Abstract
Objectives
Over-the-counter (OTC) pharmacy medicines are considered relatively safe in contrast to prescribed and illicit substances, but their abuse and addiction potential is increasingly recognised. Those affected represent a hard to reach group, with little known about their experiences. Study objectives were to describe the experiences and views of those self-reporting OTC medicine abuse, and why medicines were taken, how they were obtained and associated treatment and support sought.
Design
Qualitative study using in-depth mainly telephone interviews.
Participants
A purposive sample of 25 adults, aged 20–60s, 13 women.
Setting
UK, via two internet support groups.
Results
Individuals considered themselves ‘addicted’, but socially and economically active and different from illicit substance misusers. They blamed themselves for losing control over their medicine use, which usually began for genuine medical reasons and not experimentation and was often linked to the cessation of, or ongoing, medical prescribing. Codeine, in compound analgesics, was the main medicine implicated with three distinct dose ranges emerging with decongestant and sedative antihistamine abuse also being reported. Subsequent use was for the ‘buzz’ or similar effects of the opiate, which was obtained unproblematically by having lists of pharmacies to visit and occasionally using internet suppliers. Perceived withdrawal symptoms were described for all three dose ranges, and work and health problems were reported with higher doses. Mixed views about different treatment and support options emerged with standard drug treatment services being considered inappropriate for OTC medicines and concerns that this ‘hidden addiction’ was recorded in medical notes. Most supported the continued availability of OTC medicines with appropriate addiction warnings.
Conclusions
Greater awareness of the addiction potential of OTC medicines is needed for the public, pharmacists and medical prescribers, along with appropriate communication about, and reviews of, treatment and support options, for this distinct group.
Keywords: Qualitative Research, Primary Care
ARTICLE SUMMARY.
Article focus
Over-the-counter (OTC) medicines are increasingly recognised as having addiction potential.
To describe the experiences and views of individuals addicted to OTC medicines.
Key messages
Addiction to OTC medicines was associated with genuine medical reasons initially and linked to medical prescribing.
Codeine is main medicine abused for non-therapeutic effects in distinct dose ranges, but other medicines also identified.
Current treatment may not be appropriate, based on hidden nature of OTC addiction and perceived differences to other forms of addiction.
Strengths and limitations of this study
First qualitative study to explore a variety of OTC addictions and associated reasons and treatment in a recognised hard to reach group.
Recruitment via internet support groups reflects only those with internet access and those who have identified themselves already as having an addiction problem.
Introduction
In contrast to prescribed and illicit drugs, those available for individuals to purchase legally without prescription have often been perceived by the public to be relatively safe.1 2 Such non-prescription, or over-the-counter (OTC) medicines as they are also known, are typically those purchased from non-medical outlets such as pharmacies and increasingly the internet3 and have enabled individuals to be active participants in their own health.4 There has been increasing concern, however, about the potential for OTC medicines to cause harm, as a recent All Party Parliamentary report,5 and a joint consensus statement6 on addiction to medicines in the UK illustrate. Implicated medicines and therapeutic groups include stimulants, laxatives, sedatives, dissociative substances and opiate-containing medicines such as codeine.7 8 There has been increased reporting of harms associated with codeine addiction and particularly from side effects of additional ingredients, such as ibuprofen and paracetamol which have led to fatalities.7 9 These have resulted in regulatory changes in countries such as the UK10 and Australia involving restricted indications and addiction warnings on codeine-containing analgesic packets.
Despite these emerging concerns, the scale of the problem remains uncertain and very little is known about the characteristics and particularly the experiences of those affected.7 11 Empirical quantitative studies have provided some evidence suggesting that a diverse group of individuals may be affected, ranging from adolescents experimenting with cough medicines in the USA,12 to older individuals abusing analgesics in Nigeria,13 and abuse of codeine-containing medicines and sedatives involving ‘middle-aged females’ in the UK.14 15 Such individuals have been recognised as a hard to reach group5 and this has resulted in indirect attempts to describe those affected, such as seeking pharmacists’ proxy views of those affected through surveys.7 16 This paper describes the findings of a study that sought to explore the views and experiences of individuals who considered themselves affected by OTC medicine addiction in the UK, to understand how it arose, what medicines were implicated and how they were obtained and what forms of treatment and support were used.
