Abstract
Many nations are struggling with the design, implementation, and ongoing improvement of health care systems to meet the needs of their citizens. In the United Arab Emirates, a small nation with vast wealth, the lives of average citizens have evolved from a harsh, nomadic existence to enjoyment of the comforts of modern life. Substantial progress has been made in the provision of education, housing, health, employment, and other forms of social advancement. Having covered these basic needs, the government of Abu Dhabi, United Arab Emirates, is responding to the challenge of developing a comprehensive health system to serve the needs of its citizens, including restructuring the nation's graduate medical education (GME) system. We describe how Abu Dhabi is establishing GME policies and infrastructure to develop and support a comprehensive health care system, while also being responsive to population health needs. We review recent progress in developing a systematic approach for developing GME infrastructure in this small emirate, and discuss how the process of designing a GME system to meet the needs of Emirati citizens has benefited from the experience of “Western” nations. We also examine the challenges we encountered in this process and the solutions adopted, adapted, or specifically developed to meet local needs. We conclude by highlighting how our experience “at the GME drawing board” reflects the challenges encountered by scholars, administrators, and policymakers in nations around the world as they seek to coordinate health care and GME resources to ensure care for populations.
“The best investment of our wealth is in creating cultured and educated citizens. We have to be swift and make our progress in education faster than our progress in any other field.”
—the late Sheikh Zayed
Introduction
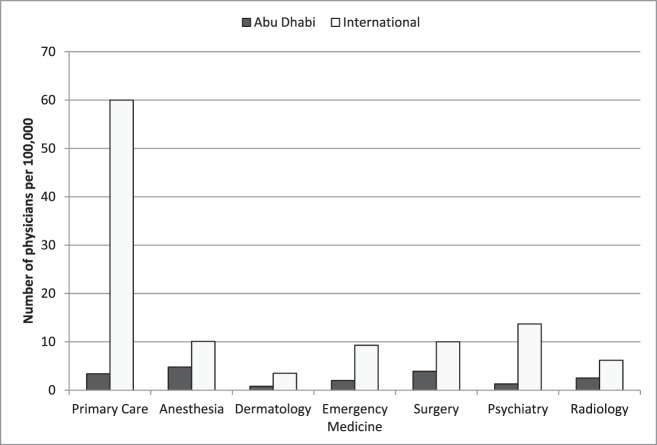
The United Arab Emirates (UAE) is a small nation with vast wealth, which has achieved impressive advances and is setting regional and international benchmarks in development, including multiple man-made island communities, the tallest building in the world, and plans to be the world's only city powered entirely by renewable energy. Concurrently, the lives of average Emirati citizens have advanced from a harsh, nomadic desert existence to enjoying the comforts and necessities of modern life.1 This rapid progress is made possible through generous government subsidies in the provision of education, housing, health, employment, and other forms of social advancement. Having covered these population needs, the government of Abu Dhabi, responsible for the largest emirate of the UAE, which also serves as the nation's capital, is poised to take on the challenge of developing a comprehensive health care system. One of the most challenging health system factors to be addressed is the marked insufficiency of the physician supply, which places Abu Dhabi behind other developed nations (figure 1).2
FIGURE 1.
Number of Specialty Physicians per 100 000 Population for Abu Dhabi Compared to International Examples16–19
Source: Abu Dhabi Data: Department of Health Professional Licensing, HAAD 2010; International Data: United States and Australia.16–19
Background
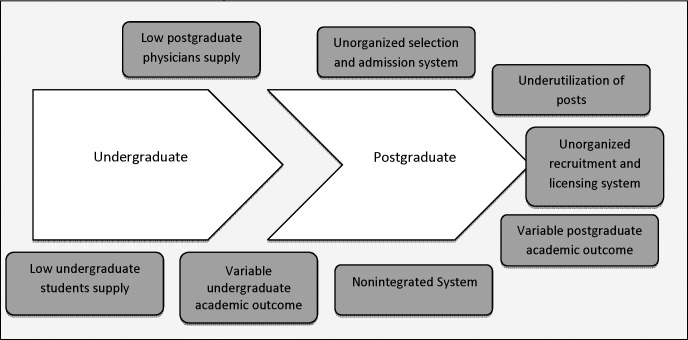
Although just over 40 years old as a nation, the UAE has conducted graduate medical education (GME) programs since the mid 1990s, with accreditation and certification provided by the Arab Board of Health Specializations (Arab Board).3,4 Despite the regulatory framework provided by this reputable board, variations in program-level implementation of standards resulted in programs that lacked a defined structure, clear outcomes, and adequate ongoing oversight within sponsoring institutions. The introduction of Western-trained hospital administrators from academic institutions in the United States and the United Kingdom has resulted in rapid advancements in clinical services, yet improvements in the residency programs have lagged behind. At every stage of the emirate's medical education trajectory, problems contributed to a host of workforce deficiencies shown in figure 2. GME quality remained subpar, with poor board certification rates for UAE graduates.
