Abstract
Background
Rising costs pose a major threat to US health care. Residency programs are being asked to teach residents how to provide cost-conscious medical care.
Methods
An educational intervention incorporating the American College of Radiology appropriateness criteria with lectures on cost-consciousness and on the actual hospital charges for abdominal imaging was implemented for residents at Scripps Mercy Hospital in San Diego, CA. We hypothesized that residents would order fewer abdominal imaging examinations for patients with complaints of abdominal pain after the intervention. We analyzed the type and number of abdominal imaging studies completed for patients admitted to the inpatient teaching service with primary abdominal complaints for 18 months before (738 patients) and 12 months following the intervention (632 patients).
Results
There was a significant reduction in mean abdominal computed tomography (CT) scans per patient (1.7–1.4 studies per patient, P < .001) and total abdominal radiology studies per patient (3.1–2.7 studies per patient, P = .02) following the intervention. The avoidance of charges solely due to the reduction in abdominal CT scans following the intervention was $129 per patient or $81,528 in total.
Conclusions
A simple educational intervention appeared to change the radiologic test-ordering behavior of internal medicine residents. Widespread adoption of similar interventions by residency programs could result in significant savings for the health care system.
Editor’s Note: The online version of this article contains an example of the carry-along card provided to residents in this study. (34KB, doc)
What was known
Despite rising health care costs, residency programs have yet to seriously teach cost-conscious medical decision making to future physicians.
What is new
An educational intervention incorporating the American College of Radiology appropriateness criteria with lectures on cost-consciousness and on the actual hospital charges for abdominal imaging.
Limitations
Single-site, single-specialty intervention limits generalizability.
Bottom line
A simple educational intervention appeared to change the radiologic test-ordering behavior of internal medicine residents.
Introduction
“Nobody would quarrel with the proposition that there is a limit to the resources any society can devote to medical care and few would question the suggestion that we are approaching such a limit.”1 This statement from an editorial written in 1975 reminds us that reducing health-care expenditures in the United States has been a long-lasting struggle. The United States has the most expensive health care system in the world.2 The relentless increase in the cost of health care has been identified as the single largest threat to the future of health care in our nation.3,4
Optimizing the practice of cost-conscious medicine is essential. Nevertheless, US medical education has yet to seriously teach cost-conscious medical decision making to future physicians.5,6 Only 25% of residency programs have formal methods to teach about the costs of diagnostic tests, treatments, and medications to residents.6 Surveys of residents across multiple specialties suggest that current efforts to teach cost-conscious test ordering in undergraduate medical education are inadequate.7 It is therefore not surprising that most physicians do not appear to know the costs of the laboratory tests, imaging studies, or medications they order for their patients.3,8–18
The call has been made for residency programs to include teaching cost-consciousness in providing care as part of their educational curriculum.6,7,16,17,19. Adoption of cost-consciousness and stewardship of resources has been proposed as a new seventh competency.3 Medical imaging has been identified as an attractive target for resident education because data suggest that many imaging examinations are ordered inappropriately, and that there are acceptable, less expensive diagnostic alternatives.20–22
An educational intervention on cost-conscious and appropriate abdominal imaging was launched at Scripps Mercy Hospital in September 2010. This intervention incorporated the American College of Radiology (ACR) appropriateness criteria for abdominal imaging,23,24 along with lectures on cost-conscious medical decision making and discussion of the actual hospital charges for commonly ordered abdominal studies. We hypothesized that the intervention would reduce resident ordering of abdominal computed tomography (CT) scans and result in demonstrable overall cost reductions.
Methods
Study Site
Scripps Mercy Hospital is a community-based teaching hospital and level-one trauma center in San Diego, CA. Scripps Mercy has an Accreditation Council for Graduate Medical Education (ACGME)-accredited internal medicine program with 33 residents, a family medicine program with 24 residents, and a transitional year program with 18 residents.
Inclusion Criteria
Patients included in this study were retrospectively identified by hospital records showing a diagnosis-related group (DRG) assigned to an attending physician on the internal medicine inpatient teaching service. Patients were included if they were admitted between March 1, 2008, and February 28, 2011, and if they had an International Classification of Diseases, Ninth Revision (ICD-9) code from discharge that was among 166 codes identified by the primary authors to signify an abdominal pain complaint during admission. Representative ICD-9 codes included 150.1 to 157.9, 530.1 to 578.9, and 787.01 to 789.09. There were 1370 patients who met inclusion criteria. Less than 5% of patients were seen privately by an attending physician without resident involvement. These private patients were included because they could not be distinguished from patients with resident involvement by available records.
