Abstract
Mucosa-associated lymphoid tissue lymphomas (MALT lymphoma) are well known, but colonic MALT lymphomas are extremely rare. We report the first case of mucosa-associated lymphoid tissue (MALT) lymphoma in the cecum from India presenting as acute intestinal obstruction with mass in right iliac fossa showing diffuse thickening of ascending colon and caecum with obliterated lumen along with nodular mass on CECT scan of abdomen. On video colonoscopy, circumferential ulcerated growth was seen at cecum, and the rest of the colon was normal. Multiple biopsies from growth suggested malignancy. Right hemicolectomy was performed. The histopathology of resected specimen demonstrated low-grade B-cell MALT lymphoma of the cecum, and the depth of invasion was up to the muscular layer. This was confirmed by immunohistochemistry.
Keywords: GI tract, Cecum, MALT lymphoma, Immunohistochemistry, Intestinal obstruction, B-cell lymphoma, H. pylori
Introduction
Mucosa-associated lymphoid tissue lymphoma (MALT lymphoma) is a low-grade B-cell lymphoma. The very concept of MALT type of lymphoma was introduced by Isaacson and Wright [1]. As per the latest WHO classification, it belongs to the extranodal marginal zone lymphoma [2]. Primary colorectal lymphomas are particularly rare and contribute to 0.2 % of all colorectal malignancies. Helicobacter pylori and gluten are attributed as possible causative agents of this disease [3]. The gastrointestinal tract is the most common site for extranodal lymphoma and accounts for 30–45 % of all extranodal cases. The stomach is the most commonly involved organ followed by the small intestine and esophagus. The appendix may also rarely be involved [4]. The clinical presentation depends on the site of involvement. Pain, loss of appetite, weight loss, and gross gastrointestinal bleeding are the most common symptoms. Perforation and hemorrhage is reported as one of the complications. Surgical and endoscopic resection is effective treatment for rectal MALT lymphoma [5]. We report the first case of mucosa-associated lymphoid tissue (MALT) lymphoma in the cecum from India presenting as acute intestinal obstruction.
Case Report
We report a case of a 55-year-old man who was admitted to the surgical emergency department with pain in abdomen, generalized distention, vomiting, and inability to pass flatus and feces. On clinical examination, he was anemic, dehydrated with PR 120/min, BP 90/70 mmHg, RR 30/min, and temperature 100°F. His abdomen was distended with a tender mass in the right iliac fossa along with increased bowel sounds. The patient gave previous history of a gradually progressing mass in the right iliac fossa, dull pain in the lower abdomen, low-grade fever, anorexia, and weight loss. For these problems he was kept on conservative treatment with partial response. Video colonoscopy done at that time revealed circumferential ulcero-nodular growth at the cecum. Multiple biopsies were taken which showed loose stroma infiltrated by tumor cells of small to medium size, round to oval in shape, having hyperchromatic nuclei with homogenous chromatin and scant cytoplasm. Later the patient was admitted and investigated in our unit. His investigation showed Hb 8 mg/dl, TLC 10,200 mm3, DLC P60, L35, E02, M02, B01, RBS 86 mg/dl, S. Na+ 136, S. Ka+ 4.3, S. Ca+2 4.49, S. urea 23 mg/dl, S. creatinine 0 .7, INR 1.04, and serum CEA 1.23 ng/ml. On CECT abdomen, findings were suggestive of diffuse thickening of the ascending colon and cecum with obliterated lumen and a nodular mass in the right iliac fossa (Figs. 1 and 2).
Fig. 1.
CECT abdomen showing cecal growth
Fig. 2.
CECT abdomen showing enlarged lymph nodes along with dilated bowel loops
After correction of dehydration and taking consent, we explored the abdomen under general anesthesia. Per operatively we found loops of distended small bowels with friable growth of size 10 cm × 5 cm in the cecum with the thickened and edematous ascending colon. The growth was having cheesy material over it. The cecum and ileocecal junction showed necrotic and hemorrhagic areas with enlarged mesenteric lymph nodes. Right hemicolectomy was carried out and ileotransverse stoma was brought out with drainage of the pelvic cavity. Postoperative period was uneventful. The specimen was sent to the pathology department. Cut surface of the tumor was grayish white (Figs. 3 and 4). On microscopy there was focal ulceration on lining mucosa with subepithelium zone showing diffuse infiltration by the atypical lymphoid cell which was two times of the mature lymphocyte with clumped chromatin and scanty cytoplasm (Figs. 5, 6, 7 and 8). There is immune reactivity for CD20 and negative for CD3 on immunohistochemistry (Fig. 9). Histological and immune-profile findings were consistent with MALT lymphoma of the cecum with muscle invasion. Lymph nodes were positive for metastasis. Histological diagnosis was low-grade B-cell lymphoma.