FIGURE 2.
Aspects of the Educational System that Contribute to Observed Workforce Deficiencies
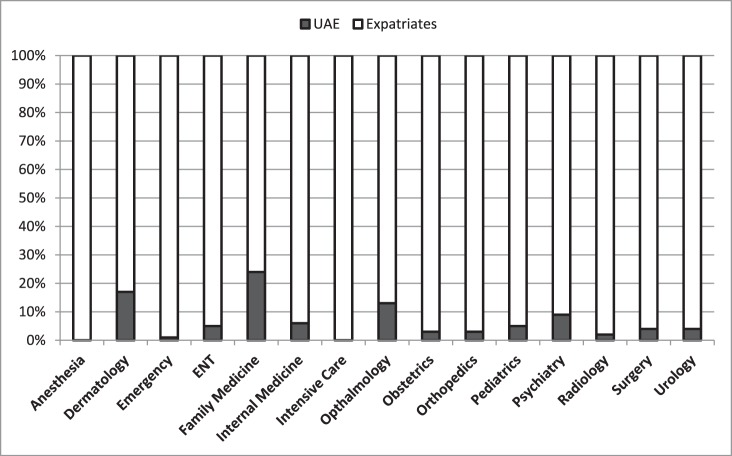
To provide Emirati physicians with improved training opportunities, Abu Dhabi traditionally has relied on funding graduates to complete residency and/or fellowship training in the Western educational systems. Several cohorts of graduates who trained abroad have returned, and now work in the emirate's health care sector. Additionally, expatriate physicians, trained outside the UAE, have been a major driver in shaping the quality of the emirate's health care. An influx of Western-trained physicians has resulted in expatriates comprising more than 93% of medical professionals in Abu Dhabi (figure 3).1 The combination of an ample supply of potential educators already present in the system, the shrinking number of available training positions for international medical graduates in Western nations, and the potential instability that could result from a reliance on a highly migratory expatriate medical workforce triggered a paradigm shift in Abu Dhabi's health system policy, moving it toward development of a sustainable, grassroots GME strategy aimed at improving both numbers and the quality of Emirati-trained physicians.
FIGURE 3.
Percentage Distribution of United Arab Emirates (UAE) and Expatriate Physicians Practicing in the Emirate of Abu Dhabi, 2012
Abbreviation: ENT, ear, nose, and throat (Otolaryngology). Source: Department of Health Professional Licensing, Health Authority Abu Dhabi.
Western Lessons: Eastern Solutions
The first step entailed establishing an office of postgraduate medical education in the Health Authority Abu Dhabi (HAAD), the emirate's sole regulatory body for the health care industry. Our charge included the creation of a regulatory framework to ensure the provision of high-quality GME responsive to the needs of our local health care system. To develop Abu Dhabi's GME strategy we drew on our backgrounds as an American general internist and an Emirati pulmonologist trained in the United States and Canada. When we compared our own training abroad with the “on-the-ground” experiences in Abu Dhabi residency programs, it became obvious that reconciling the 2 systems would require a rethinking of GME. With financial support, buy-in from stakeholders, and considerable regulatory authority, we began the process of redesigning the GME system for our emirate.
Given our mandate and the existence of a single regulatory body for health care, we found ourselves in an advantageous position, compared to many of our Western counterparts who must navigate a more fragmented regulatory framework. Despite this difference, we thought it important to review the GME road map chartered by our Western colleagues. The question was: How could Abu Dhabi learn from these experiences while adapting our approach to Emirati culture and the needs of our citizens?
