Abstract
Objective
To examine the relationships among low back pain (LBP), inadequate physical activity, and sleep deficiency among patient care workers, and of these outcomes to work context.
Methods
A cross-sectional survey of patient care workers (N=1572, response rate=79%).
Results
53% reported LBP, 46%, inadequate physical activity, and 59%, sleep deficiency. Inadequate physical activity and sleep deficiency were associated (p=0.02), but LBP was not significantly related to either. Increased risk of LBP was significantly related to job demands, harassment at work, decreased supervisor support, and job title. Inadequate physical activity was significantly associated with low decision latitude. Sleep deficiency was significantly related to low supervisor support, harassment at work, low ergonomic practices, people-oriented culture, and job title.
Conclusions
These findings point to shared pathways in the work environment that jointly influence multiple health and wellbeing outcomes.
Keywords: healthcare workers, registered nurses, aides, musculoskeletal disorders (MSDs), back pain, physical activity, insufficient sleep, safety practice, job strain, ergonomic practice, culture, harassment, shift work
Introduction
Healthcare is the second-fastest-growing sector of the U.S. economy, employing over 12 million workers,1 and is one of the most dangerous places to be employed. 2 Compared to other sectors, healthcare workers sustain the second highest number of nonfatal injuries and illnesses. 3,4 These workers face a wide range of hazards on the job, including a high risk for musculoskeletal disorders (MSDs), especially low back pain (LBP). Reports of LBP among nurses and other patient care workers range from 30–60%, 5–8 and may contribute to the exodus of nurses from this profession. 6, 9
LBP has been associated with inadequate physical activity and sleep deficiencies. 10–17 The potential for synergistic impacts across these outcomes is apparent. Workers who sustain injuries are less able to be physically active during leisure time. 18 Conversely, sedentary behavior increases risk for LBP and injury 10 and among those already injured, prolongs disability and adds to the risk of further occurrence of LBP.19, 20 There is clear evidence that sedentary behavior is also associated with increased risk of all-cause and cardiovascular disease mortality.21–26 National guidelines for physical activity recommend that adults engage in at least 30 minutes of moderate-intensity activity, five days per week, or 20 minutes of vigorous intensity activity, three days per week.27 Nonetheless, in 2007, the percentage of U.S. adults classified as physically active was only 48.8%, including 50.7% of men and 47.0% of women, based on self-reports in telephone interview.28 When physical activity is measured using accelerometers, estimates of adherence to these guidelines may be as low as 5%.29 For workers in physically demanding jobs, being on one’s feet all day may contribute to fatigue and the need for recovery at the end of the day.30 Contrary to workers’ perceptions, however, being in a physically demanding job does not necessarily contribute to meeting physical activity recommendations. For example, the physical demands of lifting patients do not provide a means of building cardiovascular fitness, as through the recommended levels of moderate to vigorous physical activity. Low levels of physical activity are also associated with absenteeism, reduced productivity, increased health care costs, and short-term disability. 31–34
Similarly, research clearly points to the influence of work patterns, such as long work hours, on sleep, and underscores the hazards of work patterns that cause sleep deficiency (insufficient sleep duration and/or inadequate sleep quality).35 Habitual patterns of insufficient sleep duration independently predict an increased risk of a fall or other injury requiring an emergency room visit.36 In healthcare workers, sleep duration and extended shifts are related to healthcare workplace-associated injuries and patient safety-related errors, including motor vehicle crashes,37 medical errors38 and percutaneous injuries.39 Working night or rotating shifts (i.e., sleeping during the daytime) has deleterious consequences not only for sleep cycles but for health outcomes as well.40–43 In addition, for patient care workers, working nights and the associated sleep disruptions may contribute to increased risk of MSD’s, reduced physical activity, and compromised dietary patterns, often contributing to increased weight.40
Prior research points to the important roles of job characteristics and the context of the work environment in risk of LBP, inadequate physical activity, and sleep deficiencies. In addition to the physically demanding nature of the work,44, 45 patient care workers’ increased risk for MSDs, including LBP, is associated with high work demands, low social support, and long work hours. 46–49 Similar characteristics of the work environment may contribute to sleep deficiency.43, 50 and inadequate physical activity.51–53 Despite the shared risks posed by the work environment, however, little research has systematically explored these cross-cutting pathways and their implications for improving the effectiveness of comprehensive worksite interventions to address the broad spectrum of worker health outcomes.54
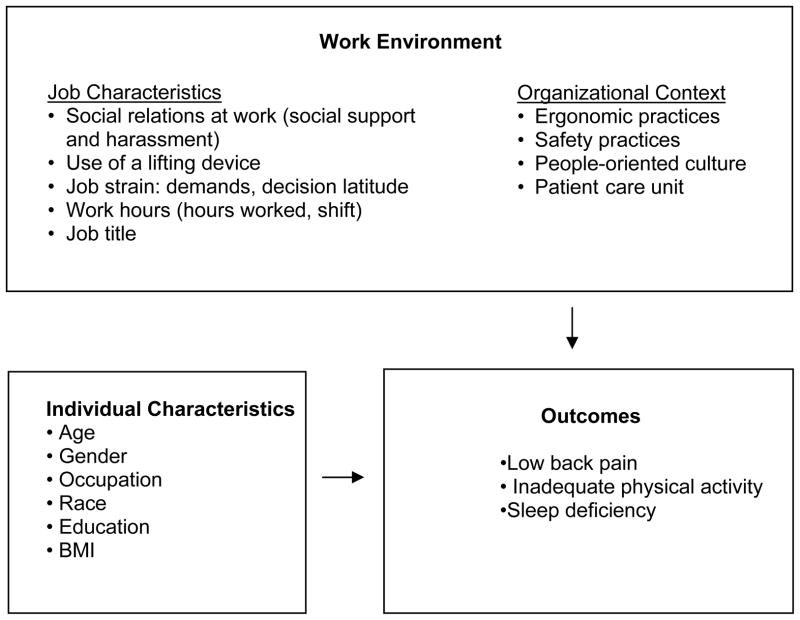
This paper examines the relationships among LBP, inadequate physical activity, and sleep deficiency among hospital patient care workers, which in combination, may pose an additive threat to worker health and wellbeing. In addition, we explore the relationships of characteristics of the work environment to these wellness outcomes, as illustrated in Figure 1. These findings may inform intervention design by helping to prioritize intervention targets; elements of the work environment that impact more than one outcome may be an especially high priority for workplace interventions. Specifically, we hypothesize that: (1) the three wellness outcomes -- presence of LBP, inadequate physical activity and sleep deficiency –are associated with one another; and (2) the three wellness outcomes are associated with common characteristics of the work environment, including job characteristics (i.e., social relations at work, job strain, use of a lifting device, work hours and schedule, and job title) and organizational context (i.e., the safety practices, ergonomic practices, a people-oriented culture, and work unit).
Figure 1.
Conceptual model
Methods
Study Design
The “Be Well Work Well Study” is one of three studies conducted by the Harvard School of Public Health Center for Work, Health and Wellbeing. Data presented here were collected through a cross-sectional survey of patient care workers conducted in two large teaching hospitals in the Boston area in late 2009. This survey was conducted as part of research aimed at identifying the relationships among worksite policies, programs and practices, and worker health and economic outcomes, through analysis of employee record data, a review of policies and an examination of their implementation through a survey of nurse managers, and this survey of patient care workers. This survey was designed to evaluate associations of MSDs and worker health behaviors to physical and psychosocial exposures on the job, as well as preventive measures in place. This study was approved by the applicable Institutional Review Board for protection of human subjects.
Sample
The sampling frame for the Patient Care Worker Survey included all workers employed between October 1, 2008 and September 30, 2009, who worked 20 hours per week or more or who were designated as at least half time in Patient Care Services and who had direct patient care responsibilities (including registered nurses, licensed practical nurses, and patient care assistants/nursing assistants). Eligible employees worked in patient care units under the direction of a nurse director. Patient care workers assigned to the “float” unit were eligible to participate in the survey; allied health professionals (e.g., physical therapy, occupational therapy), support staff assigned to environmental services any staff on physical medicine units were excluded. Also ineligible were workers on an extended absence greater than 12 weeks, per diem staff, and traveling or contract nurses.
Data collection
This survey was conducted between October 2009 and February 2010 at two large teaching hospitals in the greater Boston area. We randomly selected 2000 eligible workers, and invited them via email to participate in the survey on line. After two reminders and four weeks, we mailed a paper version of the survey to workers who had not yet completed the survey on-line. A second paper survey and a third email reminder were sent to all non-respondents after another two weeks; one month later a final email reminder was sent to all non-respondents. A total of 1572 workers initiated completion of the survey on line. Of those, 1399 (89%) completed at least 50% of the survey items and met our definition of survey completion. An additional 173 workers returned a completed mailed version of the survey. The total number of completed surveys is 1572 for a response rate of 79%.
