Abstract
Endovascular intervention has emerged as an accepted modality for treating patients with critical limb ischemia. However, this therapy poses multiple challenges to the interventionalist due to the presence of widespread multilevel disease, long and complex occlusive lesions, and the common involvement of the tibial vessels. Retrograde pedal/tibial access is a relatively new technique that allows the treatment of tibial occlusive lesions when conventional endovascular techniques fail. This article reviews the technical details and published data regarding this technique and evaluates its use in this difficult-to-treat patient population.
Keywords: critical limb ischemia, endovascular intervention, retrograde access, tibial arterial occlusive disease

Introduction
Critical limb ischemia (CLI) is a severe degree of peripheral arterial occlusive disease (PAD) that requires intervention to avoid limb loss and its associated morbidity and mortality. While endovascular intervention has emerged as an accepted modality of therapy for these patients, it poses multiple challenges to the interventionalist due to the presence of widespread multilevel disease, long and complex occlusive lesions, and involvement of the tibial vessels, which itself poses specific interventional challenges.1-3
Although the usual treatment strategy for tibial lesions requires either a retrograde or antegrade femoral artery approach, in 10-20% of the patients those approaches do not allow the crossing of the lesion itself.4 Until recently, the inability to cross tibial lesions in an antegrade fashion was accepted as a failure of interventional therapy and an indication for an open surgical approach.
In 1990, Iyer and colleagues described the use of a retrograde pedal/tibial approach to handle cases in which the conventional way of crossing the tibial lesion had failed.5 Early in the experience, access into the pedal vessels was obtained via a cut down and was accomplished later on using direct percutaneous arterial puncture.6-9 In this article we present the technical details of this approach and review the published data on its use in this challenging patient population.
Technique
The retrograde access technique comprises two steps. The first step requires gaining percutaneous access into the pedal vessel. The second step involves crossing the occlusion in a retrograde fashion.
Access into the Pedal/Tibial Vessel
Patients should be prepped in a way to allow the usual access through either a retrograde or antegrade femoral approach; additionally, the foot should be prepped for the pedal access (Figure 1). Patients should be sedated only enough to relax them in order to minimize foot movement, especially if the roadmapping technique is used for access. Too much sedation will interfere with patient cooperation—they will actually move more frequently and will not be able to respond to the verbal instructions provided by the interventionalist. Local anesthesia used at the proposed puncture site should be minimal to avoid compression of the vessel to be accessed. These vessels usually have a very low perfusion pressure, and extrinsic compression by the local anesthetic can interfere with accessing the vessel.4
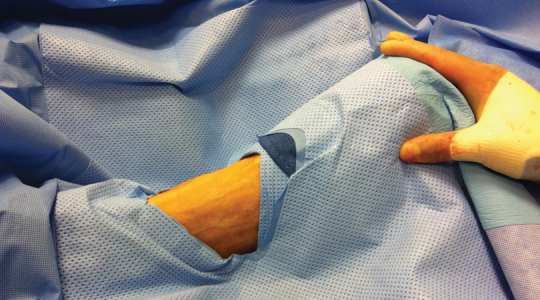
Figure 1.
Foot is prepped for anterior dorsalis pedis artery access.
All tibial vessels, including the anterior tibial, posterior tibial, and peroneal arteries, can be accessed in retrograde fashion. The access can be obtained using standard surgical cut down on the vessel, as in the original description of the technique by Iyer and colleagues.5 This technique, however, carries the risk of creating a surgical wound in the distal part of an ischemic limb; this wound has to heal after the intervention and will potentially add to the problem should the retrograde approach be unsuccessful in restoring inline flow to the access area.
Currently, most of the published data and our own institutional practice recommend using the percutaneous approach. This can be done directly in heavily calcified vessels based on fluoroscopic guidance alone. Another guidance technique utilizes roadmapping. This is aided by antegrade angiography from the femoral access site to identify the pedal/tibial vessel to be accessed. The degree of vessel opacification can be enhanced by using vasodilators through the femoral access site to maximize the caliber of the arterial target. Patient cooperation and proper sedation are of utmost importance for the success of this approach.
In our opinion, the use of duplex-guided access is the most feasible technique for accessing the pedal/tibial vessels (Figure 2). The vessel is identified with the ultrasound probe in either longitudinal or transverse position relative to the vessel. Color flow is used to identify flow in the target artery; then, using gray scale, the needle is used to access the anterior wall of the vessel under duplex guidance. There are a couple of technical points worth mentioning when using this technique. Use of the smallest available ultrasound probe is recommended as the large ones are quite bulky and will interfere with the access process. Also, heavily calcified vessels can cause extensive shadowing that will make the technique difficult. In these situations, straight fluoroscopy or roadmapping may offer a better chance for successful access. Also, use of micropuncture needles that are purported to be echogenic is recommended as it is difficult to see the tip of the regular needles using the duplex ultrasound probe.