Lesson 1: GME and Workforce Strategy
For our small nation, the importance of linking strategic needs and medical workforce composition is critical. The US GME experience has demonstrated the perils of market-based, largely unregulated residency selection, with many US graduates choosing to subspecialize despite serious shortages in primary care physicians.4,5 This lack of alignment between national health care needs and health care workforce production has long been recognized as a major threat to optimizing health services for US citizens.6,7 The disadvantages of this lack of alignment also were highlighted in the June 2010 Medicare Payment Advisory Commission report, which emphasized the need for regulatory oversight or effective incentive systems to promote the production of primary care physicians.8 In addition, the passage of President Obama's Affordable Care Act prompted the commissioning of a National Health Care Workforce Committee to examine this issue.9 Taking advantage of its relatively small size and central authority, Abu Dhabi was able to conduct a strategic review of its health care system resources with input from major educational and health sector stakeholders. As a result of these efforts, the emirate has developed a set of strategies to create a workforce to care for its citizens (box).
Box Strategies to Enhance the Health Care Workforce for Abu Dhabi
TANSEEQ (emirate-wide residency post determination and matching process)
Central database of graduate medical education (GME) infrastructure (residency programs, hospitals, and key academic administrators)
Funding GME positions according to health care need and educational quality
Increase the attractiveness of health professions as a career choice through payment strategies and provision of internationally accredited training
Identify reasons for leaving the healthcare sector and/or Abu Dhabi and develop retention policies with specific targets for increasing Emirati citizen representation in the healthcare workforce
Training and support of health professionals in critically needed specialties
Identify delivery models (eg, use of physician extenders) to reduce dependency on expensive/rare specialists and consultants
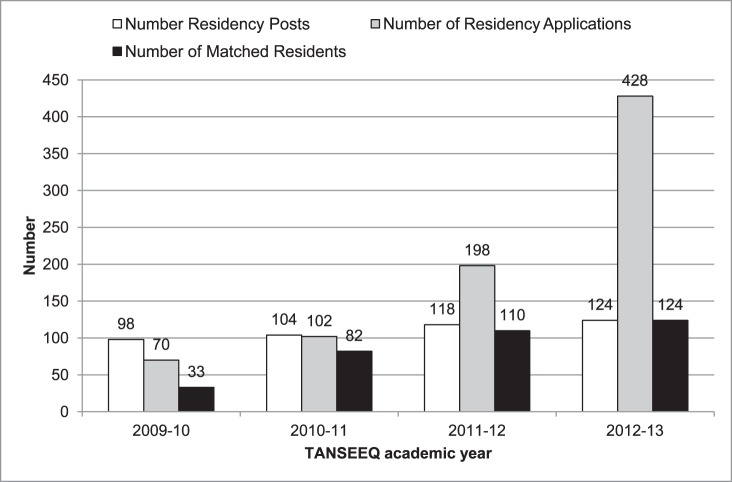
GME is a key vector to ensure an adequate supply of physicians for the emirate. An important component of Abu Dhabi's new approach is the “TANSEEQ” program. Implemented in 2010, TANSEEQ is the first emirate-wide residency post determination and match process initiated by the HAAD.10 It also represents the first “international” match done on a contract basis by the National Residency Matching Program (NRMP). In the United States, the NRMP executes the residency match without involvement in the specialty allocation of available positions (positions are entered in the match without any central determination of the number and specialty distribution). In contrast, the TANSEEQ program not only matches residency positions with eligible medical graduates, but also allows HAAD (in partnership with local educational stakeholders) to establish the number and specialty of residency posts across all teaching facilities in Abu Dhabi. Allocation is based on community disease burden and an in-depth analysis and prioritization of shortages in the current workforce. By determining the strategic utility of positions to the health of its citizens, the HAAD plans to develop a physician workforce that is aligned with population needs. Although developments toward this grassroots policy are essential, we also recognize that Abu Dhabi will likely continue its reliance on Western nations for specific “low volume/high expertise” subspecialties to foster the development of a subspecialty workforce.
To date, the TANSEEQ program has produced a significant increase in the fill rate for residency positions, from an average of only 34% (in the 5 years before TANSEEQ) to 100% of all residency positions being occupied at the conclusion of the 2012 TANSEEQ cycle (figure 4). Another principle achievement of TANSEEQ was the development of a central database of all existing residency education programs, hospitals, and key academic administrators, representing valuable GME infrastructure data that were previously unknown. Lastly, previously “hidden” GME silos operating in their respective hospitals throughout Abu Dhabi were acknowledged and recognized. This enabling effect of TANSEEQ has now spawned a robust network of lead academicians, administrators, and clinicians—a GME workforce of immeasurable value for Abu Dhabi.