Measures
Outcomes
Low back pain was measured using an adaptation of the Nordic question, “During the past 3 months, have you had pain or aching in any of the areas shown on the diagram?” 55 Using a diagram as a reference, respondents were asked to identify areas in which they experienced pain: lower back, shoulder, wrist or forearm, knee, neck, ankle or feet, and none of the above.
The measure of physical activity was adapted from the Centers for Disease Control Behavioral Risk Factor and Surveillance System Physical Activity measure.56 We asked respondents about their participation in vigorous and moderate physical activity of at least 10 minutes’ duration outside of work. For each, we asked the number of days per week they participate in the activity and the total time (hours and minutes) per day. Adequate physical activity was defined as reporting at least 30 minutes of moderate or vigorous activity on at least 5 days a week or at least 20 minutes of vigorous activity on at least 3 days a week.27
Sleep deficiency was operationalized as the presence of insufficient sleep duration and/or inadequate sleep quality using responses to a series of questions regarding sleep habits in the preceding four weeks, as adapted from the Pittsburgh Sleep Quality Index. 57 Respondents were asked how many hours they slept each night. Insomnia symptoms were assessed by asking how often they had difficulty falling asleep, woke in the middle of the night or awoke early, with four response categories from not at all in the last 4 weeks to 3 or more times a week. Sleep quality was assessed by asking how often they got enough sleep to feel rested upon waking, with five response categories from never to always. 58 Sleep deficiency was defined as a report of at least one of the following: insufficient sleep duration (<6h/day) or inadequate sleep quality (never feeling rested on waking) or insomnia symptoms 3 or more times a week.
Job characteristics
Three aspects of social relations on the job were measured. Coworker support was assessed using two items: “If needed, I can get support and help with my work from my co-workers.” “The people I work with are helpful in getting the job done.” The responses, each ranging from 1 to 5, were summed resulting in a scale that ranged from 2 to 10. Similarly, supervisor support was measured using three items: “If needed, I can get support and help with my work from my immediate supervisor,” “My supervisor is helpful in getting the job done,” “My work achievements are appreciated by my immediate supervisor,” with response categories on the same five point scale. The responses were summed resulting in a scale that ranged from 3 to 15. These social support scales were adapted from the Job Content Questionnaire.59, 60 Harassment was measured by asking five questions, assessing frequency in the last 12 months of someone at work yelling or screaming at the respondent, making hostile or offensive gestures, swearing at, talking down to, or treating the respondent poorly.61 A participant was coded as experiencing harassment if she/he reported “more than once” to any of the five questions.
Job strain was assessed using the abbreviated version of the Job Content Questionnaire (JCQ),59 focusing on the three sub-scales: psychological job demand (5 items); decision authority (3 items); and skill discretion (5 items). Decision latitude was created as a weighted sum of decision authority and skill discretion. A worker was defined as having job strain if his/her psychological demand was greater than the national median while decision latitude was below the national median. National medians 60, 62 were re-scaled to adjust for the different number of items used in our study.
Use of a lifting device was measured by a single item, “In general, when a patient needs to be moved, how often do you use a lifting device?” with five response categories from “never” to “always “ as well as an option to indicate that the respondent does not lift patients.
We measured work hours by self-report of the number of hours worked in a typical week at this job. Work shift was also measured by self-report. Job title was categorized as Assistant Nurse Manager, Clinical Nurse Specialist, Staff Nurse, Patient Care Associate, Operations Coordinator, and other.
Organizational context
We measured four indicators of the organizational context: people-oriented culture, ergonomic practices, safety practices, and work unit. For three of these measures, we used the Organizational Policies and Practices (OPPs) questionnaire, developed by Amick et al, which was designed to address organizational context in relation to injury claims and disability management. 63 We adapted some of the item wording to better match the healthcare setting and to indicate that the item was referring to the work unit, not the entire workplace. We also designed several related items to capture similar constructs in ways appropriate for this work setting. We used factor analysis to evaluate the new items in conjunction with the standard and reworded items and based our study scales on those results. The people-oriented culture scale included four items to assess the extent to which employees are engaged in meaningful decision making in their work unit. Our ergonomic practices scale included six items concerning the design of work to reduce lifting; pushing and pulling; bending reaching and stooping; the use of other ergonomic factors in work design and the purchase of equipment. Our safety practices scale combined items from the OPPs measures of safety diligence and safety training; it was comprised of eight items, including the identification and improvement of unsafe work conditions, housekeeping, equipment maintenance, action when safety rules are broken and whether supervisors confront and correct unsafe behaviors or hazards as well as items assessing safety leadership (e.g., the training of supervisors and employees in job hazards and safe work hazards) and two questions designed for this setting: “I feel free to report any unsafe working conditions where I work;” and “On this unit, employee suggestions about worker safety are supported by management.” The response scale for all items was a five-point scale, from strongly disagree to strongly agree. The responses were coded so that a high score indicated positive people-oriented culture, ergonomic practice or safety as appropriate and the items in each scale were summed. For comparability with the original OPPs scores, each score was divided by the number of items in the scale to create a scale ranging from 1 to 5.
Participants worked in 128 patient care units. The patient care work units were grouped into 12 categories reflecting similar workloads: Emergency Department (ER), Operating Room (OR), Adult Medical/Surgical, Adult intensive care (ICU), step-down, Pediatric Medical/Surgical, Pediatric/Neonatal intensive care, Psychiatry, Obstetrics/Postpartum, Float Pool, Ambulatory units and Orthopedics.
Individual characteristics
We asked participants about their individual characteristics including occupation, race/ethnicity, education, gender, age, height and weight. BMI was computed as weight (kg) per cm2 of height.
Statistical analyses
To evaluate the association among the three outcomes - LBP, inadequate physical activity and sleep deficiency - we used log-linear modeling methods. To explore the bivariate associations of job characteristics and organizational context with each of the outcomes, we used cross-classification and the Chi-square test of homogeneity. For each outcome, we then computed a multiple logistic regression analysis including all the measures that were bivariately associated with the outcome at p < 0.2. We then removed all variables with p> 0.05 in the multivariable model, resulting in a final model for each outcome that included only significant independent variables. We computed a common model for all the outcomes including all variables that were in the final model for any outcome so that the associations could be compared across outcomes. All analyses were carried out using SAS statistical software, version 9.2.64
Results
Characteristics of the sample
The sample of 1572 patient care workers was 91% women and 41 years old, on average. Most were of non-Hispanic white ethnicity (79%) (Table 1). Only 30% worked a regular day shift and nearly two-thirds (63%) worked fewer than 40 hours in a typical week.
Table 1.
Selected characteristics of hospital patient care workers (n=1572)
| Individual Characteristics | N | % |
|---|---|---|
|
|
||
| Gender | ||
| Male | 143 | 9.5 |
| Female | 1369 | 90.5 |
| Race/Ethnicity | ||
| Hispanic | 65 | 4.3 |
| White, non-Hispanic | 1185 | 79.1 |
| Black, non-Hispanic | 159 | 10.6 |
| Other | 89 | 5.9 |
| Education | ||
| Grade 12/GED or less | 78 | 5.2 |
| 1–3 years of college | 360 | 23.9 |
| Baccalaureate degree | 803 | 53.4 |
| Graduate degree | 264 | 17.5 |
| Mean (s.d.) | Min - Max | |
| Age (years) | 41.4 (11.7) | 21 – 73 |
| BMI (kg/m2) | 26.3 (5.3) | 18 – 44 |
|
|
||
| Work Context/Job Characteristics | N | % |
|
|
||
| Job Title | ||
| Staff Nurse | 1103 | 70.5 |
| Patient Care Associate | 127 | 8.1 |
| Other | 335 | 21.4 |
| Hours Worked per Week | ||
| Less than 29 hours | 347 | 22.2 |
| 30–34 | 188 | 12.0 |
| 35–39 | 453 | 28.9 |
| 40–44 | 508 | 32.4 |
| 45 or more | 70 | 4.5 |
| Shift | ||
| Regular day | 469 | 30.0 |
| All others | 1097 | 70.0 |
| Job Strain | ||
| Yes | 266 | 17.4 |
| No | 1259 | 82.6 |
| Harassment at work | ||
| Yes | 913 | 59.7 |
| No | 617 | 40.3 |
| Mean (s.d.) | Min - Max | |
| Decision latitude | 71.7 (9.7) | 28.5 – 96 |
| Demands | 35.9 (5.2) | 13.5 – 48 |
| Supervisor support | 10.6 (2.9) | 3 – 15 |
| Coworker support | 8.0 (1.5) | 2 – 10 |
| Safety Practices Scale | 3.83 (0.60) | 1.25 – 5 |
| Ergonomic Practices Scale | 3.13 (0.83) | 1 – 5 |
| People-oriented Culture Scale | 3.59 (0.75 | 1 – 5 |
Among the 1496 respondents for whom we had complete data for all three outcomes, 788 (53%) reported experiencing LBP in the last 3 months, 677 (45%) reported not meeting the recommended guidelines for physical activity (PA) and 884 (59%) reported sleep deficiency. A total of 234 (16%) reported all three outcomes and 569 (38%) reported two of the three outcomes (Table 2). Sleep deficiency was higher among those with inadequate PA, and similarly the prevalence of inadequate PA was higher in those with sleep deficiency. These relationships were the same whether a person reported LBP or not. Thus we saw a two-way association of sleep deficiency and inadequate PA that was independent of the presence of LBP. Log-linear modeling of the co-occurrence of the three risks confirmed that the three-way effect was not statistically significant (p=0.71); and that the two-way effects of LBP and inadequate physical activity, and LBP and sleep deficiency were not statistically significant. (p=0.33 and p=0.12, respectively). The association of inadequate physical activity and sleep deficiency, however, was statistically significant (p=0.02).