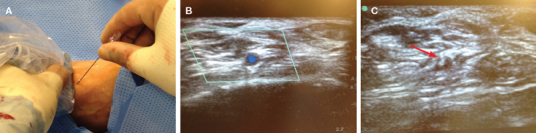
Figure 2.
Duplex ultrasound-guided access into the dorsalis pedis artery. (A) Duplex ultrasound probe and 21-gauge needle in place. (B) Color duplex identifies the patent anterior tibial artery lumen. (C) Tip of the needle inside the vessel on ultrasound (red arrow).
The position of the foot during the access procedure is important. We recommend placing the foot in plantar flexion when accessing the dorsalis pedis and anterior tibial artery and inverting the foot when accessing the distal peroneal artery in the leg, which is not a vessel that is typically accessed. We also prefer eversion and dorsiflexion when accessing the posterior tibial artery in the distal leg.
Choosing the site of vessel access is important to achieve success, and it is usually an area that is patent and as healthy as possible. A micropuncture needle is used for access. Sometimes bending the needle tip rather than keeping the needle straight can make easier it to access the vessel. This is particularly helpful if the point of access is in the anterior tibial artery, just above the ankle, or in the posterior tibial artery. After accessing the artery (as evidenced by back bleeding), the micropuncture access wire (0.018 in) is passed through the needle into the vessel under fluoroscopic guidance (Figure 3). The needle is removed, and a micropuncture 4-Fr sheath is passed over the wire, securing access. Sometimes we use only the dilator of the sheath without the sheath itself to secure access (Figure 4). Cook Medical Inc. (Bloomington, IN) has a commercially available dedicated pedal access kit. The kit includes a 21-gauge, 4-cm echogenic needle; a 7-cm long micropuncture 4-Fr introducer with a 2.9-Fr inner diameter; and a Check-Flo® hemostasis valve that attaches directly to the introducer to inject fluids and contrast (Figure 5). Once the retrograde introducer is in place, the patient is fully heparinized in the usual fashion to avoid any thrombosis in the tibial vessels during the intervention. Some operators elect to use the 0.018-in wire in a sheathless manner to reduce the risk of disrupting the access vessel—the dorsalis pedis or distal tibial arteries.8 We recommend placing at least the inner dilator of the micropuncture sheath into the vessel to secure access. We also suggest performing an angiogram through the dilator to confirm placement in the true lumen of the artery at the access site, something that is never certain if the wire is used in a sheathless manner.
Figure 3.
Successful dorsalis pedis artery access. (A) Dilator of micropuncture sheath in place. (B) Fluoroscopy showing the wire through the distal anterior tibial artery.
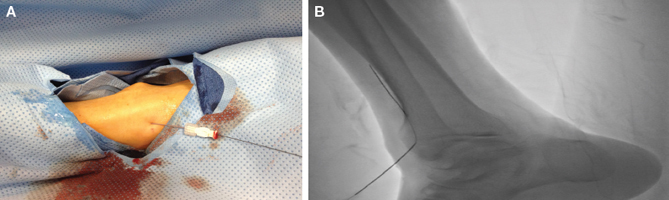
Figure 4.
Confirmation of the intraluminal position of the micropuncture sheath dilator in the anterior tibial artery.
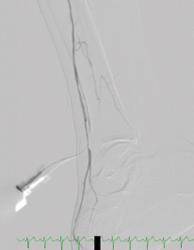
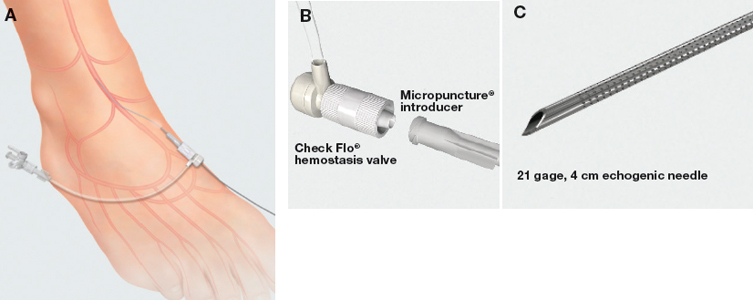
Figure 5.
