Abstract
Background
Few studies have evaluated the long-term outcomes of bariatric surgery patients in relation to obese individuals not participating in weight loss interventions. Our objective was to evaluate the 6-year changes in health-related quality of life (HRQOL) in gastric bypass (GB) patients versus 2 obese groups not undergoing surgical weight loss. The study setting was a bariatric surgery practice.
Methods
A total of 323 GB patients were compared with 257 individuals who sought but did not undergo gastric bypass and 272 population-based obese individuals using weight-specific (Impact of Weight on Quality of Life-Lite) and general (Medical Outcomes Study Short-Form 36 Health Survey) HRQOL questionnaires at baseline and 2 and 6 years later.
Results
At 6 years, compared with the controls, the GB group exhibited significant improvements in all domains of weight-specific and most domains of general HRQOL (i.e., all physical and some mental/psychosocial). The 6-year percentage of excess weight loss correlated significantly with improvements in both weight-specific and physical HRQOL. The HRQOL scores were fairly stable from 2 to 6 years for the GB group, with small decreases in HRQOL corresponding to some weight regain.
Conclusions
GB patients demonstrated significant improvements in most aspects of HRQOL at 6 years compared with 2 nonsurgical obese groups. Despite some weight regain and small decreases in HRQOL from 2 to 6 years postoperatively, the HRQOL was relatively stable. These results support the effectiveness of weight loss achieved with gastric bypass surgery for improving and maintaining long-term HRQOL.
Keywords: Gastric bypass surgery, Health-related quality of life, HRQOL, Cohort trial, Impact of Weight on Quality of Life-Lite, IWQOL-Lite, Medical Outcomes Study Short-Form Health survey, SF-36
Numerous studies have reported the reduced health-related quality of life (HRQOL) of patients seeking bariatric surgery compared with obese individuals seeking nonsurgical weight loss interventions [1,2], obese individuals not seeking weight loss treatment [2], and general population norms [3,4]. Likewise, a great many studies have reported improved HRQOL after bariatric surgery [5]. With few exceptions, the studies of HRQOL outcomes for bariatric surgery patients have not included comparison groups of nonsurgically treated individuals, and, often, the comparison group has received some other type of bariatric surgery [6–9]. Still other studies have used a cross-sectional design [10–12]. Another limitation of many of these studies has been the absence of long-term follow-up (≥5 yr). An important research question is whether early improvements in HRQOL are maintained over time compared with nonsurgically treated obese individuals.
One prospective, nonrandomized intervention study (Swedish Obese Subjects study) evaluated the 10-year HRQOL changes in obese individuals undergoing 3 types of bariatric surgery compared with nonsurgically treated individuals undergoing conventional treatment [1]. At 10 years, significantly better outcomes were shown for several aspects of HRQOL among the surgically treated participants (n = 655) compared with the conventionally treated participants (n = 621) [13]. During the 10-year period, the pattern of change in HRQOL corresponded, for the most part, with the phases of weight loss, weight regain, and weight stability. Peak improvements in HRQOL were observed for the surgical group during the first year of weight loss. However, from years 1 to 6, a gradual decline occurred in HRQOL that corresponded with weight regain. From years 6 to 10, the HRQOL and weight both stabilized, and at 10 years, HRQOL remained improved compared with that at baseline.
A smaller study evaluated long-term HRQOL outcomes (yearly at 3–6 yr postoperatively) for 21 patients who had undergone gastric banding compared with 29 obese individuals who were evaluated for gastric banding but did not undergo the surgery [14]. Statistically significant differences in favor of the surgical group were observed for all domains of the Medical Outcomes Study Short-Form 36 (SF-36) [15] at all assessment points. Although the mean body mass index (BMI) decreased during the entire 6-year period for the gastric banding patients, the scores on the SF-36 were relatively unchanged from 3 to 6 years after surgery.
Other studies have provide evidenced that early improvements in HRQOL after bariatric surgery are maintained during long-term follow-up, regardless of continued weight loss or weight regain; however, none of these studies include comparison groups. For example, both Helmiö et al. [16] and Caiazzo et al. [17] reported no additional improvements in HRQOL from 1 to 5 years after laparoscopic adjustable gastric banding despite increasing weight loss. Suter et al. [18] reported no changes in HRQOL from 1 to 5 years after gastric bypass surgery despite some weight regain.
The Utah Obesity Study is an ongoing prospective study of gastric bypass (GB) patients that includes 2 obese control groups: those seeking gastric bypass surgery who did not undergo the surgery (primarily as a result of insurance coverage restrictions) (no GB) and population-based obese individuals (Pop OB) who did not seek bariatric surgery [19]. The first control group is comparable to those who subsequently underwent gastric bypass surgery and provides an opportunity to study the HRQOL outcomes of obese patients who sought but did not undergo gastric bypass surgery. The second control group allows for inferences about the long-term HRQOL of the general obese subset of the population in relation to those undergoing gastric bypass surgery. In our previous report of 2-year HRQOL outcomes [20], 308 GB patients were compared with 253 individuals who sought but did not undergo gastric bypass (no GB group) and 272 population-based obese individuals (Pop OB) using both weight-specific (Impact of Weight on Quality of Life-Lite [IWQOL-Lite]) [21] and general (SF-36) [15] HRQOL measures. Dramatic improvements were observed in both weight-specific and physical HRQOL for the GB group compared with the control groups. The present study reports the 6-year changes in HRQOL for these 3 groups. In addition, we examined whether the very large improvements in HRQOL observed in the GB patients at 2 years were maintained at 6 years or whether the initial improvements in HRQOL diminished over time, perhaps because of weight regain.