Methods
A qualitative methodology—neglected to date in this area—was adopted for this study, which represented part of a larger overall study that included stakeholders and pharmacy staff17—using semistructured in-depth mainly telephone interviews. Purposive sampling was used, based on a review of the literature,7 to ensure that a range of ages, gender, medicines used, reasons for initial use (genuine or experimental) and treatment and support options were represented. Individuals describing only prescribed medicines were excluded and since the aim was to capture self-perception of OTC medicine addiction, a dependency screening measure was not considered appropriate.18 Recruitment was undertaken via two internet-based support groups for those affected—‘Overcount’ and ‘Codeinefree’. A total of 25 interviews were undertaken (see table 1) over an 18-month period between 2009 and 2010, reflecting a slow uptake to participate. This was considered to be related to the hard to reach nature of this group, and prospective participants often made initial contact to discuss provisions for remaining anonymous in the study. The final sample size was determined by theoretical saturation being achieved in emergent themes. An interview schedule was developed based on a review of the literature7 and since recruitment occurred both before and after addiction warnings were introduced in the UK, participants were either asked for their views about warnings in general or their experiences or views of the actual change, respectively.10 Interviews were conducted by telephone in all but two cases, and were digitally audio recorded and then fully transcribed and anonymised. Analysis of transcripts involved an initial process of open coding, which was also informed by the themes from the available literature7 and the interview schedule. Axial coding between participant transcripts was then undertaken using the constant comparison process which involved reading and re-reading transcripts to identify links between emerging codes and participants and their characteristics. A final process of further refining of themes was undertaken until these provided explanatory accounts of the data. University ethical approval was obtained.
Table 1.
Participant details
| Participant | Sex | Age | Employment | Product | Dose(s) used | Use of medicine at time of study? | Treatment(s) and support used |
|---|---|---|---|---|---|---|---|
| 1 | F | 40s | Housewife | Solpadeine+diverted Solpadol | Varied, up to 12–13/day II | No | ‘Cold turkey’, CF website |
| 2 | F | 60s | Professional | Nurofen Plus | No more than 6/day I | No | CF |
| 3 | M | 40s | Unemployed | Paramol, alcohol and Sudafed for short period | Up to 36/day either 16+16 or 12+12+12 III | No | GP, DAAT (methadone), Overcount |
| 4 | M | ND | Professional | Co-codamol, then Syndol | Up to 8/day I | Yes | GP, CF |
| 5 | M | 30s | Professional | Co-codamol | 12–14/day II | Yes | CF |
| 6 | M | 30s | Professional self-employed | Nurofen Plus+prev. non-opiate illicit substances | Max of 60 tablets/day III | No | GP, DAAT (buprenorphine) CF |
| 7 | F | ND | Former healthcare professional | Solpadeine | Up to 8/day I | No | CF |
| 8 | F | ND | Co-codamol soluble+prescription co-codamol 30/500 | Up to 16/day (max 4/dose) II | No | CFM | |
| 9 | F | ND | Healthcare professional | Nurofen Plus | 32/day (very occ. 64/day) III | No | CF+buprenorphine |
| 10 | F | 30s | University student | Feminax then Cuprofen Plus prev. alcohol | 36/day III | Yes | CF |
| 11 | F | 40s | Professional | Nurofen Plus | 24/day III | No | CF |
| 12 | F | 20s | Professional | Co-codamol+prescribed | Up to 8/day I | No | CF |
| 13 | F | ND | Professional | Co-codamol+prescribed | up to 16/day occasionally+prescribed II | Yes | GP, Overcount |
| 14 | M | 50s | Retired professional | Nurofen Plus+prescribed codeine phosphate | 10/day Nurofen plus+MDD of codeine III | No | Overcount |
| 15 | M | 60s | Professional | Solpadeine soluble | very occasionally 10/day II | No | Private treatment |
| 16 | M | ND | Professional | Phensedyl | 90 bottles/week III | No | GP, DAAT |
| 17 | M | ND | Professional | Panadol Ultra and Nurofen Plus | 15–20 of each III | No | GP |
| 18 | M | ND | ND | Solpadeine | 4/day I | No | Overcount |
| 19 | M | ND | Self-employed | Nurofen Plus | 10/day II | Yes | CF, DAAT, GP |
| 20 | F | ND | ND | Solpadeine | Up to 8/day I | Yes | Overcount |
| 21 | F | ND | ND | Syndol | Up to 8/day I | Yes | CF, GP |
| 22 | M | ND | Former healthcare professional | Codeine linctus, Gees linctus, stolen dihydrocodiene | Varied but much above max daily dose. III | No | CF+DAAT (methadone) |
| 23 | M | 60s | Retired professional | Phensedyl, actifed, codeine linctus diverted prescription codeine | 200 mL codeine linctus/day III | No | CF+GP+DAAT (methadone) |
| 24 | F | 30s | Professional | Syndol+Nytol | Syndol: prev. up to 8/day, now 12/day in last 12 months II | Yes Syndol | Overcount |
| 25 | F | 50s | Professional | Feminax, then Veganin | 6–10/day. Max=12/day II | Yes | Overcount+GP+drug action |
I, consuming less than maximum recommended dose; II, consuming slightly higher than maximum recommended doses; III, consuming significantly higher than maximum recommended doses; CF, CodeineFree (internet support); DAAT, drug and alcohol treatment; F, female; GP, general practitioner (doctor); M, male; ND, not disclosed; Overcount, Internet support.