The micropuncture tibial set from Cook Medical. (A) Cook introducer inserted percutaneously into the dorsalis pedis artery. (B) Check-Flo® hemostasis valve attachment to the introducer. (C) 21-gauge, 4-cm echogenic access needle. Printed with permission from Cook Medical Inc., Bloomington, Indiana.
Crossing the Occlusion
Once access into the tibial/pedal vessel is gained, the next step is crossing the occlusion. The process usually starts with an attempt at passing a wire from the pedal access site proximally, which in most cases is successful at crossing the occlusion and obtaining access into the proximal patent true lumen above the occlusion. The choice of wire is a point of personal preference. Some operators use 0.014-in wires, which have the advantage of being the smallest available caliber.10 However, in our experience and that of others, use of the 0.014-in wire has been disappointing as this platform does not usually have enough body to support the retrograde crossing of the tibial occlusion.4 Some other operators use the 0.035-in Terumo Glidewire® (Terumo Medical, Somerset, New Jersey) as the main wire for crossing the tibial occlusion.11 In our experience and others,8 the 0.018-in system had the best results crossing the occlusion. The V-18™ ControlWire® Guidewire (Boston Scientific, Natick, Massachusetts), is specifically helpful in this matter. It has a hydrophilic tip that can be modified in shape; the characteristics of the wire enable it to glide through the blockage with minimal friction and provide enough stiffness to push through total occlusions.
Use of the wire alone for crossing the lesion is not sufficient when there are long total occlusions and when there is significant calcification, since the platform needs more support to allow the crossing. In these cases, upsizing the access to a 4-Fr sheath, through which a Glidewire and glide catheter can be used, is extremely helpful.
Once the occlusion is crossed, the wire needs to be snared from above using a microsnare that is inserted from the common femoral artery access (Figure 6). The snaring process is better accomplished as distally as possible, just above the crossed occluded segment. This technique avoids the possibility of the tibial retrograde wire inadvertently finding its way into the subintimal plane above the occlusion in the popliteal or the superficial femoral artery.
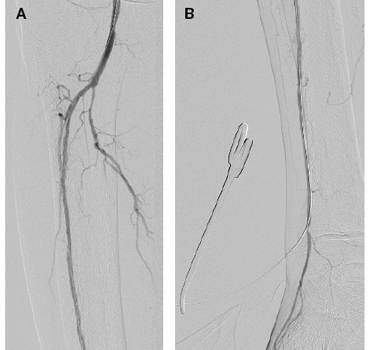
Figure 6.
Successful crossing of the anterior tibial artery occlusion. (A) Occluded anterior tibial artery. (B) Snaring of the 0.018-in wire (V-18TM) using microsnare. (C) Wire across the occluded segment. (D) The distal end of the wire outside the foot with ballooning of the channel.

A word of caution: the retrograde wire should always be an exchange-length wire to allow snaring and to provide enough wire length outside the body at the common femoral artery access site; this allows the passage of catheters, balloons, and other devices to treat the channel created through the occlusion.
Occasionally, the retrograde wire enters a subintimal plane that is different from that of the wire from the common femoral access; this will prevent successful snaring of the retrograde wire from above. In these situations, a novel technique is used to allow successful crossing of the septum between the two subintimal planes and allow snaring of the retrograde wire, as described by Montero-Baker and colleagues.11 With both wires in the separate subintimal planes, simultaneous balloon inflation over each wire is performed, just above the proximal end of the occlusion where both distal ends of the balloons are essentially touching each other (Figure 7). The goal of this maneuver is to disrupt the septum separating the two subintimal spaces to create a single lumen where snaring of the retrograde wire is possible.
Figure 7.
Double balloon technique for crossing the septum between two different subintimal planes. (A) Both balloons are in place in the different planes. (B) Successful wire crossing between the two lumens.

Once wire access across the occlusion is established, intervention is performed in the standard fashion, usually by balloon angioplasty or atherectomy. In our experience, we leave the tip of the retrograde wire protruding out of the introducer until the end of the procedure; the wire is kept in place by securing it with a hemostat. This approach provides a body-floss configuration of the wire that may be needed to help its trackability through a heavily calcified lesion and to improve its pushability. After the intervention is completed, and the inline flow through the occluded segment is confirmed by angiogram, the retrograde wire is withdrawn from above through the pedal/tibial puncture site. The retrograde introducer or sheath is then withdrawn and hemostasis is secured through digital compression for 5 to 10 minutes (Figure 8).