Table 2.
Number of respondents who report low back pain, inadequate physical activity and sleep deficiency.
| Low Back Pain | Physical Activity | Sleep deficiency
|
% Sleep deficient | |
|---|---|---|---|---|
| Yes | No | |||
|
| ||||
| Yes | Inadequate | 234 | 133 | 63.8 |
| Adequate | 247 | 174 | 58.7 | |
|
|
||||
| % Inadequate PA | 48.6 | 43.3 | ||
|
| ||||
| No | Inadequate | 189 | 121 | 61.0 |
| Adequate | 214 | 184 | 54.0 | |
|
|
||||
| % Inadequate PA | 46.9 | 39.7 | ||
Factors associated with the three outcomes
Bivariate associations of low back pain (LBP) with worker and work characteristics (Table 3)
Table 3.
Bivariate associations of low back pain, work context, and worker characteristics (N=1568)
| Variables | LOW BACK PAIN | P- value | |
|---|---|---|---|
| Yes (n=828, 52.8 %) | No (n=740, 47.2%) | ||
|
| |||
| Job Characteristics | |||
| Mean Support from Coworkers (SD) | 7.9 (1.5) | 8.1 (1.5) | 0.05 |
| Mean Support from Supervisor (SD) | 10.3 (3.0) | 11.0 (2.9) | < 0.0001 |
| Harassment at work | < 0.0001 | ||
| No | 263 (32.3%) | 352 (49.5%) | |
| Yes | 552 (67.7%) | 359 (50.5%) | |
| Use of a lifting device | 0.007 | ||
| Low (n %) | 310 (42.1%) | 234 (39.5%) | |
| Medium (n %) | 231 (31.3%) | 156 (26.2%) | |
| High (n %) | 196 (26.6%) | 203 (34.3%) | |
| Hours worked per week | 0.02 | ||
| Less than 30 hours (n %) | 184 (22.3%) | 164 (22.2%) | |
| 30–34 (n %) | 100 (12.1%) | 87 (11.8%) | |
| 35–39 (n %) | 258 (31.2%) | 193 (26.2%) | |
| 40–44 (n %) | 258 (31.2%) | 250 (33.9%) | |
| Over 44 hours (n %) | 26 (3.1%) | 44 (6.0%) | |
| Shift | 0.03 | ||
| Regular day (n %) | 229 (27.7%) | 240 (32.9%) | |
| All others (n %) | 598 (72.3%) | 496 (67.4%) | |
| Job title | |||
| Staff Nurse (n %) | 634 (76.8%) | 465 (63.3%) | < 0.0001 |
| Patient Care Associate (n %) | 65 (7.9%) | 62 (8.4%) | |
| Other (n %) | 127 (15.4%) | 208 (28.3%) |
|
| Job Strain |
<0.0001
|
||
| 0. No | 632 (78.4%) | 623(87.1%) |
|
| 1. Yes | 174 (21.6%) | 92 (12.9%) |
|
| Mean Demands (SD) | 36.8 (4.9) | 35.0 (5.3) | <0.0001 |
| Mean Decision Latitude (SD) | 71.4 (9.5) | 71.9 (9.8) | 0.32 |
| Organizational Context | |||
| Mean People-oriented Culture (SD) | 3.53 (0.76) | 3.65 (0.74) | 0.002 |
| Mean Ergonomic Practices Scale (SD) | 3.02 (0.80) | 3.25 (0.80) | < 0.0001 |
| Mean Safety Practices Scale (SD) | 3.76 (0.60) | 3.91 (0.58) | < 0.0001 |
| Work Unit | 0.26 | ||
| ER | 48 (5.8%) | 38 (5.1%) | |
| OR | 76 (9.2%) | 81 (11.0%) | |
| Variables | LOW BACK PAIN | ||
| Yes (n=828, 52.6 %) | No (n=747, 47.4%) | ||
|
|
|||
| Adult Med/Surg | 329 (39.7%) | 252 (34.0%) | |
| Adult ICU | 102 (12.3%) | 94 (12.7%) | |
| Step-down | 45 (5.4%) | 37 (5.0%) | |
| Ped Med/Surg | 9 (1.1%) | 11 (1.5%) | |
| Ped ICU/NICU | 33 (4.0%) | 33 (4.5%) | |
| Psychiatry | 6 (0.7%) | 14 (1.9%) | |
| OB/Post-partum | 60 (7.2%) | 70 (9.5%) | |
| Float Pool | 35 (4.2%) | 30 (4.0%) | |
| Amb/Consult/Educ | 85 (10.3%) | 80 (10.8%) | |
| Orthopedics | 20 (2.4%) | 21 (2.8%) | |
| Individual Characteristics | |||
| Gender | 0.21 | ||
| Male | 68 (8.6%) | 75 (10.4%) | |
| Female | 726 (91.4%) | 643 (89.6%) | |
| Race/ethnicity | 0.01 | ||
| Hispanic (n %) | 32 (4.0%) | 33 (4.7%) | |
| White (n %) | 649 (82.2%) | 536 (75.7%) | |
| Black (n %) | 67 (8.5%) | 92 (13.0%) | |
| Mixed/Other (n %) | 42 (5.3%) | 47 (6.6%) | |
| Education | 0.15 | ||
| Grade 12/GED or less (n %) | 29 (3.7%) | 49 (6.9%) | |
| 1–3 years of college (n %) | 178 (22.5%) | 182 (25.4%) | |
| 4 year college degree (n %) | 439 (55.6%) | 364 (50.9%) | |
| Any graduate school (n %) | 144 (18.2%) | 120 (16.8%) | |
| Mean Age (SD) | 40.5 (11.9) | 42.4 (11.4) | 0.001 |
| Mean BMI (SD) | 26.2 (5.3) | 26.4 (5.3) | 0.42 |
Workers who reported LBP also reported significantly lower levels of supervisor and coworker support, were more likely to report harassment at work, and were less likely use of a lifting device, compared with those not reporting LBP. Those who worked regular day shifts were less likely than other workers to report LBP, and a greater proportion of staff nurses than other workers reported LBP. In addition, workers with LBP reported significantly greater job demands, and correspondingly, higher levels of job strain, compared to workers without LBP. Workers with LBP also were significantly more likely to report lower people-oriented culture, lower safety practices and lower ergonomic practices than those without LBP.
Bivariate associations of physical activity with worker and work characteristics (Table 4)
Table 4.
