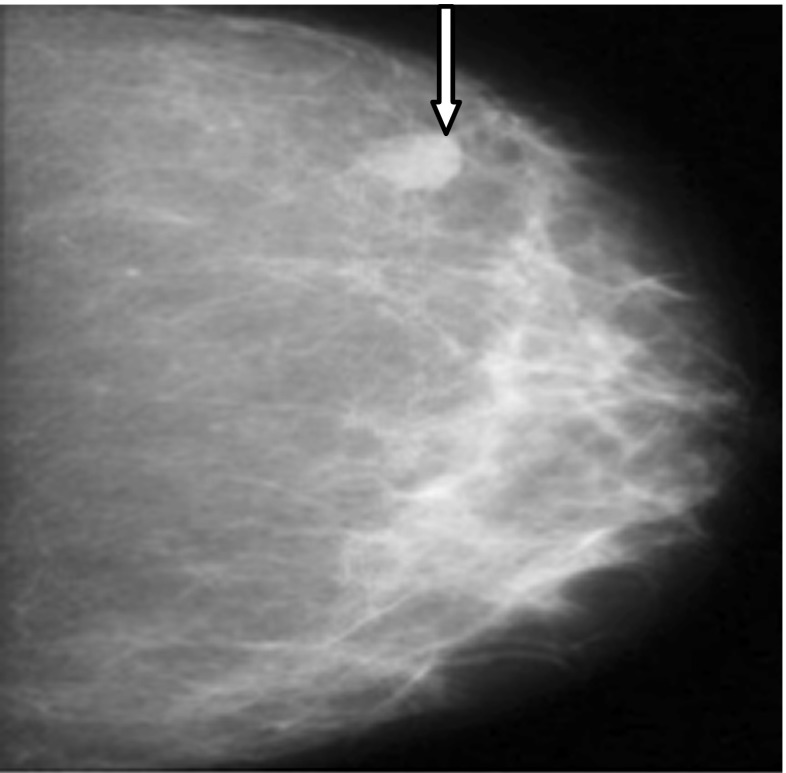
Mammogram showed a well-circumscribed dense, oval mass in the UMQ of the left breast (refer to Fig. 1). This mass showed no calcification, while no other lesions were detected in either of the breasts. No axillary lymphadenopathy was observed, and the mass was finally assessed and classified as that of a BIRADS category 2.
Fig. 1.
Craniocaudal mammographic view of the left breast, which shows a dense, oval mass with well-circumscribed margins (pointed by an arrow)
Pathologic and Immunohistochemical Findings
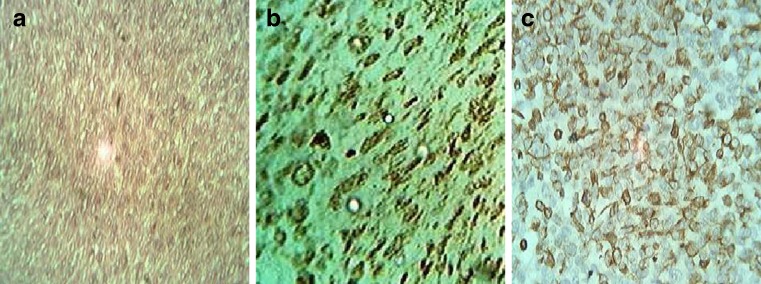
Based on clinical findings and the mammogram report, excisional biopsy of the lesion was performed. Gross examination revealed one nodular smooth firm tissue, 2 × 2 cm in diameter. The cross-section of the lesion showed a fleshy, pale white colour tissue, while histopathological examination showed a tumor composed of spindle cells arranged in interlacing bundles with interspersed vascular spaces. The cells exhibited vesicular nuclei and small inconspicuous nucleoli with minimal pleomorphism and infrequent mitosis (Fig. 2a). Immunohistochemical stains revealed diffused strong positivity for smooth muscle actin (Fig. 2b) and vimentin (Fig. 2c). These findings led to the diagnosis of intraparenchymal leiomyoma of the breast.
Fig. 2.
Microscopic view of sections of surgical specimen (H&E, 400×) through histopathological (a) and immunohistochemical (b, c) examinations. In particular, (a) shows proliferation of spindled-shaped cells with ovoid nuclei, arranged in interlacing bundles while (b) and (c) show diffused positivity for smooth muscle actin and vimentin, respectively
Discussion
Leiomyomas of the breast parenchyma are extremely rare [1] and its origin is uncertain. Diaz-Arias et al. have proposed five different theories for its cause [4]. Generally, the patients experience slowl-growing painless lumps, and on examination through mammogram these intraparenchymal leiomyoma lesions show well-defined margins [1, 4] that appear homogeneous and highly dense, with the absence of microcalcification, architectural distortion, skin thickening or nipple retraction [5]. The common histopathological features show groups of interlacing bundles of spindle-shaped cells with vesicular nuclei and eosinophilic cytoplasm, with no or infrequent mitosis [3]. Finally, immunohistochemical staining for this condition indicates positivity for vimentin, desmin and smooth muscle actin [1, 4]. Mammography, histopathological and immunohistochemical findings of the 27-year-old patient match with the above-mentioned facts of leiomyomas. The recommended treatment for intraparenchymal leiomyoma is simple excision.
The two common differential diagnosis of leiomyoma are fibroadenoma and leiomyosarcoma. Fibroadenoma can be distinguished by lack of distal attenuation on sonography [1, 2, 5], while leiomyosarcoma can be identified by the presence of cytologic atypia, numerous mitotic figures, atypical mitotic figures, vascular invasion and necrosis on histological examination [5]. The significance of this case is marked by the presence of intraparenchymal leiomyoma in a 27-year-old woman.
Conclusions
This case report summarises the diagnosis of intraparenchymal leiomyoma of the breast in a 27-year-old woman, which is extremely rare. It should be distinguished from its malignant counterpart–leiomysarcoma, because these two conditions differ significantly, as far as the line of treatment and prognosis are concerned.
References
- 1.Son EJ, Oh KK, Kim EK, et al. Leiomyoma of the breast in a 50-year-old woman receiving tamoxifen. AJR. 1998;171:1684–1686. doi: 10.2214/ajr.171.6.9843313. [DOI] [PubMed] [Google Scholar]
- 2.Lauren E, Cecilia M, Deborah A. Intraparenchymal leiomyoma of the breast: a case report and review of the literature. Annal Clin Lab Sci. 2007;37:3. [PubMed] [Google Scholar]
- 3.Strong LW. Leiomyoma of the breast. Am J Obstet. 1913;68:53–55. [Google Scholar]
- 4.Diaz-Arias AA, Hurt MA, Loy TS, et al. Leiomyoma of the breast. Hum Pathol. 1989;20:396–399. doi: 10.1016/0046-8177(89)90052-X. [DOI] [PubMed] [Google Scholar]
- 5.Kotsuma Y, Wakasa K, Yayoi E, et al. A case of leiomyoma of the breast. Breast Cancer. 2001;8:166–169. doi: 10.1007/BF02967498. [DOI] [PubMed] [Google Scholar]