Abstract
Pneumobilia denotes an abnormal connection between the gastrointestinal and the biliary tracts. In the absence of surgically created anastomosis between the bowel and the bile duct, the common causes for pneumobilia are gallstone obstruction, endoscopic interventions or emphysematous cholecystitis. We present the case of a young male with traumatic pneumobilia with gastric perforation and a tear in the mesentery of the small gut following penetrating trauma in the form of stab in the abdomen.
Keywords: Pneumobilia, Trauma, Perforation
Introduction
Most cases of pneumobilia are related to gallstone ileus of the duodenum, emphysematous cholecystitis, surgically created anastomosis between the bowel and the extrahepatic biliary tract or endoscopic interventions [1]. However, pneumobilia may also be caused by a sphincter of Oddi (SO) dysfunction [2, 3]. In case of smooth muscle, hypotension of the SO air can reach from the duodenum into the biliary tract. We present a case of young male with traumatic pneumobilia along with gastric perforation and a linear tear in the mesentery of the small gut following penetrating trauma in the form of stab in the abdomen.
Case report
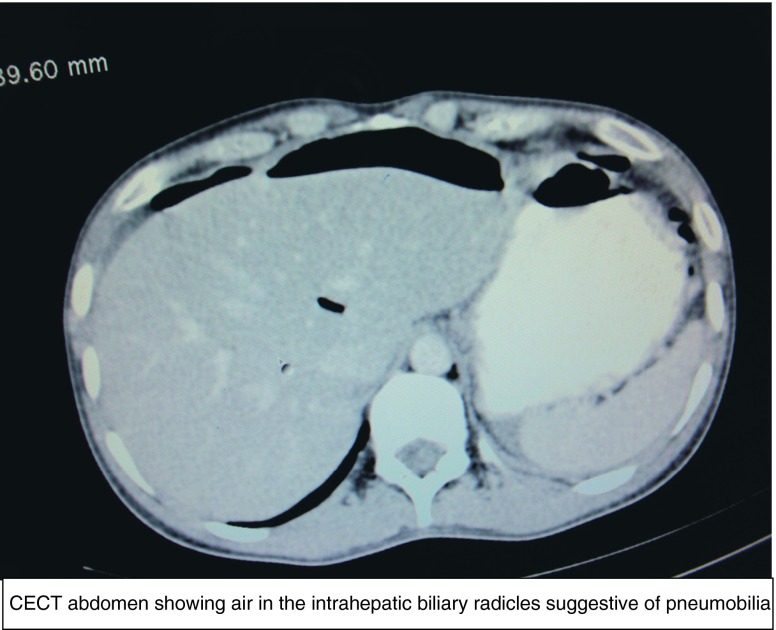
A 25-year-old male patient was stabbed in the abdomen in the epigastrium. The patient reported to our hospital about 2 h after the incident. On examination, the abdomen was soft with generalised tenderness. Abdominal X-ray in the erect posture showed gas under both domes of the diaphragm. To rule out any other visceral injury contrast enhanced CT scan was done, which showed the findings of pneumobilia along with pneumoperitoneum and ascites (Fig. 1). Air was confined to the intrahepatic biliary radicles. There was no gallstone or any other pathology of the biliary tract. An exploratory laparotomy was performed. It was found that a small perforation of about 1 cm was present in the anterior wall of the stomach. There was also a small tear in the mesentery of the small gut. The gastric perforation was closed with vicryl 2–0 and an omental patch applied. The tear in the mesentery was repaired. Liver was found to be normal and so were the rest of the gut and other viscera. The source of pneumobilia could not be traced. The peritoneal cavity was irrigated with saline and toilet was performed. The abdomen was closed in layers after achieving haemostasis. Postoperative period remained uneventful.
Fig. 1.
CECT abdomen showing air in the intrahepatic biliary radicles suggestive of pneumobilia
Discussion
Pneumobilia denotes an abnormal connection between the gastrointestinal and the biliary tracts. In the absence of surgically created anastomosis between the bowel and the bile duct, most cases of pneumobilia are related to gallstones [4]. Spontaneous biliary-enteric fistulas may develop if a gallstone erodes through the gall bladder wall into an adjacent viscus, i.e. stomach, duodenum, small bowel or colon [5, 6]. Endoscopic retrograde cholangiopancreatography with papillotomy or surgical transduodenal sphincteroplasty may disrupt the SO, and have been reported to cause pneumobilia [7]. Finally, emphysematous cholecystitis and biliary-bronchial fistulas secondary to liver abscess are cited as rare reasons for developing pneumobilia [8]. Diagnosis of pneumobilia is made by plain radiography, ultrasonography or CT. Linear branching or tubular radiolucencies in the central portion of the liver are suspicious on plain radiography. On ultrasonography, air in the biliary tree may be seen as bright linear and branching echoes within the intrahepatic bile ducts. However, CT is the most sensitive and specific technique to diagnose pneumobilia. Our patient had no history of former surgery, and revealed no gallstones. Therefore, gallstone disease could be ruled out as cause for pneumobilia. Some authors discuss the SO dysfunction in combination with an increased intraabdominal pressure as a possible reason for retrograde transition of air into the biliary tract [8]. The principal SO functions are to prevent duodenum- to-bile-duct reflux and to regulate the bile and pancreatic juice flow. The dysfunction is a motor SO abnormality, which may result in a hypotonic or more commonly in a hypertonic sphincter. In our case, the exact cause of pneumobilia could not be traced. The whole of the gut was found to be normal. Pneumobilia was an incidental CT finding. Surgical exploration was necessary on account of gut perforation.
Conclusion
For the first time we report about pneumobilia following penetrating trauma of the abdomen since former biliary pathology, inflammations or biliary-enteric fistulas were excluded. In our opinion, pneumobilia was an incidental CT finding and it strengthens the opinion that pneumobilia does not always necessitate surgical exploration.
References
- 1.Bautista JL, Budhraja MD, Barcia TD, Shankel SW. Pneumobilia associated with small-bowel obstruction. JAMA. 1988;260:1930–1931. doi: 10.1001/jama.1988.03410130138039. [DOI] [PubMed] [Google Scholar]
- 2.Sherman S, Lehman GA. Sphincter of Oddi dysfunction: diagnosis and treatment. JOP. 2001;2:382–400. [PubMed] [Google Scholar]
- 3.Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686. doi: 10.1136/gut.49.5.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gering SA, Foster MA, Harnisch MC, McNeil JJ. Traumatic pneumobilia: case report. J Trauma. 2001;51:391–394. doi: 10.1097/00005373-200108000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Baz MA, Sharara AI. The clinical significance of spontaneous pneumobilia. N C Med J. 1995;56:398–340. [PubMed] [Google Scholar]
- 6.Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60:441–446. [PubMed] [Google Scholar]
- 7.Motta G, Ratoore GB, Barone D, Pugliese V, Aste H, Gianquinto D. Endoscopic papillosphincterotomy and surgical sphincteroplasty for the treatment of bile duct stones: a comparative analysis. Ital J Surg Sci. 1989;19:165–171. [PubMed] [Google Scholar]
- 8.Sarr MG, Smith GW, DeLeon EF. Biliary bronchial fistula after right hepatic lobectomy. Arch Surg. 1985;120:1376–1380. doi: 10.1001/archsurg.1985.01390360042010. [DOI] [PubMed] [Google Scholar]