Bivariate associations of physical activity, work context and worker characteristics (N=1518)
| Variables | PHYSICAL ACTIVITY | P-value | |
|---|---|---|---|
| Adequate (n=825,54.3 %) | Inadequate (n=693, 45.7%) | ||
|
| |||
| Job Characteristics | |||
| Mean Support from Coworkers (SD) | 8.2 (1.4) | 7.8 (1.5) | <.0001 |
| Mean Support from Supervisor (SD) | 10.8 (3.0) | 10.5 (2.9) | 0.06 |
| Harassment at work (n %) | 0.23 | ||
| No | 337 (41.7) | 261 (38.6) | |
| Yes | 471 (58.3) | 415 (61.4) | |
| Use of a lifting device | 0.75 | ||
| Low (n %) | 300 (41.5) | 226 (39.8) | |
| Medium (n %) | 206 (28.5) | 172 (30.3) | |
| High (n %) | 218 (30.0) | 170 (29.9) | |
| Hours worked per week | 0.15 | ||
| Less than 30 hours (n %) | 205 (24.9) | 135 (19.6) | |
| 30–34 (n %) | 98 (11.9) | 84 (12.2) | |
| 35–39 (n %) | 227 (27.6) | 205 (29.7) | |
| 40–44 (n %) | 260 (31.6) | 231 (33.4) | |
| Over 44 hours (n %) | 33 (4.0) | 35 (5.1) | |
| Shift | 0.73 | ||
| Regular day (n %) | 243 (29.5) | 209 (30.3) | |
| All others (n %) | 580 (70.5) | 480 (69.7) | |
| Job title | 0.0001 | ||
| Staff Nurse (n %) | 611 (74.2) | 455 (66.0) | |
| Patient Care Associate (n %) | 46 (5.6) | 74(10.7) | |
| Other, please specify (n %) | 166 (20.2) | 160 (23.2) | |
| Job Strain | 0.57 | ||
| No | 655 (81.8) | 558 (82.9) | |
| Yes | 146 (18.2) | 115 (17.1) | |
| Mean Demands (SD) | 36.1 (5.2) | 35.8 (5.2) | 0.27 |
| Mean Decision latitude (SD) | 72.7 (9.1) | 70.5 (10.0) | <.0001 |
| Organizational context | |||
| Mean People-oriented Culture Scale (SD) | 3.65 (0.72) | 3.54 (0.78) | 0.004 |
| Mean Ergonomic Practices Scale (SD) | 3.11 (0.84) | 3.17 (0.82) | 0.13 |
| Mean Safety Practices Scale (SD) | 3.85 (0.59) | 3.81 (0.61) | 0.25 |
| Work Unit | 0.90 | ||
| OR | 53 (6.4%) | 32 (4.6%) | |
| ER | 83 (10.1%) | 71 (10.2%) | |
| Adult Med/Surg | 309 (37.5%) | 256 (36.9%) | |
| Adult ICU | 106 (12.9%) | 80 (11.5%) | |
| Step-down | 42 (5.1%) | 39 (5.6%) | |
| Ped Med/Surg | 9 (1.1%) | 10 (1.4%) | |
| Variables | PHYSICAL ACTIVITY | P-value | |
| Adequate (n=825,54.3 %) | Inadequate (n=694, 45.7%) | ||
|
|
|||
| Ped ICU/NICU | 32 (3.9%) | 30 (4.3%) | |
| Psychiatry | 11 (1.3%) | 9 (1.3%) | |
| OB/Post-partum | 60 (7.3%) | 65 (9.4%) | |
| Float Pool | 34 (4.1%) | 28 (4.0%) | |
| Amb/Consult/Educ | 86 (10.4%) | 73 (10.5%) | |
| Orthopedics | 21 (2.6%) | 19 (2.7%) | |
| Individual Characteristics | |||
| Gender | 0.36 | ||
| Male | 83 (10.2) | 59 (8.8) | |
| Female | 734 (89.8) | 614 (91.2) | |
| Race/ethnicity | <.0001 | ||
| Hispanic (n %) | 25 (3.1) | 40 (6.0) | |
| White (n %) | 697 (85.8) | 477 (71.5) | |
| Black (n %) | 56 (6.9) | 98 (14.7) | |
| Mixed/Other (n %) | 34 (4.2) | 52 (4.2) | |
| Education | 0.0007 | ||
| Grade 12/GED or less (n %) | 27 (3.3) | 49 (7.34) | |
| 1–3 years of college (n %) | 181 (22.2) | 168 (25.1) | |
| 4 year college degree (n %) | 466 (57.2) | 331 (49.4) | |
| Any graduate school (n %) | 140 (17.2) | 122 (18.2) | |
| Mean Age (SD) | 40.6 (11.6) | 42.0 (11.7) | 0.02 |
| Mean BMI (SD) | 25.5 (4.8) | 27.4 (5.6) | <.0001 |
Respondents with inadequate physical activity reported significantly lower coworker support. A greater proportion of staff nurses reported adequate physical activity than other workers. Respondents with inadequate physical activity also reported lower decision latitude on the job as well as lower people-oriented culture and, compared with those with adequate physical activity. Physical activity was strongly associated with worker characteristics including race/ethnicity, education, BMI and age. Workers with inadequate physical activity had significantly higher BMI and were significantly older than those with adequate physical activity.
Bivariate associations of sleep deficiency with worker and work characteristics (Table 5)
Table 5.
Bivariate associations of sleep deficiency, work context and worker characteristics (N=1516)
| Variables | SLEEP DEFICIENCY | P-value | |
|---|---|---|---|
| Yes (n=896, 59.1 %) | No (n=620, 40.9%) | ||
|
| |||
| Job Characteristics | |||
| Mean Support from Coworkers (SD) | 7.9 (1.5) | 8.1 (1.5) | 0.003 |
| Mean Support from Supervisor (SD) | 10.4 (3.0) | 11.0 (2.9) | 0.0002 |
| Harassment at work | 0.0008 | ||
| No | 319 (36.5%) | 274 (45.1%) | |
| Yes | 555 (63.5%) | 333 (54.9%) | |
| Use of a lifting device | 0.92 | ||
| Low (n %) | 306 (40.2%) | 217 (41.3%) | |
| Medium (n %) | 226 (29.7%) | 152 (28.9%) | |
| High (n %) | 229 (30.1%) | 157 (29.9%) | |
| Hours worked per week | 0.047 | ||
| Less than 30 hours (n %) | 183 (20.5%) | 156 (25.3%) | |
| 30–34 (n %) | 116 (13.0%) | 66 (10.7%) | |
| 35–39 (n %) | 252 (28.2%) | 183 (29.7%) | |
| 40–44 (n %) | 296 (33.2%) | 193 (31.3%) | |
| Over 44 hours (n %) | 46 (5.2%) | 19 (3.1%) | |
| Shift | 0.65 | ||
| Regular day (n %) | 271 (30.4%) | 181 (29.3%) | |
| All others (n %) | 621 (69.7%) | 437 (70.7%) | |
| Job Title | 0.02 | ||
| Staff Nurse (n %) | 610 (68.3%) | 457 (74.1%) | |
| Patient Care Associate (n %) | 67 (7.5%) | 49 (7.9%) | |
| Other (n %) | 216 (24.2%) | 111 (18.0%) | |
| Job Strain | 0.01 | ||
| 0. No | 695 (80.3%) | 516 (85.4%) | |
| 1. Yes | 171 (19.8%) | 88 (14.6%) | |
| Mean Demands (SD) | 36.2 (5.2) | 35.5 (5.2) | 0.008 |
| Mean Decision latitude (SD) | 71.1 (10.0) | 72.6 (9.1) | 0.005 |
| Organizational Context | |||
| Mean People-oriented Culture Scale (SD) | 3.56 (0.75) | 3.65 (0.74) | 0.02 |
| Mean Ergonomic Practices Scale (SD) | 3.06 (0.83) | 3.23 (0.82) | <0.0001 |
| Mean Safety Practices Scale (SD) | 3.79 (0.62) | 3.90 (0.56) | 0.0004 |
| Variables | SLEEP DEFICIENCY | P-value | |
| Yes (n=1058, 70.1 %) | No (n=452, 29.9%) | ||
|
| |||
| Work Unit | 0.24 | ||
| ER | 54 (6.0%) | 30 (4.8%) | |
| OR | 94(10.5%) | 58 (9.4%) | |
| Adult Med/Surg | 300 (33.5%) | 219 (35.3%) | |
| Adult ICU | 120 (13.4%) | 71 (11.5%) | |
| Step-down | 46 (5.1%) | 35 (5.7%) | |
| Ped Med/Surg | 12 (1.3%) | 8 (1.2%) | |
| Ped ICU/NICU | 37 (4.1%) | 26 (4.2%) | |
| Psychiatry | 9 (1.0%) | 11 (1.8%) | |
| OB/Post-partum | 77 (8.6%) | 50 (8.1%) | |
| Float Pool | 35 (3.9%) | 29 (4.7%) | |
| Amb/Consult/Educ | 98 (10.9%) | 59 (9.5%) | |
| Orthopedics | 14 (1.6%) | 24 (3.9%) | |
| Individual Characteristics | |||
| Gender | 0.60 | ||
| Male | 81 (9.1%) | 61 (9.9%) | |
| Female | 806 (90.9%) | 553 (90.1%) | |
| Race/ethnicity | 0.52 | ||
| Hispanic (n %) | 39 (3.7%) | 23 (5.2%) | |
| White (n %) | 832 (79.7%) | 349 (78.8%) | |
| Black (n %) | 108 (10.3%) | 48 (10.8%) | |
| Mixed/Other (n %) | 65 (6.2%) | 23 (5.2%) | |
| Education | 0.24 | ||
| Grade 12/GED or less (n %) | 44 (5.0%) | 33 (5.4%) | |
| 1–3 years of college (n %) | 225 (25.5%) | 131 (21.4%) | |
| 4 year college degree (n %) | 456 (51.7%) | 344 (56.3%) | |
| Any graduate school (n %) | 157 (17.8%) | 103 (16.9%) | |
| Mean Age (SD) | 42.0 (12.0) | 40.5 (12.0) | 0.02 |
| Mean BMI (SD) | 26.6 (5.5) | 25.9 (4.9) | 0.01 |
Compared to workers reporting sufficient sleep, workers who reported sleep deficiency were significantly more likely to report low supervisor support and low coworker support, harassment at work, lower decision latitude, lower people-oriented culture, poorer safety practices, and poorer ergonomic practices. In addition those reporting sleep deficiency were more likely to be staff nurses and to work 40 hours per week or more than those reporting no deficiency. They were also significantly older and had greater BMI.
Multivariable associations with the outcomes (Table 6)
Table 6.
