Abstract
The malignant peripheral nerve sheath tumour is the malignant counterpart to benign soft tissue tumours such as neurofibromas and schwannomas. Malignant Triton Tumour is a histological variant of malignant peripheral nerve sheath tumours with rhabdomyosarcomatous differentiation. They are known to develop in cases of neurofibromatosis type 1 (von Recklinghausen’s disease). Malignant peripheral nerve sheath tumor is biologically an aggressive tumour for which the treatment of choice is surgery. Here we report a rare case of malignant peripheral nerve sheath tumour, not associated with neurofibromatosis type 1 and arising in the retroperitoneum.
Keywords: Peripheral nerve sheath tumour, Malignant triton tumour, Neurofibromatosis
Introduction
The malignant peripheral nerve sheath tumour (MPNST) is the malignant counterpart to benign soft tissue tumours such as neurofibromas and schwannomas. Malignant triton tumour (MTT) is a histological variant of MPNSTs with rhabdomyosarcomatous differentiation. MPNSTs are known to develop in cases of neurofibromatosis type 1 (von Recklinghausen’s disease, NF-1) and sometimes occur in the retroperitoneal space. There are few reports of MTTs developing in the retroperitoneal space. We report an extremely rare case of MTT developing in the retroperitoneal space which is not associated with NF-1.
Case Report
A 62 year old male presented with complaints of a palpable lump in the left upper abdomen of 3 months duration which was gradually increasing in size and difficulty in swallowing food for 2 months. General examination revealed no abnormalities with no signs of neurofibromatosis. On investigation, routine blood and urine tests were normal. Plain chest radiograph showed a moderate pleural effusion on the left side. Ultrasonography of the abdomen showed a hypoechoic mass to the left of the abdominal aorta, displacing the spleen antero-superiorly and the left kidney postero-inferiorly. Computed Tomography Scan showed a retroperitoneal mass of about 10.5 × 7.8 × 6.2 cm. Rest of the findings were consistent with the ultrasonography findings. Fine needle aspiration cytology of the tumour showed spindle cell tumour. A provisional diagnosis of retroperitoneal liposarcoma or a spindle cell tumour was made and the patient was posted for exploratory laparotomy.
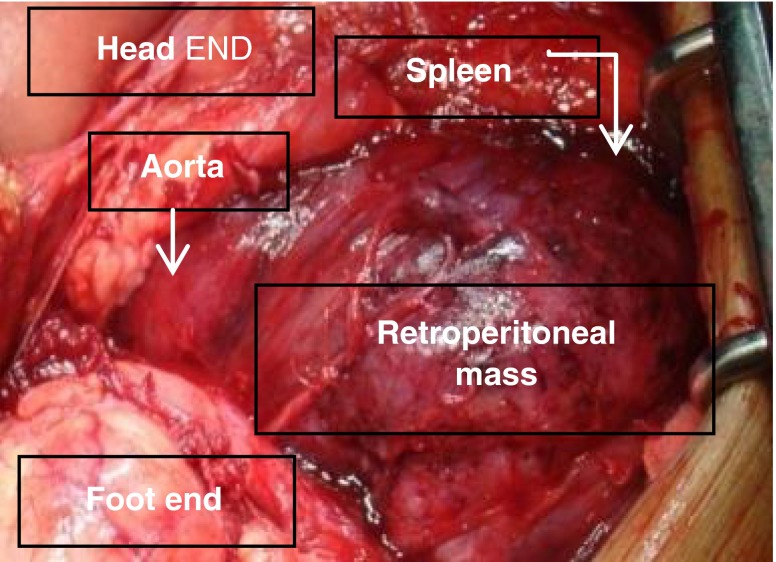
The retroperitoneum was reached through a transperitoneal approach. The tumour was identified and seen approaching the abdominal aorta on the left side and the spleen (Fig. 1). The adhesions were released and the tumour removed en bloc. The left kidney was seen embedded in the tumour and hence a nephrectomy was necessary. Splenectomy was necessary as the tumour was encroaching the spleen.
Fig. 1.
Intraoperative photograph
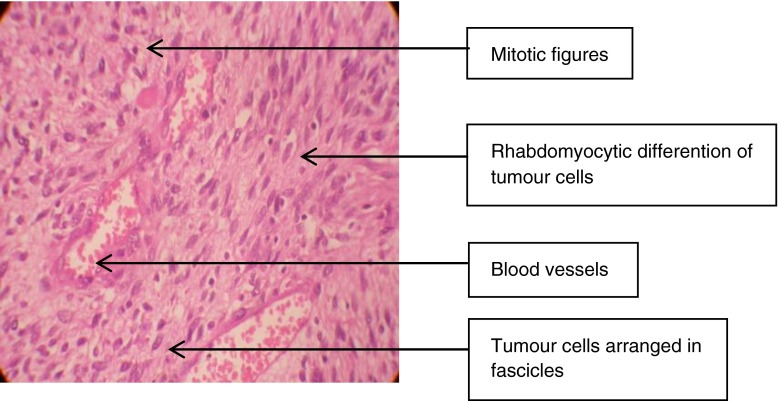
The specimen was sent for histopathological examination which gave a diagnosis of ‘high grade MPNST of triton type’ (Fig. 2).
