Abstract
Objective
This study tested the hypothesis that wideband aural absorbance predicts conductive hearing loss (CHL) in children medically classified as having otitis media with effusion.
Design
Absorbance was measured in the ear canal over frequencies from 0.25 to 8 kHz at ambient pressure or as a swept tympanogram. CHL was defined using criterion air-bone gaps of 20, 25 and 30 dB at octaves from 0.25 to 4 kHz. A likelihood-ratio predictor of CHL was constructed across frequency for ambient absorbance and across frequency and pressure for absorbance tympanometry. Performance was evaluated at individual frequencies and for any frequency at which a CHL was present.
Study Sample
Absorbance and conventional 226-Hz tympanograms were measured in children of age 3 to 8 years with CHL and with normal hearing.
Results
Absorbance was smaller at frequencies above 0.7 kHz in the CHL group than the control group. Based on the area under the receiver operating characteristic curve, wideband absorbance in ambient and tympanometric tests were significantly better predictors of CHL than tympanometric width, the best 226-Hz predictor. Accuracies of ambient and tympanometric wideband absorbance did not differ.
Conclusions
Absorbance accurately predicted CHL in children and was more accurate than conventional 226-Hz tympanometry.
Keywords: Wideband aural acoustic absorbance, Conductive hearing loss, Tympanometry, Otitis media
INTRODUCTION
Otitis media with effusion (OME) is the most common cause of childhood hearing impairment (Rosenfeld et al., 2004). Medical management of OME aims at remediation of both the fluid in the middle ear and any related conductive hearing loss (CHL). While a comparison of pure-tone air and bone conduction thresholds provides the definition of CHL, an objective method to detect CHL may be helpful when evaluating difficult-to-test populations such as infants, children, and/or patients with developmental disabilities. The aim of the present study was to evaluate the accuracy of wideband (WB) acoustic transfer function measurements in identifying CHL in children.
Background
Tympanometric measurement of acoustic admittance using a 226-Hz probe stimulus is commonly used to evaluate middle-ear function (Margolis & Hunter, 2000). Typically evaluated criteria include tympanometric peak pressure, peak-compensated static acoustic admittance, equivalent volume, and tympanometric width or gradient (ASHA, 1997; Nozza et al., 1994; Shanks et al., 1992). These measures are useful for identifying middle-ear pathologies (Vanhuyse, 1975; Margolis & Hunter, 2000) including OME. However, the relationships between tympanometric measures and degree of CHL are not clear cut (Lildholdt et al., 1979; Margolis et al. 1994; Medical Research Council (MRC), 2009a). Studies relating tympanometric measures and CHL have produced test sensitivities ranging from 58 to 95% and specificities ranging from 37 to 91% (Dempster & MacKenzie, 1991; MRC, 1999), with the highest combined values of sensitivity and specificity of 88% and 84%, respectively (MRC, 2009b). Difficulties in identifying CHL may stem from insensitivity of the tympanometric measure, the variety of middle-ear pathologies and the varying degrees of CHL that they cause (Fria et al., 1985).
Energy reflectance (Stinson et al., 1982; Hudde, 1983) is approximately independent of the depth of the probe insertion and interpretable over a wider frequency range than acoustic admittance, inasmuch as admittance varies with probe location within the ear canal. For an incident transient sound presented in the ear canal and directed towards the tympanic membrane, absorbance is the ratio of the energy absorbed by the middle and external ear relative to the total energy of the incident sound. If the ear-canal walls absorb negligible sound energy compared to the tympanic membrane, then absorbance is the fraction of incident sound energy absorbed by the middle ear. Through conservation of energy, absorbance and energy reflectance are related by the fact that absorbance is one minus the energy reflectance; absorbance is dimensionless and varies between 0 and 1. The use of absorbance has these different properties from energy reflectance: (1) absorbance is large at frequencies for which the middle ear is efficient in collecting sound energy, and (2) absorbance and 226-Hz admittance magnitude tympanograms have single-peaked responses below 2 kHz in a healthy adult middle ear. Both responses are approximately independent of probe-insertion depth.
At ambient pressure, energy reflectance and related acoustic transfer functions such as admittance have been measured in normal-hearing adults (Keefe et al., 1993; Voss & Allen, 1994; Feeney & Sanford, 2004; Shahnaz & Bork, 2006), children and infants (Keefe et al., 1993; Vander Werff et al., 2007; Hunter et al., 2008a; Hunter et al., 2008b), and newborns (Keefe et al., 2000; Sanford et al., 2009; Hunter et al., 2010). Energy reflectance changes when middle-ear disorders exist, including OME, otosclerosis, ossicular discontinuity, and tympanic-membrane perforation (Piskorski et al., 1999; Feeney et al., 2003; Allen et al., 2005; Shahnaz et al., 2009; Voss et al., 2001). WB energy-reflectance tympanometry, with energy reflectance as a joint function of frequency and air pressure (Keefe and Levi, 1996), reveals more information than energy reflectance at ambient pressure (Margolis et al., 1999; Sanford & Feeney, 2008).
The following studies used WB acoustic transfer function testing in children to predict CHL or to predict OME in which a CHL was used in the inclusion criteria for OME. Piskorski et al. (1999) evaluated the performance of conventional 226-Hz tympanometry and ambient WB measurements (energy reflectance and admittance) in predicting CHL in children of ages 2 to 10 years. Multivariate WB tests performed better than any univariate predictor (tympanometric or frequency-specific WB measures) in predicting CHL in some of their test conditions. Piskorski et al. proposed that a WB tympanometry test based on an aural acoustic transfer function, such as absorbance, may be desirable for diagnostic applications, but did not evaluation this conjecture. The present study investigates this idea by directly comparing the accuracy of tympanometric and ambient WB measurements in predicting CHL in children.
Keefe and Simmons (2003) reported that CHL in older children and adults was more accurately predicted by WB tympanometry than 226-Hz tympanometry (static acoustic admittance) and ambient WB acoustic transfer functions. This is the only study that used WB tympanometry to predict CHL, although a limitation of the methods is that the WB tympanogram was measured at a set of 17 fixed air pressures over a 500 daPa range rather than as a pressure sweep as typically used in clinical practice. This undersampling of air pressure limited the measurement precision at those pressures at which the tympanometric response was rapidly varying, and test duration was 40 s, which may be too long for screening applications. Beers et al. (2010) performed WB reflectance testing on normal-hearing children and children with OME of ages 3 to 12 years. Ears were included in the OME group based on a combination of elevated air-conduction thresholds, absent otoacoustic emissions, abnormal impedance results, and bone-conduction testing to confirm presence of CHL. Children with OME had increased energy reflectance relative to normal-hearing children. Beers et al. concluded that energy reflectance at 1.25 kHz was more accurate than conventional 226-Hz tympanometry.
Few previous studies have quantitatively assessed the ability of ambient WB acoustic transfer functions to predict CHL in children at risk for OME, and no study has evaluated the ability of WB tympanometry to predict CHL in this age group. The present study tested the extent to which ambient and tympanometric WB acoustic transfer function tests predict CHL in children.
METHODS
Equipment
WB acoustic transfer function measurements were performed using prototype hardware provided by Interacoustics consisting of a computer, 24-bit soundcard (CardDeluxe, Digital Audio Labs), and pressure pump (modified by Interacoustics from its AT235 device). Custom software was used for stimulus generation and data acquisition. A receiver in the ear-canal probe presented a repeated sequence of acoustic clicks, and a microphone measured ear-canal sound pressure over a bandwidth 0.22 to 8 kHz. Plastic ear tips provided a hermetic pressure seal in the ear canal. A pressure pump, attached to a separate port in the probe, was used to vary ear-canal pressure. A calibration procedure was performed daily prior to data acquisition. More detailed descriptions of the WB equipment and the stimulus-generation and calibration procedures are given in Liu et al. (2008) and Sanford et al. (2009). WB tympanograms were measured using a descending pressure sweep from +200 to −300 daPa at a rate of 100 daPa/s (Liu et al.2008).
Standard 226-Hz tympanograms were obtained with a GSI Tympstar middle-ear analyzer. Pressure was swept from +200 to −300 daPa at a rate of 200 daPa/s. Peak-compensated static acoustic admittance magnitude and tympanometric width (TW) were analyzed. TW was defined as the pressure width at ½ of its peak amplitude relative to its positive tail, except that the TW of a flat tympanogram was coded as 500 daPa, which equaled the total pressure range of the tympanometry sweep. This procedure preserved the rank order that a flat tympanogram had a larger TW than any other type of tympanogram, yet provided a numerical value of TW for each ear.
