Abstract
Spontaneous perforation of common bile duct (CBD) in an adult is an exceedingly rare phenomenon. It is mostly seen in infants due to congenital anomalies. The diagnosis of biliary tract perforations is often delayed due to their nonspecific symptoms, which results in high morbidity. Early diagnosis and aggressive therapy are mandatory to alleviate this condition. Delayed diagnoses and treatment may have more serious consequences in terms of morbidity as well as mortality. We herein report spontaneous perforation of CBD in a middle-aged male who presented to our accident and emergency department with acute abdominal pain. Exploratory laparotomy revealed a small perforation with necrosed margins in the supraduodenal part of CBD, which was managed by a T-tube drain. However, no apparent cause for the perforation was found.
Keywords: Spontaneous, Common bile duct perforation, Peritonitis, T-tube decompression
Case Report
A 35-year-old male, chronic cannabis abuser, presented to our accident and emergency department with a 2-day history of diffuse abdominal pain, which started in the epigastric region. There was no history of vomiting, fever, abdominal distension, jaundice, constipation, or upper or lower gastrointestinal bleed. He had previously been well with no relevant medical history. On examination, the patient was ill looking, febrile with tachycardia (118/min, low volume), and hypotensive (90/60 mmHg). Abdominal examination showed features suggestive of peritonitis. Baseline hematological investigations revealed only marked leukocytosis. Erect chest X-ray did not show any free gas under the right dome of diaphragm. Abdominal X-ray showed a ground glass appearance. Ultrasound abdomen revealed moderate amount of free fluid in the peritoneal cavity. Contrast-enhanced computed tomography scan of the abdomen showed only free fluid in the peritoneal cavity with omental heaping, in the right upper quadrant of the abdomen. Abdominal paracentesis revealed bilious fluid. In view of confusing picture of contrast-enhanced computed tomography abdomen and clinical features of peritonitis, the patient after being expeditiously resuscitated, was taken for urgent exploratory laparotomy with a preliminary impression of duodenal ulcer perforation. Operative findings revealed gross biliary contamination with about 3 L of bilious fluid in the peritoneal cavity. There were thin flimsy adhesions between gut loops, and the omentum was edematous and friable; however, no perforation was appreciated in the duodenum. On further dissection in the area, a small perforation (5–6 mm) was noticed in the normal caliber common bile duct (CBD), just distal to the opening of cystic duct in the CBD (Fig. 1). The perforation had unhealthy margins and was constantly oozing out bile. Gallbladder did not show any evidence of cholecystitis or perforation and there was no stone, sludge, or worm in the lumen of the gallbladder. Hence, cholecystectomy was performed and CBD exploration was carried out through the same perforation. No evidence of obstruction was found in the CBD despite meticulously looking for the same. T-tube drainage of CBD was performed and a thorough peritoneal lavage was done with warm normal saline. Peritoneal cavity was moped dry. Postoperatively, the patient fared well and was allowed orals on 2nd postoperative day. Postoperative liver function tests revealed isolated elevation of alkaline phosphatase, which then showed a decreasing trend on subsequent analysis. T-tube cholangiogram was done on 7th postoperative day, delineating whole of the ductal system with no filling defects; contrast was normally going into the duodenum. The T-tube was removed on 14th postoperative day and the patient was discharged home. Three days after the patient was discharged, he was readmitted with bilious ooze from the T-tube drain site. Magnetic resonance cholangiopancreaticography was performed, which revealed a normal ductal anatomy and minimal ooze from a well-formed T-tube tract (Fig. 2). Endoscopic retrograde cholangiopancreaticography was planned and endoscopic papillotomy with stenting was done. The patient fared well and the leak from the T-tube site subsided. The patient is on regular follow-up since then and is living a normal life.
Fig. 1.

Intraoperative photograph showing bile emanating from a small perforation in supraduodenal part of common bile duct
Fig. 2.