Methods
Participants
The participants were recruited from a bariatric surgery practice in Salt Lake City, Utah, from March 2001 to May 2004 as a part of the Utah Obesity Study [19]. Individuals who were evaluated for and underwent gastric bypass surgery (GB group) were compared with those who sought and were evaluated for gastric bypass surgery but did not have the surgery (no GB) and obese individuals without a history of bariatric surgery randomly chosen from a population database (Pop OB) representing >1 million first-degree relatives from 120,000 Utah families [22–24]. The exclusion criteria for all groups were previous gastric surgery for weight loss, gastric or duodenal ulcers in the previous 6 months, active cancer (with the exception of nonmelanoma skin cancer within the past 5 years), and myocardial infarction in the previous 6 months.
Data for the present study were from participants who completed both HRQOL measures at baseline and ≥1 measure at either the 2- or 6-year assessment. Using these criteria, a total of 323 participants were in the GB group, 257 in the no GB group, and 272 in the Pop OB group. This sample size was slightly larger than that reported in the 2-year HRQOL report [20] because some participants completed the 6-year but not the 2-year assessment. Also, 45 participants from the control groups (37 no GB and 8 Pop OB) underwent gastric bypass surgery between the 2- and 6-year assessment and were analyzed in the GB group at the 6-year assessment to be consistent with the methods used in the primary outcome study.
Methods
On initial evaluation and again at the 2- and 6-year assessments, the participants completed demographic questionnaires and 2 measures of HRQOL. Their height and weight were obtained by study personnel. Weight change was determined by computing the percentage of excess weight loss (%EWL), using the midpoint of the 1983 Metropolitan Life Insurance tables for a medium frame: [(operative weight – follow-up weight)/operative excess weight] × 100.
The university institutional review board approved the study, and all participants provided informed consent. All research was conducted in compliance with the Helsinki Declaration.
Measures
IWQOL-Lite questionnaire
The IWQOL-Lite [21] is a 31-item measure of weight-related quality of life. There are 5 domain scores (physical function, self-esteem, sexual life, public distress, and work) and a total score. The scores for all domains and the total score range from 0 to 100, with lower scores indicating greater impairment. The IWQOL-Lite has demonstrated excellent reliability and validity [21,25].
SF-36 questionnaire
The SF-36 [15] is a 36-item measure of general HRQOL, consisting of 8 subscales (physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health) and 2 summary scores (physical component summary [PCS] and mental component summary [MCS]). The summary scores represent independent (orthogonal) indexes based on factor analysis of subscale scores using the Medical Outcomes Study data [15]. The scores for all subscales range from 0 to 100, where 100 represents the best HRQOL. The scores for PCS and MCS are norm-based, with a mean of 50 and standard deviation (SD) of 10, with higher scores representing better HRQOL. Estimates of internal consistency for the SF-36 have typically exceeded .80 for all subscales across diverse patient groups [26,27].
Statistical analysis
The GB, no GB, and Pop OB groups were compared on baseline demographic and weight characteristics using analysis of variance with Tukey's honestly significant difference [28] post hoc comparisons for age, years of education, weight, and BMI and the chi-square test for gender, marital status, and race. An α of .05 was used for omnibus tests and .0167 (.05/3) for post hoc chi-square comparisons.
Baseline differences in the demographic characteristics and HRQOL scores were compared between participants who did and did not complete the 6-year follow-up assessment separately by group using analysis of variance or the chi-square test. The groups were compared by the %EWL at 6 years using analysis of variance with Tukey's honestly significant difference post hoc comparisons. Pearson's correlations were calculated between the %EWL from baseline to 6 years and the changes in the HRQOL scores. A regression analysis based on a general linear model was used to evaluate the relationship between the %EWL and change in HRQOL scores, controlling for age, gender, baseline BMI, and baseline HRQOL.
Analysis of covariance was used to compare the groups on the changes in the 6-year HRQOL scores, controlling for age, baseline BMI, gender, and baseline scores. An α of .003 (.05/16) was used for omnibus tests and .001 (.003/3) for covariate-adjusted post hoc comparisons. Between-group effect size information for these comparisons is reported in terms of partial eta squared (η2), which expresses the proportion of unique variance in the outcome measure accounted for by group. Within-group effect sizes were calculated as the mean change from baseline to 6 years divided by the baseline SD.
The number and percentage of participants in each group demonstrating meaningful improvement in the IWQOL-Lite total score from baseline to 6 years were calculated using the algorithm described by Crosby et al. [29], in which meaningful improvements are defined as an increase in the IWQOL-Lite total score of 7–12 points, depending on baseline severity. The percentage of patients demonstrating meaningful improvement, no change, deterioration was compared across the groups using chi-square analysis. Finally, analysis of covariance was used to compare groups for the changes in HRQOL scores from 2 to 6 years, controlling for age, baseline BMI, gender, and 2-year scores. Within-group effect sizes from 2 to 6 years were calculated using the baseline SD to allow direct comparisons with the baseline to 6-year effect sizes. All analyses were conducted using the Statistical Package for Social Sciences, version 19.0.0 (SPSS, Chicago, IL).
Results
Baseline demographic and weight characteristics
The baseline characteristics are presented in Table 1. The GB group had a significantly greater weight and BMI than did the no GB and Pop OB groups but did not differ from the no GB on other characteristics. The Pop OB group was significantly older, more likely to be white, and more likely to be married than the no GB group. The groups differed significantly by gender; however, post hoc comparisons revealed no significant pair wise differences.