Multiple logistic regression analysis of each outcome on work context and worker characteristics
| Measure | Low Back Pain N=1228 |
Inadequate physical activity N=1219 |
Sleep deficiency N=1225 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
|
| |||||||||
| Job Characteristics | |||||||||
| Supervisor support | 0.95 | 0.91, 0.997 | 0.04 | 0.99 | 0.95, 1.04 | 0.78 | 0.94 | 0.89, 0.98 | 0.008 |
| Harassment at work | 1.72 | 1.34, 2.24 | <0.0001 | 1.21 | 0.93, 1.57 | 0.16 | 1.38 | 1.07, 1.79 | 0.01 |
| Job title | 0.0008 | 0.56 | 0.04 | ||||||
| Nurse vs. Other | 1.67 | 1.23, 2.26 | 1.18 | 0.87, 1.60 | 0.69 | 0.50, 0.93 | |||
| Pt care Assoc. vs. Other | 2.20 | 1.25, 3.88 | 1.15 | 0.66, 2.03 | 0.64 | 0.36, 1.12 | |||
| Job Demands | 1.04 | 1.01, 1.06 | 0.004 | 1.00 | 0.98, 1.03 | 0.98 | 1.01 | 0.99, 1.00 | 0.36 |
| Decision Latitude | 1.00 | 0.98, 1.01 | 0.43 | 0.98 | 0.97, 1.00 | 0.01 | 0.99 | 0.97, 1.00 | 0.15 |
| Organizational context | |||||||||
| Ergonomic Practices | 0.92 | 0.78, 1.08 | 0.30 | 1.13 | 0.96, 1.33 | 0.15 | 0.83 | 0.71, 0.97 | 0.02 |
| People-oriented Culture | 1.12 | 0.90, 1.39 | 0.31 | 0.96 | 0.77, 1.19 | 0.72 | 1.26 | 1.01, 1.56 | 0.04 |
| Individual Characteristics | |||||||||
| Race Ethnicity | 0.46 | 0.0005 | 0.68 | ||||||
| Hispanic vs. Other | 1.13 | 0.51, 2.51 | 0.90 | 0.40, 1.99 | 0.66 | 0.30, 1.48 | |||
| White vs. Other | 1.19 | 0.70, 2.03 | 0.43 | 0.25, 0.73 | 0.73 | 0.42, 1.26 | |||
| Black vs. Other | 0.83 | 0.43, 1.62 | 0.78 | 0.40, 1.51 | 0.70 | 0.36, 1.37 | |||
| Age (10 yr) | 0.89 | 0.80, 0.99 | 0.03 | 1.15 | 1.03, 1.27 | 0.01 | 1.08 | 0.98, 1.21 | 0.13 |
| BMI | 1.00 | 0.98, 1.03 | 0.92 | 1.07 | 1.04, 1.09 | <0.0001 | 1.02 | 0.998, 1.05 | 0.07 |
The results of the final logistic regression models for the three outcomes are presented in Table 6. In multivariable analysis, variables associated with increased risk of LBP included decreased supervisor support, increased harassment at work, being a staff nurse or patient care associate, increased job demands, and younger age. The safety and ergonomic practices scales were no longer significantly associated with LBP when the other characteristics were controlled, nor were use of lifts, hours worked, shift or race/ethnicity. Variables that remained significantly associated with inadequate physical activity included low decision latitude, increased age, increased BMI and “other” race/ethnicity compared to whites. People-oriented culture, coworker support, occupation and education were no longer associated with physical activity when the other factors were controlled. Low supervisor support, harassment at work, and low ergonomic practices were significantly associated with sleep deficiency in multivariable analysis, as was not working as a staff nurse. The relationship between sleep deficiency and people-oriented culture remained statistically significant but the direction was reversed compared to that shown in bivariate analyses. The safety practices scale and coworker support were not significantly associated with sleep deficiency when other variables in the model were controlled.
Discussion
Increasing attention has been given to the multiple risks workers face related to hazards on the job as well as individual health behaviors. A growing literature points to the need for integrated interventions that can effectively coordinate efforts to address multiple outcomes influencing worker health and wellness.54, 65, 66 In the analyses presented here, we examined the relationships among three important wellness outcomes among hospital patient care workers: LBP, inadequate physical activity, and sleep deficiency. We hypothesized that these outcomes would be associated with one another, posing increased risk to health and wellbeing for these workers. We found that sleep deficiency, common among these workers, was significantly associated with inadequate physical activity. Unexpectedly, however, LBP was not associated with either physical activity or sleep deficiency in these cross-sectional data. We also hypothesized that the three outcomes would be associated with common characteristics of the work environment, as illustrated in Figure 1. In multivariable analyses, we found several important themes in the nature of the relationships of these outcomes to job characteristics (i.e., social relations at work, job strain, use of a lifting device, work hours and schedule, and job title) and organizational context (i.e., safety practices, ergonomic practices, a people-oriented culture, and patient care work unit).
Our finding of the relationship between inadequate physical activity and sleep deficiency is consistent with prior reports in the literature.67 Indeed, research has indicated that improved fitness can improve sleep.68 The lack of association of either sleep or physical activity to LBP is contrary to our hypothesis and is in contrast to prior research which has shown a relationship between sedentary behavior and increased risk for MSDs of both the low back and neck. 69 In addition, others have reported that among those already injured, physical inactivity prolongs disability and adds to the risk of further occurrence of musculoskeletal pain.70, 71 Prior research has also found that workers who sustain injuries are less able to be physically active during leisure time. 10, 30, 72–74 These results are also inconsistent with prior studies that have shown that adequate restorative sleep improves long-term pain.75 For patient care workers, working nights and the associated sleep disruptions contribute to increased risk of MSDs and predict a decreased probability of returning to work.76 The discrepancies between prior research and the findings presented here may reflect the cross-sectional nature of our data, the focus on LBP rather than other MSDs, or the specific work experiences of these patient care workers employed in acute care settings. Further research exploring the nature of these relationships, particularly for patient care workers, is warranted.
We found several cross-cutting associations with the work environment among the three outcomes in our multivariable analyses. Harassment on the job and low supervisor support were significantly associated with both LBP and sleep deficiency. The importance of these central indicators of social relationships on the job is of clear relevance to efforts to improve the work environment. Being a staff nurse or patient care associate as compared to other occupations also increased risk of LBP and sleep deficiency. In addition, core indicators of job strain played an important role: Low decision latitude was significantly associated with inadequate physical activity, and high job demands increased the risk of LBP. In addition, poor ergonomic practices were associated with sleep deficiency.
Other studies have underscored importance of experiences at work as important determinants of worker health and wellbeing.77–81 For example, consistent with our findings, in a study of nurses aids, Eriksen, Burrsgaard and Knardahl82 found that LBP was associated not only with ergonomic exposures, but also with working night shift, lack of support from one’s superior, and work culture. Others have also shown the importance of workplace abuse or harassment in workplace injuries and other worker health outcomes. 83, 84 Prior studies have also reported that risk of injury on the job is associated with the pace of work and a sense of time urgency, staffing patterns and resulting workload that may be associated with them, the degree of perceived control over work, and the nature of job tasks, such as the extent to which high physical exertion is a requirement of the job.44–49, 79, 81, 85–89
Similarly, prior research has found that insomnia and poor sleep quality are associated with high job demands, low influence over decisions on the job, and other work-related factors.17, 90, 91 The role of supervisor support has also been demonstrated. For example, supervising managers of healthcare workers who are inflexible about their employee’s work-family conflicts have employees with measured sleep duration about one half hour shorter per night, on average, than employees with more flexible managers.42
We also found that job decision latitude was associated with physical activity. This finding is consistent with prior literature demonstrating that physical activity is positively associated with job control, and inversely related with both job demands and generalized occupational stress.15–17, 51–53, 80, 90–95 Nonetheless, others have reported stronger associations between the work organization and physical activity levels, compared to the findings we reported here. Although we found that in bivariate analyses, inadequate physical activity was additionally associated with lower people-oriented culture and lower coworker support, only the association with decision latitude remained significant in multivariate analyses. The nature of patient care work may indeed involve a different dynamic in these pathways, and further research may help to elucidate these pathways.
Knowledge about the co-occurrence of risks associated with exposures on the job and health behaviors is clearly relevant to understanding the patterns of risks. For example, consistent evidence underscores the pattern of increased risk of both MSDs and risk-related behaviors by socio-economic position, with higher risk among workers in lower status service positions and with lower levels of education.96, 97 In our findings, staff nurses and patient care assistants were at elevated risk for LBP relative to other workers, although these occupational differences did not hold in multivariate analyses for the other two outcomes.
We recognize that in general the magnitudes of the odds ratios we found to be statistically significant may not be seen as “clinically relevant.” Others have observed, however, that small changes in risk at a population level have meaningful public health implications. 98, 99 Indeed, while the associations observed here may have limited implications for the treatment of individual workers, they represent an opportunity for health professionals and others to work with hospital leadership on organizational changes to optimize wellness and wellbeing in the workforce. The combined impact of these work factors suggests in addition that worksite interventions target multiple factors in the work environment for optimal impact.