Interventions
The educational intervention was launched at Scripps Mercy Hospital on September 2, 2009, for internal medicine and transitional year residents. It consisted of four 60-minute lectures for the 2009–2010 and 2010–2011 academic years with provision of a pocket-sized carry-along card residents were instructed to carry while on duty. The card contained abbreviated ACR appropriateness criteria for common abdominal pain complaints, the actual hospital charges in dollars, and the radiation exposure in millisieverts (mSv) for common abdominal imaging studies (the card is provided as online supplemental material). The internal medicine residency program director also provided ongoing instruction on cost-consciousness and appropriate medical decision making during resident morning report.
The intervention was targeted toward residents instead of teaching faculty because residents were thought to be more apt to change their ordering behavior. Furthermore, residents were expected to write all orders for diagnostic imaging on teaching in-patients. In practice, interns (postgraduate year-1 residents) write these orders under the supervision of the senior internal medicine resident.
Lectures were given between September 2, 2009, and March 31, 2010, and between November 29, 2010, and January 5, 2011, for each respective year. Cumulative lecture attendance by residents was 66% compared to an overall attendance of 62% for all lectures during these academic years. Attending physicians from the teaching service were aware of the intervention but largely did not attend the lectures.
Lecture topics included ACR appropriateness criteria for abdominal imaging, hospital charges for common abdominal imaging modalities, and general principles of cost-conscious medicine. Lectures were taught by chief residents and senior program faculty from the departments of internal medicine and radiology. The lectures replaced alternative lecture topics and did not reduce clinical work. The cost estimate for faculty preparation and teaching time is $3125 (25 hours at $125 per hour). The cost of the carry-along cards was $480.
Outcomes
Primary outcomes were the total number of abdominal and pelvic CT scans, magnetic resonance imaging (MRI) plus ultrasound examinations, and abdominal imaging studies of all modalities (including plain radiographs) per patient before and after the intervention. Secondary outcomes included average patient length of stay, in-hospital mortality, average patient radiation exposure from medical imaging, patient satisfaction scores, average patients per in-patient team and average imaging studies completed per patient per hospital day.
Data Collection
Hospital financial records were accessed for patients meeting inclusion criteria. A database was created that contained the total units of CT, MRI, ultrasound and plain film examinations of the abdomen and pelvis and the other outcome measures, as described. Institutional Review Board approval for this study was obtained from Scripps Health on September 8, 2011.
Statistical Analysis
Patients were divided into 2 groups according to hospital admission dates. The preintervention group consisted of patients admitted prior to September 2, 2009 (first date of intervention), totaling 18 months. The postintervention group included patients admitted after March 9, 2010 (the last date of the 2009–2010 intervention). Patients receiving care while the intervention was ongoing were excluded from analysis. There were 738 patients in the preintervention and 632 patients in the postintervention group.
Statistical analysis was completed using SPSS (version 12.0). Independent samples t-tests were completed for each of the outcome measures. P < .05 was considered significant.