FIGURE 4.
Number of Accredited Positions, Number of Applications, and Number of Match Residents, Compared to Prior Years and After Implementation of TANSEEQ
Source: Department of Health Professional Licensing, Health Authority Abu Dhabi, United Arab Emirates.
Lesson 2: Funding GME
In the United States, few other topics elicit more dread and controversy in the educational community than GME funding. Although there is ongoing debate around the source and distribution of funding, the United States and several Western nations provide facilities engaged in medical education with a stream of funding dedicated to postgraduate physician training. Owing to the wealth of the emirate and its relatively small population, many of the fiscal pressures faced by Western nations are not as prominent in the Abu Dhabi GME funding model. Whereas many systems in the West struggle with quantifying the costs of the intangible product of “resident education,”11 in Abu Dhabi the focus is on ensuring the highest quality of the physician education programs. In fact, the emirate has taken the approach of dedicating government funds for positions with strategic relevance and based on educational outcomes achieved, in contrast to payment models that reimburse for the health services provided by individuals in training. A HAAD task force is engaged in determining the educational outcomes most relevant to this funding policy.
Lesson 3: Measurement of Educational Outcomes
Increasingly, Western nations have shifted their educational models from structure, process, and time-based models to an approach based on educational outcomes.12–14 The traditional “tea-steeping” model of medical education,15 which measured progress solely by time spent in the educational program, is being reexamined. Curricula and assessment methods are undergoing revisions to ensure the identification of distinct, specialty-based competencies that signify key dimensions of physicians' performance.14
The Arab Board accreditation criteria used by Abu Dhabi are less stringent than those used in Western accreditation systems. This is in part due to the Arab Board's need to create unifying criteria for countries in North Africa and the Middle East, which possess vastly different health care systems. Abu Dhabi's GME system is now prepared to adopt rigorous standards to match its rapidly progressing health sector. It is with this goal in mind that our office at the HAAD spearheaded the first memorandum of understanding between the Accreditation Council for Graduate Medical Education–International (ACGME-I) and Abu Dhabi. As of 2012, most Abu Dhabi residency-sponsoring institutions have attained ACGME-I accreditation. Residency programs in Abu Dhabi are poised to apply for ACGME-I accreditation, which demonstrates the monumental shift toward outcomes-based education. The next step entails identifying and measuring macrolevel GME performance indicators to allow tracking and rewarding programs for performance, such as through funding.
Lesson 4: Quality Assurance Through GME
The quality of any nation's health care system depends on the quality of its health professional workforce. In the United States, state licensure requirements specify that all international medical graduates must undergo some GME training in the United States. This provides for a regulatory quality assurance check to ensure common clinical practice expectations and outcomes across practitioners with diverse prior medical training. In Abu Dhabi, a reliance on expatriate populations with differing educational standards and backgrounds to provide health services is of concern when the quality and sustainability of services are considered. While “emiratization” mandates are in place in virtually every industry to foster the recruitment and advancement of Emiratis in the workforce, in the health care sector, the investment in the education of citizens is vital to achieving a sufficient degree of quality and standardization in the health services delivered.
In 2010, expatriate medical graduates in Abu Dhabi were accepted into residency training positions by participating in the TANSEEQ residency match. These expatriate medical graduates previously were without the option to pursue GME training and thus remained “general practitioners” throughout their careers. While following emiratization mandates, these expatriate physicians-in-training were distributed to critically needed specialties, with their education fully sponsored by the government of Abu Dhabi. This strategy recognizes the advantage of advancing the quality of health services provided by this previously “educationally stagnant” group of physicians.
Finding Commonality
We believe the lessons described have served to advance health care and GME policy in Abu Dhabi. Perhaps the most valuable concept we have learned from our experience is the value of seeking commonality in challenges encountered by educators, scholars, academicians, and administrators around the world. These may be overlooked as a result of social, economic, and political differences. We plan to share our experiences as we move forward in our transformational GME journey.
Footnotes
Sawsan Abdel-Razig, MD, FACP, is Senior Post Graduate Education Officer, Health Authority Abu Dhabi, and Adjunct Assistant Professor of Medicine, Department of Medicine, United Arab Emirates University, United Arab Emirates; and Hatem Alameri, MD, FRCPC, FCCP, is Manager, Health Professional Licensing, Health Authority Abu Dhabi, and Adjunct Associate Professor of Medicine, Department of Medicine, Faculty of Medicine and Health Sciences, United Arab Emirates University, United Arab Emirates.