Participants
Data were obtained from children identified with CHL and a Control group of children without CHL. Both groups were matched in age with nearly equal distributions of right and left ears, and of males and females. Data collection was governed by a research protocol approved by the institutional review board of Boys Town National Research Hospital (BTNRH). Behavioral air-conduction thresholds were measured at octave frequencies from 0.25 to 8 kHz, and BC thresholds were measured (with masking as needed) at octaves from 0.25 to 4 kHz.
Control Group
Twenty-six participants (43 ears) were included in the Control group (age range 2.6 to 8.2 yrs, mean 5.5 yrs, standard deviation (SD) 1.3 yrs). Subjects in the Control group had no otitis media within the last 6 months, no history of pressure-equalization tubes, audiometric air- and bone- conduction thresholds ≤ 15 dB HL, and air-bone gaps (ABGs) ≤ 15 dB.
CHL Group
Participants with CHL were recruited from children receiving services at BTNRH. Audiological data were acquired as part of each child’s clinic visit. Twenty-four participants (35 ears) were included in the CHL group (age range 3.5 to 8.2 yrs, mean 5.1 yrs, SD 1.5 yrs). Complete audiometric data were not acquired for some children due to insufficient child cooperation, although BC thresholds were always measured at 0.5 kHz and at least one other frequency, and usually obtained at all frequencies. Participants were included in the CHL group based on the following criteria: (1) ABG ≥ 20 dB for at least one frequency, and (2) otitis media judged to be the probable cause of CHL.
WB Acoustic Transfer Function Responses
Each ambient WB acoustic transfer function was measured at frequencies from 0.22 to 8 kHz, and averaged into 60 1/12th-octave frequency bins from 0.25 to 8 kHz. A transfer-function test includes measurements of absorbance and admittance. The complex admittance can be represented either in terms of magnitude and phase, or conductance and susceptance. The latter pairs were used to assess whether the complex admittance response was a more accurate predictor of CHL than either the admittance magnitude or phase considered singly. Preliminary analyses showed that predictors based on WB acoustic transfer function had similar accuracy, but absorbance usually had the best overall performance. In particular, no admittance function was a significantly better predictor than absorbance for any condition. Consequently, detailed WB results are presented only for absorbance.
Each WB absorbance tympanometry response was measured as a joint function of air pressure (−300 to +200 daPa) and frequency (0.22 to 8 kHz), and analyzed into a grid of air pressures in 5-daPa increments and the same set of frequency bins as the ambient WB absorbance.
Data Analyses
A potential benefit of measuring a WB response is to obtain information across a wider frequency range than is possible with conventional clinical tests, but a suitable predictor of CHL must be constructed. The method used here was to calculate for each ear the most likely group from which it was selected (Control or CHL). A log likelihood ratio (Van Trees, 1967) was calculated for each individual ear response based on the sample population means and standard errors (SEs) of the mean for Control and CHL groups. The multivariate inputs of the log likelihood ratio were the ambient response across all frequencies, and the tympanometric response across all frequencies and air pressures. The log likelihood ratio output classified each ear as normal or having a CHL, and its application to hearing testing is further described in Sanford et al. (2009), except for a change resulting from the analysis of responses in small CHL groups (with as few as 4 ears). Such groups might include data in a test ear with zero absorbance at a particular frequency and pressure, which would lead to a calculated mean absorbance and SE of zero. Any SE of zero posed a numerical problem in calculating the log likelihood ratio predictor, which was avoided by setting SE at all frequencies and pressures to the larger of either the calculated SE or 10−6.
Comparing Test Performance
Clinical decision theory (Swets, 1988), including the use of receiver operating characteristic (ROC) curves, was used to evaluate the accuracy of a diagnostic test in classifying each test ear as normal or having a CHL. The area under the ROC curve (AUC) was used as a summary statistic to quantify test accuracy. The point of symmetry (SYM) on the ROC curve at which the sensitivity and specificity are most nearly equal (Pepe, 2003) was also used as a summary statistic. AUC and SYM values of 0.5 represent chance performance, and values of 1 represent ideal performance. SYM summarizes test accuracy for the case in which both a high sensitivity and a high specificity are equally desirable. ROC curves were analyzed for each of six frequency conditions: a CHL at one octave frequency from 0.25 to 4 kHz, and a CHL at any octave frequency between 0.25 and 4 kHz. AUC and SYM for each frequency criterion were calculated non-parametrically for three ABG criteria (ABG ≥ 20, 25 and 30 dB).
Several hearing-screening and diagnostic- testing studies have used ROC curve analyses to estimate test accuracy using middle-ear tests to detect CHL (Piskorski et al., 1999; Keefe and Simmons, 2003; Beers et al., 2010), and to detect middle-ear dysfunction in infants (Keefe et al., 2003a; Keefe et al., 2003b; Sanford et al., 2009; Hunter et al., 2010) and adults (Shahnaz et al., 2009). None of these studies, however, reported the statistical significance of any difference in accuracy between multiple tests using a ROC summary statistic.
Statistical significance at the 0.05 level was used in the present study to determine whether a particular test was more or less accurate than any other test according to the difference in their AUC and SYM statistics. The bootstrap procedure is a computational approach to estimate the variability of any statistic calculated from sampled data (Efron and Tibshirani, 1986), whether a mean value or, as in the present study, AUC (and SYM). In contrast to assuming any theoretical distribution of AUC, its distribution was calculated by resampling the measured data and recalculating AUC for that resampling. Resampling is performed using the measured sample distribution of test results in N ears: a new sample of N test results is randomly sampled with replacement from this sample distribution. A key concept in the bootstrap is that the operation of resampling with replacement effectively uses the empirically measured data distribution as the estimate of its underlying unknown distribution. When using the bootstrap to estimate the confidence interval (CI) of a statistic, the number of bootstrap replications was recommended to be at least B=1,000 (Efron and Tibshirani, 1986). This is mainly because one must estimate the 2.5% and 97.5% tails of a distribution to calculate the 95% CI used in the present study. The bootstrap calculation of a CI is improved in accuracy by using a bias-corrected and accelerated method (Efron, 1987), and this method was used in the present study. The number of bootstrap replications has more recently been recommended to be B=4,000 (Efron, 2000). Data were analyzed using the Matlab Statistics Toolkit using B=10,000 bootstrap replications to provide a margin of sufficiently large B.
In each bootstrap replication, significance was tested by calculating AUC for each pair of tests to determine their difference ΔAUC. If the resulting 95% CI of ΔAUC included zero, then the AUCs for these tests were the same (i.e., the null hypothesis was satisfied that the pair of tests had the same AUC). Otherwise, the AUCs were significantly different according to whether the CI of ΔAUC was entirely positive or negative. Separate bootstrap calculations were performed for each pair of tests, e.g., WB ambient absorbance and TW from the 226-Hz tympanogram, and over each of 18 conditions (i.e., for six frequency conditions on defining the CHL and three ABG criterion levels).
CIs were calculated for each of AUC, SYM, ΔAUC and ΔSYM. Any CI of AUC or SYM with a lower bound larger than 0.5 would demonstrate that the test performed better than chance. Because multiple tests (i.e., WB and 226-Hz tympanometry tests) were performed on each ear, their AUC and SYM values were correlated across tests. A particular bootstrap replication resulting in a larger estimate of AUC on one test would likely be associated with a larger estimate of AUC on another test, and similarly for replications with smaller estimates of AUC. Thus, the calculated CIs on AUC (and SYM) would be large, but the correlation across tests in the same ear would tend to obscure the difference in AUC between each test. That is the rationale for using the bootstrap method to calculate ΔAUC for each pair of B tests. Bootstrapping to calculate significant differences is recommended for any ROC summary statistic by Pepe (2003, pages 99–113).
