Abstract
Introduction:
Substantial evidence suggests that concerns about postcessation weight gain interfere with cessation efforts. However, it is unclear to what extent weight pretreatment affects smoking-related weight concerns. Given that the prevalence of overweight and obesity among callers to tobacco quitlines mirrors that of the population at large, and that women and obese smokers may be more concerned about weight gain, we sought to compare weight gain concerns among normal weight, overweight, and obese callers to a quitline.
Methods:
A sample of 34.6% (n = 206) normal weight, 30.6% (n = 182) overweight, and 34.8% (n = 207) obese quitline callers completed assessments of tobacco use history and smoking-specific weight concerns. Weight categories were compared and gender differences evaluated.
Results:
Obese smokers endorsed significantly more concerns about postcessation weight gain [F(2, 592) = 20.35, p < .0001], had less confidence in their ability to maintain their weight without smoking [F(2, 592) = 7.67, p = .0005], and were willing to tolerate less weight gain after quitting than normal weight or overweight smokers [F(2,574) = 30.59, p < .0001). There also were gender differences in weight concerns by weight status. Significantly more women callers were obese (38.2% vs. 28.4%, p = .011), and women consistently endorsed more concern about postcessation weight gain than did men [F(1,588) = 24.04, p < .0001).
Conclusions:
Overweight and obese smokers, particularly women, express substantial concern about gaining weight after quitting. It is possible that smokers who begin quitline treatment with a BMI in the obese range may benefit from adjunctive interventions designed to address smoking-related weight concerns.
INTRODUCTION
Smoking cessation is robustly associated with weight gain (Hudmon, Gritz, Clayton, & Nisenbaum, 1999; Killen, Fortmann, & Newman, 1990; Klesges et al., 1997; Perkins, 1993; Streater, Sargent, & Ward, 1989; Williamson, et al., 1991). Smokers who are concerned about postcessation weight gain have poorer cessation outcomes (Jeffery, Hennrikus, Lando, Murray, & Liu, 2000; Meyers et al., 1997; Mizes et al., 1998) and gain more weight after quitting (Perkins et al., 2001) than do smokers without weight concerns. Despite consistent evidence that smokers, on average, weigh less than do nonsmokers (Williamson, et al., 1991), overweight and obese individuals smoke.
Smokers interested in cessation treatment are more likely to be overweight or obese than are those not interested in quitting (LaRowe, Piper, Schlam, Fiore, & Baker, 2009). Initial evidence also suggests that obese smokers report larger than average weight gain after quitting. For example, overweight or obese individuals presenting for weight loss surgery report gaining an average of 12.7kg in prior quit attempts (Levine, Kalarchian, Courcoulas, Wisinski, & Marcus, 2007) compared to the 4.5 kg in samples not selected on degree of obesity (e.g., Perkins, et al., 2001). Moreover, women and obese smokers are more likely to be concerned about the weight gain that commonly accompanies an attempt to quit smoking than are men (Meyers, et al., 1997) or normal weight smokers (Pomerleau & Saules, 2007).
Although there is burgeoning evidence of an association between obesity and smoking, it is unclear whether the degree of concern about cessation-related weight gain differs across weight categories. It is possible that a smoker’s weight status at the beginning of treatment will affect the outcome of cessation intervention. We have previously documented that the prevalence of overweight and obesity among quitline users mirrors that of the population at large (Bush et al., 2009). Given that quitlines are a widely used cessation resource (Lichtenstein, Zhu, & Tedeschi, 2010; Zhu et al., 2002), that more than 60% of callers to quitlines in the United States are overweight or obese (Bush et al., 2009), and that weight concerns can interfere with cessation efforts, we sought to characterize the concerns about weight gain and smoking behaviors of quitline users across weight categories.
METHODS
Participants and Setting
Participants were callers to five state tobacco quitlines: Georgia, Louisiana, Maryland, South Carolina, and Texas (with the exception of Harris County, Texas). The study was reviewed and approved by the Western Institutional Review Board, and recruitment occurred between August 10, 2010, and December, 2010. There were no changes to the standard quitline services that were offered to callers.
