Abstract
Traumatic cysts of liver are amongst the less frequently known sequelae of liver trauma. The incidence of this entity is very low. We report a case of large posttraumatic liver cyst in a young adult female, who sustained blunt abdominal trauma 2 months back. The cyst was diagnosed by CECT Abdomen and was treated by hepatic resection(left lobe). The aim of presentation of this report is to highlight the fact that blunt trauma abdomen can result in such rare presentations which can lead to hepatic resection.
Keywords: A 34 year old female presented with epigastric swelling and pain abdomen of 2 months duration, Further when CECT abdomen was done it showed a large haemorrhagic cyst involving the left lobe of liver, Left hepatic resection, Cyst mainly contained bile and small amount of altered blood and necrotic tissue
Introduction
Solitary liver cysts were recognized as early as 1937. These can be congenital or acquired, congenital varieties being more common. Acquired can be traumatic, inflammatory or neoplastic. The liver is one of the most commonly injured organs in abdominal trauma. Most often hepatic trauma results only in superficial lacerations. Traumatic liver cysts are unusual sequelae of hepatic trauma. Very few cases of post-traumatic liver cysts have been described in the literature. This case represents a typical natural history of a traumatic liver cyst.
Case Report
A 34-year-old female presented with epigastric swelling and pain abdomen of
2 months duration. There was a history of trauma 2 months back in
the form of assault. Following this, she developed pain in the epigastric region and
was treated at a local hospital with antibiotics and analgesics for 10 days.
Subsequently, the pain subsided. Since then she gradually has developed an
epigastric swelling with dull aching pain. Now she complains of associated loss of
appetite and post-prandial nausea . On examination, there was an epigastric swelling
of about 10 x 10 cm, which was firm in consistency and moved with
respiration. The lower border was palpable and was regular. The upper border could
not be felt suggestive of left hepatic lobe enlargement. Swelling was mildly tender
and no other mass was palpable. On investigation, blood routine, urine routine and
liver function tests were all normal. USG showed a possibility of cystic mass placed
anterior to pancreas, probably a pseudocyst of pancreas or a resolving hematoma.
Tumor markers were all negative except CA19-9, which was mildly elevated
(180 IU). Further when CECT abdomen was done, it showed a large hemorrhagic
cyst involving the left lobe of the liver.
The patient was taken up for surgery and deroofing procedure was planned, but
intra-operatively it was found that all of the left lobe was involved and only a
thin strip of liver tissue was viable on the left side of the cyst, so the procedure
was changed to left hepatic resection. The cyst mainly contained bile and a small
amount of altered blood and necrotic material.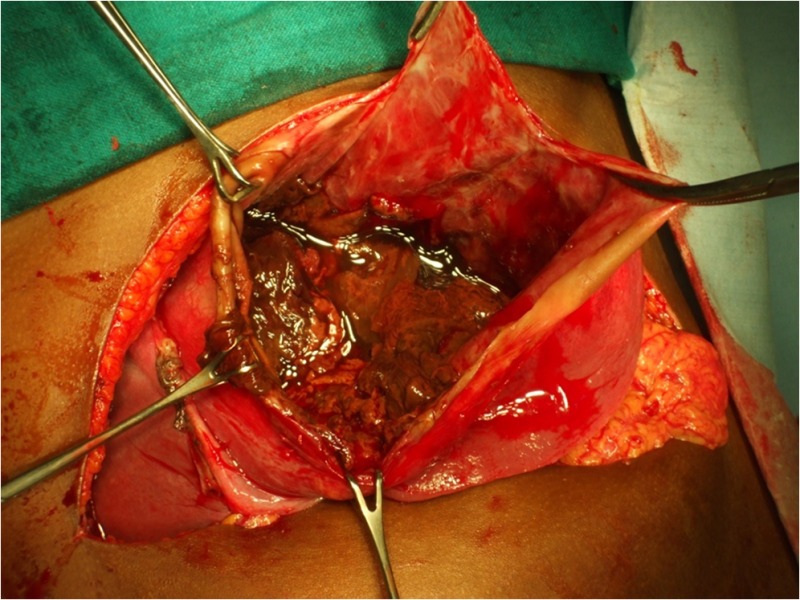
Post-operatively, the patient is recovered well. She was afebrile, urine output was
adequate, wound was clean and blood investigations were normal. Immediate
post-operative period showed slight elevation of liver enzymes, but subsequently the
level returned to normal on the 4th post-operative day. Abdominal drain was removed
on the 5th post-operative day and she started oral feed on the 6th post-operative
day.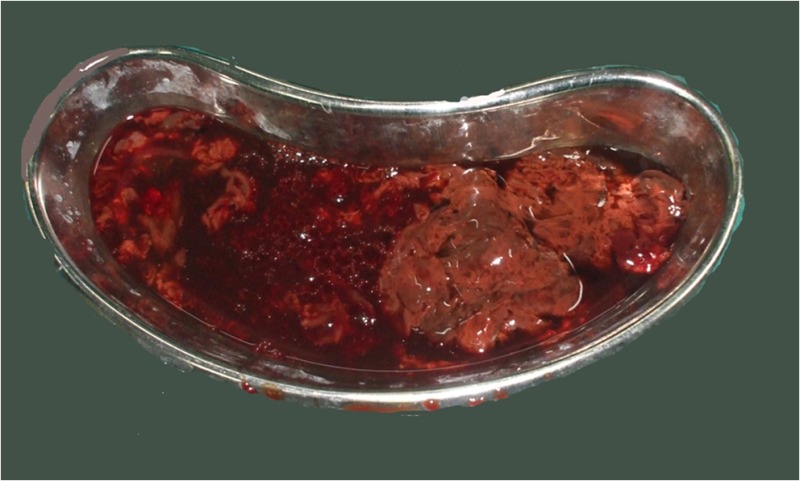
The contents of the cyst were sent for culture and sensitivity and found to be sterile. The histopathology report showed that it was a pseudocyst suggestive of a traumatic origin and ruling out a post-traumatic hemorrhage in a pre-existing simple cyst. CA19-9 returned to the normal level 1 week following surgery.