RESULTS
Ambient Absorbance
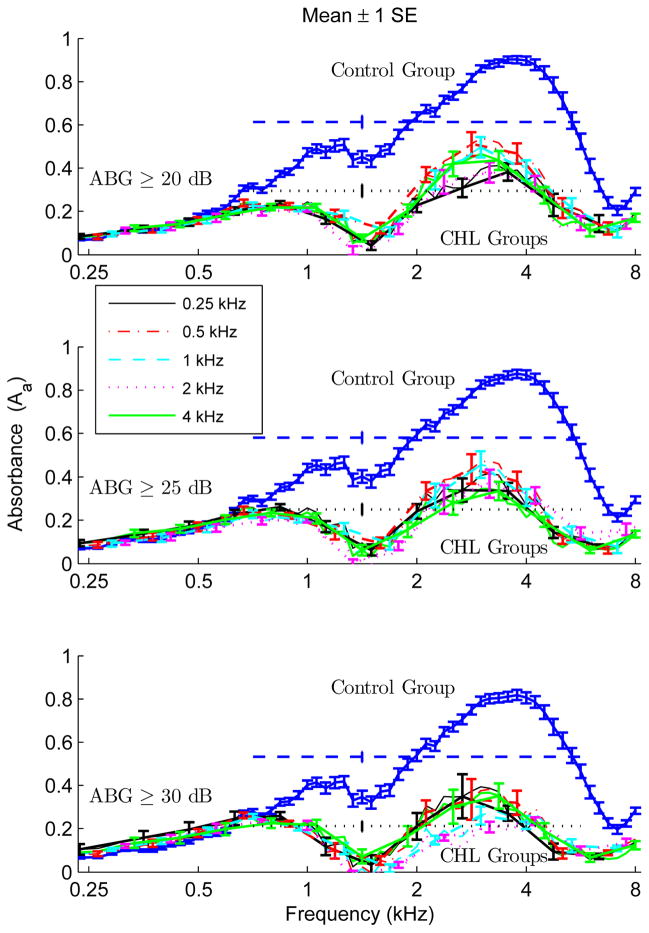
To examine the distribution of ambient absorbance in CHL and Control groups, the means and SEs are plotted versus frequency in Fig. 1. Separate curves in each panel show data for CHL groups based on criterion ABGs at 0.25, 0.5, 1, 2 and 4 kHz. Across all ABGs, the ambient absorbance was larger in the Control group than in any of the CHL groups over a broad frequency range. This effect was clearly evident in the much larger frequency-averaged absorbance in the Control group compared to the group with a CHL at any frequency. Second, the relative difference in ambient absorbance between any pair of CHL groups was much smaller than the difference between the Control group and any CHL group. Ambient absorbance for the group with a CHL at any frequency (not plotted) was in the range of the ambient absorbance plotted for the other CHL groups. Third, the ambient absorbance for the CHL groups varied inversely with the magnitude of the ABG criterion. That is, absorbance was largest for the Control group, but was also trended to slightly larger values for CHL groups with smaller amounts of CHL.
Figure 1.
The mean absorbance is plotted versus frequency for the text-labeled Control group and for each CHL group based on single-frequency ABGs as specified in the legend. Each error bar denotes ±1 SE from the mean. Based on a frequency average from 0.71–5.6 kHz, the mean absorbance of the Control group is plotted in a dashed line and of the CHL group at any frequency is plotted in a dotted line, with single error bars to represent ±1SE from the mean. Results are shown for criterion ABG levels of 20 dB (top panel), 25 dB (middle panel) and 30 dB (bottom panel).
These results demonstrate that the middle ear was less efficient at collecting sound energy at frequencies above 0.7 kHz when a CHL was present. Below 0.6 kHz, the mean ambient absorbance was similar between the Control group and all CHL groups for all ABG criterion values, making measurements at these low frequencies less informative. A horizontal dashed line shows the mean absorbance (with ±1SE) of the Control group averaged from 0.7–5.6 kHz. A horizontal dotted line shows the mean absorbance (with ±1SE) of the CHL group at any ABG frequency. The mean absorbance of that CHL group was less than one half the mean absorbance of the Control group, with no overlap between groups between about 0.8 kHz and 8 kHz.
The finding that ears with a CHL at 0.25 kHz had reduced absorbance at frequencies above 0.7 kHz is evidence that the relationship between the frequency of the CHL and the test frequency was not one-to-one. Acquisition of data in the same test ears at differing frequencies of CHL may have contributed to this relationship, because the presence of CHL at one frequency may have been related to the presence of CHL at another frequency in the same ear. The correlations calculated from the audiometric data across all subjects are listed in Table 1. The ABGs at pairs of frequencies were always positively correlated, with correlations ranging from as low as 0.54 between the 0.25 and 2 kHz ABGs, to as high as 0.83 between the 1 and 4 kHz ABGs. Thus, the absorbance may have been reduced across a wide frequency range in a particular ear because the subject’s ABGs in that ear were also elevated across a correspondingly wide frequency range. The ability of absorbance to predict a CHL between 1 and 4 kHz may have contributed to predicting a CHL at 0.25 and 0.5 kHz due to this correlation between CHLs, even though the mean absorbance of the Control and CHL groups overlapped at lower frequencies.
TABLE 1.
Correlations between air/bone gap measurements across all subjects at each octave frequency
| Correlations Between Air-Bone Gaps | |||||
|---|---|---|---|---|---|
| Frequency (kHz) | 0.25 | 0.5 | 1.0 | 2.0 | 4.0 |
| 0.25 | 1.00 | 0.78 | 0.73 | 0.54 | 0.74 |
| 0.5 | 1.00 | 0.84 | 0.70 | 0.77 | |
| 1.0 | 1.00 | 0.69 | 0.83 | ||
| 2.0 | 1.00 | 0.72 | |||
| 4.0 | 1.00 | ||||
Absorbance Tympanometry
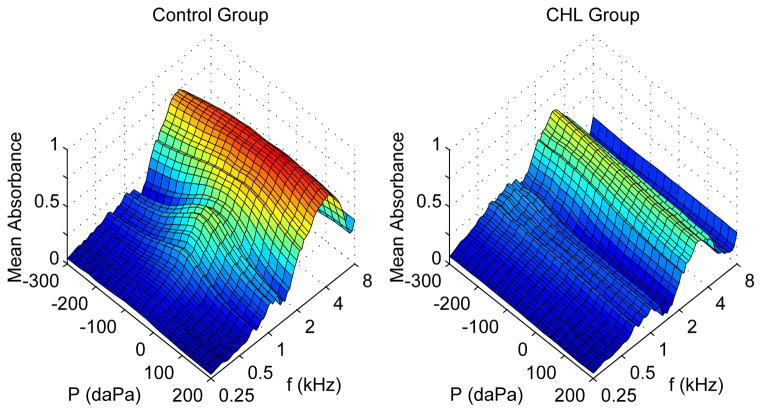
In contrast to admittance tympanometry, a measurement of an absorbance tympanogram, for which the WB response in plots is denoted as At, does not require any compensation for acoustic effects related to the volume of air enclosed between the probe and tympanic membrane. Figure 2 shows results for the mean tympanometric absorbance in the Control group (left panel) and the CHL group (right panel) using the ABG criterion ≥20 at any frequency (the group with the smallest ABGs among the groups with CHL). Across all frequencies and pressures, the maximum SE of the tympanometric absorbance was 0.0025 for the Control group and 0.0011 for the CHL group. Each SE was small compared to the minimum of the mean tympanometric absorbance across all frequencies and pressures. This minimum absorbance was 0.0384 for the Control group and 0.0458 for the CHL group.
Figure 2.
WB tympanograms for mean absorbance are plotted versus tympanometric pressure and frequency for the Control group (left panel) and the CHL group (right panel) based on a criterion ABG of 20 dB at any frequency.
The mean tympanometric absorbance was larger in the Control group than the CHL group at frequencies above 0.7 kHz. The maximum mean tympanometric absorbance was 0.87 in the Control group compared to 0.61 in the CHL group. An absorbance tympanogram varying over pressure and frequency may be interpreted as a set of measured absorbances varying over pressure, with each “slice” measured at the same frequency. The pressure variation in tympanometric absorbance at fixed frequencies down to 0.25 kHz is similar to the pressure variation in a 226-Hz admittance tympanogram inasmuch as 0.25 kHz is only 11% larger than 226 Hz. In contrast, it is the higher frequencies in tympanometric absorbance that are important for predicting CHL; this high-frequency response is absent in conventional tympanometry at 226 Hz. With respect to frequency variation, both the ambient and tympanometric absorbance typically showed a single peak in ears with normal middle-ear function. This single-peak structure was evident in the mean absorbance of the Control group at 0.25 kHz and higher frequencies. An absorbance tympanogram varying over pressure and frequency may also be interpreted as a set of measured absorbances varying over frequency, with each “slice” measured at the same pressure, e.g., the ambient pressure or tympanometric peak pressure. The frequency variation in tympanometric absorbance at any fixed pressure is similar to the frequency variation in ambient absorbance at ambient pressure.
While not shown, the mean tympanometric absorbances in all other CHL groups across ABG frequency conditions were reduced compared to the mean tympanometric absorbance in the Control group above 0.7 kHz. This was similar to the pattern observed for ambient absorbance in Fig. 1. Also, the difference between the mean tympanometric absorbance in any pair of CHL groups was small compared to the difference between the Control and CHL groups. Whether measured at ambient pressure or as a tympanometric sweep, the presence of a CHL was associated with a reduction in power absorbed by the middle ear.
