Abstract
Symptomatic primary hyperparathyroidism is still predominant form in developing countries. Sumit Shukla et al. (2008) Most of these lesions are usually less than 2 cm in diameter with serum calcium levels between 11 to 13 mg/dl. Our case had 3.9 × 2 × 1.7 cm non palpable right inferior parathyroid adenoma extending into superior mediastinum, serum calcium 17 mg/dl and vomiting as presenting symptom a case report.
Keywords: Hypercalcemia, Parathyroid adenoma, Superior mediastinum
Introduction
Parathyroid glands are located posterolateral and inferior to the thyroid gland. When the parathyroid glands enlarge they descent from their normal anatomic position. The inferior parathyroid glands arise from the third branchial pouche and since the embryologic journey is a longer one, ectopic sites for the inferior glands are more common and more widely distributed than ectopic sites for superior glands [2]. Our case was a 52 year old female who presented with recurrent vomiting for 3 days. Investigations showed serum calcium levels of 17 mg/dl with high parathormone levels. Sestamibi scanning and Ultrasound scan of neck detected a giant right inferior parathyroid adenoma extending into the superior mediastinum.
Case Report
A 52 year old female presented with recurrent vomiting for 3 days. Gastroduodenoscopy was normal. Serum calcium was17 mg/dl, serum albumin 3.7 gm/dl and serum creatinine 1.7 mg/dl. Further investigations revealed high parathormone (598 ng/ml) and phosphorus (1.7). Parathyroid scan showed retention of radiotracer over thyroid region. It was diagnosed as right parathyroid adenoma. USG of neck showed a large hypoechoic lesion 3.9 × 2 × 1.7 cm in the right paratracheal region extending from lower pole of right thyroid lobe medial to major vessels of neck. Inferior margin of lesion could not be traced due to retrosternal extension. After hemodialysis (with serum calcium 14.3 mg/dl) right inferior parathyroid adenoma was removed via low anterior cervical approach (Fig. 1).
Fig. 1.
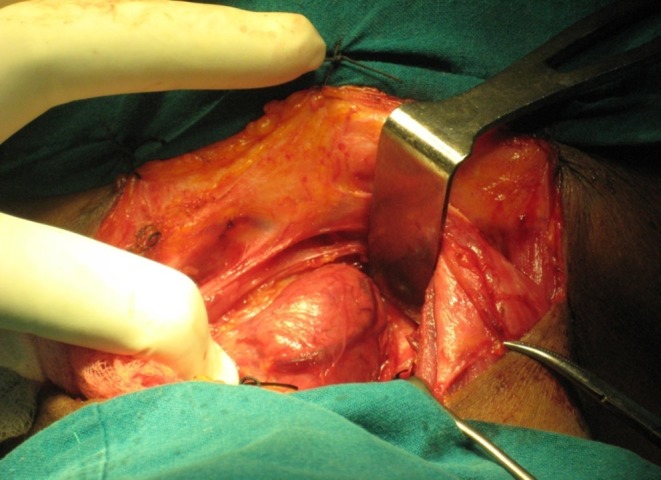
Shows giant right inferior parathyroid adenoma extending into superior mediastinum
Post-operatively patient had hypocalcaemia for which calcium gluconate injections were given followed by oral calcium. After 1 month of surgery, patient was fine with a calcium level of 9 mg/dl and reduced oral calcium requirement.
Discussion
Indian patients with primary hyperparathyroidism present at young age (below 40 years) due to prevalence of Vitamin D deficiency or due to genetic profile as compared to mean age of 55–62 years in developed countries. Abdominal symptoms are seen in more than 50% of primary hyperparathyroid patients but are less common in Indian patients [1]. Sestamibi scanning is done to localize adenoma as ectopic parathyroid occur in 16% of cases. It is 95% accurate and sensitive for locating parathyroid adenoma [3]. Ultrasound or CT scan of neck is done to assess exact site, size and related surrounding structures. Bilateral parathyroid exploration with thyroid mobilization by capsular dissection is the procedure of choice for primary hyperparathyroidism [4]. The standard surgical approach through a low anterior cervical incision is used for most adenoma resections, as well as resections of aorticopulmonary window parathyroid tumour [5]. Intraoperative parathormone assay is necessary in solitary adenoma for high success rate of minimal invasive parathyroidectomy where a scan directed removal of an abnormal parathyroid gland through an incision of less than 2.5 cm in length is done [6].
Parathyroid carcinoma is the cause of primary hyperparathyroidism in less than 1% of patients. Diagnosis requires presence of at least two of the following factors: histologic presence of capsular invasion, angioinvasion, tumor necrosis, fibrosis, pleomorphic cell in trabecular growth pattern, numerous mitotic figures, nuclear atypia and signs of invasion of the surrounding structures (venous structures, esophagus). Ki-67 labelling index use for differential diagnosis between parathyroid adenoma and carcinoma has been reported [7]. DNA ploidy analysis may be useful as most parathyroid carcinomas are aneuploid. Treatment for monolateral parathyroid carcinoma is total parathyroidectomy with ipsilateral thyroid lobectomy. Radical neck dissection is performed in case of lymph node metastases [8].
References
- 1.Shukla S, Kaushal M, Shukla SK. Primary hyperparathyroidism: retrospective 10 year study of 32 cases. Indian J Surg. 2008;70:169–174. doi: 10.1007/s12262-008-0047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sahin M, Cemil ER, Unlu Y, Tekin S, Seker M. An ectopic parathyroid gland in the left axillary region. Int Surg. 2004;89:6–9. [PubMed] [Google Scholar]
- 3.Bargallo E, Cabral AH, Mesko TW. Detecting intrathyroidal parathyroid adenoma with radioguided surgery. Surg Rounds. 2001;24:195–198. [Google Scholar]
- 4.Joshua CC, Shenoy J, Alfred AJ, Gaurav M, Keshav P. Familial isolated hyperparathyroidism caused by single adenoma. Indian J Surg. 2005;67:265–266. [Google Scholar]
- 5.Tovar EA. Transcervical resection of an aorticopulmonary window parathyroid tumor. Surg Rounds. 1999;22:638–640. [Google Scholar]
- 6.Pang T, Stalberg P, Sidhu S, Wilkinson M, Reeve TS, Delbridge L. Minimally invasive parathyroidectomy using the lateral focused mini-incision technique without intraoperative parathyroid hormone monitoring. BritJ Surg. 2007;94:315–319. doi: 10.1002/bjs.5608. [DOI] [PubMed] [Google Scholar]
- 7.Iihara M, Okamoto T, Suzuki R, Kawamata A, Nishikawa T, Kobayashi M, Obara T. Functional parathyroid carcinoma: Long term treatment outcome and risk factor analysis. Surgery. 2007;142(6):936–943. doi: 10.1016/j.surg.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 8.Falvo L, Catania A, Palermo S, Salvatore S, Bonifazi AP, De Stefano M, Berni A. Bilateral synchronous parathyroid carcinoma in a patient on long-term hemodialysis. Int Surg. 2005;90:18–22. [PubMed] [Google Scholar]