Results
Analysis of interviews revealed three broad, chronological themes: initial use of the medicine, often linked to genuine medical reasons; awareness of a problem with the medicine over time, with three distinct groups of dose levels being apparent, and finally attempts to seek treatment and help, which were associated with varying degrees of success. All participants described having a problem with an opiate (codeine and occasionally dihydrocodeine), although the stimulant decongestant pseudoephedrine and sedative antihistamines in sleeping medicines or cold remedies were also referred to by some. However, spanning these themes was also a dominant concern relating to the hidden nature of OTC medicine addiction and of participant's presentation of themselves as being normal and distinct from those with other, illicit addictions. This theme will be described along with other themes related to the unproblematic nature of obtaining medicines and views about regulation and responsibility.
Initial use of OTC medicines
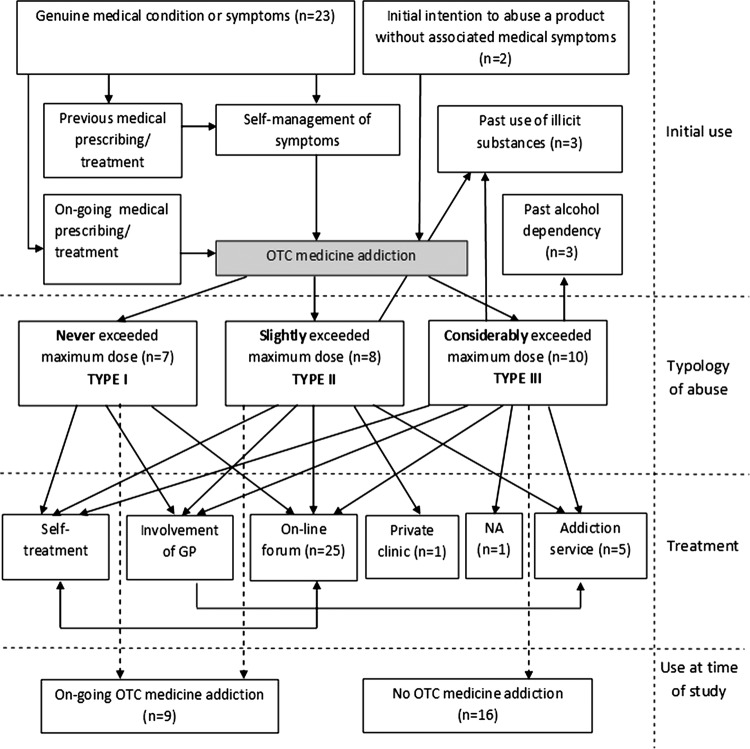
Genuine medical reasons were almost always associated with the initial use of an OTC medicine and due to the involvement of codeine for almost all of these patients; there was not an unexpected range of pain-related symptoms or conditions, including headaches and migraine, abdominal and period pain and hangover treatments. Of note was that there was often an association with medically prescribed medicines, either through initial prescribing that had then stopped or on-going prescribing (figure 1):
I mean my story started by being on painkillers for gynaecological problems and that was when I first took codeine [...] Then I found when I couldn't get codeine on prescription any longer it was readily available over the counter. P9
Figure 1.
Relationship between over-the-counter medicine use and prescribed medicines.
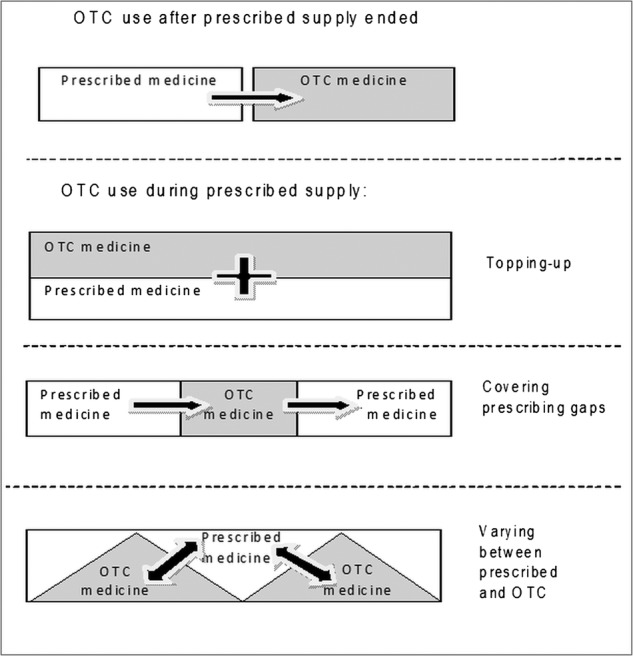
Participants using both prescribed and OTC medicines described either using OTC medicines to cover gaps before a new prescription started, or to allow the strength of medicine used to be varied. In contract, two participants described intentionally experimenting with an OTC medicine—pseudoephedrine and codeine—having been told about their abuse potential by others (see figure 2).