Comparison of Test Performance in Detecting a CHL
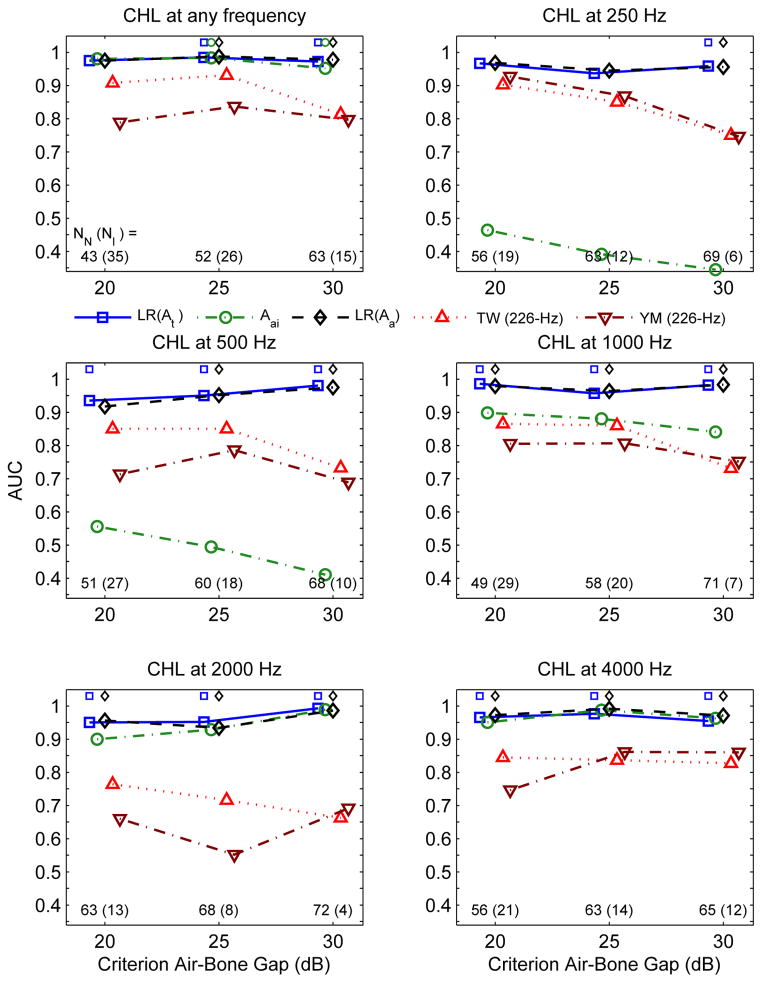
The accuracy of each predictive test was evaluated across the range of definitions of CHL. The predictive tests for CHL based on the ABG at a single octave frequency included: (1) the log likelihood ratio of ambient absorbance denoted as (LR (Aa)), (2) the iso-frequency ambient absorbance (Aai) at the center frequency of the 1/12th octave equal to the ABG frequency, (3) LR of the absorbance tympanogram (LR (At)), (4) tympanometric width of the 226-Hz admittance tympanogram (TW (226 – Hz)), and the compensated magnitude of the 226-Hz admittance tympanogram (YM (226 –Hz) ). These predictive tests were also performed for CHL based on a criterion ABG at any frequency, except that the iso-frequency ambient absorbance test, which was also denoted as Aai on plots was based on the frequency-averaged absorbance over the bandwidth 0.7–5.6 kHz (this average is shown in Fig. 1). To summarize, Aai is used to denote: (i) an “iso-frequency” predictor when classifying ears as having a CHL at a particular frequency because the test frequency of the absorbance is at the ABG frequency; and (ii) a “frequency-averaged” predictor when classifying ears as having a CHL at any frequency.
Each panel of Fig. 3 shows AUC for a particular frequency condition defining the CHL. Within a panel, each marker represents AUC for a particular test as a function of the criterion ABG. The numbers of Control and CHL ears are listed in the bottom of each panel at each criterion ABG. Results for CHL groups with fewer than 10 ears should be interpreted with caution.
Figure 3.
AUC is plotted for each predictor of CHL at any frequency at which a CHL is present (upper left panel) and at each frequency of CHL (remaining five panels) as a function of the criterion ABG level (in dB) used to define the CHL. Results are shown for predictors: LR (At ) for WB absorbance tympanometry (squares), Aai for iso-frequency ambient absorbance (averaged over 1/6th octave) (circles), LR (Aa ) for ambient absorbance (diamonds), and the predictors for the 226-Hz admittance tympanogram TW (226-Hz) (triangles with up vertex) and YM (226-Hz) (triangles with down vertex). The numbers of ears in the Control group (NN ) and CHL group (NI ) are listed at the bottom of each panel for each ABG level in the format NN (NI ). The cases for which the AUC of LR(At ) is significantly larger than the AUCs of both 226-Hz predictors are shown by a square placed at the top of each panel just above AUC=1. The cases for which the AUC of LR (Aa ) is significantly larger than the AUCs of both 226-Hz predictors are shown by a diamond placed at the top of each panel just above AUC=1. For the CHL at any frequency (upper left panel), the cases for which the AUC of the frequency-averaged ambient absorbance (Aai) is significantly larger than the AUCs of both 226-Hz predictors are shown by a circle placed at the top of each panel just above AUC=1.
Calculations of the CI of AUC showed that the iso-frequency predictor Aai was at chance performance at 0.25 and 0.5 kHz at all ABGs, inasmuch as the CI of AUC included 0.5 (not plotted). All other predictors performed better than chance at classifying ears with CHL. Except for AUC for the iso-frequency predictors at 0.25 and 0.5 kHz, AUC for the TW (226-Hz) predictor was always smaller than AUC for any of the other WB predictors, and especially so for the criterion ABG of 30 dB. The predictors with the largest AUCs were the multivariate absorbance predictors LR (Aa) and LR (At). Results are described for predicting CHL at any frequency, because such a general-purpose hearing screener appears well suited for clinical applications. AUC for LR (Aa) ranged from 0.98 to 0.99 across criterion ABGs, while AUC for LR (At) ranged from 0.97 to 0.98. For predicting a CHL at each of the five octave frequencies at different criterion ABGs using either WB likelihood-ratio predictor, the AUC averaged across the five frequencies ranged from 0.95 to 0.98. The frequency-averaged ambient absorbance predictor (Aai) performed nearly as well as WB likelihood-ratio predictors in classifying ears with CHL at any frequency (upper left panel of Fig. 3). This emphasizes that ears with CHL had reduced absorbance at frequencies from 0.7 to 5.6 kHz.
Although the significance testing of differences between AUCs involved 18 conditions per pair of tests, the overall results were relatively simple to characterize. Regarding the pair of 226-Hz tympanometry tests, the AUC for TW (226-Hz) was usually larger than YM (226-Hz). Their difference in AUC was significant only for 3 of 18 conditions, for which TW was a more accurate predictor of CHL (for a CHL at any frequency at 20 and 25 dB ABG, and a CHL at 500 Hz at 20 dB ABG).
The most clinically meaningful comparisons were the differences in AUC between the 226- tympanometric predictors (TW and peak-compensated static acoustic admittance magnitude) and each of the ambient and tympanometric WB absorbance predictors (denoted LR(Aa) and. LR(At), respectively). No 226-Hz tympanometric predictor was ever significantly larger on AUC than either WB absorbance predictor for any condition. As shown in Fig. 3, WB ambient absorbance was significantly more accurate using AUC than both 226-Hz tympanometric predictors in 14 of 18 test conditions. WB tympanometric absorbance using AUC was significantly more accurate than both 226-Hz tympanometric predictors in 15 of 18 test conditions. For predicting a CHL at any frequency (upper left panel, Fig. 3), the ambient absorbance frequency-averaged between 0.7 and 5.6 kHz (denoted Aai) using AUC was significantly more accurate than both 226-Hz tympanometric predictors in the same 2 of 3 test conditions as the other WB predictors.
The plotted AUC values were similar for the likelihood-ratio predictors of ambient absorbance and tympanometric absorbance in Fig. 3. Consistent with that similarity, the ambient and tympanometric absorbance predictors had no significant differences in AUC for any test condition.
