
Case Report
A 29-year-old female with a history of Wegener’s granulomatosis presented with new-onset chest pain and shortness of breath. The chest pain was described as a sharp, pressure type of pain located over her entire chest, radiating to her back, and becoming worse when both lying down and breathing deeply. A day prior to admission, the patient’s chest pain worsened to the point that she could not lie flat in any position; this prompted her visit to the emergency room.
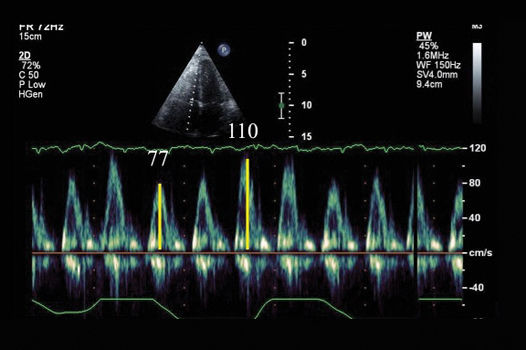
Pertinent physical findings include jugular venous distention and pulsus paradoxus. Chest X-ray showed prominent cardiac silhouette, and a 12-lead EKG showed sinus tachycardia (rate 120 bpm). A computed tomography (CT) chest scan showed no evidence of pulmonary embolism; however, a moderate-sized pericardial effusion was noted. A two-dimensional echocardiogram revealed normal left ventricular (LV) systolic function, diastolic septal bounce, and a moderate-sized anterior pericardial effusion. Doppler interrogation study showed significant respiratory variation of LV and RV inflow velocities (Figures 1, 2) consistent with ventricular septal interdependence, a feature of pericardial constraint. Based on these clinical and echocardiographic findings, the patient was diagnosed with acute effusive/constrictive pericarditis (CP).
Figure 1.
MV inflow Doppler. Peak E velocity showing a 39% decrease during inspiration. A >25% MV inflow variation is consistent with constrictive physiology.4
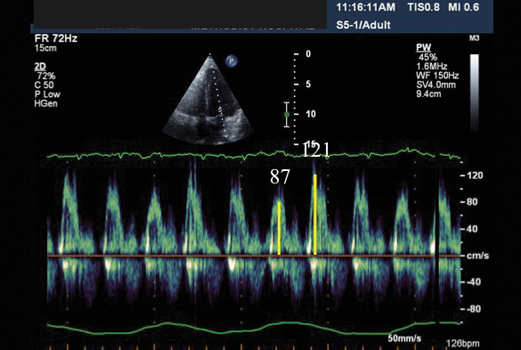
Figure 2.
TV inflow Doppler. Peak E velocity showing a 43% increase during inspiration. A >40% TV inflow variation is consistent with constrictive physiology.5
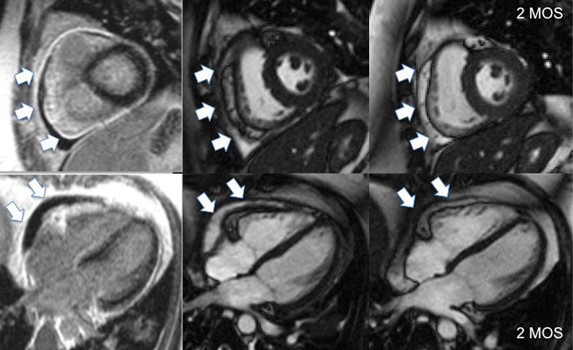
Cardiac magnetic resonance imaging (CMR) was ordered to further assess pericardial thickening and constriction. The pericardium was thickened (6 mm) and appeared bright on delayed enhancement (DE) imaging (Figure 3), which is consistent with an acute inflammatory process. A trial of steroid therapy was recommended, and the patient was sent home with a tapering dose of oral prednisone. Two months later the patient returned for a follow-up clinic visit and repeat CMR study. Her chest discomfort and dyspnea had completely resolved. The CMR demonstrated significant decrease in both pericardial thickness and pericardial hyperenhancement with complete resolution of the pericardial effusion (Figure 3).
Figure 3.
The left column depicts inversion recovery gradient echo sequences showing hyperenhancement of the pericardium (arrows) at time of diagnosis. The middle column shows steady-state free precession images that illustrate the pericardial thickness at baseline. The right column shows significant decrease in pericardial thickness of the pericardium at 2 months after receiving steroid therapy.