Figure 2.
Summary of different initial use, types of use and treatment.
For all those participants who described a genuine initial use of a product, this led eventually to the medicine being taken for different reasons. The key reason cited related to codeine and while the effect varied, common phrases used were the ‘buzz’ or ‘calm’ associated with its use, although exploiting sedative side effects were also reported by some:
I remember when I took them that it would give you a lift and a buzz, but that lift or buzz would go and the only way to sustain that is to take more. P11
Pseudoephedrine was associated with its stimulant-related side effects and antihistamines like diphenhydramine were used to promote sleep. Participants reflected that abused medicines and particularly codeine allowed them to cope, particularly with significant life events such as bereavements, work or relationship problems.
Obtaining medicines
Participants all described the use of pharmacies to obtain supplies and two also described using internet pharmacies. A key feature of both was how unproblematic it was to obtain medicines, with policies to restrict supplies being perceived to be ineffective, and some pharmacies were considered easier than others to obtain supplies (box 1).
Box 1. Reasons why pharmacy purchases were considered unproblematic.
Many participants, and especially those taking higher doses, varied where they made purchases.
A number of different pharmacies were often located in proximity to participants.
Pharmacy staff often asked questions but seldom challenged participants.
Participants provided responses to pharmacy staff questions that would not lead to challenges.
Occasional references were made to pharmacies that sold multiple packs.
Participants, such as those taking doses less than the maximum, did not need to visit pharmacies often.
Avoiding detection was a key concern for individuals who described intentionally varying the pharmacy used, using ‘schedules, ‘tables’ or ‘lists’ of those visited and lying and fabricating responses to questions from staff:
I had to go to different pharmacies and I didn't want to get knocked back. I would go in and I would make out that I had a toothache, so I didn't know the best thing. I wouldn't directly ask for the product, because I know that was suspicious. P10
Most participants did recall isolated and uncomfortable instances of being challenged; in some cases, resulting in avoiding that pharmacy or visiting less:
I've only ever been challenged once and it was quite a confrontational challenge and…but that was back in the days when I was taking eight a day and […] that one experience kind of altered how I did things. I started pharmacy shopping, I started varying where I went and I started to notice you know the shop workers’ routines. P18
However, several participants considered these challenges to have influenced their attempts to seek help:
I knew it would come sometime but you know to actually face it, that she had actually confronted me with it and that was really a wakeup call for me. P19
Internet pharmacy purchases were mentioned by two participants, who reported being able to obtain multiple quantities repeatedly. Although policies varied between suppliers, questionnaires or identification checks were recognised as being mechanisms that were intended to limit supplies, but which could be easily circumvented. Other participants were cautious of internet medicine supplies and expressed concerns about the lack of safety of such supplies.
Awareness of a problem
The second key chronological theme involved participants becoming aware of having a problem. Strikingly, the words ‘addiction’ or ‘addicted’ were frequently spontaneously used by participants to describe themselves and their situation. Awareness of a problem centred mainly on perceived withdrawal symptoms, although awareness of prolonged consumption over time, critical incidents and a perceived loss of control generally were also identified. Anxiety, generalised pain or headache and gastrointestinal problems were variously described and attributed to the medicine having been stopped:
Yeah I am an addict, no doubt about it. As much as a heroin addict, yeah. Shameful and it makes you feel dirty and guilty, but I was an addict, yeah. Well I have stopped taking codeine before and for the past few days I have had cold sweats and had palpitations and had withdrawal symptoms. So the physical symptoms suggest that I am addicted to it and also the psychological. P10
Critical incidents such as rare instances of being confronted in a pharmacy, medical problem such as a gastrointestinal bleed or illegal activity also appeared to represent moments when participants considered themselves to have a problem. A recurrent theme involved participants’ perceived loss of control over their medicine consumption, either gradually and suddenly and several participants expressed disbelief that addiction could have happened to them, and often drew upon professional, educational status or intelligence claims to argue that they should have had the understanding or insight to prevent this happening.
The role of the two internet support forums—particularly in postings of other individual's descriptions—appeared to be confirmatory of their problem and participants’ use of words like ‘addiction’ and ‘rebound headache’ appeared to have originated from here. Several argued that genetic factors—in references to family members with addictions—might explain their OTC medicine addiction, and several felt that their personality and previous problems—with alcohol misuse for example—were explanatory. In these accounts, participants made explicit and sustained attempts to distinguish themselves from individuals with other addictions and particularly illicit substance users, who they viewed more negatively in both a behavioural and visual sense:
Addicts are people on the street who haven't got a job and I am sat here in a suit in an office, my own office with a very good career, senior manager within a very large organisation and I can't be an addict. I am. P5
A respectable appearance, good employment status and education were often cited as reasons why participants were different, although there was also recognition that their addiction was ultimately the same.