A total of 11,043 adults called one of these state quitlines during the study recruitment period. Callers were eligible to participate if they were at least 18 years of age, currently using tobacco, not currently pregnant, smoking at least 5 cigarettes per day, planning to quit smoking in the next 30 days, comfortable speaking English, provided a valid phone number and address, and reported their height and weight. Screening continued until the selected sample was approximately 33% normal weight, 33% overweight, and 33% obese. Participants meeting initial screening criteria were invited to participate.
Procedures
Interested and initially eligible callers were transferred to a specially trained quit coach who provided informed verbal consent and conducted a baseline survey. Participants were then provided with standard quitline services. A total of 595 eligible participants agreed to participate in the study, comprising 15.5%, 14.3%, 29.9%, 8%, and 32.3% of quitline users from Georgia, Louisiana, Maryland, South Carolina, and Texas, respectively.
Assessments
Demographics
Age, sex, educational attainment, race and ethnicity, height, and weight were obtained by self-report. Body Mass Index (BMI; weight in kg/height in m2) was calculated.
Tobacco Use
Number of years of tobacco use and the frequency of current smoking was determined by asking if the caller smoked cigarettes every day or some days. The number of previous quit attempts and current number of cigarettes smoked per day was also ascertained.
Smoking-Specific Weight Concerns
Several smoking-related weight concerns measures were used. First, participants answered a six-item questionnaire designed to assess cessation specific weight concerns and a separate six-item questionnaire assessing self-efficacy for weight management after quitting smoking (Borrelli & Mermelstein, 1998). Both the weight self-efficacy and weight concerns scales range from 0 to 10. In addition, based on previous work on the treatment of weight-concerned smokers (Levine et al., 2010; Perkins, et al., 2001), individuals answered the following two questions using a scale of 0–100 (where 0 = not at all and 100 = extremely): 1) “How concerned are you about gaining weight after quitting?” and 2) “How concerned would you be if quitting smoking caused you to permanently gain 10 pounds (4.54 kg)?” Finally, callers were asked about the amount of weight they expected to gain upon successfully quitting smoking and about the amount of postcessation weight gain they would be willing to accept as well as the amount of maximum weight gain in any previous quit attempt.
Motivation to Quit Smoking
Participants rated their motivation on a scale from 1 (not strong at all) to 10 (extremely strong), in response to the question “How strong is your motivation to quit?”
Depressive Symptoms
Two depressive symptoms were queried. Participants were asked how often they experienced anhedonia or felt “down, depressed or hopeless” over the past two weeks. Response options were “not at all, several days and more than half the days.” Participants who responded “more than half the days” to at least one option were rated positive for depressive symptoms.
Data Analyses
Participants were categorized according to initial BMI (kg/m2) as normal weight (BMI = 18.5–24.99), overweight (BMI = 25.0–29.99), or obese (BMI > 30.0). Chi-square tests and ANOVA were used to compare across these weight categories on the initial demographic variables as well as tobacco history, weight concerns, motivation, and depressive symptoms. To evaluate gender differences, a general linear model was fit, with terms for gender, BMI group, and the gender by BMI group interaction. In addition, two-sample tests of weight concerns by gender were conducted separately for normal weight, overweight, and obese participants based on the general model.
RESULTS
Descriptive information as well as information on the smoking history and current smoking behavior of participants is shown in Table 1. As planned, we obtained a sample comprised of 34.6% (n = 206) normal weight, 30.6% (n = 182) overweight, and 34.8% (n = 207) obese quitline callers. There were no differences in age, race, ethnicity, educational background, depressive symptoms, tobacco use frequency, duration of smoking, number of previous quit attempts or maximum weight gain in previous quit attempts across weight categories. In addition, overweight and obese smokers did not differ from normal weight smokers on motivation to quit smoking.
Table 1.