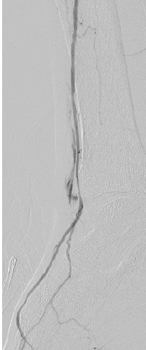
Figure 8.
Successfully recanalized anterior tibial artery. Note the patency of the vessel at the access site. (A) Patent proximal anterior tibial artery. (B) Patent access site.
There is often significant spasm at the arteriotomy and dilator/sheath site following dilator/sheath removal (Figure 9). This typically resolves through administration of intra-arterial nitroglycerin and/or low-pressure angioplasty with appropriately sized balloons.4
Figure 9.
Spasm and minimal extravasation at the puncture site after removal of the wire.
Published Data
The use of the pedal/tibial retrograde approach for the treatment of infrageniculate arterial occlusive disease has been reported only in case reports and some small case series.4, 6, 7, 9, 11-13
Botti and colleagues presented a series of six cases in which the retrograde pedal approach was attempted for critical limb ischemia with ulceration and failed antegrade recanalization of at least one tibial vessel runoff to the foot.13 Access was obtained through the posterior tibial artery in four patients and through the dorsalis pedis artery in two patients. All cases were successfully recanalized using the technique, with no major complications. Five patients showed complete healing and one patient had below-the-knee amputation due to a severe foot infection 3 months after the procedure.
Roger and colleagues presented a series of 13 cases with failed conventional antegrade recanalization of the tibial vessels.4 Indication for treatment was critical limb ischemia in eight cases, severe claudication in three cases, and acute limb ischemia in two cases. Eleven cases were accessed through the posterior tibial and two through the dorsalis pedis. In 11 cases, the technique was successful in recanalizing the accessed tibial vessel with restoration of inline flow. The two failed cases showed no deterioration in the condition of the limb, and there were no access-site complications in any of the cases.
Montero-Baker and colleagues reported using the technique in 51 cases.11 The indication for intervention was failed antegrade recanalization of at least one tibial vessel. Of the 51 patients, 45 had critical limb ischemia and 6 had severe claudication; 44 patients had successful recanalization of the anterior tibial or posterior tibial artery. There was a single instance of dorsalis pedis artery occlusion at the access site after a failed attempt to recanalize the anterior tibial artery. In that case, the patient underwent surgical thrombectomy and in situ pedal bypass the following day. No major complications related to the technique occurred.
At the VEITH symposium in 2010, Walker presented his series of 273 cases with critical limb ischemia in which the retrograde approach was attempted.12 The access was performed via the anterior tibial artery in 54% of cases, the posterior tibial in 45%, and the peroneal in 1%. Technical success was achieved in 96% of cases. The author noted a decrease in the level of amputation after revascularization in 49 of 57 patients who initially presented with advanced gangrenous changes.
Table 1 summarizes the results of the current published data on retrograde pedal/tibial access cases.
Table 1.
Current literature on the retrograde pedal/tibial approach for treating complex tibial occlusive disease.
| Series | Number | Indication | Vessel Accessed | Tech Success | Local complication | ||||
| CLI | Claudication | Acute Ischemia | ATA/ DPA | PTA | Per A | ||||
| Botti et al. (2003)13 | 6 | 6 (100%) | 0 | 0 | 2 | 4 | 0 | 6 (100%) | 0 |
| Fusaro et al. (2007)8 | 1 | 1 (100%) | 0 | 0 | 1 | 0 | 0 | 1 (100%) | 0 |
| Downer and Uberoi (2007)9 | 1 | 0 | 0 | 1 (100%) | 1 | 0 | 0 | 1 (100%) | 0 |
| Montero-Baker et al. (2008)11 | 51 | 45 (88%) | 6 (12%) | 0 | 22 | 29 | 0 | 44 (86%) | 1 (2%) |
| Walker C. (2010)12 | 273 | 273 (100%) | 0 | 0 | 148 | 123 | 2 | 254 (93%) | 0 |
| Rogers et al. (2011)4 | 13 | 8 (62%) | 3 (23%) | 2 (15%) | 2 | 11 | 0 | 11 (85%) | 0 |
| Total | 345 | 333 (96%) | 9 (3%) | 3 (1%) | 176 | 167 | 2 | 317 (92%) | 1 (0.3%) |
CLI: critical limb ischemia; ATA: anterior tibial artery; DPA: dorsalis pedis artery; PTA: posterior tibial artery; Per A: peroneal artery
Discussion
Pedal access is a relatively recent innovation in vascular interventions. It is important for the treatment of critical limb ischemia patients with tibial disease when the regular antegrade approach for crossing the occlusion is not possible, which occurs in about 20% of these patients. In these cases, the retrograde approach is a very successful technique for crossing the occlusion, and it has a very low rate of occlusion at the access point of the pedal/tibial vessel. It is not known why accessing the pedal/tibial vessels in retrograde fashion is more successful than the antegrade approach, but there are several technical advantages of this technique compared to the traditional approach that might contribute to its high success rate. The access point into the vessel is very close to the occlusive lesion, which provides more control and pushability of the wire through the occlusion. There is much less tendency of the wire to be diverted from the main vessel into a side or collateral branch, as these usually are pointing downwards, opposite to the direction of the wire. It has been proposed through the cardiac literature that the distal part of the occlusion might consist of less fibrotic or calcific tissue, allowing easier passage of the guidewire into the occlusion.14 We believe, as others do,4 that this proposed scenario also applies to the lower-extremity occlusive lesions. All of these factors allow the successful crossing of the tibial disease occlusion in a retrograde fashion when the usual antegrade approach fails.