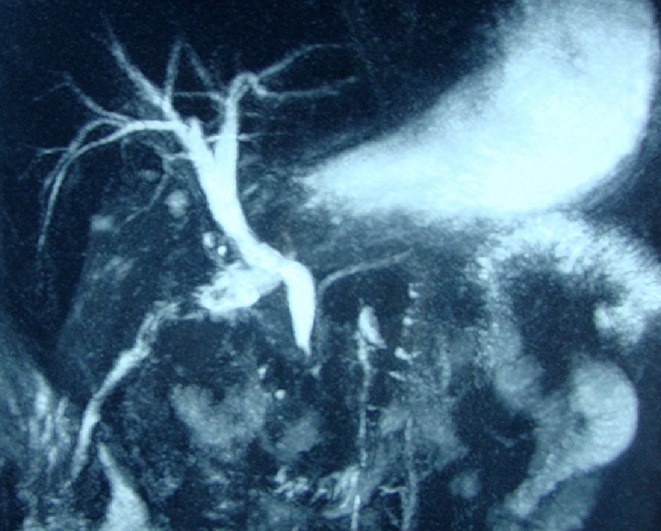
Post operative Magnetic Resonance Cholangiopancreatography (MRCP) showing normal ductal anatomy of biliary tree with a tract from the T-tube site
Discussion
Spontaneous perforation of CBD is very rarely found in adults, although it has been reported to occur more frequently in infants between 2 and 6 weeks of age [1]. The perforation is always found at the junction of cystic duct and CBD, which supports the suggestion of an area of developmental weakness [2]. Obstruction with inspissated bile has been demonstrated in several of the affected infants and is a likely cause of high intraluminal pressure [3]. Till date, spontaneous perforation of the bile duct in adults has been reported in only 70 cases in the English literature since its first description by Freeland in 1882 [4–7]. Different hypotheses in adults such as distal obstruction of the CBD [8], thrombosis of mural vessels leading to ischaemic damage of CBD wall, or pressure necrosis of the CBD due to impacted calculus and perforation of diverticulum have been put forth [9]. Spontaneous perforation in the biliary tree is initially manifested as an acute abdominal pain requiring surgical intervention, but usually the diagnosis is not made preoperatively owing to the rarity of this entity. The prognosis depends on the severity of the illness [4] and the time taken for definite operative management. High morbidity and mortality rates have been reported despite postoperative intensive care in cases of delayed management [4, 10]. Most adult cases (70%) are associated with obstruction to the biliary tract by stone disease [11]. Excluding gallbladder, the commonest sites of perforation are the CBD and cystic/hepatic duct junction. Spontaneous perforation of the bile ducts is uncommonly associated with a tumor because the slow rise of intraductal pressure caused by a tumor is much less likely to cause rupture of the duct than a sudden increase in pressure, such as that associated with stone disease [9]. Our patient was a chronic cannabis abuser and possibly had developed perforation of the CBD as a result of cannabis-induced ischemic damage to the mural vessels of CBD. Alternative pathological explanation suggested in our patient includes necrosis of the duct wall due to reflux of pancreatic secretions secondary to spasm of sphincter of Oddi.
All reported patients in the literature have either been treated surgically or have been diagnosed post-mortem. Common sense and widely accepted principles of biliary tract surgery are certainly central to minimizing mortality and morbidity rates in this setting. Recommended treatment is cholecystectomy with T-tube drainage of choledochus [12]. A cholecystostomy may be performed if dense adhesions are present in the region of CBD. A gallbladder flap may be applied over the perforation if it is large and friable along with T-tube biliary drainage. Primary repair of the CBD is considered unnecessary and even hazardous due to local inflammation. If ductal disruption is severe, a Roux-en-Y hepaticoenterostomy may be contemplated. Adequate drainage of the right upper quadrant is also important, as is parenteral antibiotic therapy with agents specific for bile flora.
In conclusion, spontaneous perforation of the bile ducts is a rare but important condition in adults. A very high index of suspicion supplemented by a good radiological diagnostic support can clinch the diagnosis preoperatively. Early surgical intervention forms the cornerstone of management of these patients, if both morbidity and mortality are to be prevented.
References
- 1.Kyzer S, Bayer I, Chaimoff C. Spontaneous rupture of the common bile duct. Can J Surg. 1986;29(1):68–69. [PubMed] [Google Scholar]
- 2.Patterson G. Spontaneous perforation of common bile duct in infants. Acta ChirScard. 1955;60:192–201. [PubMed] [Google Scholar]
- 3.Davenport M, Heaton ND, Howard ER. Spontaneous perforation of bile ducts in infants. Br J Surg. 1991;78:1068–1070. doi: 10.1002/bjs.1800780912. [DOI] [PubMed] [Google Scholar]
- 4.Paladugu R, Rau A, Schein M, Wise L. Spontaneous perforation of the hepatic duct in adults. Dig Surg. 1998;15:417–420. doi: 10.1159/000018655. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen WD, Daza E. Spontaneous perforation of the right hepatic duct. Hepatogastroenterology. 2001;48:1028–1029. [PubMed] [Google Scholar]
- 6.Ng WT. “Spontaneous” perforation of the common bile duct. Surgery. 1999;126:99–100. doi: 10.1016/S0039-6060(99)70049-8. [DOI] [PubMed] [Google Scholar]
- 7.Freeland J. Rupture of the hepatic duct. Lancet. 1882;1:731–732. doi: 10.1016/S0140-6736(02)21289-1. [DOI] [Google Scholar]
- 8.Megison SM, Votteler TP. Management of common bile duct obstruction associated with spontaneous perforation of the biliary tree. Surgery. 1992;111:237–239. [PubMed] [Google Scholar]
- 9.Hill NS, Colapinto ND. Spontaneous perforation of common bile duct. Br J Surg. 1981;68:661–662. doi: 10.1002/bjs.1800680916. [DOI] [PubMed] [Google Scholar]
- 10.Suarez L, Detmer DE, Jarrett F. Surgical management of spontaneous hepatic duct perforations. Ann Surg. 1981;194:176–179. doi: 10.1097/00000658-198108000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Piotrowski JJ, Van Stiegmann G, Liechty RD. Spontaneous bile duct rupture in pregnancy. HPB Surg. 1990;2:205–209. doi: 10.1155/1990/32017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neidbala A, Lankford A, Boswell WC, Rittmeyer C. Am Surg. 2000;66(11):1061–3. [PubMed] [Google Scholar]