Table 1.
Baseline demographic and weight characteristics by group
| Characteristic | GB (n = 323) | No GB (n = 257) | Pop OB (n = 272) | Significance* |
|---|---|---|---|---|
| Women† | 271 (83.9) | 217 (84.4) | 209 (76.8) | χ2(2) = 6.66, P = .036 |
| Age (yr) | 43.4 ± 10.7a | 44.7 ± 10.9a | 49.7 ± 10.5b | F2,849 = 27.45, P < .001 |
| Married | 206 (63.8)a,b | 145 (56.4)a | 189 (69.5)b | χ2(2) = 9.75, P = .008 |
| White | 289 (89.5)a | 236 (91.8)a | 266 (97.8)b | χ2(2) = 15.95, P < .001 |
| Education (yr) | 14.2 ± 2.3 | 14.0 ± 2.4 | 13.9 ± 2.3 | F2,806 = .83, P =.44 |
| Weight (kg) | 134.3 ± 27.1a | 128.5 ± 25.6b | 123.0 ± 22.7c | F2,849 = 14.67, P < .001 |
| BMI (kg/m2) | 47.4 ± 7.7a | 45.9 ± 7.9a | 43.6 ± 6.4c | F2,849 = 19.55, P < .001 |
GB = gastric bypass; no GB = obese individuals seeking gastric bypass surgery who did not undergo the surgery; Pop OB = population-based obese individuals not seeking gastric bypass surgery; BMI = body mass index.
Data presented as numbers, with percentages in parentheses, or mean ± standard deviation.
Data without superscript letters are not significantly different at P < .05; data with superscript letters that are not in common are significantly different at P < .05 according to Tukey's honestly significant difference (F test) or Bonferroni (chi-square test).
α Levels for omnibus tests = .05; α levels for post hoc comparisons = .0167 (.05/3).
No pair wise differences between groups using Bonferroni-corrected contrasts.
Six-year HRQOL completion rates
The 6-year HRQOL completion rate was 72.3% overall (616 of 852), 71.2% GB (230 of 323), 64.2% no GB (165 of 257), and 81.3% Pop OB (221 of 272). The GB patients who completed the 6-year assessment were significantly older but did not differ significantly on any other demographic characteristics or baseline HRQOL scores. The Pop OB group completers had a significantly lower BMI and greater IWQOL-Lite scores at baseline. No statistically significant differences were found between the completers and non-completers in the no GB group.
Weight loss
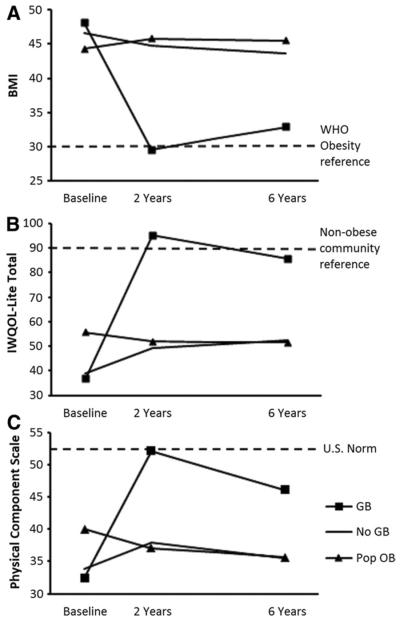
Figure 1A shows the mean BMI adjusted for age, gender, and baseline BMI for each of the 3 groups at baseline and 2 and 6 years compared with the World Health Organization cutoff for obesity [30]. At 2 years after surgery, the GB group had a mean adjusted BMI (29.6 ± 6.4 kg/m2) just below the cutoff for obesity; however, at 6 years, the mean adjusted BMI was in the obese range (32.9 ± 7.4 kg/m2).
Fig. 1.
(A) Mean BMI at baseline and 2 and 6 years, adjusted for age, gender, and baseline BMI. (B) Mean IWQOL-Lite total score at baseline and 2 and 6 years, adjusted for age, gender, and baseline BMI. (C) Mean SF-36 PCS score at baseline and 2 and 6 years, adjusted for age, gender, and baseline BMI. WHO = World Health Organization; GB = Gastric bypass patients; no GB = Obese individuals seeking gastric bypass surgery who did not have the surgery; Pop OB = Population-based obese individuals not seeking gastric bypass surgery.
The average %EWL at 6 years was 56.4% ± 21.4% for the GB group, .3% ± 22.2% for the no GB group, and .2% ± 23.3% for the Pop OB group (F2,614 = 458.09; P < .001; partial η2 = .599; GB greater than no GB equal to Pop OB). The %EWL at 6 years correlated significantly with changes in the IWQOL-Lite total score (r = −.78, P < .001) and SF-36 PCS (r = −.55, P < .001) but did not correlate significantly with the SF-36 MCS (r = −.07, P = .10). After controlling for age, gender, baseline BMI, and baseline HRQOL, the %EWL at 6 years explained 59.0% of the variance for changes in the IWQOL-Lite total score and 28.5% of the variance for changes in the SF-36 PCS.
HRQOL results
IWQOL-Lite questionnaire
Changes in the IWQOL-Lite scores from baseline to 6 years are reported by group in Table 2. The GB group experienced significantly greater improvement than both the no GB and Pop OB groups in all IWQOL-Lite scores. The between-group differences were large, with partial η2 values ranging from .253 (sexual life) to .448 (physical function) for the 5 domain scores and was .473 for the total score. Within-group changes for the GB group were large to very large—ranging from 1.24 (sexual life) to 2.44 (physical function) for the 5 domain scores and was 2.61 for total score. In contrast, the within-group changes for the no GB and Pop OB groups were small to medium.