Discussion
Classic CP is characterized by thick pericardial fibrosis and frequent calcification that causes progressively debilitating heart failure.1 Transient CP was coined by Sagrista-Sauleda et al. in 1987.2 They reported that 16 of 177 patients (9%) experiencing acute effusive pericarditis with signs of constriction had resolution of symptoms with medical therapy and observation. They also described a three-phase evolutionary pattern of constrictive pericarditis. The first phase occurs with a moderate amount of pericardial effusion without signs of constriction. The second phase involves development of constrictive physiology. The third phase is normalization of hemodynamics with no evidence of constriction recurrence.2 In another observational study, Haley et al. identified 212 patients with echocardiographic findings of CP from 1988 to 1999.3 A total of 36 patients from this group showed resolution of constrictive hemodynamics without pericardiotomy. The most common cause of transient CP in these 36 patients was pericardial inflammation after pericardiotomy (9 patients, 25%), but transient constrictive physiologic features were reported to occur with any condition that causes chronic CP except for radiation therapy.
The ability of DE-CMR to detect reversible/transient CP is relatively new, and prior to this, no known imaging modality has been able to identify pericardial inflammation. Histopathological correlation has revealed that in CP patients who are positive for DE, there is more fibroblastic proliferation and neovascularization and more prominent inflammation and granulation tissue.6 In a pilot study, Feng et al. was able to show that anti-inflammatory therapy for CP was associated with a reduction in pericardial and systemic inflammation, DE and pericardial thickness, and resolution of CP physiology and symptoms.1 This knowledge can give us the ability to delineate between reversible and classic CP and focus medical therapies or invasive intervention based on the etiology of CP.
Summary
This case underscores the classic use of Doppler echocardiography to demonstrate the augmented variation in left and right ventricular filling velocities due, in part, to the ventricular septal shift that can occur with pericardial constraint of ventricular filling. In addition, this case highlights the additional value of CMR in assessing not only pericardial thickening but also acute pericardial inflammation and recovery following medical therapy.
Contributor Information
Jeffrey D. Dela Cruz, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
Dipan J. Shah, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
Stephen H. Little, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
References
- 1.Feng D, Glockner J, Kim K, Martinez M, Syed IS, Araoz P, et al. Cardiac magnetic resonance imaging pericardial late gadolinium enhancement and elevated inflammatory markers can predict the reversibility of constrictive pericarditis after antiinflammatory medical therapy: A pilot study. Circulation. 2011 Oct 25;124(17):1830–7. doi: 10.1161/CIRCULATIONAHA.111.026070. [DOI] [PubMed] [Google Scholar]
- 2.Sagristà-Sauleda J, Permanyer-Miralda G, Candell-Riera J, Angel J, Soler-Soler J. Transient cardiac constriction: an unrecognized pattern of evolution in effusive acute idiopathic pericarditis. Am J Cardiol. 1987 Apr 15;59(9):961–6. doi: 10.1016/0002-9149(87)91134-9. [DOI] [PubMed] [Google Scholar]
- 3.Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK. Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol. 2004 Jan 21;43(2):271–5. doi: 10.1016/j.jacc.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 4.Hatle LK, Appleton CP, Popp RL. Differentiation of constrictive pericarditis and restrictive cardiomyopathy by Doppler echocardiography. Circulation. 1989 Feb;79(2):357–70. doi: 10.1161/01.cir.79.2.357. [DOI] [PubMed] [Google Scholar]
- 5.Klein AL, Cohen GI, Pietrolungo JF, White RD, Bailey A, Pearce GL, et al. Differentiation of constrictive pericarditis from restrictive cardiomyopathy by Doppler transesophageal echocardiographic measurements of respiratory variations in pulmonary venous flow. J Am Coll Cardiol. 1993 Dec;22(7):1935–43. doi: 10.1016/0735-1097(93)90782-v. [DOI] [PubMed] [Google Scholar]
- 6.Zurick AO, Bolen MA, Kwon DH, Tan CD, Popovic ZB, Rajeswaran J, et al. Pericardial delayed hyperenhancement with CMR imaging in patients with constrictive pericarditis undergoing surgical pericardiectomy: a case series with histopathological correlation. JACC Cardiovasc Imaging. 2011 Nov;4(11):1180–91. doi: 10.1016/j.jcmg.2011.08.011. [DOI] [PubMed] [Google Scholar]