Results
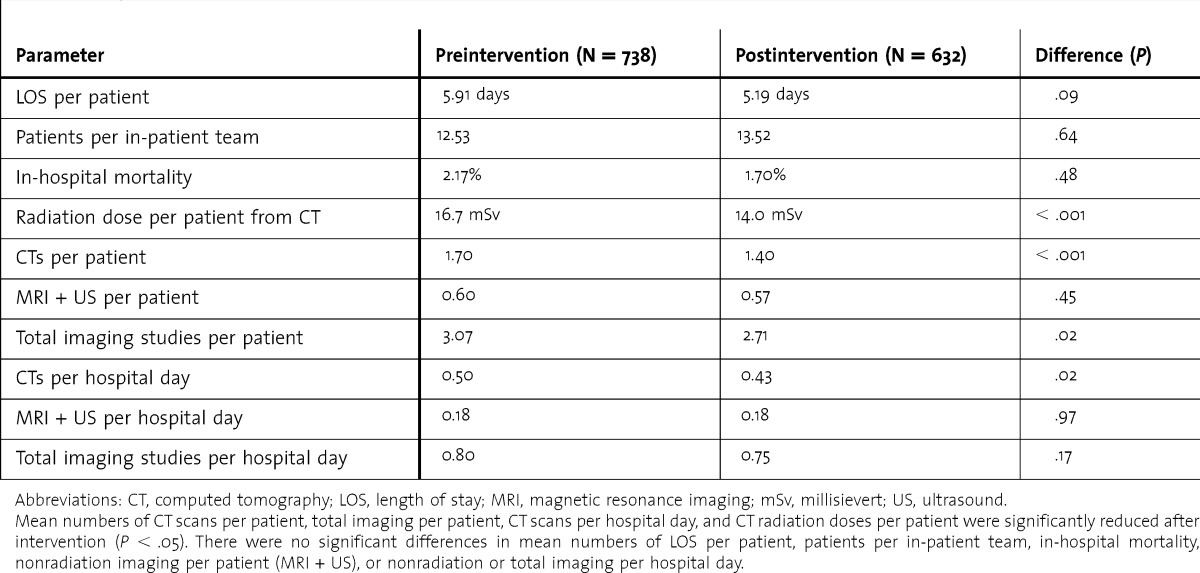
Following the educational intervention mean abdominal CT scans per patient were significantly reduced from 1.7 to 1.4 studies (P < .001). Total abdominal imaging studies per patient (all imaging modalities) also were significantly reduced from 3.1 to 2.7 studies (P = .02). Combined MRI and ultrasound studies per patient (radiation-free modalities) showed no significant difference (0.60–0.57 studies, respectively, P = .45).
The mean number of abdominal CT scans per patient per hospital day decreased significantly from 0.50 studies to 0.43 studies (P = .02). Combined MRI and ultrasound studies per patient per hospital day was unchanged at 0.18 studies (P = .97). The total radiology studies per patient per hospital day (all modalities) and the average patient length of stay demonstrated no significant difference (0.80–0.75 studies per patient per day, P = .17 and 5.4–4.8 days, P = .42, respectively).
There was no difference for in-hospital mortality pre- and postintervention (2.17% and 1.70%, respectively, P = .48). The average patient radiation dose from medical imaging decreased significantly from 16.7 mSv to 14.0 mSv (P < .001). There was no significant difference in the average number of patients per inpatient team (12.53 for pre- and 13.53 for postintervention periods, P = .64 (table shows a summary of results).
Table.
Results of Intervention
The distribution of types of patient insurance had no significant difference pre- and postintervention (HMO and PPO, 11.7% and 10.4%; Medicare, Medicaid, and other government insurance, 71.1% and 70.7%; self-pay, 16.3% and 16.6%; and hospice 0.8% and hospice 0.8% and 0.2%, respectively).
Patient satisfaction data corresponding to the exact pre-and postintervention periods was not available. Patient satisfaction scores for the calendar years encompassing much of the preintervention (January 1, 2008 to December 31, 2009, n = 1064) and postintervention periods (January 1, 2010 to December 31, 2011, n = 780) were available. The proportion of teaching service in-patients who rated their overall medical care as 9 or greater on a 10-point survey (10 signifying excellence) was not significantly different between the 2 years (69% and 68%, respectively, P = 0.65).
Discussion
Our study demonstrates that a simple educational intervention at a community-based teaching hospital significantly reduced radiologic test-ordering behavior of internal medicine residents on the inpatient floors. The avoidance of charges attributed to the intervention from abdominal CT scans alone was $129 per patient or $81,528 in total. This is significant because the intervention was completed at minimal cost (total costs are estimated at $3,605).
A number of educational interventions have attempted to teach cost-consciousness to physicians and many have been costly to implement. Many of these interventions require significant alterations of electronic medical records,9,13,25,26 or active auditing of physician orders and patient charges for physician feedback.12,27,28 The high cost of implementation stands as a barrier to widespread adoption of similar interventions by other residency programs. The simplicity and affordability of this intervention are its most notable features. Any residency program could institute a similar intervention without burdening financial or faculty resources. At the same time, there are nonfinancial barriers to implementing similar interventions, including ease by which advanced imaging answers clinical questions and the capability of modalities such as CT to exclude a myriad of alternative diagnoses thereby reducing missed diagnoses and medical malpractice. These barriers to implementation may have a greater impact on programs such as emergency medicine residencies.