Table 2.
Changes in IWQOL-Lite and SF-36 by group
| Variable | Baseline* | Change from baseline to 6 yr |
Change from 2 to 6 yr |
||||
|---|---|---|---|---|---|---|---|
| Mean ± SD† | Effect size | Significance | Mean ± SD‡ | Effect size | Significance | ||
| IWQOL-Lite scale | |||||||
| Physical function | F2,605 = 245.23, P < .001, partial η2 = .448 | F2,528 = .49, P = .62, partial η2 = .002 | |||||
| GB | 30.1 ± 18.8 (n = 322) | 45.8 ± 20.1a (n = 229) | 2.44 | −2.3 ± 13.4 (n = 200) | −.12 | ||
| No GB | 33.6 ± 21.0 (n = 257) | 10.0 ± 23.8b (n = 162) | .48 | −4.7 ± 20.3 (n = 127) | −.22 | ||
| Pop OB | 49.1 ± 20.6 (n = 272) | 8.2 ± 18.1b (n = 221) | .40 | −4.3 ± 18.1 (n = 208) | −.21 | ||
| Self-esteem | F2,607 = 137.48, P < .001, partial η2 = .312 | F2,527 = 5.45, P = .005, partial η2 = .020 | |||||
| GB | 30.1 ± 21.1 (n = 323) | 43.9 ± 27.7a (n = 230) | 2.08 | −6.6 ± 21.7 (n = 200) | −.31 | ||
| No GB | 31.4 ± 22.0 (n = 257) | 12.2 ± 21.1b (n = 163) | .55 | −.3 ± 17.4 (n= 126) | −.01 | ||
| Pop OB | 48.9 ± 25.6 (n = 272) | 12.5 ± 18.5b (n = 221) | .49 | −.8 ± 17.5 (n = 208) | −.03 | ||
| Sexual life | F2,503 = 85.29, P < .001, partial η2 = .253 | F2,440 = .39, P = .68, partial η2 = .002 | |||||
| GB | 44.4 ± 29.4 (n = 292) | 36.6 ± 32.0a (n = 200) | 1.24 | −1.5 ± 22.7 (n = 176) | −.05 | ||
| No GB | 49.0 ± 32.8 (n = 232) | 4.5 ± 25.6b (n = 130) | .14 | −4.0 ± 32.4 (n = 99) | −.12 | ||
| Pop OB | 69.1 ± 29.7 (n = 246) | 7.1 ±24.9b (n= 180) | .24 | −3.6 ± 21.3 (n = 172) | −.12 | ||
| Public distress | F2,605 = 239.97, P < .001, partial η2 = .442 | F2,526 = 1.86, P = .16, partial η2 .007 | |||||
| GB | 42.9 ± 23.5 (n = 323) | 44.3 ± 22.0a (n = 229) | 1.89 | 1.1 ± 13.9 (n = 199) | .05 | ||
| No GB | 45.0 ± 25.7 (n = 257) | 7.1 ± 22.2b (n = 162) | .28 | −3.5 ± 18.5 (n = 126) | −.14 | ||
| Pop OB | 59.8 ± 24.0 (n = 272) | 11.1 ± 18.1b (n = 221) | .46 | −.8± 17.7 (n = 208) | −.03 | ||
| Work | F2,591 = 102.22, P < .001, partial η2 = .257 | F2,516 = .72, P = .49, partial η2 = .003 | |||||
| GB | 50.8 ± 26.4 (n = 322) | 37.3 ± 28.2a (n = 227) | 1.41 | 1.4 ± 14.8 (n= 198) | .05 | ||
| No GB | 51.1 ± 26.9 (n = 253) | 11.0 ± 24.9b (n = 159) | .41 | −1.4 ± 22.0 (n = 125) | −.05 | ||
| Pop OB | 68.7 ± 23.8 (n = 268) | 12.7 ± 20.7b (n = 212) | .53 | .2 ± 19.3 (n = 200) | .01 | ||
| Total | F2,605 = 271.15, P < .001, partial η2 = .473 | F2,524 = .84, P = .43, partial η2 = .003 | |||||
| GB | 36.7 ± 16.6 (n = 323) | 43.4 ± 19.3a (n = 229) | 2.61 | −3.8 ± 13.4 (n = 199) | −.23 | ||
| No GB | 39.1 ± 18.8 (n = 257) | 9.9 ± 18.6b (n= 162) | .53 | −1.5 ± 15.8 (n = 124) | −.08 | ||
| Pop OB | 55.7 ± 18.9 (n = 272) | 8.9 ± 14.3b (n = 221) | .47 | −1.5 ± 13.8 (n = 208) | −.08 | ||
| SF-36 scale | |||||||
| Physical functioning | F2,606 = 136.70, P < .001, partial η2 = .311 | F2,529 = 10.72, P < .001, partial η2 .039 | |||||
| GB | 41.5 ± 22.3 (n = 323) | 32.9 ± 24.8a (n = 227) | 1.48 | .4 ± 26.1a (n= 198) | .02 | ||
| No GB | 45.4 ± 24.7 (n = 257) | .3 ± 25.0b (n = 165) | .01 | −12.4 ± 23.3b (n = 129) | −.50 | ||
| Pop OB | 59.5 ± 23.2 (n = 272) | 1.8 ± 21.9b (n = 221) | .08 | −7.7 ± 21.8b (n = 209) | −.33 | ||
| Role physical | F2,604 = 14.32, P < .001, partial η2 = .045 | F2,525 = 1.78, P = .17, partial η2 = .007 | |||||
| GB | 38.5 ± 35.7 (n = 323) | 28.3 ± 47.4a (n = 227) | .79 | −4.7 ± 40.7 (n = 195) | −.13 | ||
| No GB | 40.9 ± 39.7 (n = 257) | 10.7 ± 47.3b (n = 164) | .27 | −10.4 ± 47.2 (n= 129) | −.26 | ||
| Pop OB | 60.4 ± 38.9 (n = 272) | 11.4 ± 37.1b (n = 220) | .29 | −2.7 ± 38.4 (n = 208) | −.01 | ||