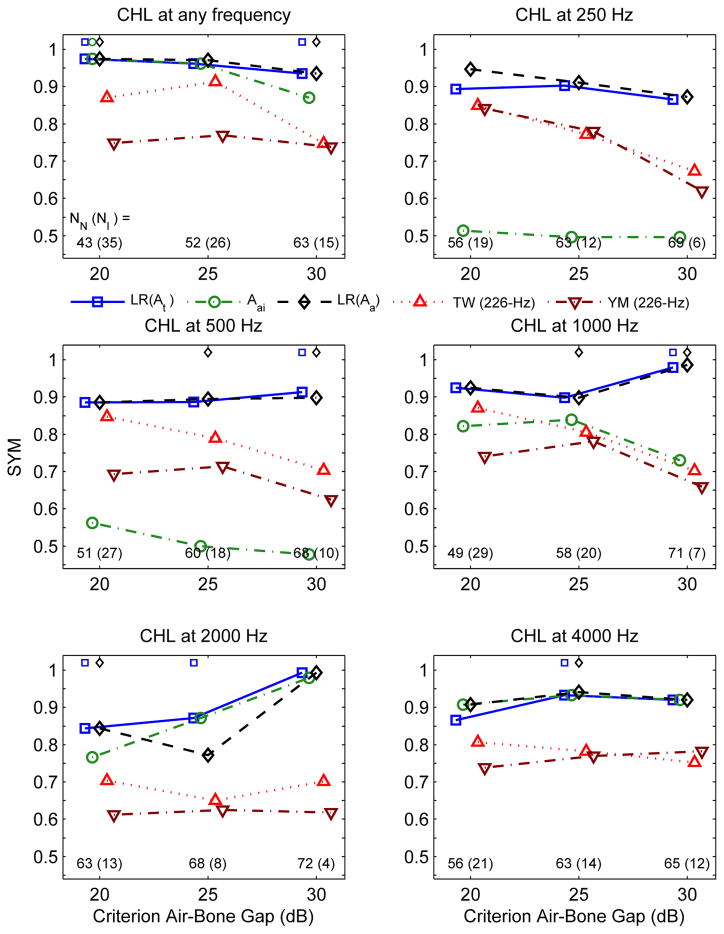
As expected, the overall patterns of test performance for SYM (see Fig. 4) were similar to those for AUC. For predicting CHL at any frequency, SYM for LR(Aa) and LR(At) ranged from 0.93 to 0.97 across criterion ABGs. The SYM comparisons between pairs of tests were less often significant than the corresponding AUC comparisons, and for this reason are presented in summary detail. Regarding the pair of 226-Hz tympanometry tests, SYM for TW (226-Hz) was usually larger than YM (226-Hz). Their difference in SYM was significant only for 3 of 18 conditions, for which TW was a more accurate predictor of CHL WB ambient absorbance was more accurate on SYM than TW (226-Hz) in 10 of 18 test conditions, and more accurate than YM (226-Hz) in 14 of 18 conditions. WB tympanometric absorbance was more accurate on SYM than TW (226-Hz) in 9 of 18 test conditions, and more accurate than YM (226-Hz) in 13 of 18 conditions. The SYM values in Fig. 4 for the WB ambient absorbance and WB tympanometric absorbance were similar and ranged from 0.84 to 0.99.
Figure 4.
SYM is plotted for each predictor of a CHL at any frequency at which a CHL is present (upper left panel) and at each frequency of CHL (remaining five panels) as a function of the criterion ABG level (in dB) used to define the CHL. The formats of the SYM plots, the numbers of test ears and the significant differences in SYM are the same as the corresponding formats of the AUC plots in Fig. 3.
Concerning the comparative accuracy based on SYM, no 226-Hz tympanometric predictor was significantly more accurate than either WB absorbance predictor for any condition. In general, SYM was less sensitive to test differences than AUC. As shown in Fig. 4, WB ambient absorbance was significantly more accurate using SYM than both 226-Hz tympanometric predictors in 8 of 18 test conditions. WB tympanometric absorbance using SYM was significantly more accurate than both 226-Hz tympanometric predictors in 7 of 18 test conditions. For predicting a CHL at any frequency (upper left panel, Fig. 4), the ambient absorbance frequency-averaged between 0.7 and 5.6 kHz (denoted Aai) using SYM was significantly more accurate than both 226-Hz tympanometric predictors in 1 of 3 test conditions.
Consistent with the similarity in SYM, the WB ambient and tympanometric absorbance predictors had no significant differences in SYM for any test condition.
DISCUSSION
Screening for CHL and Guidelines for Managing Patients with OME
This study addressed the problem of detecting CHL using an objective test of middle-ear status in children. An undetected CHL, especially one persisting for a few months, may exist in children with OME. The procedures in this study to detect CHL have advantages over conventional tests to assess middle-ear function. Existing tympanometric procedures based on acoustic admittance are sensitive to probe location within the ear canal at test frequencies above approximately 0.7 kHz due to standing-wave effects, whereas a measurement of acoustic absorbance is insensitive to probe location. Standard clinical procedures to compensate admittance tympanometry with respect to probe location based on the volume of air enclosed between the probe and the eardrum are limited to low frequencies (i.e., 0.226 kHz); however, much of the diagnostic information for CHL was present at higher frequencies (above 0.7 kHz). The WB absorbance test duration is approximately 2–3 s for an ambient test and 5–8 s for a tympanometric test, which takes no more time than current procedures used to assess middle-ear function.
Current clinical practice guidelines in the U.S. recommend that children with OME receive hearing testing whenever a hearing loss is suspected (Rosenfeld et al., 2004). A problem in implementing these guidelines is to determine when a hearing loss is suspected. Existing tests of middle-ear status such as single-frequency admittance tympanometry and acoustic reflectometry do not accurately identify the existence of CHL.
Test Performance of WB Absorbance and 226-Hz Tympanometry
Whether performed at ambient pressure (see Fig. 1) or as a tympanometric pressure sweep (see Fig. 2), WB absorbance was decreased in ears with ABG ≥ 20 dB compared to a control group of children with normal hearing. There was essentially no difference in WB absorbance between the groups at frequencies below 0.6 kHz. This is significant because many tests of middle-ear function use probe frequencies at or below 0.6 kHz, and, therefore, would be expected to be less accurate in identifying ears with CHL.
AUC and SYM were lower for the 226-Hz tympanometric tests (TW and peak-compensated static admittance magnitude) compared to either of the WB absorbance tests in every condition (Figs. 3–4), i.e., no matter how the CHL group was defined. Across all definitions of CHL, AUC ranged from 0.68 to 0.93 for TW at 226 Hz compared to 0.92 to 0.99 for LR(Aa) and 0.94 to 0.99 for LR(At). The increased accuracy of the WB tests compared to 226-Hz tympanometric tests was significant in as many as 15 of the 18 conditions for AUC for WB tympanometric absorbance compared to both 226-Hz tympanometric tests. All WB tests were significantly more accurate than any 226-Hz tympanometry test at detecting a CHL at any frequency for an ABG of 25 dB or more. A lack of significance in a subset of the differences in AUC or SYM between WB and 226-Hz tests was due either to similar predictive performance in any given pair of tests or an insufficient power in the measurements to detect a difference. Measurements using larger groups of subjects would be helpful in better understanding this issue.
The most broadly defined CHL group was the group with a CHL at any frequency (from 0.25 to 4 kHz). An objective acoustical test that accurately identified an ear as having a suspected CHL at any frequency would provide evidence to refer that child for hearing testing. The WB absorbance tests were the most accurate tests in detecting a CHL at any frequency. For example, the likelihood-ratio predictors for WB ambient and tympanometric absorbance had AUCs ranging from 0.97 to 0.99, whereas the predictors for 226-Hz tympanometry ranged from 0.80 to 0.93 (Fig. 3). This is close to ideal test performance for the WB predictors. The likelihood-ratio predictors for WB ambient and tympanometric absorbance had SYMs ranging between 0.93 and 0.97, so that their median SYM represented a correct classification of 96.5% of both normal-hearing and CHL ears. The predictors for 226-Hz tympanometry ranged from 0.74 to 0.91, so that their median SYM represented a classification of only 76% of normal-hearing and CHL ears.
The WB ambient and tympanometric absorbance tests had no significant difference in accuracy based on AUC or SYM for any CHL group. With their accuracies so close to ideal performance, it would require larger groups of test subjects to detect any residual performance difference in these tests if any such difference exists. Either WB ambient or tympanometric absorbance testing is recommended to detect a CHL in a child. Their comparative accuracy in detecting any other form of middle-ear dysfunction is outside the scope of this study.