Fig. 3.
Cut-open specimen of caecum showing ulcerated growth
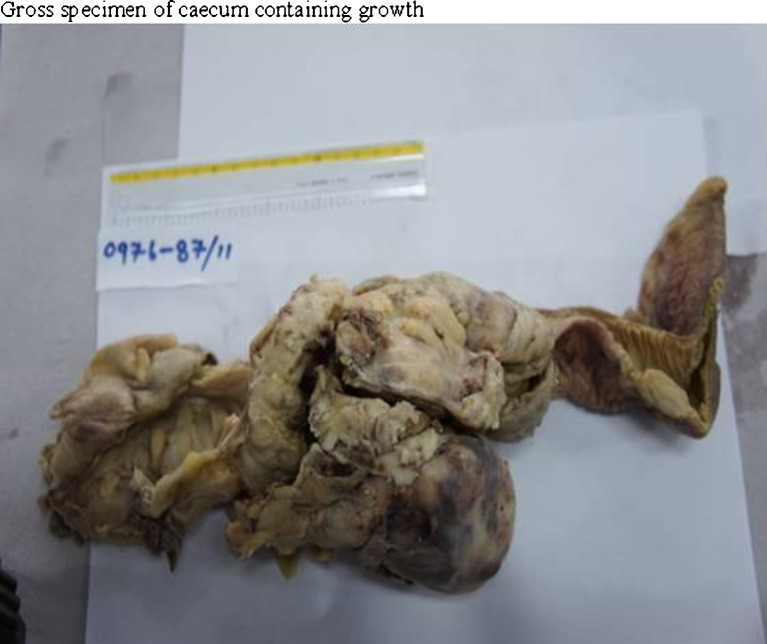
Fig. 4.
Gross specimen of cacum containing growth
Fig. 5.
Microphotograph showing lympho-epithelial lesion of MALT lymphoma (H&E stain 20×)
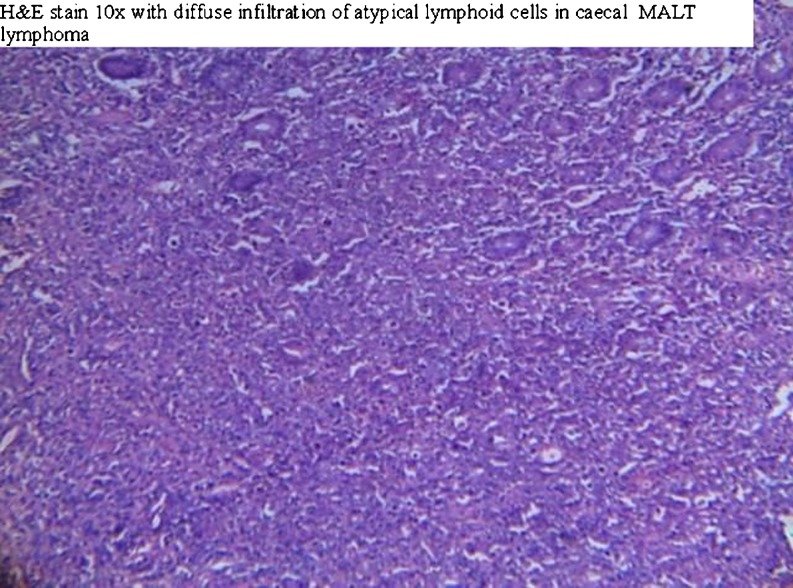
Fig. 6.
Diffuse infiltration of atypical lymphoid cells in cecal MALT lymphoma (H&E stain 10×)
Fig. 7.
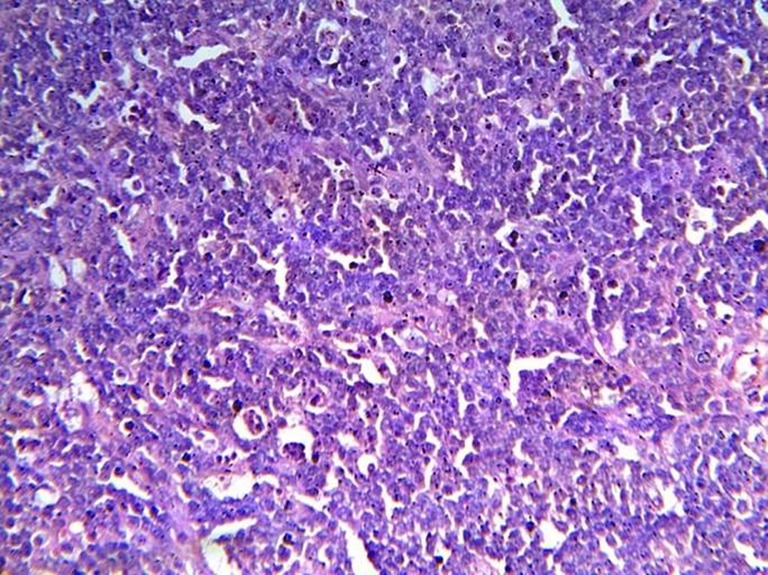
Atypical lymphoid cell in MALT lymphoma (H&E stain 40×)
Fig. 8.