Funding: The authors report no external funding source for this study.
References
- 1.Human Development Report of the Emirate of Abu Dhabi 2011/2012. http://www.ameinfo.com/human-development-report-emirate-abu-dhabi-314587. Accessed January 8, 2012. [Google Scholar]
- 2.Health Authority Annual Report 2010. Abu Dhabi: 2011. [Google Scholar]
- 3.Abyad A, Al-Baho AK, Unluoglu I, Tarawneh M, Al Hilfy TK. Development of family medicine in the middle East. Fam Med. 2007;39(10):736–741. [PubMed] [Google Scholar]
- 4.Abou-Saleh M. The graduate exodus. Med Educ. 1995;29(1 suppl):92–94. doi: 10.1111/j.1365-2923.1995.tb02902.x. [DOI] [PubMed] [Google Scholar]
- 5.Bieck AD, Biggs WS, Crosley PW, Kozakowski SM. Results of the 2012 National Resident Matching Program: family medicine. Fam Med. 2012;44(9):615–619. [PubMed] [Google Scholar]
- 6.Josiah Macy Jr Foundation and Association of Academic Health Centers. Optimizing the Structure, Support, Oversight, and Accountability of GME to Best Meet the Needs of the American People. Vol. 2010. Atlanta, GA: Association of Academic Health Centers; Ensuring an effective physician workforce for America: recommendations for an accountable workforce for America; pp. 2–3. [Google Scholar]
- 7.Girard DE, Brunett P, Cedfeldt A, Bower EA, Flores C, Rajhbeharrysingh U, et al. Plug the leak: align public spending with public need. J Grad Med Educ. 2012;4(3):293–295. doi: 10.4300/JGME-D-11-00199.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medicare Payment Advisory Commission. Report to the Congress: Aligning Incentives in Medicare. Washington, DC: Medicare Payment Advisory Commission; 2010. [Google Scholar]
- 9.GAO announces appointments to new National Health Care Workforce Commission. http://www.gao.gov/press/nhcwc_2010sep30.html. Accessed April 29, 2013. [Google Scholar]
- 10.HAAD standards for the allocation of physicians in residency training programs in the Emirate of Abu Dhabi (TANSEEQ) http://www.haad.ae/HAAD/LinkClick.aspx?fileticket=-tIvjCDbVi4%3d&tabid=819. Accessed April 29, 2013. [Google Scholar]
- 11.Zeidel ML, Kroboth F, McDermot S, Mehalic M, Clayton CP, Rich EC, et al. Estimating the cost to departments of medicine of training residents and fellows: a collaborative analysis. Am J Med. 2005;118(5):557–564. doi: 10.1016/j.amjmed.2005.02.025. [DOI] [PubMed] [Google Scholar]
- 12.Frank JR, editor. The CanMEDS 2005 Physician Competency Framework: Better Standards. Better Physicians. Better Care. Ottawa, Canada: Royal College of Physicians and Surgeons of Canada; 2005. [Google Scholar]
- 13.Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007;29(7):648–654. doi: 10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 14.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system—rationale and benefits. New Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 15.Hodges BD. A tea-steeping or i-Doc model for medical education. Acad Med. 2010;85(9 suppl):S34–S44. doi: 10.1097/ACM.0b013e3181f12f32. [DOI] [PubMed] [Google Scholar]
- 16.Britt H, Miller GC, Charles J, Henderson J, Bayram C, Valenti L, et al. 2009. General practice activity in Australia 1999–00 to 2008–09: 10 year data tables. General practice series no. 26. Cat. no. GEP 26. Canberra: AIHW.18. [Google Scholar]
- 17.Australian Health Workforce Advisory Committee. 2004. The Australian Allied Health Workforce—An Overview of Workforce Planning Issues, AMWAC Report 2006.1. Sydney: [Google Scholar]
- 18.Australian Medical Workforce Advisory Committee. 2001. The Specialist Anaesthesia Workforce In Australia, AMWAC Report 2001.5. Sydney: [Google Scholar]
- 19.McGinnis S, Moore J, Armstrong D. The Emergency Care Workforce in the United States. Rensselaer, NY: Center for Health Workforce Studies, School of Public Health, SUNY Albany. August 2006. [Google Scholar]