Demographic Information and Weight Concerns by Weight Category
| Normal weight(n = 206) | Overweight(n = 182) | Obese(n = 207) | Total sample(n = 595) | |
|---|---|---|---|---|
| M(SD) | M(SD) | M(SD) | ||
| BMI (kg/m2) | 22.4 (1.8) | 27.5 (1.4) | 36.4 (6.6) | 28.8 (7.2) |
| Age | 44.3 (13.0) | 46.3 (12.8) | 42.8 (12.6) | 44.4 (12.8) |
| Gender (% female) | 67.0 | 57.7 | 72.5 | 66.1 |
| % White | 63.1 | 54.4 | 60.9 | 59.7 |
| % Non-Hispanic | 93.2 | 94.0 | 87.9 | 91.6 |
| Education (% at least some college) | 38.7 | 36.5 | 46.4 | 40.7 |
| Smoking frequency (% every day) | 98.1 | 98.9 | 97.6 | 98.2 |
| Years smoking | 27.7 (12.7) | 29.0 (13.2) | 26.2 (12.9) | 27.6 (13.0) |
| # previous quit attempts (% ≥ 2 attempts) | 61.5 | 70.2 | 61.7 | 64.2 |
| Motivationa (1–10) | 9.2 (1.4) | 9.1 (1.4) | 9.1 (1.4) | 9.1 (1.4) |
| Weight self-efficacy (1–10) | 6.9 (2.3) | 6.6 (2.2) | 6.0 (2.2) | 6.5 (2.2) |
| Weight gain concerns (1–10) | 3.5 (2.3) | 4.1 (2.4) | 5.0 (2.3) | 4.2 (2.4) |
| Concern about 10 pound (4.5kg) gain (0–100) | 22.7 (34.3) | 31.0 (38.0) | 50.6 (41.6) | 34.9 (39.9) |
| Expected weight gain (kg) | 6.2 (5.1) | 6.4 (6.0) | 7.0 (6.2) | 6.5 (5.8) |
| Tolerable weight gain (kg) | 7.0 (5.6) | 4.6 (4.7) | 3.4 (3.5) | 5.0 (4.9) |
| Maximum weight gained in previous attempt (kg) (number reporting previous quit attempt) | 4.9 (7.0) (n = 151) | 5.3 (7.5) (n = 133) | 5.7 (7.3) (n = 157) | 5.3 (7.3) (n = 441) |
| Depressive symptoms (% yes) | 35.4 | 34.1 | 41.1 | 37.0 |
Note. aThe motivation variable was missing on 58 individuals. Missing responses were evenly distributed across BMI (p = .82) and gender (p = .74) groups.
Smoking-Related Weight Concerns
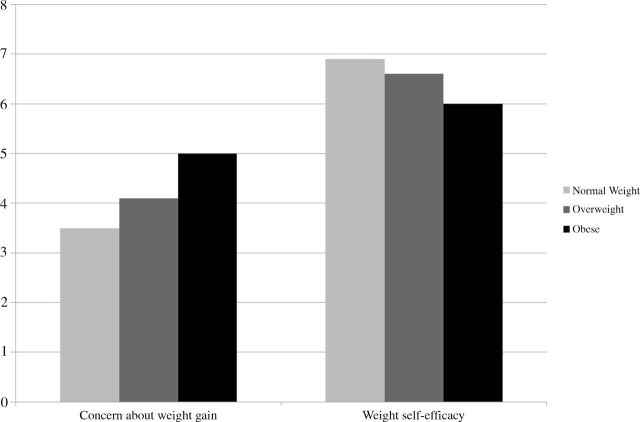
Smoking-related weight concerns differed across the weight categories. As shown in Figure 1, quitline callers who were obese reported significantly greater concern about postcessation weight gain than did either normal weight or overweight callers, F(2, 592) = 20.35, p < .0001. Similarly, obese smokers reported feeling significantly less confident in their ability to maintain their weight without smoking than did normal weight or overweight callers, F(2, 592) = 7.67, p = .0005.
Figure 1.
Weight concerns by weight status.