Discussion
Traumatic cysts of liver are among the less frequently known sequelae of liver trauma. The incidence of this entity is very low and has been reported to be even less than 0.5 % [1]. Abdominal pain, distension and hepatomegaly were the most common presenting features in the cases described in the literature. In many patients, the diagnosis was made only at laparotomy performed due to complications of the post-traumatic hepatic cyst [1–3]. These complications are obstructive jaundice, abscess formation, hemorrhagic shock or bile peritonitis due to cyst rupture [1–3]. Our patient also presented with abdominal pain and distension. In addition, she had an epigastric mass, which mimicked the presentation of a post-traumatic pseudopancreatic cyst, both clinically and radiologically.
Christopher [4] has classified traumatic liver rupture into three types: central, subcapsular and rupture of liver tissue with its capsule. Intra-hepatic rupture of liver tissue causes oozing of blood and bile, which usually results in the formation of a traumatic liver cyst [4]. The bleeding may stop, while flow of bile may continue and hence the cyst continues to grow. Therefore, there is usually a delay of several days to several months, or even years after the hepatic trauma, before the patient becomes symptomatic [2, 3, 5]. However, patients becoming symptomatic within a few hours of injury have also been observed [2].
The differential diagnosis of a post-traumatic liver cyst clinically and at imaging includes a solitary unilocular cyst or hydatid cyst of liver, a pseudopancreatic cyst and loculated ascites, especially due to tuberculosis [6]. Diagnosis is established by the nature and location of the mass at surgery. In a post-traumatic cyst, altered blood and bile are the chief constituents while a simple unilocular hepatic cyst contains thin clear fluid and a hydatid cyst contains scolices [6]. Definitive diagnosis at histopathology is based on recognizing a true epithelial lining in a unilocular hepatic cyst [6] while a post-traumatic cyst does not have a true epithelial lining.
The modalities of treatment employed in the past for these cysts included simple drainage, intermittent irrigation and drainage by means of a tube, marsupialization of the cyst to the abdominal wall and repeated packings. In a few cases, partial hepatectomy was resorted to. Recently, Chuang and Huang treated their patients of the post-traumatic hepatic cyst by decortication of the cyst wall and omentoplasty. Generally, the results of treatment by any of the described methods were found to be satisfactory. However, a few cases of traumatic hepatic cysts with spontaneous resolution have also been recorded.
References
- 1.Sugimoto T, Yoshioko T, Sawada Y, Sugimoto H, Maemura K. Post traumatic cyst of the liver found on CT scan—a new concept. J Trauma. 1982;22:797–800. doi: 10.1097/00005373-198209000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Henson SW, Jr, Gray HK, Dockerty MB. Benign tumors of the liver vs traumatic cysts. Surg Gynaec Obs. 1957;104:302–306. [PubMed] [Google Scholar]
- 3.Jones HV, Harley HR. Traumatic cyst of the liver. Br J Surg. 1970;57:468–470. doi: 10.1002/bjs.1800570616. [DOI] [PubMed] [Google Scholar]
- 4.Christopher F. Rupture of the liver. Ann Surg. 1936;103:461–464. doi: 10.1097/00000658-193603000-00019. [DOI] [Google Scholar]
- 5.Chuang JH, Huang SC. Post traumatic hepatic cyst—an unusual sequel of liver injury in the era of imaging. J Pediatr Surg. 1996;31:272–274. doi: 10.1016/S0022-3468(96)90013-5. [DOI] [PubMed] [Google Scholar]
- 6.Peltokallio V. Non parasitic cysts of the liver—a clinical study of 117 cases. Ann Chir Gynecol Fenn. 1970;59(Suppl 174):1–63. [PubMed] [Google Scholar]