| Bodily pain | F2,608 = 17.29, P < .001, partial η2 = .054 | F2,529 = 1.61, P = .20, partial η2 = .006 | |||||
| GB | 46.2 ± 22.4 (n = 323) | 12.0 ± 26.2a (n = 230) | .54 | −6.2 ± 24.8 (n = 200) | −.28 | ||
| No GB | 45.9 ± 21.6 (n = 257) | 1.0 ± 23.2b (n = 165) | .05 | −7.5 ± 24.2 (n = 207) | −.35 | ||
| Pop OB | 61.0 ± 22.8 (n = 272) | 1.2 ± 22.2b (n = 220) | .05 | −3.4 ± 20.6 (n = 129) | −.15 | ||
| General health | F2,606 = 65.77, P < .001, partial η2 = .178 | F2,527 = 2.49, P = .08, partial η2 = .009 | |||||
| GB | 42.0 ± 19.4 (n = 323) | 19.3 ± 21.3a (n = 230) | .99 | −7.6 ± 17.0 (n = 200) | −.39 | ||
| No GB | 40.5 ± 20.5 (n = 257) | 1.6 ± 22.5b (n = 164) | .08 | −9.4 ± 18.0 (n = 128) | −.46 | ||
| Pop OB | 53.1 ± 21.3 (n = 272) | 1.1 ± 18.2b (n = 219) | .05 | −5.4 ± 15.0 (n = 206) | −.25 | ||
| Vitality | F2,607 = 26.41, P < .001, partial η2 .080 | F2,528 = 1.97, P = .14, partial η2 = .007 | |||||
| GB | 29.7 ± 17.1 (n = 323) | 19.4 ± 22.6a (n = 230) | 1.13 | −6.2 ± 19.6 (n = 200) | −.36 | ||
| No GB | 30.6 ± 19.7 (n = 257) | 7.5 ± 21.4b (n = 164) | .38 | −3.2 ± 20.0 (n = 128) | −.16 | ||
| Pop OB | 42.4 ± 20.6 (n = 272) | 6.7 ± 19.2b (n = 220) | .33 | −2.5 ± 17.9 (n = 207) | −.12 | ||
| Social functioning | F2,608 = 13.06, P < .001, partial η2 = .041 | F2,531 = .79, P = .45, partial η2 = .003 | |||||
| GB | 54.1 ± 25.7 (n = 271) | 17.4 ± 29.7a (n = 230) | .68 | −3.9 ± 22.2 (n = 201) | −.15 | ||
| No GB | 54.9 ± 27.3 (n = 257) | 6.9 ± 27.0b (n = 165) | .25 | −4.5 ± 28.7 (n = 129) | −.16 | ||
| Pop OB | 73.1 ± 24.4 (n = 272) | 6.3 ± 27.7b (n = 220) | .26 | −1.6 ± 25.0 (n = 208) | −.07 | ||
| Role emotional | F2,604 = 1.13, P = .32, partial η2 = .004 | F2,525 = .68, P = .51, partial η2 = .003 | |||||
| GB | 54.8 ± 42.7 (n = 323) | 16.1 ± 51.4 (n = 227) | .38 | −4.7 ± 42.5 (n = 196) | −.11 | ||
| No GB | 49.1 ± 43.2 (n = 257) | 10.4 ± 48.5 (n = 164) | .24 | −3.2 ± 46.0 (n = 128) | −.07 | ||
| Pop OB | 66.5 ± 39.5 (n = 272) | 12.5 ± 44.4 (n = 220) | .32 | −.2 ± 44.4 (n = 208) | −.01 | ||
| Mental health | F2,607 = 7.27, P = .001, partial η2 = .023 | F2,528 = .53, P = .59, partial η2 = .002 | |||||
| GB | 63.8 ± 18.6 (n = 323) | 8.4 ± 19.9a (n = 230) | .45 | −2.0 ± 17.5 (n = 200) | −.11 | ||
| No GB | 61.2 ± 20.7 (n = 257) | 2.8 ± 19.2b (n = 164) | .14 | −.5 ± 19.7 (n = 128) | −.02 | ||
| Pop OB | 71.1 ± 18.4 (n = 272) | 3.1 ± 16.4a,b (n = 220) | .17 | −.4 ± 17.3 (n = 207) | −.02 | ||
| PCS | F2,595 = 83.84, P < .001, partial η2 = .220 | F2,516 = 3.21, P = .04, partial η2 = .012 | |||||
| GB | 32.5 ± 9.6 (n = 323) | 11.3 ± 10.6a (n = 223) | 1.17 | −2.3 ± 9.8 (n = 192) | −.24 | ||
| No GB | 33.9 ± 10.0 (n = 257) | .7 ± 11.3b (n= 162) | .07 | −4.9 ± 9.3 (n = 127) | −.49 | ||
| Pop OB | 40.0 ± 10.3 (n = 272) | .7 ± 9.0b (n = 217) | .07 | −2.8 ± 8.1 (n = 204) | −.27 | ||
| MCS | F2,0595 = .13, P = .88, partial η2 = .000 | F2,516 = 3.00, P = .05, partial η2 = .011 | |||||
| GB | 43.8 ± 11.4 (n = 323) | 3.8 ± 12.5 (n = 223) | .33 | −1.7 ± 10.7 (n = 192) | −.15 | ||
| No GB | 42.1 ± 12.4 (n = 257) | 3.3 ± 11.9 (n = 162) | .27 | .4 ± 11.9 (n= 127) | .03 | ||
| Pop OB | 47.7 ± 11.4 (n = 272) | 3.3 ± 11.0 (n = 217) | .29 | .6 ± 10.8 (n = 204) | .05 | ||
IWQOL-Lite = Impact of Weight on Quality of Life-Lite; SF-36 = Medical Outcomes Study Short-Form 36; SD = standard deviation; GB = gastric bypass; no GB = obese individuals seeking gastric bypass surgery who did not undergo the surgery; Pop OB = population-based obese individuals not seeking gastric bypass surgery; BMI = body mass index; PCS = physical component summary; MCS = mental component summary.