Previous educational interventions designed to teach residents cost-consciousness and reduce hospital expenditures have not enjoyed universal success.29 The most prominent of these was a 2-year prospective controlled trial completed before the current prospective payment system for hospitals was enacted.30 This intervention attempted to reduce utilization of expensive services including diagnostic imaging, which was in direct conflict with the financial incentives of the institution. Recognizing this conflict, the authors stated, “Such education, however, may be an effective adjunct in settings where financial and organizational incentives promote cost control.”30 Future payment systems likely will continue to favor hospitals and physicians that reduce expenditures while maintaining high-quality care. This leads to an environment where financial incentives promote cost-conscious medicine priming interventions such as ours for success.
Past research also suggests that “a central authority figure may be a crucial experimental variable common to previous successful cost containment efforts in teaching hospitals”30 and “improvement is unlikely…if the attending staff members evidence little interest in the problem or are unwilling to be role models.”31 Our intervention benefited from the enthusiastic support and active participation of senior program faculty from multiple departments. Having respected central authority figures involved in the implementation, promotion, and daily reinforcement of the intervention was a crucial element of our design.8
There is robust evidence that increased awareness of the cost of tests results in reductions in expensive test orders by physicians.16,28,32–34 Our lectures combined instruction on the cost of medical imaging with a thorough presentation of the ACR appropriateness criteria for abdominal imaging. Combining these topics was another key element of our educational design.
Our study has several limitations. It is possible that widespread increased awareness of escalating health care costs and overuse of diagnostic imaging influenced the ordering behavior of residents independent of the intervention. If true, this increased awareness may have supported the legitimacy of our intervention and increased residents' motivation to change. A small number of patients whom residents did not treat were included in the analysis because they were not distinguishable from teaching patients from the available records. Abdominal imaging studies ordered by emergency medicine physicians prior to admission were also included in our analysis for similar reasons. We do not know what effect this may have had on our results. Any differences resulting from orders placed by these nonresident physicians may be balanced between the pre- and postintervention periods thereby having minimal overall effect.
There was no washout period in our research design. The long-term impact of our intervention on resident ordering behavior is uncertain. Other studies with similar interventions lasting 3 to 6 months demonstrated loss of approximately one-half of the intervention's effect within 1 to 5 months after the intervention ended.9,16 This suggests the need for a longer intervention period and subsequent periodic reinforcement of core principles for changes in physician behavior to persist over time.
Finally, it is possible that decreased utilization of CT imaging caused increased use of alternative diagnostic testing. We did not monitor for reciprocal increases in laboratory testing during the postintervention period. Increased ordering of alternative imaging examinations was monitored. Following the intervention there was a significant reduction in abdominal imaging studies of all modalities, including ultrasound and MRI. Reductions in CT imaging did not increase average hospital length of stay. These trends support overall cost-savings attributable to our educational intervention.
Conclusion
A simple educational intervention on cost-conscious medicine appeared to reduce radiologic test-ordering behavior of internal medicine residents on the inpatient floors. Widespread adoption of similar educational interventions by other residency programs could result in significant savings to hospitals and the health care system.
Footnotes
All authors are at Scripps Mercy Hospital. Matthew F. Covington, MD, is a transitional year resident; Donna L. Agan, EdD, is a Nursing Data Analyst; Yang Liu, MBA, is Senior Financial Analyst in the Finance Department; John O. Johnson, MD, is Chief of CT Imaging at Scripps Mercy Hospital and Chief of CT Imaging at Imaging Healthcare Specialists; and David J. Shaw, MD, MBA, is Director of Medical Education and Clinical Professor of Medicine (unsalaried) at University of California San Diego.
Funding: The authors report no external funding source for this study.
The authors wish to thank Stanley A. Amundson, MD, Program Director of the Internal Medicine Residency Program at Scripps Mercy Hospital, for expert teaching of cost-conscious medicine and appropriate medical imaging during daily resident morning reports. The authors also wish to thank Marin Xavier, MD, for superb lectures on cost-conscious use of blood products.