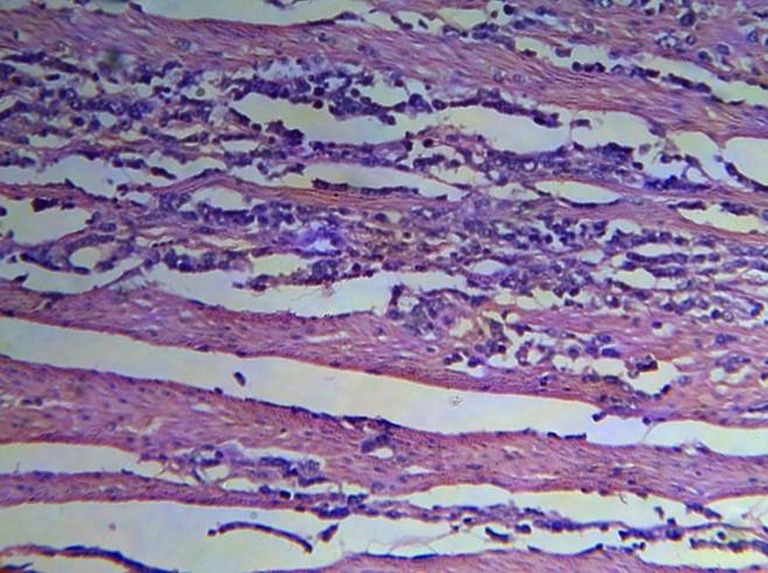
Atypical lymphoid cell infiltration in muscle bundle (H&E stain 20×)
Fig. 9.
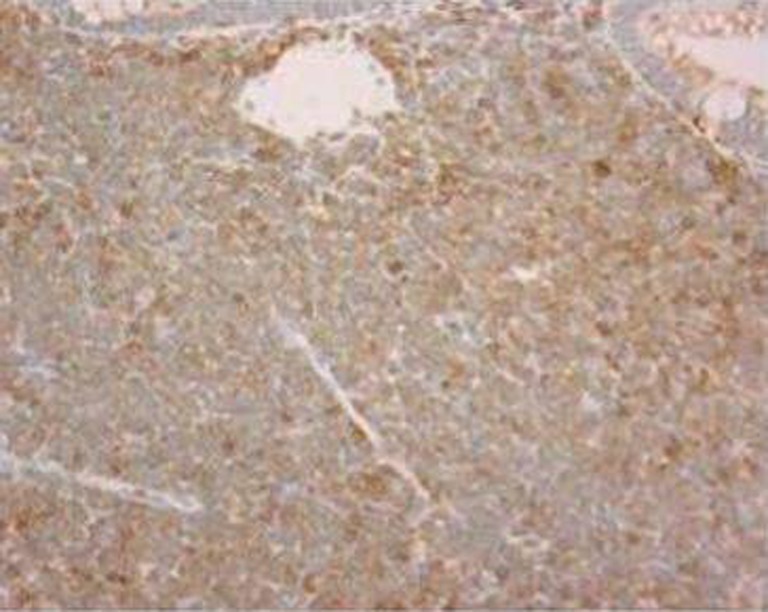
CD20-positive immunohistochemistry in MALT lymphoma
Postoperative recovery was smooth, and the patient was discharged on the 10th postoperative day. Three months later reversal of stoma was done by doing end-to-end ileotransverse anastomosis. No other therapy was given. At present patient is showing no clinical features of malignancy.
Discussion
The primary mucosa-associated lymphoid tissue (MALT) lymphoma or extranodal B-cell lymphoma is found in various anatomical locations such as stomach, appendix, salivary gland, thyroid, lung, and breast, but colorectal involvement is rare [4, 5]. Most common symptoms range from an asymptomatic stage to occult or gross gastrointestinal bleeding associated with anorexia and weight loss [6]. However, even after the thorough search of English medical literature, we could not find even a single case of MALT lymphoma of the cecum presenting as acute intestinal obstruction. Probably this is the first case report of such type. However, our case had most of common symptoms of extranodal lymphoma such as progressive lump, dull pain, low-grade fever, anorexia, and weight loss. The patient did not have history of gastrointestinal bleeding.