There also were differences by weight categories in the amount of weight smokers were willing to tolerate after quitting. Smokers of normal weight were willing to tolerate significantly larger weight gains than were either overweight or obese smokers, F(2,574) = 30.59, p < .0001. Indeed, normal weight smokers were willing to tolerate a 7.0kg weight gain (7.0±5.6kg) compared to 4.6 (±4.7) and 3.4 (±3.5) kg among overweight and obese smokers.
Gender Differences in Smoking-Related Weight Concerns
There were significant gender differences in weight and weight gain concerns. A significantly greater proportion of female relative to male callers were obese (38.2% vs. 28.4%, p = .011). Female callers also consistently endorsed greater concern about postcessation weight gain than did males, F(1,588) = 24.04, p < .0001. In addition, as shown in Table 2, the gender effect is more prominent among normal and overweight smokers. There were no differences in motivation to quit smoking, however, between men and women.
Table 2.
Weight Gain Concerns (1–10) by Gender and Weight Category
| Normal weight | Overweight | Obese | ||||
|---|---|---|---|---|---|---|
| Mean (n) | SD | Mean (n) | SD | Mean (n) | SD | |
| Female | 3.81 (138) | 2.24 | 4.63 (105) | 2.44 | 5.14 (150) | 2.43 |
| Male | 2.84 (68) | 2.30 | 3.33 (76) | 2.14 | 4.46 (57) | 2.00 |
| p value | 0.004 | 0.0002 | 0.056 | |||
Note. Overall results: Gender effect: F(1,588) = 24.04, p < .0001; BMI group effect: F(2,588) = 17.82, p < .0001; Gender X group: F(2,588) = 0.77, p = .46.
CONCLUSIONS
The current study is the first to characterize smoking-specific concerns across normal weight, overweight, and obese treatment-seeking smokers. Given the separate and combined health effects of smoking and obesity, these findings have several implications. First, these data document that obese treatment-seeking smokers are concerned about the weight gain that commonly accompanies efforts to quit smoking. Indeed obese smoker are more concerned than are their normal weight or overweight peers, and endorse feeling unable to manage weight without cigarettes. Thus, treatment approaches designed to address concerns about weight gain following smoking cessation (Levine, Marcus, & Perkins, 2003a; Levine, et al., 2010; Perkins, et al., 2001) may be a useful adjunct to cessation interventions among individuals of all weight categories.
Second, the present findings are consistent with previous data on smoking and obesity. For example, smoking may help to control a tendency toward overeating or binge eating as smokers with a history of binge eating report greater weight gain following cessation than those without a history of binge eating (White, Masheb, & Grilo, 2010) and were less successful in cessation treatment (White, Peters, & Toll, 2010). It also has been postulated that the rewarding value of food, which differs in obese individuals, relates to smoking behavior (Volkow, Wang, & Baler, 2011). A tendency to overeat after quitting or an increased experience of food as rewarding after smoking cessation suggests that obese smokers’ heightened concerns about weight gain postcessation may be justified.
Another implication of the current data is that gender remains important in the development of intervention approaches for weight and smoking. Across all weight categories, women endorsed stronger concerns about smoking-related weight gain. Thus, women may be more likely to benefit from strategies to address postcessation weight gain concerns than men. However, although weight concerns may be relevant to smokers of all pretreatment weight categories, and despite the fact that women endorsed stronger concern than did men, among quitline users, depressive symptoms, which have been associated with cessation-related weight gain concerns (Levine, Marcus & Perkins, 2003b), were not associated with weight status or gender.
There are several limitations to the current report. First, data were collected via telephone survey. Thus, the measure of depressive symptoms was brief and the data presented represent responses to screening questions rather than validated depressive symptom questionnaires. Second, weight and height were assessed solely by self-report. Although weight may be underreported by telephone (Gorber, Tremblay, Moher & Gorber, 2007), data suggest a reasonable correlation between self-report and clinic measured weight (Jeffery, 1996). Finally, the sample reflects only smokers seeking treatment from a tobacco quitline from participating states, and as such may not be indicative of concerns across all samples of treatment-seeking smokers.