References
- 1.Hiatt HH. Protecting the medical commons: who is responsible. N Engl J Med. 1975;293(5):235–241. doi: 10.1056/NEJM197507312930506. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T. High and rising health care costs. Part 1. Seeking an explanation. Ann Intern Med. 2005;142:847–854. doi: 10.7326/0003-4819-142-10-200505170-00010. [DOI] [PubMed] [Google Scholar]
- 3.Weinberger SE. Providing high-value, cost-conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155386:388. doi: 10.7326/0003-4819-155-6-201109200-00007. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. The Healthcare Imperative: Lowering Costs and Improving Outcomes. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 5.Cooke M. Cost consciousness in patient care—what is medical education's responsibility. N Engl J Med. 2010;362:1253–1255. doi: 10.1056/NEJMp0911502. [DOI] [PubMed] [Google Scholar]
- 6.Medicare Payment Advisory Commission (MedPac) 2009 report to the congress: improving incentives in the Medicare program. June 2009. http://www.medpac.gov/documents/jun09_entirereport.pdf. Accessed February 21, 2013. [Google Scholar]
- 7.Roberts JL, Ostapchuk M, Hughes K, Ziegler CH. What residents know about health care reform and what we should teach them. J Grad Med Educ. 2011;3(2):155–161. doi: 10.4300/JGME-D-10-00122.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eisenberg JM, Williams SV. Cost containment and changing physicians' practice behavior. Can the fox learn to guard the chicken coop. JAMA. 1981;246(19):2195–2201. [PubMed] [Google Scholar]
- 9.Tierney WM, Miller ME, McDonald CJ. The effect on test ordering of informing physicians of the charges for outpatient diagnostic tests. N Engl J Med. 1990;322(21):1499–1504. doi: 10.1056/NEJM199005243222105. [DOI] [PubMed] [Google Scholar]
- 10.Shulkin DJ. Cost estimates of diagnostic procedures. N Engl J Med. 1988;319:1291. doi: 10.1056/NEJM198811103191919. [DOI] [PubMed] [Google Scholar]
- 11.Thomas DR, Davis KM. Physician awareness of cost under prospective reimbursement systems. Med Care. 1987;25:181–184. doi: 10.1097/00005650-198703000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Sachdeva RC, Jefferson LS, Coss-Bu J, Done G, Campbell D, et al. Effects of availability of patient-related charges on practice patterns and cost containment in the pediatric intensive care unit. Crit Care Med. 1996;24(3):501–506. doi: 10.1097/00003246-199603000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Bates DW, Kuperman GJ, Jha A, Teich JM, Orav EJ, et al. Does the computerized display of charges affect inpatient ancillary test utilization. Arch Intern Med. 1997;157(21):2501–2508. [PubMed] [Google Scholar]
- 14.Cosimi AB. Modern day bloodletting: is that laboratory test necessary. Arch Surg. 2011;146(5):527. doi: 10.1001/archsurg.2011.104. [DOI] [PubMed] [Google Scholar]
- 15.Schaefer GR, Matus HL, Goetz C, Arora VM. Magnetic resonance imaging monsters and surgical vampires. Arch Surg. 2011;146(11):1333. doi: 10.1001/archsurg.2011.284. [DOI] [PubMed] [Google Scholar]
- 16.Hampers LC, Cha S, Gutglass DJ, Krug SE, Binns HJ. The effect of price information on test-ordering behavior and patient outcomes in a pediatric emergency department. Pedatrics. 1999;103:877–882. [PubMed] [Google Scholar]
- 17.Stuebing EA, Miner TJ. Surgical vampires and rising health care expenditure: reducing the cost of daily phlebotomy. Arch Surg. 2011;146(5):524–527. doi: 10.1001/archsurg.2011.103. [DOI] [PubMed] [Google Scholar]
- 18.Graham JD, Potyk D, Raimi E. Hospitalists' awareness of patient charges associated with inpatient care. J Hosp Med. 2010;5(5):295–297. doi: 10.1002/jhm.655. [DOI] [PubMed] [Google Scholar]