Three types of OTC medicine abuse
A distinction was evident between participants based upon the quantities of medicines taken, with three types emerging (figure 2) which were relative to the recommended maximum doses of specific products. A first group was characterised by self-reported use that never exceeded the recommended maximum dose of a medicine. A second type involved daily doses slightly above the maximum recommended dosage and often involving paracetamol and codeine (500 mg and 8 mg/tablet, respectively) compound analgesics formulations and this occurred sometimes due to combinations of OTC and prescribed medicines. In both these groups, there was awareness of the harms associated with the medicine, and use for non-therapeutic reasons and perceived withdrawal. Such participants often explicitly defended their addiction status, despite the relatively low doses, and appeared aware—usually from posts on internet support groups—of individuals taking much higher doses. Such higher doses represented the third type of consumption identified in this study and was characterised by doses much higher than recommended, with those describing codeine and ibuprofen (12.8 mg and 200 mg/tablet, respectively) compound tablet use, for example, reporting daily consumption between 32 and 64 tablets:
[…] I would take eight in one day. But then of course in increasing amounts. Till the point came that I was taking thirty two a day. Even on really bad days, I would take a second lot of thirty two. P9
Distinct to this group was that three participants had described criminal activity relating to their addiction—convictions for theft being mentioned in two cases—and this group alone was associated with descriptions of significant health problems, including gastric bleeding and hospitalisation following organ damage; significant purchasing costs were also associated with this group. However, despite these more significant issues, this group similarly differentiated themselves from those with other forms of addiction and in two cases referred to their healthcare professional backgrounds to support their claims.
A ‘hidden’ addiction
In describing their situations, individuals often made overt attempts to keep their problem hidden, and this occurred particularly at work where concerns about a perceived change in appearance or behaviour were thought likely to arouse suspicions among colleagues. Of note was that it was the change in appearance that worried participants primarily, and not being seen taking a medicine, which was considered by them to be an everyday activity which would not arouse suspicion in itself. Keeping medicine abuse hidden from family and home environments was also identified, although for a minority, friends and family were aware and had provided support. Many participants also referred to the influence of OTC abuse on their family and relationships more generally, with a tension being apparent in trying to keep OTC addiction secret, but recognising the support that others could offer. For some, family and friends were viewed positively and provided support when a participant was trying to seek treatment, but in other cases much less so
To be honest, I can't discuss it with my family. They simply wouldn't understand. It would be a horror for them. And they don't deal with things like that very well, at all. P6
Treatment and support
The third main chronological theme concerned subsequent attempts by all individuals to address their OTC medicine addiction. These varied considerably and appeared in part related to the quantities of medicine taken (box 1) and included internet support group help in all cases, as well as National Health Service (NHS) medical general practitioner (GP) consultations, specialist NHS drug and alcohol treatment services, a private clinic, counselling, self-management and narcotics anonymous (see figure 2). Perceived benefits of these varied, with initial self-treatment, for example, often being considered ineffective and there was a view that several services, particularly narcotics anonymous and specialist drug services, were not suited to OTC medicine addiction. Participants’ need for anonymity was again evident, with concerns being expressed about addiction being recorded in medical notes and employers and others becoming aware; this extended to the intentional use of pseudonyms by participants on internet support groups. Of note was that pharmacists were not referred to at all in relation to treatment and support.
GP involvement led to both positive and negative comments although some participants had specifically not sought GP advice, due either to poor existing relationships or, linked to the hidden nature of this issue, concerns about their addiction being recorded. Many participants felt that their doctor considered OTC medicine addiction to be less serious than other addictions and something not to be concerned about or suited to simple self-management:
[…] I have mentioned it to the doctor and he sort of said, ‘well it's something you handle yourself’. At this sort of level […] P19
Some GPs had attempted to treat, although experiences suggested this was not successful:
[…] my GP, he tried to detox me with the dihydrocodeine […] I just ended up taking the tablets over a week, you know, that was failure you know. P3
More positively, others described being referred by their GP to specialist drug and alcohol services, and these were associated most often with those taking considerably higher doses of medicine and occurred also from self-referrals and court orders. The overwhelming experience for all participants was that such services were not set up to accommodate those with OTC addiction and several factors were evident. The mixing of clients with different addictions was considered a problem, and there was a perception that staff viewed OTC addiction as a lesser problem, and also lacked experience:
‘I have got a problem with being addicted to co-codomol’. They thought I was being a bit stupid. I think they thought that you know that I should just withdraw slowly. P13
Treatment options involving specific medicines were also viewed problematically, mainly due to their association with illicit drug treatment or having supervised consumption:
I was turning up to [local] drug unit for my daily dose of methadone as though I was a heroin addict […] At that stage, I didn't think that methadone was appropriate. P22
However, the accounts provided from those consuming more significant amounts of opiates suggested that such services, and the use of buprenorphine and methadone, often led to positive outcomes—either on maintenance doses or opiate free—even if concerns were initially apparent about such treatments being inappropriate and suited only for illicit substance misusers.