In summary, these data suggest the need to determine the differential efficacy of standard quitline treatment on both cessation outcomes and postcessation weight gain across weight categories. We recently demonstrated the acceptability of weight-focused counseling in standard quitline counseling (Bush et al., in press), and ongoing work will provide initial evidence regarding the efficacy of standard quitline cessation treatment for obese smokers relative to smokers of lower precessation weights. If those who enter treatment with a BMI in the obese range are less likely to quit than those with lower BMIs, the present findings suggest that it will be important to explore the feasibility of smoking cessation interventions designed to address the weight concerns of obese smokers.
FUNDING
This research was supported by an award from the National Institute on Drug Abuse at the National Institutes of Health (R21DA026580).
DECLARATION OF INTERESTS
The authors have no competing interests to report.
ACKNOWLEDGMENTS
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. The authors would like to acknowledge the capable research assistance of Meghan Wisinski.
REFERENCES
- Borrelli B., Mermelstein R. (1998). The role of weight concern and self-efficacy in smoking cessation and weight gain among smokers in a clinic-based cessation program. Addictive Behaviors, 23, 609–622. 10.1016/S0306-4603(98)00014-8 [DOI] [PubMed] [Google Scholar]
- Bush T., Levine M. D., Deprey M., Cerruti B., Zbikowski S. M., McAfee T., et al. (2009). Prevalence of weight concerns and obesity among smokers calling a quit line. Journal of Smoking Cessation, 4, 74–78. 10.1375/jsc.4.2.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush T., Levine M. D., Beebe L. A., Cerutti B., Deprey M., McAfee T., Boeckman L., Zbikowski S.(in press). Addressing weight gain in smoking cessation treatment: A randomized controlled trial. American Journal of Health Promotion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorber S. C., Tremblay M., Moher D., Gorber B. (2007). A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obesity Reviews, 8, 307–326 [DOI] [PubMed] [Google Scholar]
- Hudmon K. S., Gritz E. R., Clayton S., Nisenbaum R. (1999). Eating orientation, postcessation weight gain, and continued abstinence among female smokers receiving an unsolicited smoking cessation intervention. Health Psychology, 18, 29–36. 10.1037/0278-6133.18.1.29 [DOI] [PubMed] [Google Scholar]
- Jeffery R. W. (1996). Bias in reported body weight as a function of education, occupation, health and weight concern. Addictive Behaviors, 21, 217–222 [DOI] [PubMed] [Google Scholar]
- Jeffery R. W., Hennrikus D. J., Lando H. A., Murray D. M., Liu J. W. (2000). Reconciling conflicting findings regarding postcessation weight concerns and success in smoking cessation. Health Psychology, 19, 242–246. 10.1037/0278-6133.19.3.242 [DOI] [PubMed] [Google Scholar]
- Killen J. D., Fortmann S. P., Newman B. (1990). Weight change among participants in a large sample minimal contact smoking relapse prevention trial. Addictive behaviors, 15, 323–332. 10.1016/0306-4603(90)90042-V [DOI] [PubMed] [Google Scholar]
- Klesges R. C., Winders S. E., Meyers A. W., Eck L. H., Ward K. D., Hultquist C. M. … Shadish W. R. (1997). How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. Journal of Consulting and Clinical Psychology, 65, 286–291. 10.1037/0022-006X.65.2.286 [DOI] [PubMed] [Google Scholar]
- LaRowe T. L., Piper M. E., Schlam T. R., Fiore M. C., Baker T. B. (2009). Obesity and smoking: comparing cessation treatment seekers with the general smoking population. Obesity, 17, 1301–1305. 10.1038/oby.2009.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine M. D., Kalarchian M. A., Courcoulas A. P., Wisinski M. S., Marcus M. D. (2007). History of smoking and postcessation weight gain among weight loss surgery candidates. Addictive Behaviors, 32, 2365–2371. 10.1016/j.addbeh.2007.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine M. D., Marcus M. D., Perkins K. A. (2003a). Women, weight and smoking: A cognitive behavioral approach to women’s concerns about weight gain following smoking cessation. Cognitive and Behavioral Practice, 10, 105–111. 10.1016/S1077-7229(03)80018-4 [Google Scholar]