These findings rely on a cross-sectional survey; as with any cross-sectional assessment, it is not possible to determine the temporal sequence in these relationships, and we therefore do not infer causality. Data were collected from two academic teaching hospitals in the greater Boston area; we acknowledge that findings from this setting may not be generalizable to other patient care settings. Findings reported here are based on self-reports from the survey, and accordingly are subject to recall and social-desirability bias. Additionally, while we controlled for workload by grouping similar units, we recognize that work on patient care units is highly variable and unknown confounders or work characteristics may impact the outcomes. Despite these limitations, it is important to note the high response rate to this survey (79%) and the use of multiple indicators of work experiences.
In conclusion, these findings point to important shared pathways in the work environment that jointly influence multiple wellness outcomes for patient care workers. In particular, low supervisor support and harassment on the job had implications for two of the three outcomes studied here. Efforts to improve the organization of work and social relations at work may contribute to improvements in worker health across multiple dimensions. Interventions intended to independently reduce LBP, sleep deficiency, or inadequate physical activity may benefit from synergy and coordination. These findings underscore the importance of attending to these key domains of social relationships and control over decisions at work as part of these intervention efforts. Simply put, from a public health perspective, focusing on both workplace hazards and worker health behaviors is important because it provides a more complete assessment of the risks workers face, compared to attending to one domain (e.g. physical hazards on the job) to the exclusion of another (e.g.., health behaviors). 100 Understanding the shared influences of the work environment on multiple wellness outcomes has clear implications for interventions. There is increasing recognition that an integrated approach, that attends to workers’ health behaviors as well as the potential for exposures on the job, holds promise for bolstering the impact of interventions. An integrated approach recognizes that the workplace acts as both an accelerator and preventer of chronic disease and as a key determinant of individual health behaviors, through physical, social, organizational and psychosocial mechanisms. 54
References
- 1.National Institute for Occupational Safety and Health. [Accessed October 25, 2010.];NIOSH safety and health topic: Health care workers. www.cdc.gov.niosh/topics/healthcare. www.cdc.gov.niosh/topics/healthcare.
- 2.National Institute for Occupational Safety and Health. [Accessed August 27, 2010.];Health Care Workers. URL: http://www.cdc.gov/niosh/topics/healthcare/
- 3.U.S. Department of Labor BoLS. Occupational Injuries and Illnesses: counts, rates and characteristics. Washington DC: 2006. [Google Scholar]
- 4.Bureau of Labor Statistics. Economic news release: Table 1. Incidence rates of non-fatal occupational injuries and illnesses by selected industries and case types. Washington DC: 2007. Available from: http://ww.bls.gov/news.release/osh.t01.htm. [Google Scholar]
- 5.Lagerstrom M, Hansson T, Hagberg M. Work-related low-back problems in nursing. Scand J Work Environ Health. 1998;24(6):449–464. doi: 10.5271/sjweh.369. [DOI] [PubMed] [Google Scholar]
- 6.Nelson A, Fragala G, Menzel N. Myths and facts about back injuries in nursing. Am J Nurs. 2003;103(2):32–40. 41. doi: 10.1097/00000446-200302000-00021. quiz. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine NRC. Musculoskeletal disorders and the workplaces: Low back and upper extremities. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 8.Videman T, Ojajarvi A, Riihimaki H, Troup JD. Low back pain among nurses: a follow-up beginning at entry to the nursing school. Spine (Phila Pa 1976) 2005;30(20):2334–2341. doi: 10.1097/01.brs.0000182107.14355.ca. [DOI] [PubMed] [Google Scholar]
- 9.Geiger-Brown J, Trinkoff AM, Nielsen K, Lirtmunlikaporn S, Brady B, Vasquez EI. Nurses’ perception of their work environment, health, and well-being: a qualitative perspective. Aaohn J. 2004;52(1):16–22. [PubMed] [Google Scholar]
- 10.Hildebrandt VH, Bongers PM, Dul J, van Dijk FJ, Kemper HC. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. 2000:73507–518. doi: 10.1007/s004200000167. [DOI] [PubMed] [Google Scholar]
- 11.Hartvigsen J, Christensen K. Active lifestyle protects against incident low back pain in seniors: a population-based 2-year prospective study of 1387 Danish twins aged 70–100 years. Spine (Phila Pa 1976) 2007;32(1):76–81. doi: 10.1097/01.brs.0000250292.18121.ce. [DOI] [PubMed] [Google Scholar]
- 12.Stroyer J, Jensen LD. The role of physical fitness as risk indicator of increased low back pain intensity among people working with physically and mentally disabled persons: a 30-month prospective study. Spine (Phila Pa 1976) 2008;33(5):546–554. doi: 10.1097/BRS.0b013e3181657cde. [DOI] [PubMed] [Google Scholar]
- 13.Canivet C, Ostergren PO, Choi B, Nilsson P, af Sillen U, Moghadassi M, Karasek R, Isacsson SO. Sleeping problems as a risk factor for subsequent musculoskeletal pain and the role of job strain: results from a one-year follow-up of the Malmo Shoulder Neck Study Cohort. Int J Behav Med. 2008;15(4):254–262. doi: 10.1080/10705500802365466. [DOI] [PubMed] [Google Scholar]
- 14.Jones EA, McBeth J, Nicholl B, Morriss RK, Dickens C, Jones GT, Macfarlane GJ. What characterizes persons who do not report musculoskeletal pain? Results from a 4-year Population-based longitudinal study (the Epifund study) J Rheumatol. 2009;36(5):1071–1077. doi: 10.3899/jrheum.080541. [DOI] [PubMed] [Google Scholar]
- 15.Jones F, O’Connor DB, Conner M, McMillan B, Ferguson E. Impact of daily mood, work hours, and iso-strain variables on self-reported health behaviors. J Appl Psychol. 2007;92(6):1731–1740. doi: 10.1037/0021-9010.92.6.1731. [DOI] [PubMed] [Google Scholar]
- 16.Caruso C, Hitchcock E, Dick R, Russo J, Schmitt J. Overtime and extended work shifts: recent findings on illnesses injuries, and health behaviors. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH); Apr, 2004. http://www.cdc.gov/niosh/docs/2004-143/default.html. Publication No. 2004–143. [Google Scholar]
- 17.Trinkoff AM, Storr CL, Lipscomb JA. Physically demanding work and inadequate sleep, pain medication use, and absenteeism in registered nurses. J Occup Environ Med. 2001;43(4):355–363. doi: 10.1097/00043764-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Hellsing AL, Bryngelsson IL. Predictors of musculoskeletal pain in men: A twenty-year follow-up from examination at enlistment. Spine. 2000:253080–3086. doi: 10.1097/00007632-200012010-00016. [DOI] [PubMed] [Google Scholar]
- 19.Oleske DM, Neelakantan J, Andersson GB, Hinrichs BG, Lavender SA, Morrissey MJ, Zold-Kilbourn P, Taylor E. Factors affecting recovery from work-related, low back disorders in autoworkers. Archives of Physical Medicine and Rehabilitation. 2004:851362–1364. doi: 10.1016/j.apmr.2003.11.021. [DOI] [PubMed] [Google Scholar]
- 20.Snook SH. Self-care guidelines for the management of nonspecific low back pain. Journal of Occupational Rehabilitation. 2004;14(4):243–253. doi: 10.1023/b:joor.0000047427.21710.07. [DOI] [PubMed] [Google Scholar]
- 21.Blair SN, Kampert JB, Kohl HW, 3rd, Barlow CE, Macera CA, Paffenbarger RS, Jr, Gibbons LW. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. Jama. 1996;276(3):205–210. [PubMed] [Google Scholar]
- 22.Holtermann A, Mortensen OS, Burr H, Sogaard K, Gyntelberg F, Suadicani P. Physical demands at work, physical fitness, and 30-year ischaemic heart disease and all-cause mortality in the Copenhagen Male Study. Scand J Work Environ Health. 2010;36(5):357–365. doi: 10.5271/sjweh.2913. [DOI] [PubMed] [Google Scholar]
- 23.Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, Owen N. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise too much sitting: inactivity physiology and the need for new recommendations on sedentary behaviour. Curr Cardiovascular Risk Reports. 2008:2292–298. doi: 10.1007/s12170-008-0054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunstan DW, Barr EL, Healy GN, Salmon J, Shaw JE, Balkau B, Magliano DJ, Cameron AJ, Zimmet PZ, Owen N. Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Circulation. 2010;121(3):384–391. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 26.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 27.Healthy people 2010 U.S. Department of Health and Human Services. [Accessed October 25, 2010.];Focus area 7: educational and community-based programs - worksite setting. http://www.healthypeople.gov/document/HTML/Volume1/07Ed.htm#_Toc490550857.