Self-treatment was often something considered as a first stage, when awareness of a problem had occurred, but it was also attempted as a response to guidance and support from internet support groups. Participants described either stopping completely or reducing the dose gradually:
I went cold turkey as they say. I was on my own in our place […] and I decided that I'd had enough of basically the rounds of going to the doctors and getting the stuff, having problems maybe getting the stuff and then going to different chemists. P14
The two online support groups—Overcount and Codeinefree—appeared to be particularly relevant in attempts to self-treat, and appeared to have been found during general searches of the internet for information about their addiction. The two websites were perhaps the most positively received of all the options available to participants based on their experiences, and provided treatment options, including specific advice with direct communication from website staff and participants and also generic information on the websites and from other's posts. The websites offered a positive confirmatory function for many, as when one participant (P25) noted, ‘there are many more in the same boat, going through the same struggle’ although participants’ level of engagement with the sites varied considerably and while some continued to actively interact, other stopped after the initial confirmatory aspect.
Responsibility and regulation
All participants were asked for their views on how OTC addiction could be prevented, and issues were identified in terms of the overall availability of OTC medicines, the use of information and particularly addiction warnings and the balance between professional and personal responsibility. Of note was that most participants were in favour of the continued availability of OTC medicines with addiction potential and often blamed themselves for their situation. Convenient access to medicines was often argued to outweigh the addiction risks to a minority, and this view was advanced irrespective of the level of consumption by participants:
Everyone should have a choice what they do with their life—as long as they have the awareness of the danger then it’s up to each individual what they do with that information and what path they choose. P25
Analogies were drawn by several to the current availability of other substances that can cause addiction, like tobacco and alcohol, and that their continued availability supported the availability of OTC medicines. A minority felt that the need to avoid harm was paramount and advocated prescription-only availability, although recognising that this may increase doctors’ workloads and NHS costs. The addition of addiction warnings to packets was considered relevant only to those not already addicted:
So I mean it is better than nothing certainly to have a warning on the packet […] and it will put some people off, but the people who need to be put off, I am not sure it would. P14
This view was held by those interviewed both before and after the addiction warnings were introduced and for those still taking OTC medicines at the time of the study, there was a lack of awareness, which one participant (P5) summed up as ‘I've not noticed, but then again I'm not looking’. There was little awareness of regulatory changes relating to pack sizes in the UK from those interviewed after the changes, but a view that, like warnings, these may have some benefit, but only to those who did not already have a problem.
Participants spontaneously raised the issues of responsibility and most felt that they were responsible as individuals, and had decided to use the medicine and should have noticed changes in use. This was often linked to assertions by the participant that they were intelligent and a recurrent theme was the claim that they were controlled individuals, often with successful jobs and graduate and postgraduate university qualifications, and for whom OTC addiction was in some respects atypical:
You know I am not an unintelligent fellow and I have got access to the internet like everybody else. I knew what the consequences were, but I still couldn't stop it. P14
While other factors may have been contributory for a minority—such as pharmacies who continued to supply, or a GP who prescribed inappropriately in one case or post-perative care which did not address analgesic needs—it was ultimately considered a personal cause and resultant problem.
Discussion
Main findings, strengths and weaknesses
The main findings of this study are that perceived OTC medicine addiction arises from often genuine medical reasons linked to prescribing rather than experimentation, and that obtaining medicines appeared unproblematic and treatment options vary in perceived suitability and success. The strength of the study was the use of sampling via internet support groups that enabled the recruitment of a recognised hard to reach group and to allow them to present their experiences in depth in a qualitative empirical study. However, related study limitations are that the sample reflected only those individuals who had internet access and already recognised that they had a problem and that those who had not engaged with these support groups were not represented. In addition, the dominance of codeine among participants may be related to one of the internet support groups targeting only those affected by opiates. Only UK perspectives were presented, although the range of medicines, pharmacy-based supplies and regulations in the UK are broadly similar to those found in many other countries across Europe and also Australia. Analysis of interviews solely by the researcher and hence without either participant or other researcher validation or coding, respectively, represents a further study limitation.