Data without superscript letters are not significantly different at P < .001; data with superscript letters not in common are significantly different at P < .001.
Data presented as baseline mean ± SD, adjusted for age, gender, and baseline BMI.
Data presented as mean change ± SD, adjusted for age, gender, baseline BMI, and baseline score.
Data presented as mean change ± SD, adjusted for age, gender, baseline BMI, and 2-year score; α levels for omnibus F tests = .003 (.05/16); α levels for post hoc comparisons = .001 (.003/3).
An examination of the changes in the IWQOL-Lite scores from 2 to 6 years revealed no significant between-group differences, although the change for self-esteem approached significance. The IWQOL-Lite total score and 3 of the 5 domain scores showed small decreases from 2 to 6 years for GB, with an effect size of −.31 for self-esteem and −.23 for the total score.
Figure 1B shows the mean IWQOL-Lite total scores by group adjusted for age, gender, and baseline BMI. Although at 2 years, the mean IWQOL-Lite score for the GB group slightly exceeded the score obtained by a nonobese community reference sample [29], at 6 years, the mean score was somewhat below this reference score.
SF-36 questionnaire
The changes in SF-36 scores from baseline to 6 years are presented in Table 2. The GB group experienced significantly greater improvement than the no GB and Pop OB groups for all scores, except for role emotional and MCS. In terms of the between-group differences, the partial η2 values for the SF-36 scores ranged from .023 (mental health) to .311 (physical functioning) for the domain scores that changed significantly and was .220 for the PCS. The within-group changes for the GB group ranged from .38 (role emotional) to 1.48 (physical functioning) for domain scores and was 1.17 for PCS and .33 for MCS.
The only significant difference between the groups in the changes in SF-36 scores from 2 to 6 years was for physical functioning, for which the scores for the GB group were relatively unchanged (effect size = .02) compared with to the no GB group (effect size = −.50) and Pop OB group (effect size = −.33), who experienced a small-to-moderate decline. The 2- to 6-year changes were small for the GB group, with effect sizes ranging from −.39 (minus sign indicates a decline) for general health to .02 for physical functioning.
Figure 1C shows the mean PCS scores by group adjusted for age, gender, and baseline BMI. The PCS score obtained by the GB group at 6 years remained somewhat below the U.S. norms [15].
Meaningful change for IWQOL-Lite total score
At 6 years, 223 (97.4%) of 229 GB patients had experienced meaningful improvements from baseline in the IWQOL-Lite total score compared with 77 (47.5%) of 162 in the no GB group and 77 (34.8%) of 221 in the Pop OB group (chi-square(4) = 205.55, P < .001). Only 1 GB patient (.4%) experienced meaningful deterioration in the IWQOL-Lite total score compared with 27 (16.7%) in the no GB group and 38 (17.2%) in the Pop OB group.
Discussion
Similar to the results obtained at the 2-year follow-up point [20], greater improvements in both weight-specific and general HRQOL were observed at 6 years for the GB patients compared with the no GB group and Pop OB group. The improvements exhibited by the GB patients occurred with respect to all aspects of weight-specific and physical HRQOL and some aspects of mental/psychosocial HRQOL. The changes in weight-specific HRQOL were much larger (2.61 SD for the IWQOL-Lite total score) than the changes in the physical HRQOL (1.17 SD for PCS), consistent with other HRQOL research [31]. The %EWL at 6 years, which was 56.4% for the GB group and negligible for the control groups, correlated significantly with changes in the IWQOL-Lite total score and PCS, but not the MCS. Because weight loss explained 59.0% of the variance in the IWQOL-Lite total score and 28.5% of the variance in the PCS, this suggests that factors other than weight loss might account for the HRQOL changes, such as increased attention to food intake/physical activity or improved self-efficacy (although these were not measured).