The technique, however, is not without difficulties and complications. It has a definite learning curve that requires between five and ten cases for proficiency. Tibial vessels at the point of access can be too small to allow successful access into the lumen using the micropuncture needle. The tibial vessels are usually heavily calcified, which interferes with crossing the occlusion. In our opinion, this is the most important factor causing failed recanalization using the retrograde pedal/tibial approach. Since arterial spasm at the access site is very common, the liberal use of vasodilators including nitroglycerine and papaverine is necessary during the procedure.
The possibility of arterial disruption with resultant thrombosis at the access site has been reported in the literature. Although rare, this is a devastating complication that can have a drastic effect on the involved limb. The risk increases when the access vessel is small. This has led operators to use a variety of techniques to limit the risk of injuring the accessed tibial vessel, which is essentially related to the size of the puncture site. Gandini et al. used a 4-Fr sheath for pedal access.15 Botti et al. used only the 4-Fr introducer, which allowed passage of the 0.018-in wire but did not allow use of any adjunctive tools (such as catheters or balloons) to guide the wire through the occlusion.13 Spinosa et al. used a 3-Fr sheath and a 3-Fr catheter to help the passage of the wire.7 Fusaro et al. described a sheathless approach, introducing only a 0.018-in guidewire through the puncture needle for passing the lesion, thus avoiding the introduction of a sheath and keeping the access site as small as possible.8 The current Cook Medical Micropuncture® Pedal Access Set has a 4-Fr introducer with a 2.9-Fr inner diameter that allows passage of 0.018- or 0.014-in catheters or balloons as adjunctive tools for crossing the tibial occlusion.
The technique is relatively safe and feasible based on all reports in the literature to date. However, it only should be used for limb salvage in patients with critical limb ischemia, especially for those who have no feasible open surgical options due to prohibitive surgical risk, lack of suitable conduit, or patient reluctance to utilize the open surgical option. In our opinion, the use of this approach in cases of claudication should be condemned, especially in patients with a single runoff to the foot, as it involves a small albeit real risk of destroying the only existing runoff to the foot. This may result in limb loss in someone who was not initially at risk.
Conclusion
Although retrograde pedal/tibial artery access is a relatively new technique, it is a promising alternative for patients in whom conventional endovascular techniques failed to achieve recanalization of the tibial vessels. This approach has a high technical success rate and a relatively low procedural complication rate. Reports in the literature are still few and under-reported, and there are no long-term results regarding the effects on limb salvage and quality of life measurements. As new technology and research emerge, we will continue to gain further understanding of the ideal uses of the technique.