Relevance to existing literature and implications of results
The study provides further evidence that several medicines—opiates, stimulants and sedatives7 8—are implicated in OTC medicine abuse and while illustrating the primacy of codeine as a concern, also highlights that other medicines are abused for non-therapeutic effects. It also indicates that problems can occur in a range of doses, and supports previous research in Australia18 that found both high and low dose dependency although there was less evidence of experimental or recreational use in the present study. The findings suggest that there is a need to raise awareness about the possibility of OTC medicine addiction, not only for prevention but also treatment and support. While previous research has suggested awareness among the public about the abuse potential of medicines, this may reflect terminological confusion over misuse rather than addiction potential19 and so alerting the public to the potential for addiction is necessary, such as through warnings on packets. Raising awareness amongst doctors who prescribe medicines initially is important, since this study suggests that the cessation of prescribed medicines or more complex patterns of concomitant use of prescribed and OTC medicines may be associated with OTC medicine addiction. This, again, reflected often genuine reasons for initial OTC medicine use rather than intentional experimentation. Research has suggested a high level of awareness of OTC medicine abuse potential among GPs but also the need for more training20 and this may be necessary given other concerns that doctors seldom question patient's self-treatment and use of OTC medicines.21 Raising awareness of the distinct nature and concerns of this group is also needed for other healthcare professionals, such as those in addiction services, given concerns in this study, and the literature15 as to the appropriateness of some services. This also applies to pharmacists and particularly since research suggests that they may experience uncertainty about how to support those affected17 This study offers suggestions about possible questions for healthcare professionals such as pharmacists and prescribers, particularly in relation to individuals experiencing more severe self-reported problems. For example, asking if individuals had ever taken more than the recommended maximum dose, if their medicine use had affected their work or social life, or if they felt they had lost control over their medicine use have all emerged from this study. However, it is also of note that pharmacists were not referred to by participants at all in relation to treatment or support in the present study, and this not only reflects previous omissions in the literature5 but also concerns around difficulties in implementing harm-reduction strategies in this setting.7 11 22
Emerging problems for practice
The results of this study reveal a number of tensions that may be problematic in supporting those affected and preventing addiction to medicine. The first involves reconciling individuals’ self-perception of addiction and the need for associated support with doses taken since of the three types of consumption identified, those never exceeding the maximum dose, for example, may have a much lower risk of harm and existing opiate addiction treatments may be clinically inappropriate. This is not to suggest that there are not genuine problems in all three types of consumption identified, and the qualitative nature of this study has revealed detailed accounts of a range of negative experiences of OTC addiction, with issues of shame and adverse effects on health, work and relationships, for example, which are recognised in the wider addiction literature.23 Subtherapeutic dependence has also emerged in other OTC medicine research,18 but such use may arguably also be related to a more perceived loss of control than to therapeutic dependency.18 24 A further and related tension arises in the influence of the internet support groups; while being viewed positively overall and offering important support and treatment advice, this study suggests that they may contribute to a perception in some individuals that they are addicted, even at low doses. This potential widening of the types of addiction in society is an increasing concern25 and one which may also threaten the previous aim of raising awareness among doctors, since this may suggest a wider range of affected patients than might actually require identification and referral for treatment.
A tension also arises in participants’ perception that they are different from those with other addictions and that treatments are not appropriate, and trying to reconcile this with participants’ insight that they have a problem and that existing treatments appear to be effective in some cases. This will require a consideration about how such treatments and services are presented and communicated to individuals, in a way that recognises participants’ anxieties about reporting in medical records and keeping their addiction hidden. There are parallels in this respect with addiction to prescribed medicines and of how to support those affected by these too. A final tension centres on making OTC medicines of potential abuse available to the public—which almost all participants supported—while recognising the potential harms for some individuals. This confirms the importance of choice and recognition moreover of a person who ‘wants autonomy and freedom to choose such medicines’.26
Conclusions
A range of problems have emerged from individuals who experienced addiction to OTC medicines, with distinct dose ranges emerging through often genuine initial reasons for use, via often unproblematic supplies from pharmacies and occasionally the internet, with medical prescribing being associated in many cases. Current treatment and support was not perceived appropriate, and those affected considered themselves different to others with addiction problems. Raising awareness about OTC medicine addiction is needed for the public and also healthcare professionals; providing and communicating treatment options that are sensitive to those affected are needed.
Supplementary Material
Acknowledgments
The author would like to thank all the participants in the study.
Footnotes
Contributors: RJC conceived the idea for the study, and undertook all interviews, analysis and writing of the manuscript.
Funding: This work was supported by a Pharmacy Practice Research Trust Grant.
Competing interests: None.
Patient consent: Obtained.
Ethics approval: ScHARR Departmental Ethics Committee Approval, University of Sheffield.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Anonymised copies of interview transcripts may be obtained upon request from richard.cooper@sheffield.ac.uk.