Fig. 2.
Histological appearance
Post-operative period was uneventful. The patient is free of the disease 1-year after resection with no evidence of recurrence on ultrasonography.
Discussion
MPNSTs are known to arise from major and minor peripheral nerves or within pre-existing neurofibromas, and approximately 50% of patients with MPNSTs have NF-1 [1, 2]. NF-1 is an autosomal dominant disorder characterized by café-au-lait spots, cutaneous neurofibromas, skeletal dysplasias, Lisch nodules, and sometimes malignant tumours. The precise cell of origin of MPNSTs has not yet been conclusively identified, although the Schwann cell is thought to be the major candidate cell. The capacity of MPNSTs to undergo focal divergent differentiation is well known, and tumours showing rhabdomyosarcomatous differentiation, referred to as MTTs, are identified in approximately 12% of patients with MPNSTs [1]. Woodruff et al. [3] reported a series of ten cases of malignant schwannoma with rhabdomyoblastic differentiation, which they were the first to refer to as MTTs. The average age of patients with MTTs is 31.7 years and these tumours occur with approximately equal frequency in males and females [4]. The reported incidence of MTTs occurring in association with NF-1 is in the range of 44–69%. The 5-year survival rate of patients with MTTs is 12–26% [4]. The reason for the more aggressive behaviour of MTTs than classic MPNSTs still remains unclear. MTTs occur predominantly in the trunk, head and neck, and lower extremities [5]. According to a review of 75 cases of MTTs by Yakulis et al. [4] the tumour was located in the retroperitoneum in only one case (1.3%), as seen in our case. All the three cases of MTTs developing in the retroperitoneal space reported so far, and our case, presented with a huge abdominal mass, since these retroperitoneal tumours are often asymptomatic in the earlier stages [4, 6]. Like most soft-tissue sarcomas, MTTs traditionally are insensitive to chemotherapy and radiotherapy. However, several authors have reported recently that repeated resection combined with chemotherapy and/or radiotherapy against recurrent MTTs might prolong the survival in patients with MTTs [7, 8].
Conclusion
This case is the fourth case reported in literature on the development of MTT in the retroperitoneum that is not associated with a history of NF-1. MPNSTs and MTTs have a high malignant potential, and hence patients with NF-1 should be followed-up periodically.
References
- 1.Ducatman BS, Scheithauer BW, Piepgras DG, et al. Malignant peripheral nerve sheath tumours. A clinicopathologic study of 120 cases. Cancer. 1986;57:2006–2021. doi: 10.1002/1097-0142(19860515)57:10<2006::AID-CNCR2820571022>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Wanebo JE, Malik JM, VandenBerg SR, et al. Malignant peripheral nerve sheath tumours. A clinicopathologic study of 28 cases. Cancer. 1993;71:1247–1253. doi: 10.1002/1097-0142(19930215)71:4<1247::AID-CNCR2820710413>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 3.Woodruff JM, Chernik NL, Smith MC, et al. Peripheral nerve tumours rhabdomyosarcomatous differentiation (malignant “Triton” tumours) Cancer. 1973;32:426–439. doi: 10.1002/1097-0142(197308)32:2<426::AID-CNCR2820320221>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 4.Yakulis R, Manack L, Murphy AI., Jr Post-radiation malignant triton tumour. A case report and review of the literature. Arch Pathol Lab Med. 1996;120:541–548. [PubMed] [Google Scholar]
- 5.Stasik CJ, Tawfik O. Malignant peripheral nerve sheath tumour with rhabdomyosarcomatous differentiation (malignant triton tumour) Arch Pathol Lab Med. 2006;130:1878–1881. doi: 10.5858/2006-130-1878-MPNSTW. [DOI] [PubMed] [Google Scholar]
- 6.Murtaza B, Gondal ZI, Mehmood A, et al. A huge malignant triton tumour. J Coll Physicians Surg Pak. 2005;15:728–730. [PubMed] [Google Scholar]
- 7.Kostler WJ, Amann G, Grunt TW, et al. Recurrent malignant triton tumour: first report on a long time survivor. Oncol Rep. 2003;10:533–535. [PubMed] [Google Scholar]
- 8.Lang-Lazdunski L, Pons F, Jancovici R. Malignant triton tumour of the posterior mediastinum: prolonged survival after staged resection. Ann Thorac Surg. 2003;75:1645–1648. doi: 10.1016/S0003-4975(02)04825-7. [DOI] [PubMed] [Google Scholar]