In our case, family history of such disease was negative, which is in accordance to the colonic case reported by previous authors [5]. Helicobacter pylori is suggested as one of the etiological factors because of its frequent coexistence and remission of tumors after H. pylori eradication treatment in gastric MALT lymphoma [7]. Infective etiology of such type in colonic MALT lymphoma is not yet reported. In our case too, we did not find association of H. pylori with the disease as upper GI endoscopy and biopsy of gastric mucosa, which was done after surgical treatment, was negative for H. pylori.
Regression of low-grade MALT lymphoma of extragastric site has been reported by H. pylori eradication treatment [8]. Regression of rectal MALT lymphoma has been reported after administration of quinolones. Nakase et al. reported regression even in H. pylori-negative cases in three patients [9]. Since our case reported as an acute emergency, we had no option other than exploration and surgical treatment. MALT lymphoma of the cecum is rare and surgical resection is the last and successful option for treatment of colonic MALT lymphoma. However, a standard protocol is yet to be established. We have also surgically treated our patient by standard right hemicolectomy; specimen showed 12/11 mesenteric lymph nodes positive for the tumor with tumor-free margins. Due to emergency presentation we did ileostomy with transverse colostomy after standard hemicolectomy.
In follow-up after 3 months of surgery, re-exploration of the abdomen was done for closure of stoma. We found no growth or lymph node suspicious of the tumor. End-to-end ileotransverse anastomosis was performed; postoperative follow-up up to 3 months of the second operation, the patient showed no symptoms or signs of malignancy. However, close follow-up examination is important because the long-term follow-up data are not available in such patients. MALT lymphoma of the cecum is rare. The prognosis for MALT lymphoma in the colon and cecum appears good by adequate surgery, but a standard treatment has not been established.
References
- 1.Issacson PG, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue: a distinctive type of B-cell lymphoma. Cancer. 1983;52:1410–1416. doi: 10.1002/1097-0142(19831015)52:8<1410::AID-CNCR2820520813>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 2.Stanojevic GZ, Nestorovic MD, Brankovic BR, Stojanovic MP, Jovanovic MM, Radojkovic MD. Primary colorectal lymphoma: an overview. World J Gastrointest Oncol. 2011;15:14–18. doi: 10.4251/wjgo.v3.i1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bacon CM, Du MQ, Ahmet D. Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists. J Clin Pathol. 2007;60:361–372. doi: 10.1136/jcp.2005.031146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miyazaki T, Ishiguro T, Ishibashi K, Itoyama S, Ishida H. Mucosa-associated lymphoid tissue lymphoma of the appendix vermiformis. Int Surg. 2010;95:27–32. [PubMed] [Google Scholar]
- 5.Ahlawat S, Kanber Y, Charabaty-Pishvaian A, Ozdemirli M, Cohen P, Benjamin S, et al. Primary mucosa-associated lymphoid tissue (MALT) lymphoma occurring in the rectum: a case report and review of the literature. South Med J. 2006;99:1378–1384. doi: 10.1097/01.smj.0000215855.98512.9d. [DOI] [PubMed] [Google Scholar]
- 6.Ghulam MA, Khush MS, Anwarul H, Mukhtar HR. Maltoma: a rare diagnosis in common presentation. Biomedica. 2001;17:1–2. [Google Scholar]
- 7.Neubauer A, Christian T, Birgit A, Markus R, Beatrix N, Gerhard E. Cure of Helicobacter pylori infection and duration of remission of low-grade gastric mucosa-associated lymphoid tissue lymphoma. J Natl Cancer Inst. 1997;89:1350–1355. doi: 10.1093/jnci/89.18.1350. [DOI] [PubMed] [Google Scholar]
- 8.Raderer M, Pfeffel F, Pohl G, Mannhalter C, Valencak J, Chott A. Regression of colonic low grade B cell lymphoma of the mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Gut. 2000;46:133–135. doi: 10.1136/gut.46.1.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakase H, Okazaki K, Ohana M, Ikeda K, Uchida K, Uose S, et al. The possible involvement of microorganisms other than Helicobacter pylori in the development of rectal MALT lymphoma in H. pylori-negative patients. Endoscopy. 2002;34:343–346. doi: 10.1055/s-2002-23643. [DOI] [PubMed] [Google Scholar]