References
- 1.Bissell P, Ward PR, Noyce PR. The dependent consumer: reflections on accounts of the risks of non-prescription medicines. Health 2001;5:5–30 [Google Scholar]
- 2.Roumie CL, Griffin MR. Over the counter analgesics in older adults: a call for improved labelling and consumer education. Drugs Aging 2004;21:485–98 [DOI] [PubMed] [Google Scholar]
- 3.Bessell TL. Surfing, self-medicating and safety: buying non-prescription and complementary medicines via the internet. Qual Saf Health Care 2003;12:88–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bond CM, Bradley C. Over the counter drugs: the interface between the community pharmacist and patients. BMJ 1996;312:758–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reay G. All-party parliamentary drugs misuse group. An inquiry into physical dependence and addiction to prescription and over-the-counter medication. London: All-Party Parliamentary Drugs Misuse Group, 2009 [Google Scholar]
- 6.Royal College of General Practitioners Addiction to medicines consensus statement January 2013. London: RCGP, 2013 [Google Scholar]
- 7.Cooper RJ. Over-the-counter medicine abuse: a review of the literature. J Subst Use 2013;18:82–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lessenger JE, Feinberg SD. Abuse of prescription and over-the-counter medications. J Am Board Fam Med 2008; 1:45–54 [DOI] [PubMed] [Google Scholar]
- 9.Frei MY, Nielsen S, Dobbin M, et al. Serious morbidity associated with misuse of over-the-counter codeine-ibuprofen analgesics: a series of 27 cases. Med J Aust 2011;193:294–6 [DOI] [PubMed] [Google Scholar]
- 10.Medicines and Healthcare products Regulatory Agency MHRA public assessment report. Codeine and dihydrocodeine-containing medicines: minimising the risk of addiction. London: MHRA, 2009 [Google Scholar]
- 11.Nielsen S, Cameron J, Lee N. Characteristics of a nontreatment-seeking sample of over-the-counter codeine users: implications for intervention and prevention. J Opioid Manag 2011;7:363–70 [PubMed] [Google Scholar]
- 12.Steinman K. High school students’ misuse of over-the-counter drugs: a population-based study in an urban county. J Adolesc Health 2006;38:445–7 [DOI] [PubMed] [Google Scholar]
- 13.Agaba EI, Agaba PA, Wigwe CM. Use and abuse of analgesics in Nigeria: a community survey. Niger J Med 2004;13:379–82 [PubMed] [Google Scholar]
- 14.Akram G. Over-the-counter medication: an emerging and neglected drug abuse? J Subst Use 2000;5:136–42 [Google Scholar]
- 15.National Treatment Agency Addiction to medicine: an investigation into the configuration and commissioning of treatment services to support those who develop problems with prescription-only or over-the-counter medicine. London: NTA, 2010 [Google Scholar]
- 16.Matheson C. Misuse of over-the-counter medicines from community pharmacies: a population survey of Scottish pharmacies. Pharm J 2002;269:66–8 [Google Scholar]
- 17.Cooper RJ. Surveillance and uncertainty: community pharmacy responses to over the counter medicine abuse. Health Soc Care Community 2013;21:254–62 [DOI] [PubMed] [Google Scholar]
- 18.Nielsen S, Cameron J, Pahoki S. Over the counter codeine dependence final report 2010. Victoria: Turning Point, 2010 [Google Scholar]
- 19.Wazaify M, Shields E, Hughes CM, et al. Societal perspectives on over-the-counter (OTC) medicines. Fam Pract 2005;22:170–1 [DOI] [PubMed] [Google Scholar]
- 20.Hughes GF, Bell HM, McElnay JC. General practitioners’ awareness of the appropriate and inappropriate use of over-the-counter products. Pharm J 1999;263:R29 [Google Scholar]
- 21.Britten N. Medicines and society patients, professionals and the dominance of pharmaceuticals. Basingstoke: Palgrave Macmillan, 2008 [Google Scholar]
- 22.Nielsen S, Cameron J, Pahoki S. Opportunities and challenges: over the counter codeine supply from the codeine consumer's perspective. Int J Pharm Pract 2013;21:161–8 [DOI] [PubMed] [Google Scholar]
- 23.O'Connor L, Berry JW, Inaba D, et al. Shame, guilt, and depression in men and women in recovery from addiction. J Subst Abuse Treat 1994;11:503–10 [DOI] [PubMed] [Google Scholar]
- 24.Reith G. Consumption and its discontents: addiction, identity and the problems of freedom. Br J Sociol 2004;55:283–3002 [DOI] [PubMed] [Google Scholar]
- 25.Hacking I. Making up people. In Heller T. C., Sosna M., eds. Reconstructing individualism: autonomy, individuality, and the self in Western thought. Stanford: Stanford University Press, 1987:222–36 [Google Scholar]
- 26.Hanna L, Hughes C. Public's views on making decisions about over-the-counter medication and their attitudes towards evidence of effectiveness: a cross-sectional questionnaire study. Patient Educ Couns 2011;83:345–51 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.