- 28.Carlson SA, Fulton JE, Galuska DA, Kruger J, Lobelo F, Loustalot FV Centers for Disease Control and Prevention (CDC) Prevalence of Self-Reported Physically Active Adults - United States, 2007. MMWR. 2008;57:1297–1300. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5748a1.htm. [PubMed] [Google Scholar]
- 29.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 30.Airhihenbuwa CO, Kumanyika SK, Agurs-Collins TD, Lowe A. Perceptions and beliefs about excerise, rest and health among African-Americans. Am J Health Promot. 1995;9(6):426–429. doi: 10.4278/0890-1171-9.6.426. [DOI] [PubMed] [Google Scholar]
- 31.Pronk NP, Martinson B, Kessler RC, Beck AL, Simon GE, Wang P. The association between work performance and physical activity, cardiorespiratory fitness, and obesity. J Occup Environ Med. 2004;46(1):19–25. doi: 10.1097/01.jom.0000105910.69449.b7. [DOI] [PubMed] [Google Scholar]
- 32.Anderson DR, Whitmer RW, Goetzel RZ, Ozminkowski RJ, Dunn RL, Wasserman J, Serxner S Health Enhancement Research Organization (HERO) Research Committee. The relationship between modifiable health risks and group-level health care expenditures. American Journal of Health Promotion. 2000;15(1):45–52. doi: 10.4278/0890-1171-15.1.45. [DOI] [PubMed] [Google Scholar]
- 33.Wang F, McDonald T, Champagne LJ, Edington DW. Relationship of body mass index and physical activity to health care costs among employees. J Occup Environ Med. 2004;46(5):428–436. doi: 10.1097/01.jom.0000126022.25149.bf. [DOI] [PubMed] [Google Scholar]
- 34.Burton WN, McCalister KT, Chen CY, Edington DW. The association of health status, worksite fitness center participation, and two measures of productivity. J Occup Environ Med. 2005;47(4):343–351. doi: 10.1097/01.jom.0000158719.57957.c6. [DOI] [PubMed] [Google Scholar]
- 35.Luckhaupt SE, Tak S, Calvert GM. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. Sleep. 2010;33(2):149–159. doi: 10.1093/sleep/33.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi SW, Peek-Asa C, Sprince NL, Rautiainen RH, Flamme GA, Whitten PS, Zwerling C. Sleep quantity and quality as a predictor of injuries in a rural population. Am J Emerg Med. 2006;24(2):189–196. doi: 10.1016/j.ajem.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 37.Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, Czeisler CA Harvard work hours health and safety group. Extended work shifts and the risk of motor vehicle crashes among interns. New England Journal of Medicine. 2005;352(2):125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 38.Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, Czeisler CA. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3(12):e487. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, Speizer FE, Czeisler CA. Extended work duration and the risk of self-reported percutaneous injuries in interns. Jama. 2006;296(9):1055–1062. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- 40.Ruger M, Scheer FA. Effects of circadian disruption on the cardiometabolic system. Rev Endocr Metab Disord. 2009;10(4):245–260. doi: 10.1007/s11154-009-9122-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Czeisler C, Buxton O. The Human Circadian Timing System and Sleep-Wake Regulation. In: Kryger M, Roth T, Dement WC, editors. Principles and Practices of Sleep Medicine. 5. Amsterdam: Elsevier; 2010. pp. 402–419. [Google Scholar]
- 42.Berkman LF, Buxton O, Ertel K, Okechukwu C. Managers’ practices related to work-family balance predict employee cardiovascular risk and sleep duration in extended care settings. J Occup Health Psychol. 2010;15(3):316–329. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ertel KA, Berkman LF, Buxton OM. Socioeconomic Status, Occupational Characteristics, and Sleep Duration in African/Caribbean Immigrants and US White Health Care Workers. Sleep. doi: 10.1093/sleep/34.4.509. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lipscomb JA, Trinkoff AM, Geiger-Brown J, Brady B. Work-schedule characteristics and reported musculoskeletal disorders of registered nurses. Scand J Work Environ Health. 2002;28(6):394–401. doi: 10.5271/sjweh.691. [DOI] [PubMed] [Google Scholar]
- 45.Trinkoff AM, Lipscomb JA, Geiger-Brown J, Storr CL, Brady BA. Perceived physical demands and reported musculoskeletal problems in registered nurses. Am J Prev Med. 2003;24(3):270–275. doi: 10.1016/s0749-3797(02)00639-6. [DOI] [PubMed] [Google Scholar]
- 46.Wasiak R, Verma S, Pransky G, Webster B. Risk factors for recurrent episodes of care and work disability: case of low back pain. J Occup Environ Med. 2004;46(1):68–76. doi: 10.1097/01.jom.0000105987.32375.3d. [DOI] [PubMed] [Google Scholar]
- 47.Muchmore L, Lynch WD, Gardner HH, Williamson T, Burke T. Prevalence of arthritis and associated joint disorders in an employed population and the associated healthcare, sick leave, disability, and workers’ compensation benefits cost and productivity loss of employers. J Occup Environ Med. 2003;45(4):369–378. doi: 10.1097/01.jom.0000063621.37065.26. [DOI] [PubMed] [Google Scholar]
- 48.Yassi A, Gilbert M, Cvitkovich Y. Trends in injuries, illnesses, and policies in Canadian healthcare workplaces. Can J Public Health. 2005;96(5):333–339. doi: 10.1007/BF03404026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Amick BC, Habeck RV, Hunt A, Fossel AH, Chapin A, Keller RB, Katz JN. Measuring the impact of organizational behaviors on work disability prevention and management. J Occup Rehabil. 2000;10(1):21–38. [Google Scholar]
- 50.Nakata A, Haratani T, Takahashi M, Kawakami N, Arito H, Kobayashi F, Araki S. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Soc Sci Med. 2004;59(8):1719–1730. doi: 10.1016/j.socscimed.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 51.Choi B, Schnall PL, Yang H, Dobson M, Landsbergis P, Israel L, Karasek R, Baker D. Psychosocial working conditions and active leisure-time physical activity in middle-aged us workers. Int J Occup Med Environ Health. :20101–15. doi: 10.2478/v10001-010-0029-0. [DOI] [PubMed] [Google Scholar]
- 52.Hansen AM, Blangsted AK, Hansen EA, Sogaard K, Sjogaard G. Physical activity, job demand-control, perceived stress-energy, and salivary cortisol in white-collar workers. Int Arch Occup Environ Health. 2010;83(2):143–153. doi: 10.1007/s00420-009-0440-7. [DOI] [PubMed] [Google Scholar]
- 53.Kouvonen A, Kivimaki M, Elovainio M, Virtanen M, Linna A, Vahtera J. Job strain and leisure-time physical activity in female and male public sector employees. Preventive Medicine. 2005;41(2):532–539. doi: 10.1016/j.ypmed.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Sorensen G, Landsbergis P, Hammer L, Amick B, Linnan L, Yancey A, Welch L, Goetzel R, Flannery K, Pratt C. Preventing Chronic Disease At the Workplace: A Workshop Report and Recommendations. Am J Public Health. doi: 10.2105/AJPH.2010.300075. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, Jorgensen K. Standardized Nordic Questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics. 1987:18233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 56.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta: Georgia; 2009. [Google Scholar]
- 57.Buysse D, Reynolds C, Monk T, Berman S, Kupfer D. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1998:28193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 58.Buxton OM, Quintiliani LM, Yang MH, Ebbeling CB, Stoddard AM, Pereira LK, Sorensen G. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. Am J Public Health. 2009;99(Suppl):3S636–643. doi: 10.2105/AJPH.2008.158501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Karasek R, Theorell T. Healthy work: Stress, productivity, and the reconstruction of working life. New York, NY: Basic Books; 1990. [Google Scholar]
- 60.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 61.Krieger N, Waterman PD, Hartman C, Bates LM, Stoddard AM, Quinn MM, Sorensen G, Barbeau EM. Social hazards on the job: workplace abuse, sexual harassment, and racial discrimination--a study of Black, Latino, and White low-income women and men workers in the United States. Int J Health Serv. 2006;36(1):51–85. doi: 10.2190/3EMB-YKRH-EDJ2-0H19. [DOI] [PubMed] [Google Scholar]
- 62.Schwartz JE, Pieper CF, Karasek RA. A procedure for linking psychosocial job characteristics data to health surveys. American Journal of Public Health. 1988:78904–909. doi: 10.2105/ajph.78.8.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amick BC, Habeck RV, Hunt A, Fossel AH, Chapin A, Keller RB, Katz JN. Measuring the impact of organizational behaviors on work disability prevention and management. Journal of Occupational Rehabilitation. 2000;10(1):21–38. [Google Scholar]
- 64.SAS Institute Inc. The SAS system for Windows, release 9.2. Cary, NC: 2009. [Google Scholar]