Concerning the use of the ROC curve summary statistics, AUC was more useful than SYM in detecting a significant difference between tests. This is likely related to the observation that the CIs were larger overall for SYM than AUC. Thus, AUC is the recommended ROC summary statistic for assessing differences in test performance for multiple tests performed on the same subjects. However, SYM has a closer relationship than does AUC to clinical interpretation (Sanford et al., 2009). When comparing a pair of test results for one test randomly selected from the control group and the other test randomly selected from the CHL group, AUC is the probability that the test correctly identifies the ear with CHL. Such a comparison would not be meaningful in clinical terms, inasmuch as the goal of a screening test would be to classify a single ear as either within normal functional limits or having a CHL. SYM is the point on the ROC curve at which the test correctly classifies a similar proportion of normal ears as normal and impaired ears as impaired. This is clinically meaningful, although a tester might choose to preferentially weight a criterion measure to increase the test sensitivity relative to its specificity, or vice versa. Depending on how the CHL was defined, the results on SYM showed an ability across all CHL groups to correctly classify ears using either WB absorbance test with accuracies ranging from 0.84 to 0.99.
The results of the present study might lead one to expect better performance using a probe tone above 0.7 kHz in a single-frequency admittance tympanometry test. However, there is no accepted compensation procedure to remove effects of ear-canal acoustics for admittance tympanograms measured using probe tones higher than 0.7 kHz. This does not pose a problem when using absorbance tympanograms at higher frequencies, because no compensation procedure is needed.
Iso-frequency ambient absorbance was inaccurate at predicting CHL at 0.25 and 0.5 kHz compared to any other predictor. Iso-frequency absorbance was inaccurate at predicting CHL below 0.7 kHz because the absorbance was similar below 0.7 kHz in normal-functioning ears and ears with CHL. Notwithstanding that fact, the likelihood-ratio absorbance predictors were accurate at detecting a CHL at 0.25 and 0.5 kHz based on the pattern of absorbance responses at higher frequencies. These predictors use information from a wide range of frequencies in order to increase the accuracy with which CHL is identified at any frequency. Moreover, these WB tests take no longer to complete than current clinical tests. A simple mean-absorbance predictor, which was defined as the frequency-averaged ambient absorbance between 0.7 and 5.6 kHz, was also accurate at detecting any CHL that might have occurred at 0.25 and 0.5 kHz. This is further evidence that the absorbance above 0.7 kHz conveyed important diagnostic information for detecting CHL at any frequency. A contributor to this across-frequency relationship is the fact that CHLs were positively correlated across frequency in the range from 0.54 to 0.84 (Table 1).
One limitation of the present study is that it did not evaluate how the accuracy of the multivariate absorbance predictors, which were derived using data obtained from one group of subjects, would generalize to a new group of subjects. A concern is that the present multivariate predictors may be idiosyncratic to the present set of data. Additional research on an entirely new group of subjects is needed to assess the validity of these WB absorbance tests in predicting CHL. The potential significance of this concern is partially offset by the fact that WB absorbance was smaller in ears with CHL compared to ears in the Control group over a broad range of frequencies (Figs. 1 and 2) and air pressures (Fig. 2).
WB absorbance accurately classified ears with CHL but did not predict the frequency of the CHL. This does not detract from the clinical utilization of WB absorbance testing to screen for CHL: a patient with an ear classified on the basis of WB absorbance measurements as having CHL would be referred for a comprehensive audiological test to measure the frequencies at which CHL is present and to otolaryngology for medical follow-up and treatment.
Comparisons with Related Studies
AUCs for ambient absorbance were slightly larger in the present study than those reported by Piskorski et al. (1999) for detecting CHL in children based on ambient energy reflectance, although it is not possible to assess whether this difference is significant. The Piskorski et al. study provided evidence that ambient absorbance can detect a CHL with a suggestion of increased detection accuracy when including tympanometry data at 226 Hz. Factors contributing to any difference in test performance might include sampling variability of the subject groups, improved test procedures in the present study, and methodological differences in constructing the multivariate predictors. The present study is an extension of Piskorski et al. in comparing the accuracy of WB ambient and tympanometric absorbance tests in detecting CHL in children, whereas the Piskorski et al. study did not consider any WB tympanometric test. WB ambient and tympanometric tests were highly accurate at detecting CHL, and each was significantly more accurate than 226-Hz tympanometry, but neither WB test was more accurate than the other.
AUCs for ambient absorbance and for tympanometric absorbance were larger in the present study than those reported by Keefe and Simmons (2003), who included subjects from a broader age range (10 to 48 years). Methodological differences may have contributed to differences in test performance, but both studies confirmed the ability of ambient and tympanometric absorbance to detect CHL. The present study used a sweep of air pressure to acquire data in about 5–8 seconds. Keefe and Simmons fixed air pressure at 17 values over a tympanometric range of 500 daPa. This resulted in a longer measurement duration (40 s) and reduced precision in measuring air pressure.
The measured AUC for ambient absorbance was similar in the present study to the maximum AUC of 0.97 reported by Beers et al. (2010) for ambient energy reflectance in children (age 5–7 years). Both studies showed the smallest differences in absorbance at frequencies below 0.6 kHz and increased absorbance in normal ears above 0.6 kHz, although there were several differences between the two studies. Beers et al. required absent otoacoustic emissions, abnormal impedance based on 226-Hz admittance tympanometry, and presence of a CHL for inclusion in what they termed their OME group. A diagnosis of OME was confirmed in half of these ears based on pneumatic otoscopy and video otomicroscopy. The present study used 226-Hz tympanometry as an experimental variable rather than as one component of the inclusion criteria. Some ears with CHL in the present study had 226-Hz tympanograms in the normal range. The studies also differed in procedures used to measure ambient absorbance (or energy reflectance) and to define the predictor variable. Despite these differences, AUC and SYM values were similar in the two studies, which suggest that none of these differences was important. The concurrence in outcomes increases confidence in the ability of WB ambient absorbance to classify ears with CHL.
Using the ROC Curve to Identify Ears with Borderline Results
The decision table for a dichotomous hearing-screening test has four test outcomes (true positive, false positive, true negative, false negative). Accurate screening tests have small false-positive and false-negative rates. A practical problem is that some test results are ambiguous, and a simple pass or refer outcome does not provide a level of confidence of the relative degree of risk for the impairment.
A test outcome of pass represents low probability, or low risk, that the ear is impaired, and corresponds also to a low predictor value (i.e., each predictor measures the probability of impairment of a test ear). A test outcome of refer represents high probability, or high risk, that the ear is impaired, and corresponds to a high predictor value. The ROC curve interprets a test result as to its relative probability that the test ear is normal or impaired. A test outcome of low risk was assigned for an absorbance predictor value lower than a criterion value corresponding to 95% sensitivity. A test outcome of high risk was assigned for a predictor value higher than a criterion value corresponding to 95% specificity. Any ear not classified as either high or low risk was classified as having moderate risk. Using the same criterion value for sensitivity and specificity placed equal importance on reducing error rates in classifying normal and impaired ears. Different specificity and sensitivity criteria would allow one to emphasize the reduction of one type of error relative to the other. However, SYM values in the present study were so close to ideal performance that little would be gained from choosing other criteria.
Results for WB ambient and tympanometric absorbance tests are shown in Table 2. Table 2a shows the standard 2×2 decision tables, i.e., two columns to represent the actual audiometric status as normal or having a CHL and two rows to represent the categorical classification of high or low risk. As one example, the results for the tympanometric absorbance test are described for predicting CHL at any frequency based on a criterion ABG level of 30 dB (see the 2×2 decision table in the lower right part of Table 2a). The test correctly classified 14 of the 15 CHL ears as having high risk for CHL, and correctly classified 58 of the 63 normal ears as having normal function (i.e., low risk for CHL). The false-positive rate was 5 of 63 ears and the false-negative rate was 1 of 15 ears.
TABLE 2.