One of our research questions was whether early improvements in HRQOL obtained by the GB patients would persist over time. Although the HRQOL scores for the GB group decreased for most HRQOL subscales from 2 to 6 years, these decreases were generally small. Thus, the HRQOL was fairly stable during this period for the GB group, despite some weight regain (%EWL 69.1% at 2 yr and 56.4% at 6 yr) and some small decreases in HRQOL scores. That the HRQOL scores remained relatively high at 6 years for the GB group, especially in contrast to the control groups, is encouraging and perhaps can be used to motivate patients to continue healthy habits and weight maintenance. If these same patients considered their BMI only, they might become discouraged at the “failure” to maintain a nonobese BMI (mean adjusted BMI was 32.9 ± 7.4). Furthermore, it is worth noting that the 3 scales showing the greatest declines in the 2- to 6-year period were weight-related self-esteem, general health, and vitality, perhaps suggesting that health providers should pay particular attention to these areas of HRQOL in the long term.
Other studies examining whether the initial improvements in HRQOL are maintained at long-term follow-up have yielded conflicting results, perhaps because of the varying surgical procedures and HRQOL outcome measures used. Although the Swedish Obese Subjects study found that the pattern of change in HRQOL scores corresponded for the most part to phases of weight loss, regain, and weight stability [13], several studies have reported stable HRQOL scores accompanying continuing long-term weight loss [14,16,17] and another reported stable HRQOL scores accompanying weight regain [18].
Our prospective study is unique in its use of 2 nonsurgically treated comparison groups and adds to the sparse data on HRQOL outcomes in prospective trials of bariatric surgery versus nonsurgically treated obese groups [1,14]. Other strengths of the present study include the long-term follow-up of 6 years, the large sample size, and statistical adjustment for multiple tests. Because of the many areas of life that are considered when assessing HRQOL, most scientists and scholars agree that it is a multidimensional construct [32], and assessment with multiple measures is generally recommended [33]. Thus, another strength of the present study was the use of both general and weight-specific measures. Both the Swedish Obese Subjects study [1] and the Helmiö study [16] used both types of HRQOL measures, but others used only a single measure [14,18].
Despite a very high response rate at 6 years, not all participants completed the 6-year HRQOL assessment, a limitation that possibly resulted in bias. However, no systematic differences were found between those who did and did not complete the HRQOL assessment at 6 years. Another limitation was the lack of diversity with respect to demographic characteristics and geographic location, which might limit the generalizability of our findings. In addition, 45 participants in the control groups ultimately underwent gastric bypass surgery, which decreased the sample size of the control groups and could have potentially diminished the differences between the GB and control groups.
Conclusion
At 6 years of follow-up, greater improvements in HRQOL were reported by GB patients compared with the 2 nonsurgical obese groups. These improvements occurred in multiple aspects of HRQOL and closely paralleled the amount of weight loss. Despite some weight regain between the 2- and 6-year assessments, the GB patients sustained most of the positive changes reported at 2 years. Although the present study supports the long-term efficacy of gastric bypass surgery with respect to HRQOL, it is possible that individuals achieving the same degree of weight loss with nonsurgical methods would demonstrate similar improvements in HRQOL.
Acknowledgments
This research was funded by grant DK-55006 from the National Institute of Diabetes and Digestive and Kidney Diseases and grant M01-RR00064 from the National Center for Research Resources.
Footnotes
Disclosures R. L. Kolotkin receives consulting fees as a consultant from University of Utah and royalties from Duke University as an IWQOL-Lite developer. The remaining authors have no commercial associations that might be a conflict of interest in relation to this article.
References
- [1].Karlsson J, Sjöström L, Sullivan M. Swedish obese subjects (SOS)—an intervention study of obesity: two-year follow-up of health-related quality of life (HRQL) and eating behavior after gastric surgery for severe obesity. Int J Obes Relat Metab Disord. 1998;22:113–26. doi: 10.1038/sj.ijo.0800553. [DOI] [PubMed] [Google Scholar]
- [2].Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002;10:748–56. doi: 10.1038/oby.2002.102. [DOI] [PubMed] [Google Scholar]
- [3].Dixon JB, Dixon ME, O'Brien PE. Quality of life after lap-band placement: influence of time, weight loss, and comorbidities. Obes Res. 2001;9:713–21. doi: 10.1038/oby.2001.96. [DOI] [PubMed] [Google Scholar]
- [4].Sullivan M, Karlsson J, Sjostrom L, et al. Swedish obese subjects (SOS)—an intervention study of obesity: baseline evaluation of health and psychosocial functioning in the first 1743 subjects examined. Int J Obes. 1993;1743:503–12. [PubMed] [Google Scholar]
- [5].Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13:639–48. doi: 10.1038/oby.2005.71. [DOI] [PubMed] [Google Scholar]
- [6].Hell E, Miller KA, Moorehead MK, Norman S. Evaluation of health status and quality of life after bariatric surgery: comparison of standard Roux-en-Y gastric bypass, vertical banded gastroplasty and laparoscopic adjustable silicone gastric banding. Obes Surg. 2000;10:214–19. doi: 10.1381/096089200321643485. [DOI] [PubMed] [Google Scholar]