Funding Statement
Funding/Support: The author has no funding disclosures
Footnotes
Conflict of Interest Disclosure: The author has completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
References
- 1.Bosiers M, Hart JP, Deloose K, Verbist J, Peeters P. Endovascular therapy as the primary approach for limb salvage in patients with critical limb ischemia: experience with 443 infrapopliteal procedures. Vascular. 2006 Mar-Apr;14(2):63–9. doi: 10.2310/6670.2006.00014. [DOI] [PubMed] [Google Scholar]
- 2.Dorros G, Jaff MR, Dorros AM, Mathiak LM, He T. Tibioperoneal (outflow lesion) angioplasty can be used as primary treatment in 235 patients with critical limb ischemia: five-year follow-up. Circulation. 2001 Oct 23;104(17):2057–62. doi: 10.1161/hc4201.097943. [DOI] [PubMed] [Google Scholar]
- 3.Faglia E, Dalla Paola L, Clerici G, Clerissi J, Graziani L, Fusaro M, et al. Peripheral angioplasty as the first-choice revascularization procedure in diabetic patients with critical limb ischemia: prospective study of 993 consecutive patients hospitalized and followed between 1999 and 2003. Eur J Vasc Endovasc Surg. 2005 Jun;29(6):620–7. doi: 10.1016/j.ejvs.2005.02.035. [DOI] [PubMed] [Google Scholar]
- 4.Rogers RK, Dattilo PB, Garcia JA, Tsai T, Casserly IP. Retrograde approach to recanalization of complex tibial disease. Catheter Cardiovasc Interv. 2011 May 1;77(6):915–25. doi: 10.1002/ccd.22796. [DOI] [PubMed] [Google Scholar]
- 5.Iyer SS, Dorros G, Zaitoun R, Lewin RF. Retrograde recanalization of an occluded posterior tibial artery by using a posterior tibial cutdown: two case reports. Cathet Cardiovasc Diagn. 1990 Aug;20(4):251–3. doi: 10.1002/ccd.1810200408. [DOI] [PubMed] [Google Scholar]
- 6.Spinosa DJ, Leung DA, Harthun NL, Cage DL, Fritz Angle J, Hagspiel KD, et al. Simultaneous antegrade and retrograde access for subintimal recanalization of peripheral arterial occlusion. J Vasc Interv Radiol. 2003 Nov;14(11):1449–54. doi: 10.1097/01.rvi.0000096764.74047.21. [DOI] [PubMed] [Google Scholar]
- 7.Spinosa DJ, Harthun NL, Bissonette EA, Cage D, Leung DA, Angle JF, et al. Subintimal arterial flossing with antegrade-retrograde intervention (SAFARI) for subintimal recanalization to treat chronic critical limb ischemia. J Vasc Interv Radiol. 2005 Jan;16(1):37–44. doi: 10.1097/01.RVI.0000141336.53745.4A. [DOI] [PubMed] [Google Scholar]
- 8.Fusaro M, Tashani A, Mollichelli N, Medda M, Inglese L, Biondi-Zoccai GG. Retrograde pedal artery access for below-the-knee percutaneous revascularisation. J Cardiovasc Med (Hagerstown). 2007 Mar;8(3):216–8. doi: 10.2459/01.JCM.0000260819.30423.db. [DOI] [PubMed] [Google Scholar]
- 9.Downer J, Uberoi R. Percutaneous retrograde tibial access in the endovascular treatment of acute limb ischaemia: a case report. Eur J Vasc Endovasc Surg. 2007 Sep;34(3):350–2. doi: 10.1016/j.ejvs.2007.04.025. [DOI] [PubMed] [Google Scholar]
- 10.Fusaro M, Dalla Paola L, Biondi-Zoccai GG. Retrograde posterior tibial artery access for below-the-knee percutaneous revascularization by means of sheathless approach and double wire technique. Minerva Cardioangiol. 2006 Dec;54(6):773–7. [PubMed] [Google Scholar]
- 11.Montero-Baker M, Schmidt A, Braunlich S, Ulrich M, Thieme M, Biamino G, et al. Retrograde approach for complex popliteal and tibioperoneal occlusions. J Endovasc Ther. 2008 Oct;15(5):594–604. doi: 10.1583/08-2440.1. [DOI] [PubMed] [Google Scholar]
- 12.Walker C. Durability of PTAs using pedal artery approaches. 37th Annual VEITH Symposium; November 18th 2010; New York City, NY 2010. [Google Scholar]
- 13.Botti CF, Jr, Ansel GM, Silver MJ, Barker BJ, South S. Percutaneous retrograde tibial access in limb salvage. J Endovasc Ther. 2003 Jun;10(3):614–8. doi: 10.1177/152660280301000330. [DOI] [PubMed] [Google Scholar]
- 14.Saito S. Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc Interv. 2008 Jan 1;71(1):8–19. doi: 10.1002/ccd.21316. [DOI] [PubMed] [Google Scholar]
- 15.Gandini R, Pipitone V, Stefanini M, Maresca L, Spinelli A, Colangelo V, et al. The “Safari” technique to perform difficult subintimal infragenicular vessels. Cardiovasc Intervent Radiol. 2007 May-Jun;30(3):469–73. doi: 10.1007/s00270-006-0099-3. [DOI] [PubMed] [Google Scholar]