- Levine M. D., Marcus M. D., Perkins K. A. (2003b). A history of depression and smoking cessation outcomes among women concerned about post-cessation weight gain. Nicotine & Tobacco Research, 5, 69–76 [DOI] [PubMed] [Google Scholar]
- Levine M. D., Perkins K. A., Kalarchian M. A., Cheng Y., Houck P. R., Slane J. D. … Marcus M. D. (2010). Bupropion and cognitive behavioral therapy for weight-concerned women smokers. Archives of Internal Medicine, 170, 543–550. 10.1001/archinternmed.2010.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein E., Zhu S. H., Tedeschi G. J. (2010). Smoking cessation quitlines: an underrecognized intervention success story. American Psychologist, 65, 252–261. 10.1037/a0018598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers A. W., Klesges R. C., Winders S. E., Ward K. D., Peterson B. A., Eck L. H. (1997). Are weight concerns predictive of smoking cessation? A prospective analysis. Journal of Consulting and Clinical Psychology, 65, 448–452. 10.1037/0022-006X.65.3.448 [DOI] [PubMed] [Google Scholar]
- Mizes J. S., Sloan D. M., Segraves K., Spring B., Pingitore R., Kristeller J. (1998). The influence of weight-related variables on smoking cessation. Behavior Therapy, 29, 371–385. 10.1016/S0005-7894(98)80038-5 [Google Scholar]
- Perkins K. A. (1993). Weight gain following smoking cessation. Journal of Consulting and Clinical Psychology, 61, 768–777. 10.1037/0022-006X.61.5.768 [DOI] [PubMed] [Google Scholar]
- Perkins K. A., Marcus M. D., Levine M. D., D’Amico D., Miller A., Broge M. … Shiffman S. (2001). Cognitive-behavioral therapy to reduce weight concerns improves smoking cessation outcome in weight-concerned women. Journal of Consulting and Clinical Psychology, 69, 604–613. 10.1037/0022-006X.69.4.604 [PubMed] [Google Scholar]
- Pomerleau C. S., Saules K. (2007). Body image, body satisfaction, and eating patterns in normal-weight and overweight/obese women current smokers and never-smokers. Addictive Behaviors, 32, 2329–2334. 10.1016/j.addbeh.2007.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streater J. A., Jr, Sargent R. G., Ward D. S. (1989). A study of factors associated with weight change in women who attempt smoking cessation. Addictive Behaviors, 14, 523–530. 10.1016/0306-4603(89)90072–5 [DOI] [PubMed] [Google Scholar]
- Volkow N. D., Wang G. J., Baler R. D. (2011). Reward, dopamine and the control of food intake: implications for obesity. Trends in Cognitive Sciences, 15, 37–46. 10.1016/j.tics.2010.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White M. A., Masheb R. M., Grilo C. M. (2010). Accuracy of self-reported weight and height in binge eating disorder: misreport is not related to psychological factors. Obesity, 18, 1266–1269. 10.1038/oby.2009.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White M. A., Peters E. N., Toll B. A. (2010). Effect of binge eating on treatment outcomes for smoking cessation. Nicotine & Tobacco Research, 12, 1172–1175. 10.1093/ntr/ntq163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson D. F., Madans J., Anda R. F., Kleinman J. C., Giovino G. A., Byers T. (1991). Smoking cessation and severity of weight gain in a national cohort. New England Journal of Medicine, 324, 739–745. 10.1056/NEJM199103143241106 [DOI] [PubMed] [Google Scholar]
- Zhu S. H., Anderson C. M., Tedeschi G. J., Rosbrook B., Johnson C. E., Byrd M. … Gutierrez-Terrell E. (2002). Evidence of real-world effectiveness of a telephone quitline for smokers. New England Journal of Medicine, 347, 1087–1093. 10.1056/ NEJMsa020660 [DOI] [PubMed] [Google Scholar]