Numbers of ears classified by the Ambient test LR(Aa) and Tympanometric test LR (At) for a CHL at any frequency at criterion ABG levels specified in left column.
| Table 2a, 2×2 Decision Table. Each ear was classified as high risk if its predictor was less than the predictor at SYM, and low risk otherwise. | |||||
|---|---|---|---|---|---|
| 2×2 Decision Table | Ambient | Tympanometric | |||
| CHL | Normal | CHL | Normal | ||
| ABG ≥ 20 dB | High Risk | 34 | 2 | 34 | 2 |
| Low Risk | 1 | 41 | 1 | 41 | |
| ABG ≥ 25 dB | High Risk | 26 | 1 | 25 | 3 |
| Low Risk | 0 | 51 | 1 | 49 | |
| ABG ≥ 30 dB | High Risk | 14 | 5 | 14 | 5 |
| Low Risk | 1 | 58 | 1 | 58 | |
| Table 2b, 3×2 Decision Table. An ear was classified as high risk if its predictor was greater than the predictor corresponding to 95% specificity, low risk if the predictor was less than the predictor corresponding to 95% sensitivity, and moderate risk otherwise. | |||||
|---|---|---|---|---|---|
| 3×2 Decision Table | Ambient | Tympanometric | |||
| CHL | Normal | CHL | Normal | ||
| ABG ≥ 20 dB | High Risk | 34 | 1 | 34 | 1 |
| Moderate Risk | 0 | 1 | 0 | 1 | |
| Low Risk | 1 | 41 | 1 | 41 | |
| ABG ≥ 25 dB | High Risk | 26 | 1 | 25 | 1 |
| Moderate Risk | 0 | 1 | 0 | 1 | |
| Low Risk | 0 | 50 | 1 | 50 | |
| ABG ≥ 30 dB | High Risk | 11 | 2 | 13 | 3 |
| Moderate Risk | 4 | 7 | 2 | 8 | |
| Low Risk | 0 | 54 | 0 | 52 | |
Table 2b shows the 3×2 form of the decision tables, with each decision table having two columns to represent the actual audiometric status as normal or having a CHL and three rows to represent the categorical classification of high, moderate or low risk. Results are described for the same tympanometric absorbance test with a criterion ABG of 30 dB (see the 3×2 decision table in the lower right part of Table 2b). This test correctly classified 13 of the 15 CHL ears as having high risk for CHL, and correctly classified 52 of the 63 normal ears as having normal function (i.e., low risk for CHL). Of the remaining 13 test ears, 10 were classified as having moderate risk for CHL and would be interpreted as a borderline test status. The other 3 of 63 normal test ears were mis-classified as having high risk for CHL, which takes the role of the false-positive group in a dichotomous test. No ears with CHL were mis-classified as having low risk for CHL, which would take the role of the false-negative group. Compared to a standard 2×2 decision table, the 3×2 decision table reduced these new types of false-positive and false-negative rates at the expense of also reducing the new types of true-positive and true-negative rates. This occurred as a result of the inclusion of the moderate risk, or borderline, test outcome.
Other pairs of decision tables in Table 2 had similar properties. Notwithstanding the complexity of an individual WB absorbance tympanogram, a screening test was constructed that provides an outcome measure quantifying the degree of risk for presence of CHL. The ability to provide an objective definition of a borderline test result has potential for clinical utilization.
Joint Screening for CHL and Middle-Ear Effusion
A companion study (Ellison et al., 2012) assessed the accuracy of ambient absorbance to predict middle-ear effusion in children. Inclusion criteria for the middle-ear effusion group were based on physician findings of fluid at surgery for myringotomy and tube placement. Absorbance was reduced in ears with middle-ear effusion compared to ears in a control group. This finding is consistent with the reduced absorbance in the present study in ears with CHL. The findings from Ellison et al. and the present study support the use of WB absorbance to detect the presence of both OME and CHL. Because the form of the test is the same in the two applications, it would be straightforward to screen for OME and for CHL at the same time using a single test.
CONCLUSIONS
This is the first study comparing WB absorbance at both ambient pressure and in a tympanometric paradigm to typical clinical procedures for detecting middle-ear dysfunction using aural acoustical measurements. The ambient absorbance test used information from a wide range of frequencies (0.25 to 8 kHz), while the tympanometric absorbance test used information from the same range of frequencies and a range of air pressures (−300 to 200 daPa). The test and analysis durations were sufficiently short that either test might be considered as a practical clinical procedure to assess middle-ear function. Both WB absorbance tests accurately predicted the presence of CHL in children, and each was a better predictor of CHL than conventional single-frequency tympanometry. Ears with CHL had reduced absorbance and absorbed power at frequencies between 0.7 and 8 kHz compared to ears with normal hearing. There was no significant difference in the accuracy of ambient and tympanometric predictors derived from WB absorbance testing in detecting CHL in children, and the use of either test would be more accurate than clinical testing based on 226-Hz tympanometry. The finding that no WB test predicted the frequency of the CHL does not detract from its potential use in screening, because evidence of a CHL would provide a basis to refer the child for additional audiological and medical evaluations.
Acknowledgments
The authors are grateful for the assistance of Yi-Wen Liu in software development and analysis. The authors thank the audiology staff of BTNRH for help in recruiting subjects and collecting data. Preliminary results were presented at the American Auditory Society Annual Meeting, March 2010, Scottsdale AZ (C. A. Sanford, D. H. Keefe, J.C. Ellison, D.F. Fitzpatrick, and M.P. Gorga, “Wideband acoustic transfer functions predict conductive hearing loss in children”).
List of acronyms and abbreviations
- ABG
air-bone gap
- AUC
area under the ROC curve
- CHL
conductive hearing loss
- CI
confidence interval
- OME
otitis media with effusion
- ROC
receiver operating characteristic
- SE
standard error of the mean
- SYM
point of symmetry on the ROC curve
- TW
tympanometric width
- WB
wideband
- At
tympanometric absorbance
- Aa
ambient absorbance
- Aai, iso-frequency ambient absorbance re
frequency of ABG
Footnotes
Declaration of Interest
This research was supported by the National Institute on Deafness and Other Communication Disorders (NIDCD grants DC006607, DC000013, DC004662). Douglas H. Keefe is president of Sonicom, Inc., which is a small business aiming to commercialize medical devices including those used for wideband aural acoustic transfer function testing. The NIDCD grant R42 DC006607 was awarded to Sonicom, Inc. as Application Organization with BTNRH as Research Institution. The present address of Chris A. Sanford is Department of Communication Sciences & Disorders, Idaho State University, Pocatello, ID. The present address of John C. Ellison is Research and Development, Starkey Laboratories, Eden Prairie, MN.
References
- Allen JB, Jeng PS, Levitt H. Evaluation of human middle ear function via an acoustic power assessment. J Rehabil Res Dev. 2005;42:63–78. doi: 10.1682/jrrd.2005.04.0064. [DOI] [PubMed] [Google Scholar]
- ASHA. Guidelines for audiologic screening. Rockville, MD: American Speech-Language–Hearing Association; 1997. [Google Scholar]
- Beers AN, Shahnaz N, Westerberg BD, Kozak FK. Wideband reflectance in normal Caucasian and Chinese school-aged children and in children with otitis media with effusion. Ear Hear. 2010;31:221–233. doi: 10.1097/AUD.0b013e3181c00eae. [DOI] [PubMed] [Google Scholar]
- Dempster JH, MacKenzie K. Tympanometry in the detection of hearing impairments associated with otitis media with effusion. Clin Otolaryngol. 1991;16:157–159. doi: 10.1111/j.1365-2273.1991.tb01967.x. [DOI] [PubMed] [Google Scholar]
- Ellison JC, Gorga M, Cohn E, Fitzpatrick D, Sanford CA, Keefe DH. Wideband acoustic transfer functions predict middle-ear effusion. Laryngoscope. 2012;122:887–894. doi: 10.1002/lary.23182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci. 1986;1:54–77. [Google Scholar]
- Efron B. Better bootstrap confidence intervals. J Am Stat Assoc. 1987;82:171–185. [Google Scholar]
- Efron B. The bootstrap and modern statistics. J Am Stat Assoc. 2000;95:1293–1296. [Google Scholar]