- 65.Institute of Medicine, Committee to Assess Worksite Preventive Health Program Needs for NASA Employees, Food and Nutrition Board. Integrating employee health: A model program for NASA. Washington, DC: Institute of Medicine, National Academies Press; 2005. [Google Scholar]
- 66.National Institute for Occupational Safety and Health. [Accessed March 6, 2008];NIOSH WorkLife Initiative. 2008 Feb 1; http://www.cdc.gov/niosh/worklife/
- 67.Chaput JP, Klingenberg L, Sjodin A. Do all sedentary activities lead to weight gain: sleep does not. Curr Opin Clin Nutr Metab Care. 2010;13(6):601–607. doi: 10.1097/MCO.0b013e32833ef30e. [DOI] [PubMed] [Google Scholar]
- 68.Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010;11(9):934–940. doi: 10.1016/j.sleep.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Johansson G, Johnson JV, Hall EM. Smoking and sedentary behavior as related to work organization. Soc Sci Med. 1991;32(7):837–846. doi: 10.1016/0277-9536(91)90310-9. [DOI] [PubMed] [Google Scholar]
- 70.Iwasaki Y, Zuzanek J, Mannell RC. The effects of physically active leisure on stress-health relationships. Can J Public Health. 2001;92(3):214–218. doi: 10.1007/BF03404309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu B, Porell F. Job characteristics and leisure physical activity. J Aging Health. 2000;12(4):538–559. doi: 10.1177/089826430001200405. [DOI] [PubMed] [Google Scholar]
- 72.Ratzlaff CR, Gillies JH, Koehoorn MW. Work-related repetitive strain injury and leisure-time physical activity. Arthritis Rheum. 2007;57(3):495–500. doi: 10.1002/art.22610. [DOI] [PubMed] [Google Scholar]
- 73.Bernaards CM, Ariens GA, Hildebrandt VH. The (cost-)effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on the recovery from neck and upper limb symptoms in computer workers. BMC Musculoskelet Disord. 2006:780. doi: 10.1186/1471-2474-7-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lemoyne J, Laurencelle L, Lirette M, Trudeau F. Occupational health problems and injuries among Quebec’s physical educators. Appl Ergon. 2007;38(5):625–634. doi: 10.1016/j.apergo.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 75.Davies KA, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, McBeth J. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology (Oxford) 2008;47(12):1809–1813. doi: 10.1093/rheumatology/ken389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Salo P, Oksanen T, Sivertsen B, Hall M, Pentti J, Virtanen M, Vahtera J, Kivimaki M. Sleep disturbances as a predictor of cause-specific work disability and delayed return to work. Sleep. 2010;33(10):1323–1331. doi: 10.1093/sleep/33.10.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bauman A, Ma G, Cuevas F, Omar Z, Waqanivalu T, Phongsavan P, Keke K, Bhushan A. Cross-national comparisons of socioeconomic differences in the prevalence of leisure-time and occupational physical activity, and active commuting in six Asia-Pacific countries. J Epidemiol Community Health. 2011;65(1):35–43. doi: 10.1136/jech.2008.086710. [DOI] [PubMed] [Google Scholar]
- 78.Alperovitch-Najenson D, Santo Y, Masharawi Y, Katz-Leurer M, Ushvaev D, Kalichman L. Low back pain among professional bus drivers: ergonomic and occupational-psychosocial risk factors. Isr Med Assoc J. 2010;12(1):26–31. [PubMed] [Google Scholar]
- 79.Yip VY. New low back pain in nurses: Work activities, work stress and sedentary lifestyle. Journal of Advanced Nursing. 2004:46430–440. doi: 10.1111/j.1365-2648.2004.03009.x. [DOI] [PubMed] [Google Scholar]
- 80.Harma M, Ilmarinen J, Knauth P. Physical fitness and other individual factors relating to the shiftwork tolerance of women. Chronobiol Int. 1988;5(4):417–424. doi: 10.3109/07420528809067787. [DOI] [PubMed] [Google Scholar]
- 81.Feng CK, Chen ML, Mao IF. Prevalence of and risk factors for different measures of low back pain among female nursing aides in Taiwanese nursing homes. BMC Musculoskelet Disord. 2007:852. doi: 10.1186/1471-2474-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Eriksen W. Work factors and smoking cessation in nurses’ aides: a prospective cohort study. BMC Public Health. 2005:5142. doi: 10.1186/1471-2458-5-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hoobler JM, Rospenda KM, Lemmon G, Rosa JA. A within-subject longitudinal study of the effects of positive job experiences and generalized workplace harassment on well-being. J Occup Health Psychol. 2010;15(4):434–451. doi: 10.1037/a0021000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brown LP, Rospenda KM, Sokas RK, Conroy L, Freels S, Swanson NG. Evaluating the association of workplace psychosocial stressors with occupational injury, illness, and assault. J Occup Environ Hyg. 2011;8(1):31–37. doi: 10.1080/15459624.2011.537985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Marras WS, Cutlip RG, Burt SE, Waters TR. National occupational research agenda (NORA) future directions in occupational musculoskeletal disorder health research. Appl Ergon. 2009;40(1):15–22. doi: 10.1016/j.apergo.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 86.Lipscomb J, Trinkoff A, Brady B, Geiger-Brown J. Health care system changes and reported musculoskeletal disorders among registered nurses. Am J Public Health. 2004;94(8):1431–1435. doi: 10.2105/ajph.94.8.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tullar JM, Brewer S, Amick BC, 3rd, Irvin E, Mahood Q, Pompeii LA, Wang A, Van Eerd D, Gimeno D, Evanoff B. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J Occup Rehabil. 2010;20(2):199–219. doi: 10.1007/s10926-010-9231-y. [DOI] [PubMed] [Google Scholar]
- 88.Waters T, Collins J, Galinsky T, Caruso C. NIOSH research efforts to prevent musculoskeletal disorders in the healthcare industry. Orthop Nurs. 2006;25(6):380–389. doi: 10.1097/00006416-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 89.Dawson AP, McLennan SN, Schiller SD, Jull GA, Hodges PW, Stewart S. Interventions to prevent back pain and back injury in nurses: a systematic review. Occup Environ Med. 2007;64(10):642–650. doi: 10.1136/oem.2006.030643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jansson-Frojmark M, Lundqvist D, Lundqvist N, Linton SJ. Psychosocial work stressors for insomnia: a prospective study on 50–60-year-old adults in the working population. Int J Behav Med. 2007;14(4):222–228. doi: 10.1007/BF03002996. [DOI] [PubMed] [Google Scholar]
- 91.Nishitani N, Sakakibara H. Job stress factors, stress response, and social support in association with insomnia of Japanese male workers. Ind Health. 2010;48(2):178–184. doi: 10.2486/indhealth.48.178. [DOI] [PubMed] [Google Scholar]
- 92.Kouvonen A, Kivimaki M, Vaananen A, Heponiemi T, Elovainio M, Ala-Mursula L, Virtanen M, Pentti J, Linna A, Vahtera J. Job strain and adverse health behaviors: the Finnish Public Sector Study. J Occup Environ Med. 2007;49(1):68–74. doi: 10.1097/JOM.0b013e31802db54a. [DOI] [PubMed] [Google Scholar]
- 93.Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32(6):473–481. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- 94.Hannerz H, Albertsen K, Nielsen ML, Tuchsen F, Burr H. Occupational factors and 5-year weight change among men in a danish national cohort. Health Psychol. 2004;23(3):283–288. doi: 10.1037/0278-6133.23.3.283. [DOI] [PubMed] [Google Scholar]
- 95.Aasa U, Brulin C, Angquist KA, Barnekow-Bergkvist M. Work-related psychosocial factors, worry about work conditions and health complaints among female and male ambulance personnel. Scand J Caring Sci. 2005;19(3):251–258. doi: 10.1111/j.1471-6712.2005.00333.x. [DOI] [PubMed] [Google Scholar]
- 96.National Center for Health Statistics; National Center for Health Statistics, editor. Health, United States 2003, with chartbook on trends in the health of Americans. Hyattsville, MD: National Center for Health Statistics; 2003. Table 150. Persons enrolled in health maintenance organizations (HMOs) by geographic region and state: United States, selected years 1980–2002. [Google Scholar]
- 97.National Statistics (UK) [Accessed August 29, 2004, 2004.];The National Statistics Socio-Economic Classification (NS-SEC): Introduction. 2004 Aug 9; http://www.statistics.gov.uk/methods_quality/ns_sec/default.asp.
- 98.Rose G. The strategy of preventive medicine. New York, N.Y: Oxford University Press; 1992. [Google Scholar]
- 99.Tosteson AN, Weinstein MC, Hunink MG, Mittleman MA, Williams LW, Goldman PA, Goldman L. Cost-effectiveness of populationwide educational approaches to reduce serum cholesterol levels. Circulation. 1997;95(1):24–30. doi: 10.1161/01.cir.95.1.24. [DOI] [PubMed] [Google Scholar]
- 100.Krieger N, Kaddour A, Koenen K, Kosheleva A, Chen JT, Waterman PD, Barbeau EM. Occupational, social, and relationship hazards and psychological distress among low-income workers: implications of the ‘inverse hazard law’. J Epidemiol Community Health. 2010;65(3):260–272. doi: 10.1136/jech.2009.087387. [DOI] [PubMed] [Google Scholar]