- 19.Blackstone ME, Miller RS, Hodgson AJ, Cooper SS, Blackhurst DW, et al. Lowering hospital charges in the trauma intensive care unit while maintaining quality of care by increasing resident and attending physician awareness. J Trauma. 1995;39(6):1041–1044. doi: 10.1097/00005373-199512000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Bautista AB, Burgos A, Nickel BJ, Yoon JJ, Tilara AA, et al. Do clinicians use the American College of Radiology Appropriateness criteria in the management of their patients. AJR Am J Roentgenol. 2009;192(6):1581–1585. doi: 10.2214/AJR.08.1622. [DOI] [PubMed] [Google Scholar]
- 21.Rowan K. Rising costs of medical imaging spur debate. Natl Cancer Inst. 2008;100(23):1665–1667. doi: 10.1093/jnci/djn430. [DOI] [PubMed] [Google Scholar]
- 22.Taragin BH, Feng L, Ruzal-Shapiro C. Online radiology appropriateness survey: results and conclusions from an academic internal medicine residency. Acad Radiol. 2003;10:781–785. doi: 10.1016/s1076-6332(03)80123-x. [DOI] [PubMed] [Google Scholar]
- 23.American College of Radiology. ACR appropriateness criteria. http://www.acr.org/ac. Accessed February 21, 2013. [Google Scholar]
- 24.Gunderman RB, Bettmann M, Davis LP. Promoting educational innovation: lessons from the request for proposals for ACR appropriateness criteria usage in medical education. J Am Coll Radiol. 2007;4:919–924. doi: 10.1016/j.jacr.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Sistrom CL, Dang PA, Weilburg JB, Dreyer KJ, Rosenthal DI, et al. Effect of computerized order entry with integrated decision support on the growth of outpatient procedure volumes: seven-year time series analysis. Radiology. 2009;251(1):147–155. doi: 10.1148/radiol.2511081174. [DOI] [PubMed] [Google Scholar]
- 26.Vartanians VM, Sistrom CL, Weilburg JB, Rosenthal DI, Thrall JH. Increasing the appropriateness of outpatient imaging: effects of a barrier to ordering low-yield examinations. Radiology. 2010;255(3):842–849. doi: 10.1148/radiol.10091228. [DOI] [PubMed] [Google Scholar]
- 27.Cummings KM, Frisof KB, Long MJ, Hrynkiewich G. The effects of price information on physicians' test-ordering behavior. Med Care. 1982;20(3):293–301. doi: 10.1097/00005650-198203000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Seguin P, Bleichner JP, Grolier J, Guillou YM, Malledant Y. Effects of price information on test ordering in an intensive care unit. Intensive Care Med. 2002;28:332–335. doi: 10.1007/s00134-002-1213-x. [DOI] [PubMed] [Google Scholar]
- 29.Schroeder SA. Personal reflections on the high cost of American medical care: many causes but few politically sustainable solutions. Arch Intern Med. 2011;171:722–727. doi: 10.1001/archinternmed.2011.149. [DOI] [PubMed] [Google Scholar]
- 30.Schroeder SA, Myers LP, McPhee SJ, Showstack JA, Simborg DW, et al. The failure of physician education as a cost containment strategy: report of a prospective controlled trial at a university hospital. JAMA. 1984;252(2):255–230. [PubMed] [Google Scholar]
- 31.Walt AJ. Can cost containment be learned in a surgical residency. Bull Am Coll Surg. 1994;79(9):8–12. [PubMed] [Google Scholar]
- 32.Sood R, Sood A, Ghosh AK. Nonevidenced-based variable affecting physicians' test-ordering tendencies: a systematic review. Neth J Med. 2007;65(5):167–177. [PubMed] [Google Scholar]
- 33.Rudy DW, Ramsbottom-Lucier M, Griffith CH, III, Georgesen JC, Wilson JF. A pilot study assessing the influences of charge data and group process on diagnostic test ordering by residents. Acad Med. 2001;76:635–637. doi: 10.1097/00001888-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Vegting IL, Van Beneden M, Kramer MH, Thijs A, Kostense PJ, et al. How to save costs by reducing unnecessary testing: lean thinking in clinical practice. Eur J Intern Med. 2012;23(1):70–75. doi: 10.1016/j.ejim.2011.07.003. [DOI] [PubMed] [Google Scholar]