- Feeney MP, Grant IL, Marryott LP. Wideband energy reflectance measurements in adults with middle-ear disorders. J Speech Lang Hear Res. 2003;46:901–911. doi: 10.1044/1092-4388(2003/070). [DOI] [PubMed] [Google Scholar]
- Feeney MP, Sanford CA. Age effects in the human middle ear: wideband acoustical measures. J Acoust Soc Am. 2004;116:3546–58. doi: 10.1121/1.1808221. [DOI] [PubMed] [Google Scholar]
- Fria TJ, Cantekin EI, Eichler JA. Hearing acuity of children with otitis media with effusion. Arch Otolaryngol Head Neck Surg. 1985;111:10–16. doi: 10.1001/archotol.1985.00800030044003. [DOI] [PubMed] [Google Scholar]
- Hudde H. Measurement of the eardrum impedance of human ears. J Acoust Soc Am. 1983;73:242–247. doi: 10.1121/1.388855. [DOI] [PubMed] [Google Scholar]
- Hunter LL, Bagger-Sjoback D, Lundberg M. Wideband reflectance associated with otitis media in infants and children with cleft palate. Int J Audiol. 2008a;47(Suppl 1):S57–61. doi: 10.1080/14992020802294057. [DOI] [PubMed] [Google Scholar]
- Hunter LL, Tubaugh L, Jackson A, Propes S. Wideband middle ear power measurement in infants and children. J Am Acad Audiol. 2008b;19:309–324. doi: 10.3766/jaaa.19.4.4. [DOI] [PubMed] [Google Scholar]
- Hunter LL, Feeney MP, Lapsley Miller JA, Jeng PS, Bohning S. Wideband reflectance in newborns: normative regions and relationship to hearing-screening results. Ear Hear. 2010;31:599–610. doi: 10.1097/AUD.0b013e3181e40ca7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe DH, Bulen JC, Arehart KH, Burns EM. Ear-canal impedance and reflection coefficient in human infants and adults. J Acoust Soc Am. 1993;94:2617–38. doi: 10.1121/1.407347. [DOI] [PubMed] [Google Scholar]
- Keefe DH, Folsom RC, Gorga MP, Vohr BR, Norton SJ. Identification of neonatal hearing impairment: ear-canal measurements of acoustic admittance and reflectance in neonates. Ear Hear. 2000;21:443–461. doi: 10.1097/00003446-200010000-00009. [DOI] [PubMed] [Google Scholar]
- Keefe DH, Gorga MP, Neely ST, Zhao F. Ear-canal acoustic admittance and reflectance measurements in human neonates. I. Predictions of otoacoustic emission and auditory brainstem responses. J Acoust Soc Am. 2003a;113:389–406. doi: 10.1121/1.1523387. [DOI] [PubMed] [Google Scholar]
- Keefe DH, Gorga MP, Neely ST, Zhao F. Ear-canal acoustic admittance and reflectance measurements in human neonates. II. Predictions of middle-ear dysfunction and sensorineural hearing loss. J Acoust Soc Am. 2003b;113:407–422. doi: 10.1121/1.1523388. [DOI] [PubMed] [Google Scholar]
- Keefe DH, Levi E. Maturation of the middle and external ears: acoustic power-based responses and reflectance tympanometry. Ear Hear. 1996;17:361–373. doi: 10.1097/00003446-199610000-00002. [DOI] [PubMed] [Google Scholar]
- Keefe DH, Simmons JL. Energy transmittance predicts conductive hearing loss in older children and adults. J Acoust Soc Am. 2003;114:3217–38. doi: 10.1121/1.1625931. [DOI] [PubMed] [Google Scholar]
- Lildholdt T, Courtois J, Kortholm B, Schou JW, Warrer H. The correlation between negative middle ear pressure and the corresponding conductive hearing loss in children. A 12-month study of 352 unselected 7-year-old children. Scand Audiol. 1979;8:117–120. doi: 10.3109/01050397909076310. [DOI] [PubMed] [Google Scholar]
- Liu YW, Sanford CA, Ellison JC, Fitzpatrick DF, Gorga MP, et al. Wideband absorbance tympanometry using pressure sweeps: System development and results on adults with normal hearing. J Acoust Soc Am. 2008;124:3708–3719. doi: 10.1121/1.3001712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis RH, Hunter LL. Acoustic immittance measurements. In: Roeser RJ, Valente M, Hosford-Dunn H, editors. Audiology: Diagnosis. New York: Thieme; 2000. pp. 381–423. [Google Scholar]
- Margolis RH, Hunter LL, Giebink GS. Tympanometric evaluation of middle ear function in children with otitis media. Ann Otol Rhinol Laryngol Suppl. 1994;163:34–38. doi: 10.1177/00034894941030s510. [DOI] [PubMed] [Google Scholar]
- Margolis RH, Saly GL, Keefe DH. Wideband reflectance tympanometry in normal adults. J Acoust Soc Am. 1999;106:265–280. doi: 10.1121/1.427055. [DOI] [PubMed] [Google Scholar]
- MRC Multi-centre Otitis Media Study Group. Sensitivity, specificity and predictive value of tympanometry in predicting a hearing impairment in otitis media with effusion. Clin Otolaryngol. 1999;24:294–300. doi: 10.1046/j.1365-2273.1999.00259.x. [DOI] [PubMed] [Google Scholar]
- MRC Multi-centre Otitis Media Study Group. Air-conduction estimated from tympanometry (ACET) 1: relationship to measured hearing in OME. Int J Pediatr Otorhinolaryngol. 2009a;73:21–42. doi: 10.1016/j.ijporl.2008.09.014. [DOI] [PubMed] [Google Scholar]
- MRC Multi-centre Otitis Media Study Group. Air-conduction estimated from tympanometry (ACET) 2: the use of hearing level-ACET discrepancy (HAD) to determine appropriate use of bone-conduction tests in identifying permanent and mixed impairments. Int J Pediatr Otorhinolaryngol. 2009b;73:43–55. doi: 10.1016/j.ijporl.2008.09.023. [DOI] [PubMed] [Google Scholar]
- Nozza R, Bluestone C, Kardatzke D, Bachman R. Identification of middle ear effusion by aural acoustic admittance and otoscopy. Ear Hear. 1994;15:310–323. doi: 10.1097/00003446-199408000-00005. [DOI] [PubMed] [Google Scholar]
- Pepe MS. The Statistical Evaluation of Medical Tests for Classification and Prediction. Oxford: Oxford Univ. Press; 2003. [Google Scholar]
- Piskorski P, Keefe DH, Simmons JL, Gorga MP. Prediction of conductive hearing loss based on acoustic ear-canal response using a multivariate clinical decision theory. J Acoust Soc Am. 1999;105:1749–64. doi: 10.1121/1.426713. [DOI] [PubMed] [Google Scholar]
- Rosenfeld RM, Culpepper L, Doyle KJ, et al. Clinical practice guideline: Otitis media with effusion. Pediatrics. 2004;113:1412–29. doi: 10.1016/j.otohns.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Sanford CA, Feeney MP. Effects of maturation on tympanometric wideband acoustic transfer functions in human infants. J Acoust Soc Am. 2008;124:2106–22. doi: 10.1121/1.2967864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford CA, Keefe DH, Liu Y, Fitzpatrick DF, McCreery RW, et al. Sound conduction effects on DPOAE screening outcomes in newborn infants: Test performance of wideband acoustic transfer functions and 1-kHz tympanometry. Ear Hear. 2009;30:635–652. doi: 10.1097/AUD.0b013e3181b61cdc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahnaz N, Bork K, Polka L, Longridge N, Bell D, Westerberg BD. Energy reflectance and tympanometry in normal and otosclerotic ears. Ear Hear. 2009;30:219–233. doi: 10.1097/AUD.0b013e3181976a14. [DOI] [PubMed] [Google Scholar]
- Shahnaz N, Bork K. Wideband reflectance norms for Caucasian and Chinese young adults. Ear Hear. 2006;27:74–88. doi: 10.1097/01.aud.0000240568.00816.4a. [DOI] [PubMed] [Google Scholar]
- Shanks JE, Stelmachowicz PG, Beauchaine KL, Schulte L. Equivalent ear canal volumes in children pre- and post-tympanostomy tube insertion. J Speech Hear Res. 1992;35:936–941. doi: 10.1044/jshr.3504.936. [DOI] [PubMed] [Google Scholar]
- Stinson MR, Shaw EAG, Lawton BW. Estimation of acoustical energy reflectance at the eardrum from measurements of pressure distribution in the human ear canal. J Acoust Soc Am. 1982;72:766–773. doi: 10.1121/1.388257. [DOI] [PubMed] [Google Scholar]
- Swets JA. Measuring the accuracy of diagnostic systems. J Acoust Soc Am. 1988;240:1285–1293. doi: 10.1126/science.3287615. [DOI] [PubMed] [Google Scholar]
- Vander Werff KR, Prieve BA, Georgantas LM. Test-retest reliability of wideband reflectance measures in infants under screening and diagnostic test conditions. Ear Hear. 2007;28:669–681. doi: 10.1097/AUD.0b013e31812f71b1. [DOI] [PubMed] [Google Scholar]
- Vanhuyse VJ, Creten WL, Van Camp KJ. On the W-notching of tympanograms. Scand Audiol. 1975;4:45–50. [Google Scholar]
- Van Trees HL. Detection, Estimation, and Modulation Theory. New York: Wiley; 1967. [Google Scholar]
- Voss SE, Allen JB. Measurement of acoustic impedance and reflectance in the human ear canal. J Acoust Soc Am. 1994;95:372–84. doi: 10.1121/1.408329. [DOI] [PubMed] [Google Scholar]
- Voss SE, Rosowski JJ, Merchant SN, Peake WT. Middle-ear function with tympanic-membrane perforations. I. Measurements and mechanisms. J Acoust Soc Am. 2001;110:1432–44. doi: 10.1121/1.1394195. [DOI] [PubMed] [Google Scholar]