- [7].Müller MK, Wenger C, Schiesser M, Clavien PA, Weber M. Quality of life after bariatric surgery—a comparative study of laparoscopic banding vs. bypass. Obes Surg. 2008;18:1551–7. doi: 10.1007/s11695-008-9522-y. [DOI] [PubMed] [Google Scholar]
- [8].Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234:279–91. doi: 10.1097/00000658-200109000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Campos GM, Rabl C, Roll GR, et al. Better weight loss, resolution of diabetes, and quality of life for laparoscopic gastric bypass vs banding: results of a 2-cohort pair-matched study. Arch Surg. 2011;146:149–55. doi: 10.1001/archsurg.2010.316. [DOI] [PubMed] [Google Scholar]
- [10].de Zwaan M, Lancaster KL, Mitchell JE, et al. Health-related quality of life in morbidly obese patients: effect of gastric bypass surgery. Obes Surg. 2002;12:773–80. doi: 10.1381/096089202320995547. [DOI] [PubMed] [Google Scholar]
- [11].Sanchez-Santos R, Del Barrio MJ, Gonzalez C, et al. Long-term health-related quality of life following gastric bypass: influence of depression. Obes Surg. 2006;16:580–5. doi: 10.1381/096089206776945084. [DOI] [PubMed] [Google Scholar]
- [12].van Gemert WG, Adang EM, Greve JW, Soeters PB. Quality of life assessment of morbidly obese patients: effect of weight-reducing surgery. Am J Clin Nutr. 1998;67:197–201. doi: 10.1093/ajcn/67.2.197. [DOI] [PubMed] [Google Scholar]
- [13].Karlsson J, Taft C, Ryden A, Sjostrom L, Sullivan M. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes (Lond) 2007;31:1248–61. doi: 10.1038/sj.ijo.0803573. [DOI] [PubMed] [Google Scholar]
- [14].Nickel MK, Loew TH, Bachler E. Change in mental symptoms in extreme obesity patients after gastric banding, part II: six-year follow up. Int J Psychiatry Med. 2007;37:69–79. doi: 10.2190/X40R-712P-8J44-0L3H. [DOI] [PubMed] [Google Scholar]
- [15].Ware J, Snow K, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation Guide. Health Institute; New England Medical Center; Boston: 1993. [Google Scholar]
- [16].Helmiö M, Salminen P, Sintonen H, Ovaska J, Victorzon M. A 5-year prospective quality of life analysis following laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2011;21:1585–91. doi: 10.1007/s11695-011-0425-y. [DOI] [PubMed] [Google Scholar]
- [17].Caiazzo R, Arnalsteen L, Pigeyre M, et al. Long-term metabolic outcome and quality of life after laparoscopic adjustable gastric banding in obese patients with type 2 diabetes mellitus or impaired fasting glucose. Br J Surg. 2010;97:884–91. doi: 10.1002/bjs.6993. [DOI] [PubMed] [Google Scholar]
- [18].Suter M, Donadini A, Romy S, Demartines N, Giusti V. Laparoscopic Roux-en-Y gastric bypass: significant long-term weight loss, improvement of obesity-related comorbidities and quality of life. Ann Surg. 2011;254:267–73. doi: 10.1097/SLA.0b013e3182263b66. [DOI] [PubMed] [Google Scholar]
- [19].Adams TD, Avelar E, Cloward T, et al. Design and rationale of the Utah obesity study. a study to assess morbidity following gastric bypass surgery. Contemp Clin Trials. 2005;26:534–51. doi: 10.1016/j.cct.2005.05.003. [DOI] [PubMed] [Google Scholar]
- [20].Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Adams TD. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. 2009;5:250–6. doi: 10.1016/j.soard.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9:102–11. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- [22].Hunt SC, Williams RR, Barlow GK. A comparison of positive family history definitions for defining risk of future disease. J Chronic Dis. 1986;39:809–21. doi: 10.1016/0021-9681(86)90083-4. [DOI] [PubMed] [Google Scholar]
- [23].Williams RR, Hunt SC, Barlow GK, et al. Health family trees: a tool for finding and helping young family members of coronary and cancer prone pedigrees in Texas and Utah. Am J Public Health. 1988;78:1283–6. doi: 10.2105/ajph.78.10.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Williams RR, Hunt SC, Heiss G, et al. Usefulness of cardiovascular family history data for population-based preventive medicine and medical research (the Health Family Tree Study and the NHLBI Family Heart study) Am J Cardiol. 2001;87:129–35. doi: 10.1016/s0002-9149(00)01303-5. [DOI] [PubMed] [Google Scholar]
- [25].Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-Lite questionnaire (IWQOL-Lite) in a community sample. Qual Life Res. 2002;11:157–71. doi: 10.1023/a:1015081805439. [DOI] [PubMed] [Google Scholar]
- [26].McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- [27].McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- [28].Winer BJ. Statistical principles in experimental design. 2nd ed McGraw-Hill; New York: 1971. pp. 198–201. [Google Scholar]
- [29].Crosby RD, Kolotkin RL, Williams GR. An integrated method to determine meaningful changes in health-related quality of life. J Clin Epidemiol. 2004;57:1153–60. doi: 10.1016/j.jclinepi.2004.04.004. [DOI] [PubMed] [Google Scholar]
- [30].Obesity: preventing and managing the global epidemic: report of a WHO consultation. WHO Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- [31].Kolotkin RL, Norquist JM, Crosby RD, et al. One-year health-related quality of life outcomes in weight loss trial participants: comparison of three measures. Health Qual Life Outcomes. 2009;7:53. doi: 10.1186/1477-7525-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Fayers PM, Machin D. Quality of life: assessment, analysis and interpretation. John Wiley and Sons; New York: 2000. [Google Scholar]
- [33].Maciejewski ML, Patrick DL, Williamson DF. A structured review of randomized controlled trials of weight loss showed little improvement in health-related quality of life. J Clin Epidemiol. 2005;58:568–78. doi: 10.1016/j.jclinepi.2004.10.015. [DOI] [PubMed] [Google Scholar]